Highlights
-
•
Orbital metastases of breast cancer are an exceptional event.
-
•
Orbital metastases are generally asymptomatic and therefore misdiagnosed.
-
•
Extraocular muscles are rarely infiltrated by metastatic tumors from distant sites.
-
•
Metastases usually disseminate late from breast cancer. Our case report is an unusual case of early orbital infiltration from breast cancer.
Keywords: Orbital metastasis, Breast cancer, Surgical biopsy
Abstract
Introduction
Orbital metastases from solid cancers are infrequent or underestimated, since they represent only 1–13% of tumors of the orbit. They are even less frequent in breast cancer and are rarely diagnosed. We report a case of an early diagnosed orbital metastasis from breast cancer to an extra ocular muscle.
Case report
We report the case of a 33-year-old female patient who presented, following the diagnosis of her breast cancer, headache, a progressive decrease in visual acuity of the right eye and diplopia. Brain imaging revealed a tissue process at the expense of the internal rectus muscle, which biopsy pointed to a secondary lesion of breast cancer.
Discussion
Extraocular muscles are rarely infiltrated by metastasis from distant sites. They are mostly asymptomatic and suggest a systematic spread of the disease. The treatment is generally palliative and the prognosis is generally poor.
Conclusion
Orbital metastases from breast cancer are certainly rare but are associated with significant morbidity. In order to make a precise diagnosis and offer an appropriate treatment, healthcare professionals must remain vigilant in the face of any ophthalmological symptoms.
1. Introduction
Orbital metastases from solid cancers are infrequent or underestimated, accounting for only 1–13% of orbital tumors. Breast cancer is responsible of 28%–58.5% of these metastases [1]. Orbital involvement is an exceptional event in breast cancer and only 0.7% of the cases are symptomatic [2].
Extraocular muscles are rarely infiltrated by metastatic tumors from distant sites. The purpose of this report is to describe a metastatic involvement of the medial rectus muscle as an early sign of breast carcinoma and to discuss related literature on orbital metastasis of breast carcinoma.
2. Case report
2.1. Researchregistry6302
Our work is a single case report and has been reported in line with the SCARE criteria [3].
A 33 years old woman was admitted to the department of maxillofacial surgery because of double vision appearing a month ago. This symptom was reported to be sudden with gradual progression. She has been diagnosed with left breast cancer only a month before the occurrence of the diplopia. No other personal or family history was raised during the patient interrogation.
The clinical examination had found a mild restriction of elevation and abduction of the right eye without exophthalmos (Fig. 1), pupillary asymmetry or hypoaesthesia. Left eye movements were free in nine gaze positions. The breast examination found a nodule of about three cm long axis, located in the upper-external quadrant of the left breast, fixed, painful and the opposite skin of which is retracted. The cervical and axillary lymph node areas were free.
Fig. 1.
Restriction of the elevation and abduction of the right eye.
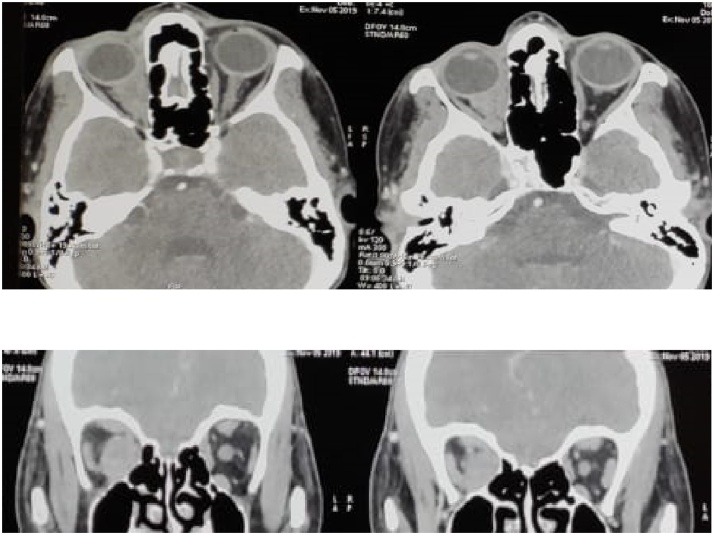
A facial computed tomography was performed showing a right orbital process at the expense of the internal rectus muscle. The patient underwent a surgical biopsy via the internal paracanthal approach in our department. Pathological examination of the surgical specimen confirmed the secondary origin of the process (Fig. 2).
Fig. 2.
Computed tomography of the orbits demonstrates a focal intraconal mass in the right eye englobing the medial rectus and optic nerve with indistinguishable borders.
The patient subsequently underwent a left mastectomy with ipsilateral lymph node dissection followed by adjuvant radio chemotherapy followed by a hormone therapy in both the gynecology and oncology departments of university hospital Ibn Rochd.
The three months, six months and one-year follow up examinations reveal a steady state of the orbital metastasis on physical examination and imaging, and the absence of new metastatic sites.
3. Discussion
Metastatic disease represents 1–13% of all orbital tumors. It is presumed that 1–5% of patients with systemic malignancies develop orbital metastases. Breast cancer is the malignant neoplasm that metastasizes to the orbit more frequently, representing 29–53% of cases [1].
While 85% of patients with orbital involvement carried a known cancer diagnosis, the metastasis was the harbinger of systemic disease in the remaining 15% [4]. The time from diagnosis of breast cancer to the onset of orbital metastases is usually prolonged, with an average of 2–8.5 years, although a case with 28 years delai has been reported [5,6]. In our case, the orbital metastasis was quickly diagnosed due to its early clinical manifestation (one month).
The pathogenesis of orbital localization of breast cancer carcinoma has not been fully understood. The presence of such metastases suggests a systemic haematogenous spread of the disease. In fact, anatomical studies describe limited lymphatic drainage in the orbit; therefore, distant metastases to the orbit occur through the blood flow [7]. Orbital metastases due to breast cancer can be the result of a cellular tropism caused by estrogens produced by periorbital fat in order to regulate tear film composition, which correlates with the majority of cases secondary to hormone-sensitive tumors [5,8]. On the other hand metastatic cancers are rarely seen in extraocular muscles. The constant movement of these muscles and their unfavorable chemical environment for neoplastic growth could prevent the neoplastic cell deposit or produce an unsuitable chemical environment for continued neoplastic growth [[9], [10], [11]].
Orbital metastasis are rarely symptomatic. An American retrospective study has detected symptomatic orbital involvement in only 0.7% of breast cancer cases [2]. Another Mexican study has reported that the most frequent symptoms of orbital metastasis were decreased visual acuity (64.2%), pain (57.1%), changes in mobility (28.5%) and edema (21.4%). Other symptoms included proptosis, diplopia, ptosis, enophthalmos and foreign body sensation [5].
A diagnostic imaging study consists of a magnetic resonance imaging (MRI) or a contrasted computed tomography (CT). It shows two patterns of orbital metastases from breast cancer: the first pattern is a mass appearance and exophthalmos and the second presents an infiltrating appearance [8]. MRI and CT are useful tools for the diagnosis; nevertheless, a definitive diagnosis is made by histological analysis of the lesion. Two technics have been described: a fine needle aspiration or open surgical biopsy, although this step may be omitted in patients with appropriately strong clinical histories and suggestive imaging features [1,12].
Since orbital involvement suggests a systematic spread of breast cancer, the treatment is generally palliative in the aims of controlling the growth of the metastatic mass, preserving eye's visual function and improving patient’s quality of life. Treatment approaches include surgery, radiotherapy, chemotherapy, hormonal therapy or a combination of these modalities. Orbital surgery is mainly used for diagnostic rather than therapeutic purposes; it may also be useful in the palliative management of some patients in order to improve their symptoms: surgical orbital decompression to reduce pressure on the optic nerve, orbitotomy, tarsorrhaphy and others [5,7]. Orbital radiotherapy (External beam radiation therapy (EBRT)) is the treatment of choice for controlling tumour’s size and preserving visual function [7,8,11,13]. Some cases of intraocular chemotherapy (bevacizumab) have been reported [2,5,13]. Systemic chemotherapy and hormone therapy are preferred especially when other synchronous metastases are present. The treatment can be adjusted depending on the clinical presentation, the extent of the metastatic disease and the immunohistochemical status of the tumor [7,13,14].
The prognosis of breast cancer with an orbital involvement has been reported to be very poor with survival ranges from 1 to 116 months with a mean of 31 months [5,7,15].
4. Conclusion
Orbital metastases from breast cancer are certainly rare but are associated with significant morbidity. In order to make a precise diagnosis and offer an appropriate treatment, healthcare professionals must remain vigilant in front of any patient with a breast cancer or breast cancer history who complains with ophthalmologic symptoms.
Conflicts of interest
None.
Sources of funding
None.
Ethical approval
Our study is exempted from ethnical approval.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Bahaa RAZEM: Study concept, data collection, writing the paper and making the revision of the manuscript following the reviewer’s instructions.
Faiçal SLIMANI: reviewing and validating the manuscript’s credibility.
Registration of research studies
researchregistry6302 available at: https://www.researchregistry.com/browse-the-registry#home/registrationdetails/5fc1316454e166001ba5a194/.
Guarantor
Slimani Faical.
RAZEM Bahaa.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Wladis E.J., Lee K.W., Nazeer T. Metastases of systemic malignancies to the orbit: a major review. Orbit. 2020:1–5. doi: 10.1080/01676830.2020.1759110. 27 avr. [DOI] [PubMed] [Google Scholar]
- 2.Pierson T.M., Tebit E.V., El Sayed A., Smolkin M.E., Dillon P.M. Orbital metastases from breast cancer: retrospective analysis at an academic cancer center. Breast J. 2016;22(4):447–540. doi: 10.1111/tbj.12604. [DOI] [PubMed] [Google Scholar]
- 3.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020 doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 4.Valenzuela A.A., Archibald C.W., Fleming B., Ong L., O’Donnell B., J JC Orbital metastasis: clinical features, management and outcome. Orbit. 2009;28(2–3):153–159. doi: 10.1080/01676830902897470. 1 janv. [DOI] [PubMed] [Google Scholar]
- 5.Grajales-Alvarez R., Gutierrez-Mata A. Orbital metastases from breast cancer: a retrospective analysis of 28 cases. Cancer Treat. Res. Commun. 2020;24 doi: 10.1016/j.ctarc.2020.100184. [DOI] [PubMed] [Google Scholar]
- 6.Milman T., Pliner L., Langer P.D. Breast carcinoma metastatic to the orbit: an unusually late presentation. Ophthal. Plast. Reconstr. Surg. 2008;24(6):480–482. doi: 10.1097/IOP.0b013e31818b6adc. [DOI] [PubMed] [Google Scholar]
- 7.Tsagkaraki I.M., Kourouniotis C.D., Gomatou G.L., Syrigos N.K., Kotteas E.A. Orbital metastases of invasive lobular breast carcinoma. Breast Dis. 2019;38(3–4):85–91. doi: 10.3233/BD-190398. [DOI] [PubMed] [Google Scholar]
- 8.Sindoni A., Fama’ F., Vinciguerra P., Dionigi G., Manara S.A.A.M., Gaeta R. Orbital metastases from breast cancer: a single institution case series. J. Surg. Oncol. 2020;122(2):170–175. doi: 10.1002/jso.25927. [DOI] [PubMed] [Google Scholar]
- 9.Coutinho I., Marques M., Almeida R., Custódio S., Simões Silva T., Águas F. Extraocular muscles involvement as the initial presentation in metastatic breast cancer. J. Breast Cancer. 2018;21(3):339–342. doi: 10.4048/jbc.2018.21.e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Framarino-dei-Malatesta M., Chiarito A., Bianciardi F., Fiorelli M., Ligato A., Naso G. Metastases to extraocular muscles from breast cancer: case report and up-to-date review of the literature. BMC Cancer. 2019;19(1):36. doi: 10.1186/s12885-018-5253-1. 8 janv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kızıloğlu Ö.Y., Türköz F.P., Gedar Ö.M.T., Mestanoğlu M., Yapıcıer Ö. Breast carcinoma metastasis to the medial rectus muscle: case report. Turk. J. Ophthalmol. 2019;49(3):168. doi: 10.4274/tjo.galenos.2018.39018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karti O., Ozdemir O., Karti D.T., Zengin M.O., Tatli S., Kusbeci T. Orbital metastasis secondary to breast cancer: a rare cause of unilateral external ophthalmoplegia. Neuro-Ophthalmology. 2020:1–3. doi: 10.1080/01658107.2019.1704030. 8 janv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kluska A., Papis-Ubych A., Fijuth J., Loga K., Spych M., Gottwald L. Intraorbital extraocular metastasis of breast cancer 11 years after mastectomy–case report and review of the literature. J. Obstet. Gynaecol. 2019;39(1):126–128. doi: 10.1080/01443615.2018.1455078. [DOI] [PubMed] [Google Scholar]
- 14.Jakobiec F.A., Stagner A.M., Homer N., Yoon M.K. Periocular breast carcinoma metastases: predominant origin from the lobular variant. Ophthal. Plast. Reconstr. Surg. 2017;33(5):361–366. doi: 10.1097/IOP.0000000000000793. [DOI] [PubMed] [Google Scholar]
- 15.Ahmad S.M., Esmaeli B. Metastatic tumors of the orbit and ocular adnexa. Curr. Opin. Ophthalmol. 2007;18(5):405–413. doi: 10.1097/ICU.0b013e3282c5077c. [DOI] [PubMed] [Google Scholar]