Highlights
-
•
Sertoli-Leydig cell tumors are rare sex-cord stromal tumors of the ovary.
-
•
We present a case of Sertoli-Leydig cell tumors with rhabdomyomatous differentiation on the setting of xeroderma pigmentosum.
-
•
We describe clinical, gross and microscopic examinations for diagnosis and treatment.
Keywords: Sertoli-Leydig cell tumor, Xeroderma pigmentosum, Heterologous elements, Rhabdomyomatous differentiation, Case report
Abstract
Introduction
Sertoli-Leydig cell tumors (SLCTs) are rare sex-cord stromal tumors of the ovary. Heterologous components may be present, most commonly in the intermediate differentiated and poorly differentiated groups. Because of their scarcity, SLCTs with heterologous differentiation represent a challenge in both diagnosis and management, with limited available experience.
Presentation of case
We report a case of a 27-year-old, Tunisian woman, followed in the Dermatology Department since the age of six months for xeroderma pigmentosum, with a history of basal cell carcinoma of the face operated on several times. The patient presented with abdominal pain and bloating associated with a medium abundance ascites on physical exam. Ultrasound showed a large left adnexal mass associated with an elevated cancer antigen 125 on serological exam. The patient underwent unilateral salpingo-oophorectomy with resection of two omental nodules. Microscopic examination concluded to poorly differentiated Sertoli-Leydig tumor with rhabdomyomatous differentiation. Adjuvant chemotherapy was performed and there was no clinical evidence of tumor recurrence during the three years of follow-up.
Discussion
SLCTs with rhabdomyomatous differentiation on the setting of xeroderma pigmentosum are exceptional, microscopic diagnosis and management is challenging, considering the tumor scarcity.
Conclusion
Further case reports and retrospective studies are required to more understand the pathogenesis of SLCTs and to determine their optimal treatment regimen.
1. Introduction
Sertoli-Leydig cell tumors (SLCTs) are rare sex-cord stromal tumors of the ovary, accounting for less than 0.5% of all ovarian tumors. SLCTs are divided into well-differentiated, intermediate differentiation, poorly differentiated, retiform, and mixed tumors. Heterologous components may be present, most commonly in the intermediate differentiation and poorly differentiated groups [1]. Because of their scarcity, SLCTs with heterologous differentiation represent a challenge in both the diagnosis and the management, with limited available experience [2].
In this article, we report a case of ovarian SLCT with rhabdomyomatous differentiation in a 27-year-old female with xeroderma pigmentosum and a review of the literature.
This work is in line with the SCARE criteria [3].
2. Case report
27-year-old Tunisian woman, single, has been followed in the Dermatology Pathology since the age of six months for xeroderma pigmentosum, with a history of basal cell carcinoma of the face operated on several times and without any family history. The patient was presented with abdominal pain and bloating associated with a medium abundance ascites on physical exam. The patient did not have drug allergy or psychosocial history. Serological studies showed elevated rate of cancer antigen125 (CA-125, 328.5 U/mL), whereas, rates of fetoprotein and CA19-9 were within the normal.
Ultrasound showed a large left adnexal mass, solid and cystic, with anarchic vascularization associated with ascites. At laparoscopy, the exploration was difficult due to the multiple adhesion of a large abdominal and pelvic tumor of ovarian origin to the pelvic wall associated with two omental nodules. Considering the young age of the patient and her desire for fertility, she underwent unilateral salpingo-oophorectomy with resection of omental nodules. A professor with 20 years of experience and the head of Obstetrics and Gynecology Department underwent the operation without any complication. The patient left the hospital after one week.
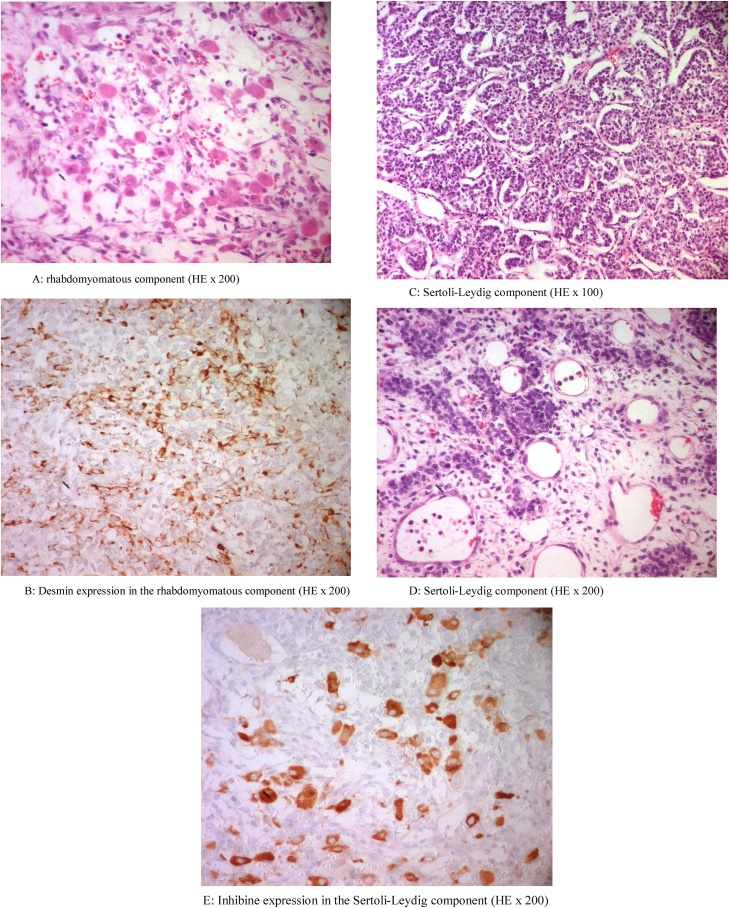
On macroscopic examination, the ovarian tumor was solid and cystic, with a thick wall and intact uniformly smooth outer surfaces, measuring 21 cm in large. The sectioning revealed gray to yellow fleshy tissue with areas of hemorrhage and necrosis. Microscopic examination showed a tumor formed by two components separated by fibrovascular septa. The first component was predominant and was formed by rhabdoid and spindle cells showing many figures of mitosis (Fig. 1a). On immunohisto chemical study, these cells displayed desmin and myogenin positivity, confirming the rhabdomyomatous differentiation (Fig. 1b). The second component comprised Sertoli cells arranged in islands or in ribbons (Fig. 1c), associated with isolated or small nests of Leydig cells (Fig. 1d); focal retiform pattern was observed as well. Using immunohistochemistry, the Sertoli cells exhibited inhibin expression (Fig. 1e) and focally cytokeratin staining. Furthermore, omental nodules were composed only of rhabdomyomatous elements.
Fig. 1.
(a) Rhabdomyomatous component (hematoxylin and eosin; magnification 200×). (b) Desmin expression in the rhabdomyomatous component (magnification 200×). (c) Sertoli-Leydig component (hematoxylin and eosin; magnification 100×). (d) Sertoli-Leydig component (hematoxylin and eosin; magnification 200×). (e) Inhibin expression in the Sertoli-Leydig component (magnification 200×).
Adjuvant chemotherapy was performed and there was no clinical evidence of recurrence during the three the threeyears of follow-up.
3. Discussion
SLCTs are extremely rare ovarian tumors. Heterologous elements occur in approximately 20% of SLCTs and are reported in all SLCTs subtypes with the exception of the well-differentiated SLCTs [1]. Heterologous elements include epithelial and/or mesenchymal tissue and tumors arising from these tissues, such as mucinous gastrointestinal epithelium, hepatocytes, skeletal muscle, cartilage, adipose tissue, mucinous carcinoma, carcinoid, rhabdomyosarcoma, and neuroblastoma. The most common heterologous element is mucinous epithelium of enteric type; whereas, others are rare and only 5% of SLCTs contain mesenchymal elements [4].
Our case is peculiar, since rhabdomyomatous differentiation is exceedingly rare. Among previous reports, around 23 cases have been documented, almost as a case report, except the study of Prat et al., reporting nine cases in 1982 [5]. Rhabdomyomatous differentiation has been described in women between 12 and 70 years with a mean age of 21 years. Clinical data are not specific and are the same of poorly differentiated SLCTs, including abdominal mass, virilization, metrorrhagia or amenorrhea; ascites are observed in cases with peritoneal involvement [5].
On macroscopic examination, the tumor is solid and cystic, with a size ranging between sixand 30 cm in diameter and usually exceeding 15 cm. Hemorrhage and necrosis are frequently observed [2,[4], [5], [6], [7], [8], [9], [10]]. Microscopically, rhabdomyomatous differentiation can be isolated or in association with other heterologous elements, most often cartilage and intestinal glands [5]. The rhabdomyosarcomatous component can range from only microscopic in size to 50% of the specimen volume [5]. Although in the majority of cases, these elements were intimately admixed with the Sertoli-Leydig cell component, some reported cases have large areas made up exclusively of immature skeletal muscle, as described in our case [5]. The spindle cell type, pleomorphic and embryonalrhabdomyosarcoma have been reported. The SLTs component can be of intermediate differentiation, poorly differentiated, or retiform [2,[4], [5], [6], [7], [8], [9], [10]]. In some cases, the primary neoplasm did not contain heterologous elements, which were identified only in recurrent tumors [4,10]. In our case, omental nodules were composed only of the heterologous elements.
Most reported cases are at a localized or locally advanced stage in the diagnosis time; however, recurrence with peritoneal involvement is frequent [2,[4], [5], [6], [7], [8], [9], [10]]. The recurrent tumor can be confined to the pelvis, involving the contralateral, or generalized within the abdomen. The recurrent tumor appeared three to 15 months postoperatively. In the 23 documented cases, ten patients died of tumor a few months after surgical treatment [5,6,8,[5], [6], [7], [8], [9], [10]]. However, six patients were alive with recurrent tumor and four patients had no evidence of disease at 11 months to four years after diagnosis.
Little is known about the pathogenesis of ovarian SLCT. Nevertheless, some previous studies reported a 60% prevalence of DICER1 mutations in SLCTs, whatever the degree of differentiation. In cases with rhabdomyomatous differentiation, DICER1 mutation has been found in one case reported by Plastini et al. [6].
Our case was unique since SLCT was occurring on the site of xeroderma pigmentosum. xeroderma pigmentosum is a group of rare autosomal recessive genodermatoses, resulting from gene mutations in the nucleotide excision repair pathway. It is characterized by an extreme sensitivity to sunlight, resulting in sunburn and pigmentary changes in the exposed skin. xeroderma pigmentosum occurs worldwide, with aprevalence estimated at 1/1 000 000 in Europe and USA, and 1/22 000 in Japan. Affected individuals have a more than 10 000 fold elevated risk of skin cancer as well as a 10–20 fold increased risk for other internal malignancies, including leukemia, sarcoma, medulloblastoma, lung, central nervous system, uterine, breast, pancreatic, gastric, renal, and testicular tumors. However, association with ovarian tumor is rare [11].
Susceptibility to ovarian cancer in patient with xeroderma pigmentosum has been studied and the results were controversial. Zhao et al. found that some variant genotypes of xeroderma pigmentosum had a significant association with the increased risk of ovarian cancer, but this susceptibility has not been studied according to the histological type [12]. By reviewing the literature, we found only one case of Sertoli-Leydigcell tumors on the setting of xeroderma pigmentosum. Interestingly, the tumor includes rhabdomyosarcomatous differentiation and the patient wasa young Tunisian girl [8].
In SLCTs with heterologous elements, hysterectomy with bilateral salpingo-oophorectomy and staging, including omentectomy, appendectomy and pelvic lymphadenectomy should be performed. Maximal tumor debulking is recommended for SLCTs with extra-ovarian spread [4]. Adjuvant chemotherapy has been suggested for cases of stage IB to IV, recurrent SLCTs and poorly differentiated SLCTs with heterologous elements. However, the value of adjuvant chemotherapy has not yet been determined. Grove et al. suggested that for moderately differentiated SLCTs with heterologous elements, the percentage of sarcoma and its cellular differentiation should be evaluated to decide whether or not to use adjuvant chemotherapy [4]. The National Comprehensive Cancer Network (NCCN) guidelines recommend adjuvant chemotherapy with a platinum-based regimen such as the association of bleomycin, etoposide and cisplatin, even in an early stage disease when considering poorly differentiated, high-grade, and heterologous tumors. Nonetheless, these recommendations are not based on any large randomized studies due to the rarity of these tumors [7].
4. Conclusion
Ovarian SLCTs with rhabdomyomatous differentiation on the setting of xeroderma pigmentosum is exceptional. Microscopic diagnosis is challenging for pathologist, considering the scarcity of the tumor. Further case reports and retrospective studies are required to further understand the pathogenesis of SLCTs and to determine their optimal treatment regimen.
Declaration of Competing Interest
The authors report no declarations of interest.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
This study is exempt from ethical approval at our institution.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Ahlem Bdioui: Conceptualization, Investigation.
Ahlem Bchir: Writing-Original Draft.
Nabiha Missaoui: Writing, Reviewing and Editing.
Sihem Hmissa: Investigation, Visualization.
Moncef Mokni: Visualization.
Registration of research studies
N/A.
Guarantor
Ahlem Bdioui.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Chen L., Tunnell C.D., De Petris G. Sertoli-Leydig cell tumor with heterologous element: a case report and a review of the literature. Int. J. Clin. Exp. Pathol. 2014;7(3):1176–1181. [PMC free article] [PubMed] [Google Scholar]
- 2.Singh C., Ahmad S., Hajjar F.M. Poorly differentiated, ovarian Sertoli-Leydig cell tumor with heterologous rhabdomyosarcoma and glandular elements: diagnosis and management of a rare neoplasm. Gynecol. Oncol. Rep. 2018;25:70–73. doi: 10.1016/j.gore.2018.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agha R.A., Borrelli M.R., Farwana R. The SCARE 2018 statement: updating consensus Surgical CAseREport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 4.Papler T.B., Grazio S.F., Kobal B. SertoliLeydig cell tumor with retiform areas and overgrowth of rhabdomyosarcomatous elements: case report and literature review. J. Ovarian Res. 2016;9:46. doi: 10.1186/s13048-016-0257-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prat J., Young R., Scully R. Ovarian Sertoli-Leydig cell tumors with heterologous elements: a clinicopathologic analysis of twelve cases. Cancer. 1982;50:2465–2475. doi: 10.1002/1097-0142(19821201)50:11<2465::aid-cncr2820501135>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 6.Plastini T., Staddon A. Sertoli-Leydig cell tumor with concurrent rhabdomyosarcoma: three case reports and a review of the literature. Case Rep. Med. 2017;2017 doi: 10.1155/2017/4587296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brightwell R., Grzankowski K., Kasznica J. Poorly differentiated Sertoli-Leydig tumor with heterologous, high-grade, sarcomatoid features: a case report. Gynecol. Oncol. Rep. 2015;14:6–8. doi: 10.1016/j.gore.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bacha D., Ben Amor A., Sassi A. Sex cord-stromal tumour with rhadomyosarcomatous contingent heterologous in A 7-year-old girl treated for xeroderma pigmentosum. Int. J. Gynecol. Cancer. 2019;29:A120. [Google Scholar]
- 9.Rekhi B., Karpate A., Deodhar K.K. Metastatic rhabdomyosarcomatous elements, mimicking a primary sarcoma, in the omentum, from a poorly differentiated ovarian Sertoli-Leydig cell tumor in a young girl: an unusual presentation with a literature review. Indian J. Pathol. Microbiol. 2009;52:554–558. doi: 10.4103/0377-4929.56165. [DOI] [PubMed] [Google Scholar]
- 10.Zaloudek C., Norris H.J. Sertoli-Leydig tumors of the ovary. A clinicopathologic study of 64 intermediate and poorly differentiated neoplasms. Am. J. Surg. Pathol. 1984;8(6):405–418. doi: 10.1097/00000478-198406000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Lichon V., Khachemoune A. Xeroderma pigmentosum: beyond skin cancer. J. Drugs Dermatol. 2007;6(3):281–288. [PubMed] [Google Scholar]
- 12.Zhao Z., Zhang A., Zhao Y. The association of polymorphisms in nucleotide excision repair genes with ovarian cancer susceptibility. Biosci. Rep. 2018;38(3) doi: 10.1042/BSR20180114. [DOI] [PMC free article] [PubMed] [Google Scholar]