ABSTRACT
The present report describes the process and results obtained with a knowledge translation project developed in three stages to identify barriers to the Implementation of the National Guidelines for Normal Childbirth in Brazil, as well strategies for effective implementation. The Improving Programme Implementation through Embedded Research (iPIER) model and the Supporting Policy Relevant Reviews and Trials (SUPPORT) tools provided the methodological framework for the project. In the first stage, the quality of the Guidelines was evaluated and the barriers preventing implementation of the recommendations were identified through review of the global evidence and analysis of contributions obtained in a public consultation process. In the second stage, an evidence synthesis was used as the basis for a deliberative dialogue aimed at prioritizing the barriers identified. Finally, a second evidence synthesis was presented in a new deliberative dialogue to discuss six options to address the prioritized barriers: 1) promote the use of multifaceted interventions; 2) promote educational interventions for the adoption of guidelines; 3) perform audits and provide feedback to adjust professional practice; 4) use reminders to mediate the interaction between workers and service users; 5) enable patient-mediated interventions; and 6) engage opinion leaders to promote use of the Guidelines. The processes and results associated with each stage were documented and formulated to inform a review and update of the Guidelines and the development of an implementation plan for the recommendations. Effective implementation of the Guidelines is important for improving the care provided during labor and childbirth in Brazil.
Keywords: Evidence-informed policy, implementation science, Evidence-based practice, practice guideline, natural childbirth, Brazil
RESUMEN
En este informe se presentan los procesos y resultados de un proyecto de traducción de conocimiento desarrollado en tres etapas para identificar los obstáculos y las estrategias para la aplicación efectiva de las Directrices Nacionales para el Parto Normal en el Brasil. El marco metodológico adoptado comprendió la iniciativa iPIER (Improving Program Implementation through Embedded Research) y las herramientas SUPPORT para políticas basadas en evidencia. En la primera etapa se evaluó la calidad de las Directrices y se identificaron los obstáculos a la aplicación de las recomendaciones, teniendo en cuenta la evidencia mundial y el análisis de las contribuciones obtenidas mediante una consulta pública. En la segunda etapa, una síntesis de la evidencia sirvió de base para un diálogo deliberativo para la priorización de los obstáculos. Por último, una nueva síntesis de la evidencia sirvió de base para un segundo diálogo deliberativo y presentó seis opciones para hacer frente a los obstáculos priorizados: 1) fomentar el uso de estrategias de intervención polifacéticas; 2) promover intervenciones educativas para mejorar el uso de directrices sanitarias; 3) realizar auditorías y proporcionar retroalimentación para la adecuación de la práctica profesional; 4) utilizar recordatorios para mediar en la interacción entre profesionales y usuarios; 5) permitir intervenciones mediadas por el paciente; y 6) incluir a líderes de opinión para fomentar el uso de directrices sanitarias. Se documentaron y presentaron los procesos y resultados de cada etapa del proyecto para fundamentar la actualización de las Directrices y la elaboración de un plan de aplicación de las recomendaciones. La aplicación efectiva de las Directrices es importante para mejorar la atención del parto y el nacimiento en el Brasil.
Palabras clave: Política informada por la evidencia, ciencia de la implementación, práctica clínica basada en la evidencia, guía de práctica clínica, parto normal, Brasil
In 2018, under a joint initiative of the Pan American Health Organization, the Alliance for Health Policy and Systems Research (AHPSR), and the Special Program for Research and Training in Tropical Diseases (TDR), a call for proposals was issued on Embedding Research for the Sustainable Development Goals (ER-SDG) (1). ER-SDG uses the successful model known as Improving Programme Implementation through Embedded Research (iPIER), which supports the integration of research into the implementation of health programs and policies. Part of this process involves identifying barriers and facilitators and embedding these findings into the formulation and/or improvement of public health policies and practices (2).
Taking into account the terms of the ER-SDG call for proposals, the objective of the project Implementation of the National Guidelines for Normal Childbirth in Brazil: Barriers and Strategies, was to identify the barriers and strategies for implementing the Guidelines through the application of knowledge translation processes and tools. The Guidelines constitute 225 recommendations for providing care to the parturient and the newborn in eight different areas: 1) the facility where the care is provided; 2) general care during labor; 3) pain relief during labor; 4) care during the first stage of labor; 5) care during the second stage of labor; 6) care during the third stage of labor; 7) immediate postpartum maternal care; and 8) care of the newborn.
Despite the Guidelines’ recognized potential to improve the organization of services and health outcomes, they are still underutilized (4–6). Typically, their application is unplanned, and when they are invoked, they are not applied effectively (7). In the case of delivery care in Brazil, despite the progress made in recent decades, the obstetric model is still strongly medicalized and characterized by unnecessary and potentially iatrogenic practices such as elective C-sections and frequently reported cases of obstetric violence (8, 9). These circumstances make implementation of the recommendations even more challenging.
The aim of this report is to describe the processes and outcomes of the project Implementation of the National Guidelines for Normal Childbirth in Brazil: Barriers and Strategies, with emphasis on the methods adopted and their outcomes. It is hoped that it will contribute to the improvement of delivery care in Brazil and also encourage the use of knowledge translation tools.
STAGES OF PROJECT DEVELOPMENT AND OUTCOMES
The project was carried out between December 2018 and November 2019 by the Oswaldo Cruz Foundation (Fiocruz Brasilia), working in collaboration with the Ministry of Health (Women’s Health Coordination), the University of Brasilia (Department of Collective Health) and the Health Institute of the São Paulo State Department of Health (Health Evidence Nucleus), with the approval of the ethics committees of Fiocruz Brasilia (CAAE 01857418.1.0000.8027) and the Pan American Health Organization (PAHO-ERC). The participants in the deliberative dialogues gave their informed consent and steps were taken to ensure the anonymity from the data collected.
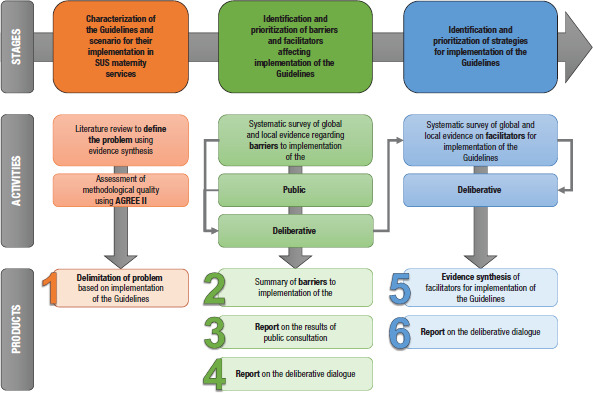
Development of the project followed an existing three-stage protocol (Supplementary Material, page 1) with focus on the following specific objectives: 1) characterization of the Guidelines for Normal Childbirth and their role in the provision of maternity services by the Unified Health System (SUS); 2) identification and prioritization of barriers and facilitators affecting their implementation; and 3) identification and prioritization of strategies for their implementation. Figure 1 summarizes the stages of the project.
FIGURE 1. Flowchart showing stages, activities, and outcomes of the project “Implementation of the National Guidelines for Normal Childbirth in Brazil”.
Stage 1: Characterization of the Guidelines for Normal Childbirth and scenario for their implementation in SUS maternity facilities
A literature review was conducted between October 2018 and March 2019 to characterize the process of preparing the Guidelines and scenarios for their implementation. The findings provided the basis for the project’s protocol (Supplementary Material, page 1). In addition, an assessment of the methodological quality of the Guidelines was performed using the AGREE II tool (10). The findings were compared against the weighting parameters proposed by AGREE II (Supplementary Material, page 10).
The exercise identified two weaknesses in the Guidelines. First, some of the actors involved are underrepresented, especially in the professional and user categories, even though the process of developing the Guidelines had been participatory. Also, the lack of a plan for implementing and monitoring the process affected the applicability of the assessment. The evaluators recommended that the Guidelines be updated with methodological adjustments and the inclusion of an implementation plan.
Stage 2: Identification and prioritization of implementation barriers and facilitators
The mapping of potential barriers to implementation was carried out from March through June 2019. It involved three activities: 1) development of a synthesis of secondary global and local evidence; 2) textual analysis of the contributions obtained from the public consultation; and 3) engagement in a deliberative dialogue to prioritize the barriers to implementation.
The synthesis of evidence on barriers to implementation of the Guidelines in clinical practice was based on the pro- and post-stages, using SUPporting POlicy-relevant Reviews and Trials (SUPPORT) tools for evidence-informed policies (11) as they relate to the implementation deficiencies addressed in Stage 1. The searches were conducted in March and April 2019 using the following electronic databases: PubMed, LILACS, BDENF, Health Systems Evidence, Health Evidence, and Epistemonikos) in March and April 2019. Structured strategies (Supplementary Material, page 19) were used to identify secondary studies (systematic reviews and qualitative syntheses) and clinical guidelines published in English, Portuguese, or Spanish on the subject of barriers to implementation. In all, 23 texts (21 articles and two sets of clinical guidelines) were accepted for inclusion in the synthesis. Data on barriers to implementation were extracted from these sources and stratified by level of organization within the health system (users, personnel, health services, and overall health systems). Only the systematic reviews were assessed for methodological quality, using the Assessing Methodological Quality of Systematic Reviews (AMSTAR) instrument (12).
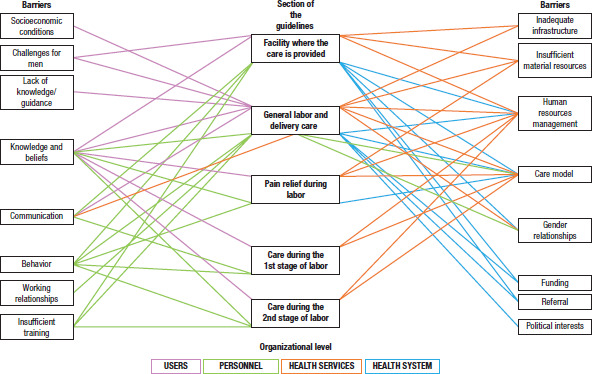
In the synthesis of the findings, the barriers were first organized according to the eight sections of the Guidelines and by organizational level. Then, within each level, they were then grouped into similar thematic categories. Finally, the categories were subdivided into cores of meaning. The results were summarized in a document (Supplementary Material, page 12) designed to serve as the basis for a deliberative dialogue on the prioritization of barriers.
The barriers identified corresponded to 25 of the 225 recommendations in the Guidelines for Normal Childbirth (Figure 2). The evidence synthesis of the barriers to implementation of the Guidelines (13) is presented in another article on the ER-SDG initiative in this special edition.
FIGURE 2. Relationships between the barriers to implementation presented in the global evidence synthesis and the National Guidelines for Normal Childbirth.
The identification of barriers to implementation was supplemented with an analysis of the textual data from the Public Consultation on National Guidelines for Normal Childbirth Care conducted by the Ministry of Health in 2016. The National Commission on the Incorporation of Technologies into the SUS (CONITEC) includes public consultation as an essential part of the process of incorporating technologies, clinical protocols, and treatment guidelines. A total of 396 individual contributions were received from individuals and institutions in several states in Brazil. A statistical analysis of the textual corpus derived from the public consultation was performed using IRAMUTEQ software (14).
In the analysis of the individual contributions, 93 records were excluded because they were limited to “yes” or “no” responses. The included contributions were combined into a single corpus and submitted to descending hierarchical classification (DHC) analysis (14). Two subcorpora were then extracted from this initial analysis: one with words related to barriers to implementing the Guidelines, and the other to facilitators. A new DHC analysis was then performed on these subcorpora to extract representative strings corresponding to the main barriers and facilitators identified. A schematic representation of this analysis of the public consultation is shown in Figure 3. A detailed report can be found in the Supplementary Material (page 69).
FIGURE 3. Main barriers to implementation of the National Guidelines for Normal Childbirth identified in the analysis of the public consultation corpus.

To prioritize the barriers identified through the evidence synthesis and the analysis of the contributions from the public consultation, a deliberative dialogue was held with nine participants, including managers from the Women’s Health Coordination in the Ministry of Health and researchers on topics related to the subject of the dialogue. The organization and conduct of the dialogue followed the structure of the SUPPORT tools (15). The participants had previously received two reports on barriers to implementation. The deliberative dialogue adopted the Chatham House rule, which allows participants to comment openly on the discussions held in the meeting as long as the identity of the authors of the statements is not revealed.
Presentation of the key messages was followed by a structured discussion. Three barriers to implementation were considered to have the highest priority: 1) the physician-centered care model, which hinders the participation of the parturient and other professionals in attending the delivery; 2) the professional education model, which perpetuates practices not backed by scientific evidence and emphasizes a biomedical perspective at the expense of the humane aspects of care and hampers the adoption of new evidence-based care practices; and 3) a health services infrastructure that is insufficient and inappropriate to support the implementation of better care strategies. The deliberations were compiled in a summary report (Supplementary Material, page 75).
Stage 3: Identification and prioritization of implementation strategies
Stage 3 was carried out from July through October 2019. Based on the results of the deliberative dialogue, a new evidence synthesis looked at options for supporting implementation of the Guidelines, bearing in mind the prioritized implementation barriers. The options were identified through systematic searches conducted in July 2019 using six databases (Scopus, PubMed, VHL-LILACS, Epistemonikos, Health Systems Evidence, and Health Evidence) (Supplementary Material, page 79) to identify systematic reviews published in English, Portuguese, or Spanish on strategies for implementing clinical guidelines in health services and/or systems. The selection was made using the Rayyan QCRI platform (16) and the methodological quality of the included reviews was assessed using the AMSTAR instrument (12).
The search yielded 3,830 documents, 3,780 of which were excluded because they were duplicates (585) or because they failed to meet the inclusion criteria (3,195). The remaining 50 articles were selected for complete reading, and 29 of them ended up being included. The data were extracted and categorized according to the Cochrane Effective Practice and Organization of Care Group (EPOC) taxonomy for health system interventions (17). The resulting evidence synthesis produced six options, which provided the basis for a second deliberative dialogue, aimed at contributing to the formulation of a plan for implementation of the Guidelines.
It is important to emphasize that not all the options identified presented the same level of confidence in terms of their effectiveness, nor were they conditioned by the same factors that affect implementation. Furthermore, the options ranged from isolated actions to multi-faceted interventions, thus requiring an analysis of their potential benefits, risks, and uncertainties. The options were organized according to the methodological quality of the reviews in which they were cited. The following paragraphs summarize the six options. The full version of the evidence synthesis is available in the Supplementary Material (page 79).
Option 1: Encouraging the use of multi-faceted intervention strategies, which entails a combination of two or more interventions. Of the 19 systematic reviews included in this option (18–36), five were deemed to be of high methodological quality, nine of average quality, and five of poor quality. The studies looked at a broad range of combinations of interventions, including educational meetings conducted by opinion leaders and educational sensitization visits (18), distribution of materials by mail, and follow-up telephone calls or subsequent checkups (19). The effectiveness of multi-faceted interventions in the field of the obstetrics depends on the nature of the strategies used. The results will differ depending on the desired behavior, the allocation unit, and the particular service providers (20). Thus, the selection of interventions to make up a multi-faceted strategy will determine the effectiveness of this option.
Option 2: Promoting educational interventions to encourage the use of health guidelines. This option was examined in 18 systematic reviews (19–21, 23-27, 29, 34, 37–39), five of which were of high methodological quality, eight of average quality, and five of poor quality. The interventions were grouped into three categories: educational materials (19, 21, 26, 34, 37), educational meetings (19, 23, 25–27, 29, 37), and educational outreach visits, or academic detailing (19, 20, 24, 26, 34–39). The interventions based on the use of educational materials refer to the distribution of information to individuals or groups to support clinical care—in other words, any intervention in which knowledge is distributed. Educational meetings are defined as courses, workshops, conferences, or other educational meetings. Educational outreach visits or academic detailing refer to visits by trained professionals to health workers in their own settings to provide information with the aim of changing practice (17).
Option 3: Using audit and feedback to improve professional practice—in other words, provide feedback to professionals on their performance and encourage them meet reference standards (40). According to 10 systematic reviews (19, 20, 24, 26, 34, 36, 37, 40–42), one of them of high methodological quality, five of average quality, and four of poor quality, audit and feedback interventions are commonly used in health services to improve the performance of professionals. A synthesis of professional performance over a given time period can be presented in various formats (40) — verbally, on paper, or via electric media—and it can include specific suggestions for improving clinical practice (43). This option includes, in particular, increased acceptance by nurses in obstetric practice than in other clinical contexts (20).
Option 4: Using reminders to mediate interaction between health professionals and users. This option was studied in 10 systematic reviews (14, 19, 20, 22, 26, 35-37, 44, 45), one of which was of high methodological quality, five of average quality, and four of poor quality. This option involves the use of reminders, which are widely utilized in decision-making support systems for health professionals to jog or aid their memory (44). Reminders are defined as actions to mediate the behavior of health professionals during their interactions with users (17). These interventions can help health professionals avoid problems like oversights, information overload, or lack of online access. Reminders can enable professionals to retrieve information they already know or would be expected to know and provide pertinent guidelines in accessible format at appropriate times (44). The structure of the reminders can vary in content (e.g., suggested tests or literature references), format (printed, electronic, computer-generated and delivered on paper, etc.) and organization. They can also be shared with other professionals on-screen, via e-mail, or by entering them in the patient record (44, 45).
Option 5: Facilitating viable patient-mediated interventions. This option was covered in five systematic reviews (19, 24, 30, 37, 38), one of which was of high methodological quality, three of average quality, and one of poor quality. It refers to any intervention designed to alter the performance of health professionals through interactions with the patient or actions that involve conveying information to the patient or receiving it from her (43). Examples might be: the patient communicating information about her health to the health professional; the patient receiving information about her health (for example, with regard to recommended care); patient education (for example, regarding her condition and options for her care); and interactions to support her in making decisions, including information regarding treatment options and the respective risks and benefits (27).
Option 6: Involving opinion leaders in promoting the use of health guidelines. This option was addressed in five systematic reviews (19, 20, 26, 37, 46), three of which were of average methodological quality and two of poor quality. Local opinion leaders are health care providers or specialists in a particular area who offer ongoing support regarding the use of guidelines and better evidence-based practices (37). This type of strategy is based on the assumption that it is possible to generate change through interaction with (and the influence of) people recognized for their expertise (20). The identification of local opinion leaders and the definition of measures they are able to take can promote good clinical practice (17). These leaders may include, for example, clinicians known by their colleagues to be respected professionals who are effective in communicating information (20), recognized health professionals in the community (19), or even experts in particular areas who are able to provide ongoing support to other professionals, helping them to improve their practice based on scientific evidence (37).
Deliberative dialogue on implementation strategies
The evidence synthesis on implementation strategies provided the basis for a second deliberative dialogue, which followed the structure of the SUPPORT tools (15). There were 15 participants, strategically selected to represent the groups and personnel levels of interest, including managers, researchers, health professionals, and user representatives. The dialogue promoted mediated interaction in discussions on the importance of combining interventions to achieve better outcomes in implementation of the guidelines and stepping up this debate in educational contexts for the development of health professionals. There was also emphasis on the need to strengthen the active participation of women and their companions, both in policy-making and when the time comes to make childbirth decisions of their own.
The participants emphasized the importance of regularly updating the Guidelines, involving women and the representation of other interested social stakeholders, and ensuring the systematic use of quality scientific evidence. However, it was also understood that effective utilization of the Guidelines in the health services and in the individual practice of health personnel will depend on local managers being open to shifting to the new care model. In addition, it was suggested to provide more clarity regarding the specific target audience for the recommendations in the proposed guidelines (users, professionals, and/or managers) and to consider producing versions in more accessible language for different audiences—for example, for the women receiving care in the health services.
To achieve these objectives, the participants proposed that specific, soundly based strategies be incorporated in a plan for implementation of the Guidelines in order to help ensure consistent application of the recommendations by professionals in the health services. The report of the second deliberative dialogue may be found in the Supplementary Material (page 111).
DISCUSSION
The objective of the ER-SDG call for proposals was to embed research results in the implementation of health programs and policies (1). As a part of this initiative, the project reported in this article adopted the paradigm of integrated knowledge translation (47) and generated processes and outputs to support the systematic and transparent use of scientific knowledge in decision-making—specifically, evidence synthesis and deliberative dialogue, which are recognized to be effective tools for knowledge translation (48-50).
The project addressed the challenges of implementation, including the weak points in the process of preparing the guidelines, as well as the barriers at different levels, ranging from the individual to the systemic. In light of these challenges, it is essential that the strategies for attacking the problems addressed in this report be based on scientific evidence that informs an effective implementation plan.
The two evidence syntheses are notable outcomes of the knowledge translation process, offering an accessible and systematic presentation of information on implementation barriers and strategies to be considered by decision-makers.
The deliberative dialogues also showed that it was possible to add valuable information on the perspectives, experiences, and opinions of the directly interested players in addressing the problem, confirming the value of its use as a tool for integrating scientific (global) and colloquial (local) evidence (47).
Some limitations on the documents presented in this report need to be noted. The first evidence synthesis identified barriers to implementation of only 25 of the 225 recommendations contained in the proposed guidelines. This large gap may be attributed to using only secondary studies. Although the selection methodology was adequate for development of the project, it is possible that important information may not have been considered. Already in the synthesis of options for supporting implementation of the guidelines, the scarcity of systematic reviews of interventions in the area of obstetric guidelines was evident. For this reason, it was decided to use indirect evidence on the implementation of guidelines in general. This limitation should be taken into account in judging the applicability of the results described, especially the policy options, in the context of the Brazilian health system.
Also, the time frame for completing the project prevented further development of the processes and outcomes. Despite this limitation, the research protocol was fully implemented. It should be recognized that the decision-making process is typically fraught with non-material limitations—not only in terms of time, but also in logistic and cognitive resources (51). Finally, it is recommended the Guidelines be updated to include a plan for their implementation that prioritizes the participation of women in the process and clearly defines the target audience for each recommendation: users, health professionals, or managers of health services or the overall health system. Effective implementation of the Guidelines will require changes aimed at improving the current childbirth care model in the SUS. It will also be necessary to strengthen other current strategies in Brazil in order to promote an understanding of the physiology of childbirth, incorporate safe, evidence-based practices, and guarantee sexual and reproductive rights.
Funding.
This study was funded by the Pan American Health Organization (PAHO/WHO), the Alliance for Research in Policies and Health Systems (AHPSR), and the Special Program for Research and Training in Tropical Diseases (TDR) through a donation to the project “Barriers and Strategies for Implementation of the National Guidelines for Normal Childbirth in Brazil [Call for Proposals on Embedding Research for the Sustainable Development Goals (ER-SDG)].” The funding agencies did not have any role in the project design, analysis process, interpretation of the data, or drafting of the manuscript.
Disclaimer.
Authors hold sole responsibility for the views expressed in the manuscript, which may not necessarily reflect the opinion or policy of the RPSP/PAJPH or the Pan American Health Organization (PAHO).
Footnotes
Authors’ contributions.
JOMB, EC, and MAN conceived the project and coordinated its execution. MCB, CDLJ, CFO, TST, AAVR, TRT, DR., AV, YM, and VC were involved in different stages of the project’s execution and the development of the results presented. JOMB wrote the initial version of the manuscript. All the authors contributed to, reviewed, and approved the final version of the manuscript.
Acknowledgments.
We wish to express our gratitude to the colleagues who collaborated on the AGREE II assessment of the National Guidelines for Normal Childbirth in Brazil: Airton Stein (Porto Alegre Federal Health Sciences University) and Daniel Melo (Federal University of São Paulo). We would also like to thank Monica Neri and Gisele Bortolini for providing the project with indispensable institutional support while they were responsible for the Women’s Health Coordination in the Ministry of Health.
Conflicts of interest.
None declared by the authors.
References
- 1.Pan AmericanHealth Organization - PAHO . 2018. [Accessed 17 May 2020]. Convocatoria: Incorporación de la investigación para avanzar en el cumplimiento de los Objetivos de Desarrollo Sostenible (ER-SDG) Available at: www.paho.org/hq/index.php?option=com_content&view=article&id=12040:call-for-applications-embedding-research-for-the-sustainable-development-goals&Itemid=41749&lang=pt. [Google Scholar]; 1. Pan AmericanHealth Organization - PAHO. Convocatoria: Incorporación de la investigación para avanzar en el cumplimiento de los Objetivos de Desarrollo Sostenible (ER-SDG). 2018. Available at: www.paho.org/hq/index.php?option=com_content&view=article&id=12040:call-for-applications-embedding-research-for-the-sustainable-development-goals&Itemid=41749&lang=pt Accessed 17 May 2020.
- 2.Langlois E V, Mancuso A, Elias V, Reveiz L. Embedding implementation research to enhance health policy and systems: a multi-country analysis from ten settings in Latin America and the Caribbean. Health Res Policy Sys. 2019;17:85. doi: 10.1186/s12961-019-0484-4. [DOI] [PMC free article] [PubMed] [Google Scholar]; 2. Langlois E V, Mancuso A, Elias V, Reveiz L. Embedding implementation research to enhance health policy and systems: a multi-country analysis from ten settings in Latin America and the Caribbean. Health Res Policy Sys. 2019;17:85. 10.1186/s12961-019-0484-4 [DOI] [PMC free article] [PubMed]
- 3.Brasil . Diretrizes nacionais de assistência ao parto normal: versão resumida. Brasília: Ministério da Saúde; 2017. [Acessado em 2 de junho de 2020]. Ministério da Saúde. Available at: pesquisa.bvsalud.org/bvsms/resource/pt/mis-39026. [Google Scholar]; 3. Brasil. Ministério da Saúde. Diretrizes nacionais de assistência ao parto normal: versão resumida. Brasília: Ministério da Saúde; 2017. Available at: pesquisa.bvsalud.org/bvsms/resource/pt/mis-39026 Acessado em 2 de junho de 2020.
- 4.FitzGerald JM, Boulet L-P, McIvor RA, Zimmerman S, Chapman KR. Asthma Control in Canada Remains Suboptimal: The Reality of Asthma Control (TRAC) Study. Can Respir J. 2006;13(5):253–259. doi: 10.1155/2006/753083. [DOI] [PMC free article] [PubMed] [Google Scholar]; 4. FitzGerald JM, Boulet L-P, McIvor RA, Zimmerman S, Chapman KR. Asthma Control in Canada Remains Suboptimal: The Reality of Asthma Control (TRAC) Study. Can Respir J. 2006;13(5):253–9. 10.1155/2006/753083 [DOI] [PMC free article] [PubMed]
- 5.Brown LC, Johnson JA, Majumdar SR, Tsuyuki RT, McAlister FA. Evidence of suboptimal management of cardiovascular risk in patients with type 2 diabetes mellitus and symptomatic atherosclerosis. CMAJ. 2004;171(10):1189–1192. doi: 10.1503/cmaj.1031965. [DOI] [PMC free article] [PubMed] [Google Scholar]; 5. Brown LC, Johnson JA, Majumdar SR, Tsuyuki RT, McAlister FA. Evidence of suboptimal management of cardiovascular risk in patients with type 2 diabetes mellitus and symptomatic atherosclerosis. CMAJ. 2004;171(10):1189–92. 10.1503/cmaj.1031965 [DOI] [PMC free article] [PubMed]
- 6.Latosinsky S, Fradette K, Lix L, Hildebrand K, Turner D. Canadian breast cancer guidelines: have they made a difference? CMAJ. 2007;176(6):771–776. doi: 10.1503/cmaj.060854. [DOI] [PMC free article] [PubMed] [Google Scholar]; 6. Latosinsky S, Fradette K, Lix L, Hildebrand K, Turner D. Canadian breast cancer guidelines: have they made a difference? CMAJ. 2007;176(6):771–6. 10.1503/cmaj.060854 [DOI] [PMC free article] [PubMed]
- 7.Gagliardi AR, Brouwers MC, Palda VA, Lemieux-Charles L, Grimshaw JM. How can we improve guideline use? A conceptual framework of implementability. Implementation Sci. 2011;6(1):26. doi: 10.1186/1748-5908-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]; 7. Gagliardi AR, Brouwers MC, Palda VA, Lemieux-Charles L, Grimshaw JM. How can we improve guideline use? A conceptual framework of implementability. Implementation Sci. 2011;6(1):26. 10.1186/1748-5908-6-26 [DOI] [PMC free article] [PubMed]
- 8.World Health Organization (WHO) Genebra: World Health Organization (WHO); 2007. Maternal mortality in 2005: estimates developed by WHO, UNICEF, UNFPA, and the World Bank. [Google Scholar]; 8. World Health Organization (WHO). Maternal mortality in 2005: estimates developed by WHO, UNICEF, UNFPA, and the World Bank. Genebra: World Health Organization (WHO); 2007.
- 9.Fundação Perseu Abramo . São Paulo, SP. 2010. [Acessado em 10 de junho de 2020]. Mulheres brasileiras e gênero nos espaços público e privado. Available at: https://fpabramo.org.br/publicacoes/wp-content/uploads/ [Google Scholar]; 9. Fundação Perseu Abramo. Mulheres brasileiras e gênero nos espaços público e privado. São Paulo, SP; 2010. Available at: https://fpabramo.org.br/publicacoes/wp-content/uploads/ Acessado em 10 de junho de 2020.
- 10.Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010;182(18):E839–E842. doi: 10.1503/cmaj.090449. [DOI] [PMC free article] [PubMed] [Google Scholar]; 10. Brouwers MC, Kho ME, Browman GP, Burgers JS, Cluzeau F, Feder G, et al. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010;182(18):E839–42. 10.1503/cmaj.090449 [DOI] [PMC free article] [PubMed]
- 11.Lavis JN, Oxman AD, Lewin S, Fretheim A. SUPPORT Tools for evidence-informed health Policymaking (STP) Health Res Policy Sys. 2009;7(S1):I1. doi: 10.1186/1478-4505-7-S1-I1. [DOI] [PMC free article] [PubMed] [Google Scholar]; 11. Lavis JN, Oxman AD, Lewin S, Fretheim A. SUPPORT Tools for evidence-informed health Policymaking (STP). Health Res Policy Sys. 2009;7(S1):I1. 10.1186/1478-4505-7-S1-I1 [DOI] [PMC free article] [PubMed]
- 12.Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7(1):10. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]; 12. Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7(1):10. 10.1186/1471-2288-7-10 [DOI] [PMC free article] [PubMed]
- 13.Oliveira CF, Ribeiro AAV, Luquine Jr CD, de Bortoli MC, Toma TS, Chapman EMG, et al. Barreiras à implementação de recomendações para assistência ao parto normal: revisão rápida de evidências. Rev Panam Salud Publica. 2020;44:e132. doi: 10.26633/RPSP.2020.132. [DOI] [PMC free article] [PubMed] [Google Scholar]; 13.Oliveira CF, Ribeiro AAV, Luquine Jr CD, de Bortoli MC, Toma TS, Chapman EMG, et al. Barreiras à implementação de recomendações para assistência ao parto normal: revisão rápida de evidências. Rev Panam Salud Publica. 2020;44:e132. 10.26633/RPSP.2020.132 [DOI] [PMC free article] [PubMed]
- 14.Camargo BV, Justo AM. IRAMUTEQ: Um software gratuito para análise de dados textuais. Temas Psicol. 2013;21(2):513–518. doi: 10.9788/TP2013.2-16. [DOI] [Google Scholar]; 14. Camargo BV, Justo AM. IRAMUTEQ: Um software gratuito para análise de dados textuais. Temas Psicol. 2013;21(2):513–8. 10.9788/TP2013.2-16 [DOI]
- 15.Lavis JN, Boyko JA, Oxman AD, Lewin S, Fretheim A. SUPPORT Tools for evidence-informed health Policymaking (STP) 14: Organising and using policy dialogues to support evidence-informed policymaking. Health Res Policy Sys. 2009;7S1:S14. doi: 10.1186/1478-4505-7-S1-S14. [DOI] [PMC free article] [PubMed] [Google Scholar]; 15. Lavis JN, Boyko JA, Oxman AD, Lewin S, Fretheim A. SUPPORT Tools for evidence-informed health Policymaking (STP) 14: Organising and using policy dialogues to support evidence-informed policymaking. Health Res Policy Sys. 2009;7(S1):S14. 10.1186/1478-4505-7-S1-S14 [DOI] [PMC free article] [PubMed]
- 16.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]; 16. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed]
- 17.Effective Practice and Organisation of Care (EPOC) EPOC Taxonomy. 2015. [Acessado em 4 de junho de 2020]. Available at: epoc.cochrane.org/epoc-taxonomy. [Google Scholar]; 17. Effective Practice and Organisation of Care (EPOC). EPOC Taxonomy. 2015. Available at: epoc.cochrane.org/epoc-taxonomy Acessado em 4 de junho de 2020.
- 18.van der Wees PJ, Jamtvedt G, Rebbeck T, de Bie RA, Dekker J, Hendriks EJM. Multifaceted strategies may increase implementation of physiotherapy clinical guidelines: a systematic review. Aust J Physiother. 2008;54(4):233–241. doi: 10.1016/S0004-9514(08)70002-3. [DOI] [PubMed] [Google Scholar]; 18. van der Wees PJ, Jamtvedt G, Rebbeck T, de Bie RA, Dekker J, Hendriks EJM. Multifaceted strategies may increase implementation of physiotherapy clinical guidelines: a systematic review. Aust J Physiother. 2008;54(4):233–41. 10.1016/S0004-9514(08)70002-3 [DOI] [PubMed]
- 19.Davis DA, Taylor-Vaisey A. Translating guidelines into practice: a systematic review of theoretic concepts, practical experience and research evidence in the adoption of clinical practice guidelines. CMAJ. 1997;157(4):408–416. [PMC free article] [PubMed] [Google Scholar]; 19. Davis DA, Taylor-Vaisey A. Translating guidelines into practice: a systematic review of theoretic concepts, practical experience and research evidence in the adoption of clinical practice guidelines. CMAJ. 1997;157(4):408–16. [PMC free article] [PubMed]
- 20.Chaillet N, Dubé E, Dugas M, Audibert F, Tourigny C, Fraser WD, et al. Evidence-based strategies for implementing guidelines in obstetrics: a systematic review. Obstet Gynecol. 2006;108(5):1234–1245. doi: 10.1097/01.AOG.0000236434.74160.8b. [DOI] [PubMed] [Google Scholar]; 20. Chaillet N, Dubé E, Dugas M, Audibert F, Tourigny C, Fraser WD, et al. Evidence-based strategies for implementing guidelines in obstetrics: a systematic review. Obstet Gynecol. 2006;108(5):1234–45. 10.1097/01.AOG.0000236434.74160.8b [DOI] [PubMed]
- 21.Ament SMC, de Groot JJA, Maessen JMC, Dirksen CD, van der Weijden T, Kleijnen J. Sustainability of professionals’ adherence to clinical practice guidelines in medical care: a systematic review. BMJ Open. 2015;5(12):e008073. doi: 10.1136/bmjopen-2015-008073. [DOI] [PMC free article] [PubMed] [Google Scholar]; 21. Ament SMC, de Groot JJA, Maessen JMC, Dirksen CD, van der Weijden T, Kleijnen J. Sustainability of professionals’ adherence to clinical practice guidelines in medical care: a systematic review. BMJ Open. 2015;5(12):e008073. 10.1136/bmjopen-2015-008073 [DOI] [PMC free article] [PubMed]
- 22.Grimshaw J, Eccles M, Thomas R, MacLennan G, Ramsay C, Fraser C, et al. Toward evidence-based quality improvement: evidence (and its limitations) on the effectiveness of guideline dissemination and implementation strategies 1966-1998. J Gen Intern Med. 2006;21(S2):S14–S20. doi: 10.1111/j.1525-1497.2006.00357.x. [DOI] [PMC free article] [PubMed] [Google Scholar]; 22. Grimshaw J, Eccles M, Thomas R, MacLennan G, Ramsay C, Fraser C, et al. Toward evidence-based quality improvement: evidence (and its limitations) on the effectiveness of guideline dissemination and implementation strategies 1966-1998. J Gen Intern Med. 2006;21(S2):S14–20. 10.1111/j.1525-1497.2006.00357.x [DOI] [PMC free article] [PubMed]
- 23.Flodgren G, Hall AM, Goulding L, Eccles MP, Grimshaw JM, Leng GC, et al. Cochrane Database Syst Rev. 8. 2016. Tools2 developed and disseminated by guideline producers to promote the uptake of their guidelines. [DOI] [PMC free article] [PubMed] [Google Scholar]; 23. Flodgren G, Hall AM, Goulding L, Eccles MP, Grimshaw JM, Leng GC, et al. Tools2 developed and disseminated by guideline producers to promote the uptake of their guidelines. Cochrane Database Syst Rev. 2016;(8). 10.1002/14651858.CD010669.pub2 [DOI] [PMC free article] [PubMed]
- 24.Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004;8(6) doi: 10.3310/hta8060. [DOI] [PubMed] [Google Scholar]; 24. Grimshaw JM, Thomas RE, MacLennan G, Fraser C, Ramsay CR, Vale L, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004;8(6). 10.3310/hta8060 [DOI] [PubMed]
- 25.Imamura M, Kanguru L, Penfold S, Stokes T, Camosso-Stefinovic J, Shaw B, et al. A systematic review of implementation strategies to deliver guidelines on obstetric care practice in low- and middle-income countries. Int J Gynecol Obstet. 2017;136(1):19–28. doi: 10.1002/ijgo.12005. [DOI] [PubMed] [Google Scholar]; 25. Imamura M, Kanguru L, Penfold S, Stokes T, Camosso-Stefinovic J, Shaw B, et al. A systematic review of implementation strategies to deliver guidelines on obstetric care practice in low- and middle-income countries. Int J Gynecol Obstet. 2017;136(1):19–28. 10.1002/ijgo.12005 [DOI] [PubMed]
- 26.Dijkstra R, Wensing M, Thomas R, Akkermans R, Braspenning J, Grimshaw JM, et al. The relationship between organisational characteristics and the effects of clinical guidelines on medical performance in hospitals, a meta-analysis. BMC Health Serv Res. 2006;6(1):53. doi: 10.1186/1472-6963-6-53. [DOI] [PMC free article] [PubMed] [Google Scholar]; 26. Dijkstra R, Wensing M, Thomas R, Akkermans R, Braspenning J, Grimshaw JM, et al. The relationship between organisational characteristics and the effects of clinical guidelines on medical performance in hospitals, a meta-analysis. BMC Health Serv Res. 2006;6(1):53. 10.1186/1472-6963-6-53 [DOI] [PMC free article] [PubMed]
- 27.Brusamento S, Legido-Quigley H, Panteli D, Turk E, Knai C, Saliba V, et al. Assessing the effectiveness of strategies to implement clinical guidelines for the management of chronic diseases at primary care level in EU Member States: A systematic review. Health Policy. 2012;107(2–3):168–183. doi: 10.1016/j.healthpol.2012.08.005. [DOI] [PubMed] [Google Scholar]; 27. Brusamento S, Legido-Quigley H, Panteli D, Turk E, Knai C, Saliba V, et al. Assessing the effectiveness of strategies to implement clinical guidelines for the management of chronic diseases at primary care level in EU Member States: A systematic review. Health Policy. 2012;107(2–3):168–83. 10.1016/j.healthpol.2012.08.005 [DOI] [PubMed]
- 28.Allanson ER, Tunçalp Ö, Vogel JP, Khan DN, Oladapo OT, Long Q, et al. Implementation of effective practices in health facilities: a systematic review of cluster randomised trials. BMJ Glob Heal. 2017;2(2):e000266. doi: 10.1136/bmjgh-2016-000266. [DOI] [PMC free article] [PubMed] [Google Scholar]; 28. Allanson ER, Tunçalp Ö, Vogel JP, Khan DN, Oladapo OT, Long Q, et al. Implementation of effective practices in health facilities: a systematic review of cluster randomised trials. BMJ Glob Heal. 2017;2(2):e000266. 10.1136/bmjgh-2016-000266 [DOI] [PMC free article] [PubMed]
- 29.Brennan N, Mattick K. A systematic review of educational interventions to change behaviour of prescribers in hospital settings, with a particular emphasis on new prescribers. Br J Clin Pharmacol. 2013;75(2):359–372. doi: 10.1111/j.1365-2125.2012.04397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]; 29. Brennan N, Mattick K. A systematic review of educational interventions to change behaviour of prescribers in hospital settings, with a particular emphasis on new prescribers. Br J Clin Pharmacol. 2013;75(2):359–72. 10.1111/j.1365-2125.2012.04397.x [DOI] [PMC free article] [PubMed]
- 30.Goodwin V, Jones-Hughes T, Thompson-Coon J, Boddy K, Stein K. Implementing the evidence for preventing falls among community-dwelling older people: a systematic review. J Safety Res. 2011;42(6):443–451. doi: 10.1016/j.jsr.2011.07.008. [DOI] [PubMed] [Google Scholar]; 30. Goodwin V, Jones-Hughes T, Thompson-Coon J, Boddy K, Stein K. Implementing the evidence for preventing falls among community-dwelling older people: a systematic review. J Safety Res. 2011;42(6):443–51. 10.1016/j.jsr.2011.07.008 [DOI] [PubMed]
- 31.Häggman-Laitila A, Mattila L-R, Melender H-L. A systematic review of the outcomes of educational interventions relevant to nurses with simultaneous strategies for guideline implementation. J Clin Nurs. 2017;26(3–4):320–340. doi: 10.1111/jocn.13405. [DOI] [PubMed] [Google Scholar]; 31. Häggman-Laitila A, Mattila L-R, Melender H-L. A systematic review of the outcomes of educational interventions relevant to nurses with simultaneous strategies for guideline implementation. J Clin Nurs. 2017;26(3–4):320–40. 10.1111/jocn.13405 [DOI] [PubMed]
- 32.Tooher R, Middleton P, Babidge W. Implementation of pressure ulcer guidelines: what constitutes a successful strategy? J Wound Care. 2003;12(10):373–382. doi: 10.12968/jowc.2003.12.10.26551. https://doi/10.12968/jowc.2003.12.10.26551. [DOI] [PubMed] [Google Scholar]; 32. Tooher R, Middleton P, Babidge W. Implementation of pressure ulcer guidelines: what constitutes a successful strategy? J Wound Care. 2003;12(10):373–82. https://doi/10.12968/jowc.2003.12.10.26551 [DOI] [PubMed]
- 33.Thomas LH, McColl E, Cullum N, Rousseau N, Soutter J, Steen N. Effect of clinical guidelines in nursing, midwifery, and the therapies: a systematic review of evaluations. Qual Health Care. 1998;7(4):183–191. doi: 10.1136/qshc.7.4.183. [DOI] [PMC free article] [PubMed] [Google Scholar]; 33. Thomas LH, McColl E, Cullum N, Rousseau N, Soutter J, Steen N. Effect of clinical guidelines in nursing, midwifery, and the therapies: a systematic review of evaluations. Qual Health Care. 1998;7(4):183–91. 10.1136/qshc.7.4.183 [DOI] [PMC free article] [PubMed]
- 34.Gross PA, Pujat D. Implementing practice guidelines for appropriate antimicrobial usage: a systematic review. Med Care. 2001;39(8, Supp II):II-55–II-69. doi: 10.1097/00005650-200108002-00004. [DOI] [PubMed] [Google Scholar]; 34. Gross PA, Pujat D. Implementing practice guidelines for appropriate antimicrobial usage: a systematic review. Med Care. 2001;39(8, Supp II):II-55–II-69. [DOI] [PubMed]
- 35.Thomas LH, McColl E, Cullum N, Rousseau N, Soutter J. Clinical guidelines in nursing, midwifery and the therapies: a systematic review. J Adv Nurs. 1999;30(1):40–50. doi: 10.1046/j.1365-2648.1999.01047.x. [DOI] [PubMed] [Google Scholar]; 35. Thomas LH, McColl E, Cullum N, Rousseau N, Soutter J. Clinical guidelines in nursing, midwifery and the therapies: a systematic review. J Adv Nurs. 1999;30(1):40–50. 10.1046/j.1365-2648.1999.01047.x [DOI] [PubMed]
- 36.Wensing M, van der Weijden T, Grol R. Implementing guidelines and innovations in general practice: which interventions are effective? Br J Gen Pract. 1998;48(427):991–997. [PMC free article] [PubMed] [Google Scholar]; 36. Wensing M, van der Weijden T, Grol R. Implementing guidelines and innovations in general practice: which interventions are effective? Br J Gen Pract. 1998;48(427):991–7. [PMC free article] [PubMed]
- 37.Medves J, Godfrey C, Turner C, Paterson M, Harrison M, MacKenzie L, et al. Systematic review of practice guideline dissemination and implementation strategies for healthcare teams and team-based practice. Int J Evid Based Healthc. 2010;8(2):79–89. doi: 10.1111/j.1744-1609.2010.00166.x. [DOI] [PubMed] [Google Scholar]; 37. Medves J, Godfrey C, Turner C, Paterson M, Harrison M, MacKenzie L, et al. Systematic review of practice guideline dissemination and implementation strategies for healthcare teams and team-based practice. Int J Evid Based Healthc. 2010;8(2):79–89. 10.1111/j.1744-1609.2010.00166.x [DOI] [PubMed]
- 38.Fønhus MS, Dalsbø TK, Johansen M, Fretheim A, Skirbekk H, Flottorp SA. Patient-mediated interventions to improve professional practice. Cochrane Database Syst Rev. 2018;9:CD012472. doi: 10.1002/14651858.CD012472.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]; 38. Fønhus MS, Dalsbø TK, Johansen M, Fretheim A, Skirbekk H, Flottorp SA. Patient-mediated interventions to improve professional practice. Cochrane Database Syst Rev. 2018;9:CD012472. 10.1002/14651858.CD012472.pub2 [DOI] [PMC free article] [PubMed]
- 39.O’Brien MA, Rogers S, Jamtvedt G, Oxman AD, Odgaard-Jensen J, Kristoffersen DT, et al. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2007;4:CD000409. doi: 10.1002/14651858.CD000409.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]; 39. O’Brien MA, Rogers S, Jamtvedt G, Oxman AD, Odgaard-Jensen J, Kristoffersen DT, et al. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2007;4:CD000409. 10.1002/14651858.CD000409.pub2 [DOI] [PMC free article] [PubMed]
- 40.Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;6:CD000259. doi: 10.1002/14651858.CD000259.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]; 40. Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;6:CD000259. 10.1002/14651858.CD000259.pub3 [DOI] [PMC free article] [PubMed]
- 41.Stokes T, Shaw EJ, Camosso-Stefinovic J, Imamura M, Kanguru L, Hussein J. Barriers and enablers to guideline implementation strategies to improve obstetric care practice in low- and middle-income countries: a systematic review of qualitative evidence. Implement Sci. 2016;11(1):144. doi: 10.1186/s13012-016-0508-1. [DOI] [PMC free article] [PubMed] [Google Scholar]; 41. Stokes T, Shaw EJ, Camosso-Stefinovic J, Imamura M, Kanguru L, Hussein J. Barriers and enablers to guideline implementation strategies to improve obstetric care practice in low- and middle-income countries: a systematic review of qualitative evidence. Implement Sci. 2016;11(1):144. 10.1186/s13012-016-0508-1 [DOI] [PMC free article] [PubMed]
- 42.Chakkalakal RJ, Cherlin E, Thompson J, Lindfield T, Lawson R, Bradley EH. Implementing clinical guidelines in low-income settings: A review of literature. Glob Public Health. 2013;8(7):784–795. doi: 10.1080/17441692.2013.81579. [DOI] [PubMed] [Google Scholar]; 42. Chakkalakal RJ, Cherlin E, Thompson J, Lindfield T, Lawson R, Bradley EH. Implementing clinical guidelines in low-income settings: A review of literature. Glob Public Health. 2013;8(7):784–95. 10.1080/17441692.2013.81579 [DOI] [PubMed]
- 43.Solberg LI. Guideline implementation: what the literature doesn’t tell us. Jt Comm J Qual Improv. 2000;26(9):525–537. doi: 10.1016/S1070-3241(00)26044-6. [DOI] [PubMed] [Google Scholar]; 43. Solberg LI. Guideline implementation: what the literature doesn’t tell us. Jt Comm J Qual Improv. 2000;26(9):525–37. 10.1016/S1070-3241(00)26044-6 [DOI] [PubMed]
- 44.Arditi C, Rège-Walther M, Durieux P, Burnand B. Computer-generated reminders delivered on paper to healthcare professionals: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2017;7:CD001175. doi: 10.1002/14651858.CD001175.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]; 44. Arditi C, Rège-Walther M, Durieux P, Burnand B. Computer-generated reminders delivered on paper to healthcare professionals: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2017;7:CD001175. 10.1002/14651858.CD001175.pub4 [DOI] [PMC free article] [PubMed]
- 45.Dexheimer JW, Borycki EM, Chiu K-W, Johnson KB, Aronsky D. A systematic review of the implementation and impact of asthma protocols. BMC Med Inform Decis Mak. 2014;14(1):82. doi: 10.1186/1472-6947-14-82. [DOI] [PMC free article] [PubMed] [Google Scholar]; 45. Dexheimer JW, Borycki EM, Chiu K-W, Johnson KB, Aronsky D. A systematic review of the implementation and impact of asthma protocols. BMC Med Inform Decis Mak. 2014;14(1):82. 10.1186/1472-6947-14-82 [DOI] [PMC free article] [PubMed]
- 46.May CR, Sibley A, Hunt K. The nursing work of hospital-based clinical practice guideline implementation: an explanatory systematic review using Normalisation Process Theory. Int J Nurs Stud. 2014;51(2):289–299. doi: 10.1016/j.ijnurstu.2013.06.019. [DOI] [PubMed] [Google Scholar]; 46. May CR, Sibley A, Hunt K. The nursing work of hospital-based clinical practice guideline implementation: an explanatory systematic review using Normalisation Process Theory. Int J Nurs Stud. 2014;51(2):289–99. 10.1016/j.ijnurstu.2013.06.019 [DOI] [PubMed]
- 47.Nguyen, et al. How does integrated knowledge translation (IKT) compare to other collaborative research approaches to generating and translating knowledge? Learning from experts in the field. Health Research Policy and Systems. 2020;18:35. doi: 10.1186/s12961-020-0539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]; 47. Nguyen et al. How does integrated knowledge translation (IKT) compare to other collaborative research approaches to generating and translating knowledge? Learning from experts in the field. Health Research Policy and Systems. 2020; 18:35. [DOI] [PMC free article] [PubMed]
- 48.Biermann O, Kuchenmüller T, Panisset U, Leys M. Int J Health Governance. Policy dialogues: facilitators’ perceived role and influence. [Google Scholar]; 48. Biermann O, Kuchenmüller T, Panisset U, Leys M. Policy dialogues: facilitators’ perceived role and influence. Int J Health Governance.
- 49.Moat KA, Lavis JN, Clancy SJ, El-Jardali F, Pantoja T. Knowledge Translation Platform Evaluation study team. Evidence briefs and deliberative dialogues: perceptions and intentions to act on what was learnt. Bull World Health Organ. 2014;92(1):20–28. doi: 10.2471/BLT.12.116806. [DOI] [PMC free article] [PubMed] [Google Scholar]; 49. Moat KA, Lavis JN, Clancy SJ, El-Jardali F, Pantoja T; Knowledge Translation Platform Evaluation study team. Evidence briefs and deliberative dialogues: perceptions and intentions to act on what was learnt. Bull World Health Organ. 2014;92(1):20-8. 10.2471/BLT.12.116806 [DOI] [PMC free article] [PubMed]
- 50.Boyko JA, Lavis JN, Abelson J, Dobbins M, Carter N. Deliberative dialogues as a mechanism for knowledge translation and exchange in health systems decision-making. Soc Sci Med. 2012;75(11):1938–1945. doi: 10.1016/j.socscimed.2012.06.016. [DOI] [PubMed] [Google Scholar]; 50. Boyko JA, Lavis JN, Abelson J, Dobbins M, Carter N. Deliberative dialogues as a mechanism for knowledge translation and exchange in health systems decision-making. Soc Sci Med. 2012;75(11):1938-45. 10.1016/j.socscimed.2012.06.016 [DOI] [PubMed]
- 51.Morgan RL, Kelley L, Guyatt GH, Johnson A, Lavis JN. Decision-making frameworks and considerations for informing coverage decisions for healthcare interventions: a critical interpretive synthesis. J Clin Epidemiol. 2018;2018;9423(2):143–150. 120–133. doi: 10.1016/j.jclinepi.2017.09.023. doi: 10.1016/j.jclinepi.2017.09.023. [DOI] [PubMed] [Google Scholar]; 51. Morgan RL, Kelley L, Guyatt GH, Johnson A, Lavis JN. Decision-making frameworks and considerations for informing coverage decisions for healthcare interventions: a critical interpretive synthesis. J Clin Epidemiol. 2018;94:143-50. 10.1016/j.jclinepi.2017.09.023 2018; 23(2): 120-33. [DOI] [PubMed]


