Introduction
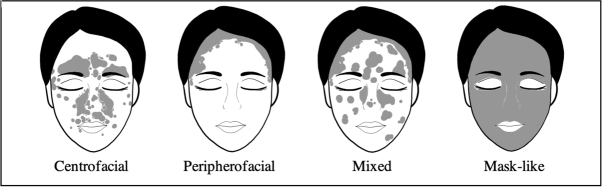
Lesions of psoriasis are commonly seen on extensor surfaces, including the elbows and knees, as well as on the scalp, the umbilicus, and the lumbar region.1,2 The presentation of psoriasis may be localized to one or more of these regions or may be generalized. Less frequently, lesions of psoriasis are seen on the face, palms, soles, and intertriginous regions.3 Facial psoriasis has been categorized into 3 descriptive subtypes: peripherofacial (hairline psoriasis), centrofacial (sebopsoriasis), and mixed (true facial psoriasis).3,4
Here we present a case of severe plaque psoriasis with diffuse facial involvement that responded to treatment with adalimumab. This case highlights a rare presentation of facial psoriasis and emphasizes the debilitating nature of facial psoriasis. Based on this disease presentation, we propose a fourth subtype of facial psoriasis involving the entire face in a mask-like distribution.
Case report
A 51-year-old Caucasian man presented to the dermatology clinic in January 2015 with an extensive rash on the face, scalp, trunk, and limbs. The patient had a history of well-controlled mild to moderate plaque psoriasis. Economic hardship and increased stress were followed by a rapid worsening of his disease, including new onset of facial psoriasis. At this time, he lost his job, distanced himself from family and friends, and followed a more reclusive lifestyle. This continued as a downward spiral into depression and increasing alcohol abuse.
Physical examination in the clinic revealed confluent erythematous plaques involving 80% of the body surface area, with plate-like hyperkeratosis covering the entire face (Fig 1, A). A complete blood count showed a mild reactive leukocytosis, and skin biopsy was consistent with plaque-type psoriasis. The patient was started on an 80-mg subcutaneous loading dose of adalimumab, a tumor necrosis factor-α antagonist approved for the treatment of plaque psoriasis and psoriatic arthritis. This was followed by a maintenance dose of 40-mg adalimumab administered subcutaneously every 2 weeks. Treatment with adalimumab resulted in complete resolution of the psoriatic plaques over several months, with significant improvement in quality of life (Fig 1, B).
Fig 1.
A, Presentation of facial psoriasis in a mask-like distribution. B, Resolution following treatment with adalimumab.
Discussion
Approximately 50% of psoriasis patients attending psoriasis clinics have facial involvement.3,5,6 Facial involvement is more common in younger individuals and those with a higher mean Psoriasis Area Severity Index (PASI).3 Thus, facial psoriasis may be considered a marker of disease severity. Among the 3 previously defined subtypes of facial psoriasis, centrofacial is the most severe and is characterized by lesions localized to the seborrheic areas.3,4 In contrast, peripherofacial psoriasis consists of lesions within the hairline.4 Mixed facial psoriasis is the most common subtype and consists of classic plaque psoriasis morphology with well-defined lesions.3,4 The case described here does not fall within any of the 3 previously defined subtypes. Our patient presented with a rare subtype of confluent facial psoriasis without predilection to either the hairline or the seborrheic areas, and this case may therefore illustrate a fourth subtype of the disease (Fig 2). There was extensive confluent involvement of the eyelids and upper lip, locations not characteristic of mixed involvement, and there was no history or evidence of coalescence at the hairline or central face involvement. The plate-like appearance of the scale is not typically seen in facial psoriasis and is more similar to that sometimes seen on the trunk and limbs.
Fig 2.
Illustrations of centrofacial, peripherofacial, mixed, and mask-like facial psoriasis.
Facial psoriasis not only results in physical challenges, including impaired vision, hearing, and chewing, but can also be psychosocially debilitating due to the visibility of the facial lesions.3,7 Studies evaluating quality of life indices showed a greater negative impact in patients diagnosed with facial psoriasis than in those diagnosed with plaque psoriasis of the body. Further, univariate analysis for depression, anxiety, stress, and impairment of quality of life by clinical characteristics revealed that facial involvement was significantly correlated with depression and anxiety.8 The increased risk of depression, anxiety, and suicide among patients diagnosed with psoriasis is often not fully appreciated by physicians; dermatologists and primary care physicians should be educated about markers of increased risk, including the presence of facial lesions. In addition to those with facial involvement, high-risk groups include young patients and patients with severe disease.8 Although both genders are at risk for suicidal ideation and depression, women present with greater distress pertaining to psoriasis.9
Therapy for facial psoriasis includes topical therapies, such as calcineurin inhibitors, systemic corticosteroids, and vitamin D analogs.3 More recently, biologic therapies have become the mainstay for treatment of moderate to severe plaque psoriasis, despite their high cost and need for subcutaneous administration. A recent study evaluating more than 1100 patients with facial psoriasis showed that ixekizumab, an interleukin 17A antagonist, is an effective treatment alternative to traditional therapies.10 Adalimumab is also efficacious in the treatment of facial psoriasis, with superior responses when compared to methotrexate or placebo.3 The selection of adalimumab as biologic therapy was based on the patient's insurance coverage in this case. Use of biologic therapies may provide both a physical and a psychosocial benefit through improvement of facial psoriasis.
In conclusion, we report a case of diffuse facial psoriasis in a mask-like distribution that may represent a fourth subtype of this disease. This case underscores the psychosocial ramifications of facial involvement in psoriasis and the dramatic psychological benefit with disease remission following biologic therapy.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
IRB approval status: Not applicable.
References
- 1.Casciano F., Pigatto P.D., Secchiero P., Gambari R., Reali E. T cell hierarchy in the pathogenesis of psoriasis and associated cardiovascular comorbidities. Front Immunol. 2018;9:1390. doi: 10.3389/fimmu.2018.01390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schön M.P., Boehncke W.H. Psoriasis. N Engl J Med. 2005;352(18):1899–1912. doi: 10.1056/NEJMra041320. [DOI] [PubMed] [Google Scholar]
- 3.Merola J.F., Qureshi A., Husni M.E. Underdiagnosed and undertreated psoriasis: nuances of treating psoriasis affecting the scalp, face, intertriginous areas, genitals, hands, feet, and nails. Dermatol Ther. 2018;31(3):e12589. doi: 10.1111/dth.12589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van de Kerkhof P.C., Murphy G.M., Austad J., Ljungberg A., Cambazard F., Duvold L.B. Psoriasis of the face and flexures. J Dermatolog Treat. 2007;18(6):351–360. doi: 10.1080/09546630701341949. [DOI] [PubMed] [Google Scholar]
- 5.Park J.Y., Rim J.H., Choe Y.B., Youn J.I. Facial psoriasis: comparison of patients with and without facial involvement. J Am Acad Dermatol. 2004;50(4):582–584. doi: 10.1016/s0190-9622(03)02793-2. [DOI] [PubMed] [Google Scholar]
- 6.Passos A.N., de A., Rego V.R.P. Facial involvement and the severity of psoriasis. Int J Dermatol. 2019;58(11):1300–1304. doi: 10.1111/ijd.14492. [DOI] [PubMed] [Google Scholar]
- 7.Beattie P.E., Lewis-Jones M.S. A comparative study of impairment of quality of life in children with skin disease and children with other chronic childhood diseases. Br J Dermatol. 2006;155(1):1145–1151. doi: 10.1111/j.1365-2133.2006.07185.x. [DOI] [PubMed] [Google Scholar]
- 8.Kwan Z., Bong Y.B., Tan L.L. Determinants of quality of life and psychological status in adults with psoriasis. Arch Dermatol Res. 2018;310(5):443–451. doi: 10.1007/s00403-018-1832-x. [DOI] [PubMed] [Google Scholar]
- 9.Nicholas M.N., Gooderham M. Psoriasis, depression, and suicidality. Skin Ther Lett. 2017;22(3):1–4. [PubMed] [Google Scholar]
- 10.Paul C., Guenther L., Torii H. Impact of ixekizumab on facial psoriasis and related quality of life measures in moderate-to-severe psoriasis patients: 12-week results from two phase III trials. J Eur Acad Dermatol Venereol. 2018;32(1):68–72. doi: 10.1111/jdv.14581. [DOI] [PubMed] [Google Scholar]