Abstract
With an ever-increasing number of revisions, the surgeons will be faced with the dilemma of choosing the right implant for the revision knee. The soft tissue viability governs the choice of an implant at the time of revision. The selection ranges from the cruciate-retaining to the rotating/fixed hinge implants. The surgeon needs to plan preoperatively, but usually, the final decisions are made intraoperative. As determining the amount of constraint necessary can be challenging, we have tried to lay down a few pointers, which would help to make that choice. The posterior stabilized implants can manage most revision knees; in certain situations where they cannot accommodate the flexion-extension gap imbalance, a varus-valgus constrained implant should be used. The rotating hinge implants are used for severe instabilities or loss of soft tissue or bone around the knee. The use of a higher constraint implant has its consequences like reduced life span and reduced function. Thus it is crucial to use the least amount of constraint as necessary – however, as much as required.
Keywords: Constraint, Revision knee, Rotating hinge, Revision total knee arthroplasty, Stems, Varus valgus constrained
1. Introduction
Revision total knee replacement (TKR) is an epidemic in the waiting, as the numbers and the indications of primary TKRs are ever increasing. While failure mechanisms have been manifold, infection, aseptic prosthetic loosening, infection, and instability have been the leading causes. Revision TKR needs to be tailored according to the cause of failure of the primary TKR. It is a complex undertaking that requires attention to detail to restore a functional joint. Revision surgery goals are the same as a primary TKR that is to achieve a well-aligned, stable, and functional joint. The revision TKR prosthesis should compensate for the bone loss and provide the stability. Wide spectrum of implants is available with varying combinations of prosthetic constraints, augmentations, and extension stems to compensate both for the instability and bone loss. The instability needs to be assessed preoperatively, but often, the decision is intra-operative when the final releases and balancing have been done.
The prosthetic design for revision TKR varies with increasing levels of constraint, ranging from posterior cruciate retention to posterior cruciate substitution, varus-valgus constraint, and hinged designs. The word constrained for revision TKR implants does not necessarily mean a hinge-linked device. These designs are a balance between conformity and constraint. Conformity is the degree to which the femoral and tibial articular surfaces match each other, and accordingly, the load is disseminated across the bearing surface. While an increase in conformity does increase constraint, constraint usually means a substitute for soft tissue, which is either torn or not functional. Biomechanically any increase in the constraint of the prosthesis also increases its capability to transmit loads to its fixation to the bone; it is preferable for the loads to be transmitted by the soft-tissue stabilizers. So as we increase the constraint, also the stress across the bone implant interface increases, which can affect the longevity of the implant. Thus, it is recommended to use the least amount of constraint as possible so that the least load is transmitted through the bone-implant interface.
1.1. Cruciate retaining prosthesis
A cruciate retaining (CR) prosthesis is the prosthesis with the least constraint and needs the posterior cruciate ligament (PCL) to be intact and functional. They are rarely used in a revision scenario and may be considered for a revision of unicondylar knee replacement with an intact and functional PCL. The PCL may be retained if flexion and extension gaps are balanced with maintenance and restoration of the anatomic joint line. Advantages of CR designs in revision knee arthroplasty are the preservation of bone stock and the theoretical benefits for retention of the PCL found in primary TKR. The PCL is frequently observed to be attenuated or grossly absent at the time of revision TKA, which necessitates the conversion to a cruciate-substituting construct. In an infrequent situation in which the implant alignment and stability are well documented and only the PCL is at fault for the instability, an insert change into an ultracongruent one (if available by the implant manufacturer) may be attempted. However, the results are not very promising.1
1.2. Cruciate substituting prosthesis (posterior stabilized {PS})
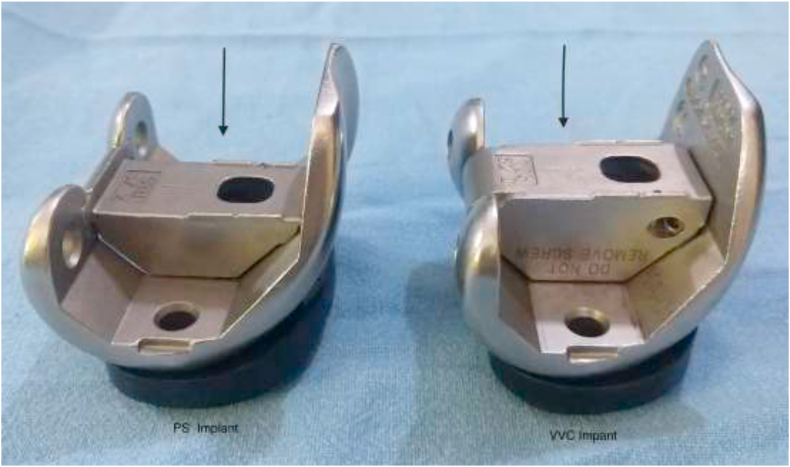
The PS implants are used in the absence of PCL and with intact collaterals. The PS design incorporates a post and cam mechanism to enhance flexion stability and posterior femoral rollback (Fig. 1, Fig. 2). There are multiple types of cam-and-post mechanisms available that differ in post size (height and width), shape, and sagittal-plane position. The surgeon must be aware of the specification of the implant that he uses, as the engagement of the post and cam may vary. Traditionally the engagement occurs at 70-degree flexion. This sometimes brings the peculiar situation of mid-flexion instability in this type of implant in early arc of flexion in some designs.2,3
Fig. 1.
Showing the deeper notch and box of the VVC compared to PS implant.
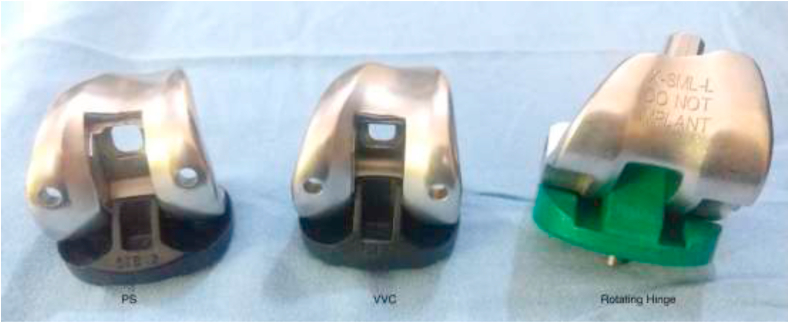
Fig. 2.
The Insert design difference between the PS, VVC & RHK.
The PS implant offers stability against posterior subluxation of the tibia in knee flexion as opposed to the CR implant. However, the PS implant does not offer any protection against mediolateral instability. It also has a tendency of dislocation of the post and cam mechanism if the flexion and extension gaps are not balanced. Especially if the flexion gap is large (as is usually the case in a revision scenario) and putting a thicker insert would either lead to flexion deformity (an imbalance of the extension gap) or a raised joint line (if the distal femur is cut further to compensate for the large flexion space). Therefore, in the scenarios where there is mediolateral instability or there is a large flexion gap (>3–5 mm) we have to use a higher constraint implant.
1.3. Varus-valgus constrained (VVC) prosthesis
These implants are labeled as unlinked constrained implants, They are typically used in situations of deficient collateral ligament support which results in intrinsic varus-valgus instability or flexion gap laxity that is large enough not to be addressed by the posterior-stabilized prosthesis. These implants typically have a deeper and larger intercondylar box in the femur and a correspondingly taller and broader polyethylene post, which may be reinforced with a metal peg (Fig. 3a &3b). The tight fit between the enhanced post and deep box imparts stability by restrictingfemoro-tibial rotation, medial-lateral translation, and varus-valgus angulation (Fig. 4a&4b). These implants do not protect against hyperextension forces because they rely on intact posterior soft tissues; thus, in the presence of hyperextension laxity, these are not ideal implants. As the constraint level is increased in these implants, they depend less on the soft tissues to transmit the strain forces and the forces are transmitted more across the bone and implant interface. In situations where the instability persists post revision surgery the post and cam mechanism is not able to compensate for the instability. In situations of persistant flexion instability the knee may dislocate with disengagement of the post and cam mechanism. In cases of hyperextension instability, the cam post may break due to the repeated stresses across the polyethlene.4,5
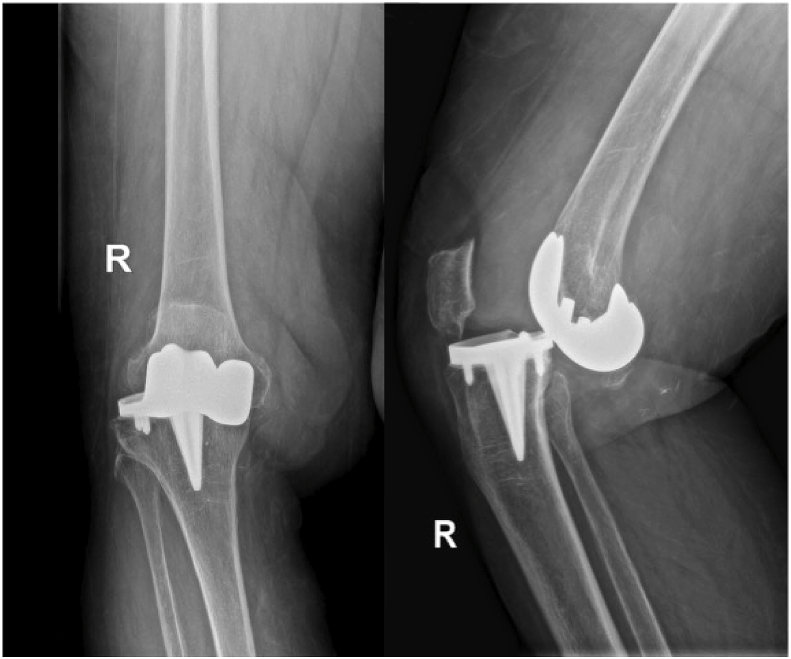
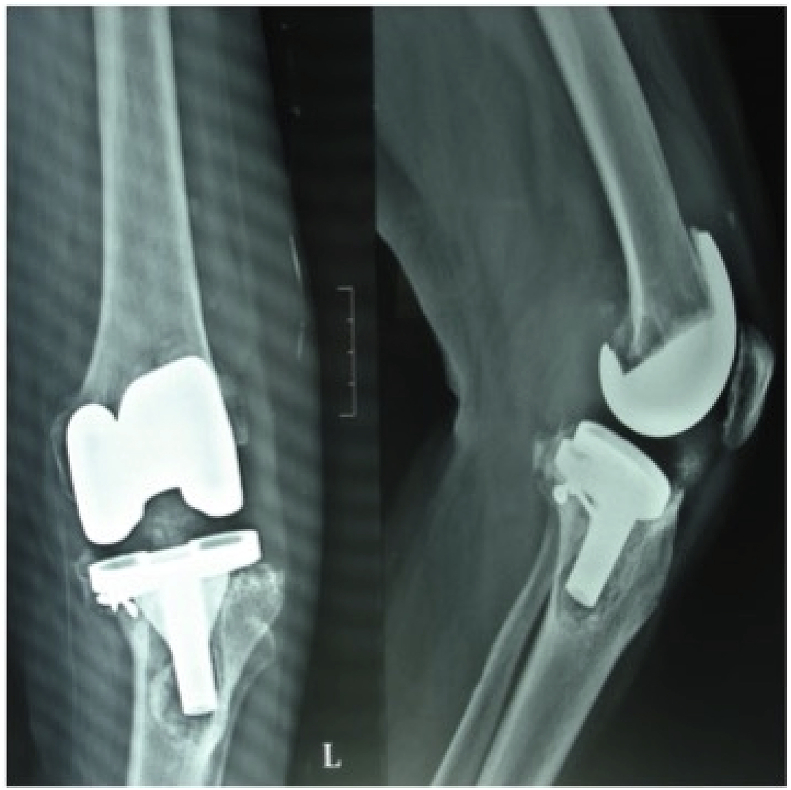
Fig. 3a.
Pre op X rays of Dislocated tibiofemoral articulation of TKR.
Fig. 3b.
Post op films showing VVC implant in situ.
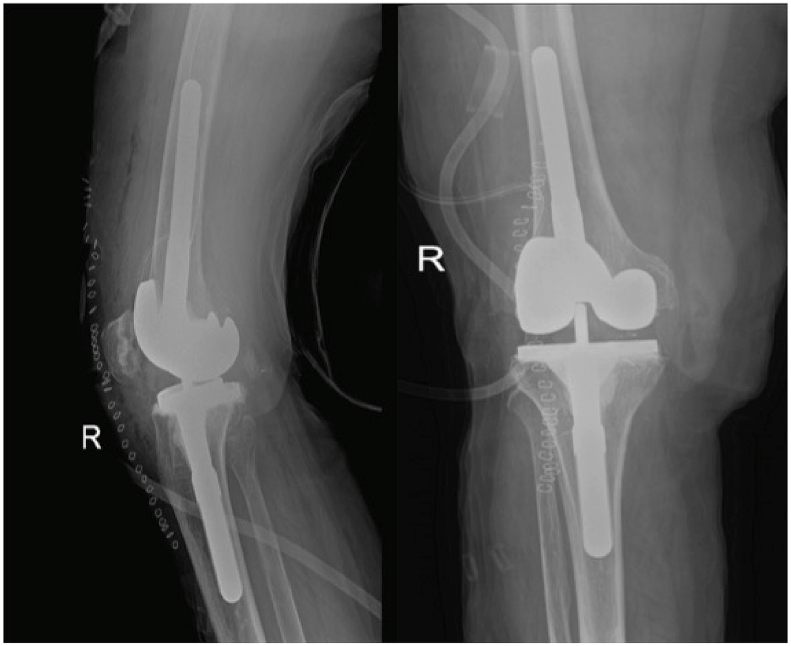
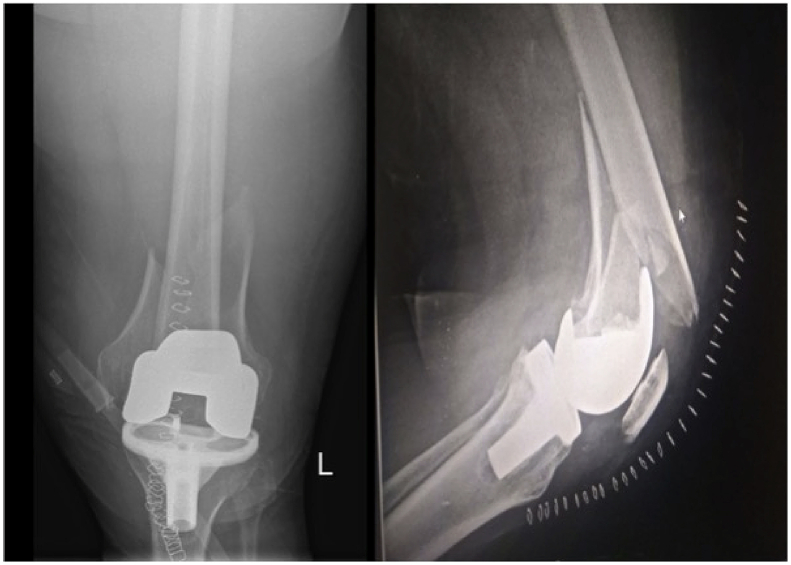
Fig. 4a.
Pre op X rays of Failed TKR with medial tibial condyle collapse.
Fig. 4b.
Post op showing defect built up with use of medial tibial wedge and then use of VVC implant.
Barrack6 when working on rotating hinge implants described certain criteria that must be met to consider a VVC implant in a revision setting: flexion-extension gap difference should be less than 10 mm, the joint line should be restored within 10 mm of the physiologic joint line, femur should be reconstructable in the anteroposterior dimension, and some functional fibers of collateral ligaments must be intact. If all of these criteria are not met, a hinged implant should be selected.6
In some aspects, the unlinked VVC implants are more rotationally constrained than the rotating hinge impacts. In rotational freedom, the rotating hinge implants allow more degrees of rotation than the VVC implants. In biomechanical studies this inability to accommodate the rotation has been proven to transmit the forces across the bone implant interface. VVC implants, if they are fixed bearing designs lead to a higher transmission of the forces in the proximal tibia which leads to increased micromotion of the implants as compared to a rotating hinge implant. In view of the higher forces transmitted use of additional fixation such femoral and tibial stems or sleeves is highly recommended with the use of these implants. The stems help by enhancing fixation and also in providing load sharing.7,8
1.4. Linked constrained prosthesis
1.4.1. Hinged prosthesis
Historically the use of hinged prostheses was started in1950s. Early designs, such as the Shiers,9 Walldius,10 and Guepar11 were used for primary arthroplasty. These were metal on metal articulations with movement along a single axis of flexion and extension with a hyperextension stop. Results with early metal-on-metal fixed-hinge implants were poor. The failures were associated with poor implant design, higher constraint leading to stress transmission across the bone cement interface and subsequent loosening.12 The metal on metal articulation producing metal debris was also linked to early failures. This led to some modifications wherein the metal was articulated with a polyethylene bushing. In a series of 103 cases in which Stanmore implants were used for both primary and revision procedures, Grimer et al.13 reported 80% prosthetic retention at an average follow-up of 68 months.
The long-term results of the hinged prosthesis even with the improvements in the implant design and the change of articulation (from metal on metal to metal on polyethylene) have not been very encouraging.14 Ruggieri et al. used modular fixed-hinge megaprosthesis (The Kotz Modular Femur-Tibia Reconstruction System (KMFTR; Stryker; UK) and the Howmedica Modular Reconstruction System (HMRS; Stryker; UK)) for musculoskeletal tumors treated with limb-salvage surgery and reconstruction and had a mean follow up for 11 years. They reported survival rate (end point revision) of 80% and 55% at 10 and 20 years, respectively, with revisions occurring for breakage, aseptic loosening, and infection.15
With the advent of rotating hinge prosthesis the usage of fixed hinge prosthesis has been limited to tumor surgeries, extensor mechanism insufficiencies and neurological situations.
1.4.2. Rotating hinge prosthesis
Rotating hinge knee (RHK) design was developed to overcome the flaws of the hinged prosthesis. The rotating hinges have tried to overcome the limitations of hinged prostheses by permitting rotational freedom, thereby helping in redistributing the forces passing through the bone implant interface. The rotational freedom can also help in patellar tracking and stability.
Early designs of rotating hinge knee prosthesis involved the Herbert, Sheehan and Spherocenteric types.16 The trochlear flange and the patellar groove were missing in the earlier versions and this led to initial failures and difficulties with poor functional outcomes. The femoral component was then modified and designed to have a flange to accommodate the patella, improving the functional scores. The Noilles rotating hinge arthroplasty was introduced in 1976. This initial design had a tibia-bearing component, which fits into a cemented polyethylene tibial component. The tibia-bearing component was then fixed between the flanges of the femoral component by an axle. The tibia bearing component had rotational freedom of up to 20° without significant prosthetic resistance. Some axial distraction of the tibia-bearing component was also possible, in theory this rotation and axial distraction would reduce stress at the bone-cement interface. Several modifications have been made in the design, like redesigning the femur to a condylar-type implant to prevent the femoral component's subsidence. It has evolved over the years to become the S-ROM modular prosthesis (Fig. 5).16
Fig. 5.
S ROM noiles prosthesis.
The Rotating hinges have established their space in the revision TKR armamentarium over the years though remaining the last choice for a surgeon. In certain conditions they offer the only solution. RHK are used in cases of instability, which is not balanced by correcting the implant placement or that cannot be managed by PS, or VVC type implants. In cases of flexion instability with an adequate extension gap – a thicker Poly insert will elevate the joint line, lead to patella infera and a flexion deformity, also cutting more of distal femur will compromise the ligament attachment. In such conditions we can consider using RHK implant. The authors tend to make the choice between the VVC and RHK on table. The difference between flexion and extension gap is more than 10 mm, which persists even after tibial build up, and femoral sizing and positioning then the use of RHK is considered.
Situations with severe bone loss wherein the bony attachments of the ligaments is compromised RHK implant should be considered when the bone defect is built up by the sleeves or cones and a good stable fit is achieved, an assessment on the table of ligament integrity would define the choice.
RHK knees have become an area of renewed interest as the numbers of re-revisions are increasing. The results have been mixed in literature. The sheer heterogeneity of data as the RHK implants have been used for very varied situations and thus having a proper study becomes difficult. However, there are case series of medium-term follow ups of surgeons who have used these implants. In cases of aseptic revisions Barack et al. followed 16 patients and compared them to revision cases done with VVC implants and found good improvement in functional scores at mean 4.6 years follow up with a 20% complication rate.17 Joshi and Navarro-Quilis followed up 78 knees using the Endo Model hinged knee for a mean of 5 years. They had a complication rate of 27% with complications like infection, extensor rupture and dislocations.18
408 consecutive cases of rotating hinged knee implants of different makes were reported by Cottino et al. using the RHK for aspetic, septic failures and for complex primary knees. At a mean follow up of 4 years they reported improved functional outcomes and a low revision rates. The cumulative incidence for aseptic loosening was 1.7% at two years and 4.5% at 10 years. The cumulative incidence for any surgical revision was 9.7% at two years and 22% at 10 years. The use of metaphyseal porous cones was associated with a lower risk of re-operation.19
In cases of distal femur or proximal tibial tumors where either the disease process or the resection of bone entails removal of the ligamentous supports megaprosthesis implants are used to replace the bone and a rotating hinge articulation is used to compensate for the absent ligamentous support. The megaprosthesis have become modular with improvements in the coating and osseous integration methods. Pala et al. used the Global Modular Replacement system (GRMS) by Stryker in 247 knees with mean follow up of 4 years.20 They had overall failure rate of 29% with infection having the highest incidence. The implant survivorship was 70% at 4 years and 58% at 8 years.20 Myers et al. published a long term follow up of tumor reconstruction of distal femur and proximal tibia. They used both fixed and rotating hinge implants. They had a mean follow up of 15 years and though the early rates of any failure were similar between fixed and rotating hinge but at 10 years the aseptic revision risk for fixed hinge was 35% and for a rotating was 24%. The overall risk of revision fell by 52% when the rotating-hinge implant was utilized.21
Periprosthetic fractures with loose implants are the expanded indications for hinged implants in older patients (Fig. 6a, 6b, 6c&6d). The use of distal femoral arthroplasty can be an option for the management of distal, comminuted supracondylar fracture around loose implants, especially in elderly osteoporotic patients who benefit from early mobilization and find it difficult to comply with weight-bearing restrictions post fixation surgery.22 Mortazavi et al. treated 22 periprosthetic fractures of the distal femur with distal femoral replacement. They followed the knees for a mean of 59 months with 18 cases being available for final follow up. They report one aseptic loosening and 3 periprosthetic fractures.23
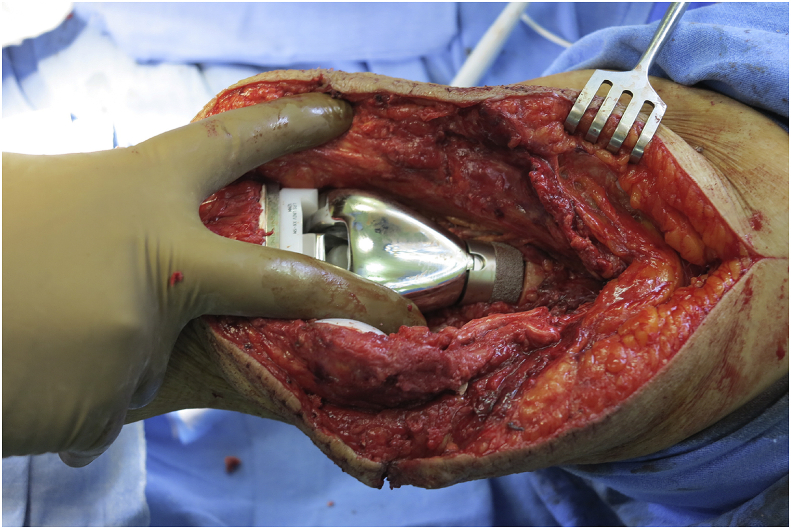
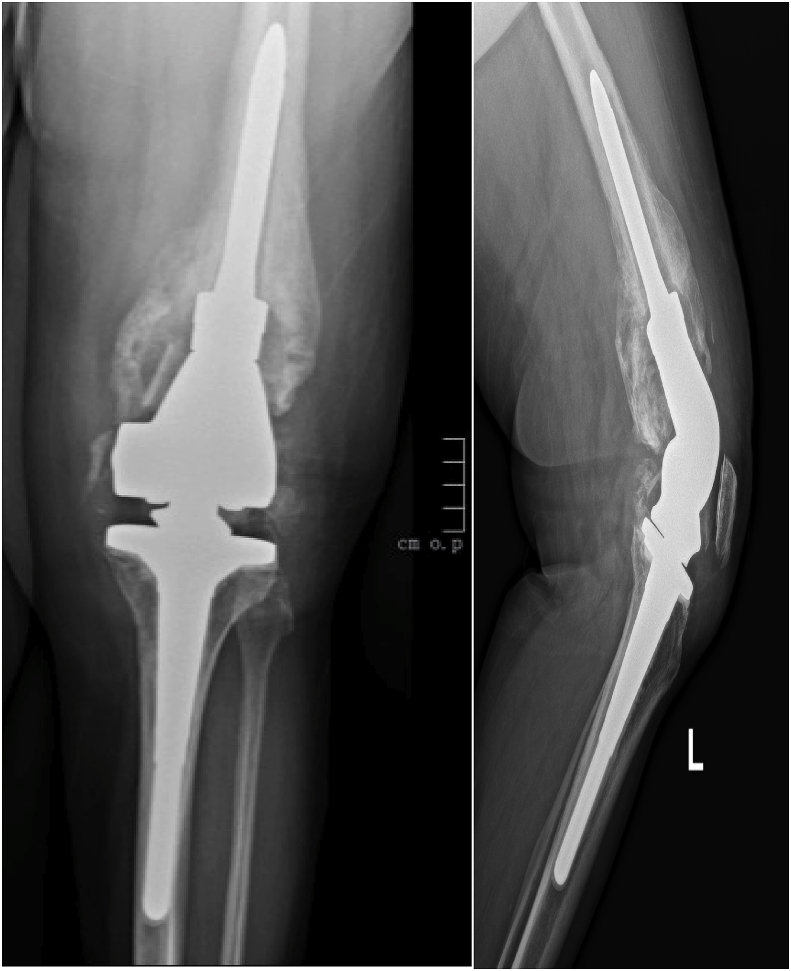
Fig. 6a.
Periprosthetic comminuted Fracture with loose Implant.
Fig. 6b.
CT Scan Picture of the comminuted periprosthetic fracture.
Fig. 6c.
Distal femur replacement prosthesis in situ.
Fig. 6d.
Post op use of Distal femur replacement with RHK as the ligament attachments were all disrupted.
1.4.3. Use of stems with increasing level of constraint
Stems are used in primary or revision TKRs to achieve distal fixation in cases of bone loss. The stems are used to augment fixation. In revision TKRs situations as the soft tissue insufficiency increases and the use of constraint rises, the stresses across the implant, cement and bone interface increases. These increased stresses lead to increased micromotion and early loosening of the implants. Thus stems are used to help in ensuring that the stress is spread across a wider area helping in stability of implants. Stems can be cemented or press fit. The press fit ones are usually used via the hybrid fixation technique where in the cement is used under the tibial tray and a distal canal fixation is achieved with a press fit stem. The choice of the stem and the technique cemented or hybrid is usually governed by the local anatomic milieu and the surgeons experience and choice. Each technique has its merits and difficulties.24 El Zayat et al. did a finite element analysis for hinged knee arthroplasty and stem fixation and found that long cemented stems had the lowest stresses and micromotion. Cementless stems showed more micromotion and increased stress levels especially at the level of the stem tip, which likely explains the stem-end pain following revision knee arthroplasty in some cases.25 There is a biomechanical study done by Anderani et al. wherein they have compared the stress loading of RHK vs. the VVC with stems in situ and found that an RHK transmits more stresses at the tibial stem tip and the VVC transmits at the proximal tibia. They have explained this phenomenon as consequent to the force transmitted by the post-cam mechanism in VVC, hence generating a lever arm that will greatly load the proximal tibia. In the hinged design the forces will transmit the stress to a more distal region in the tibia, leading then to a more gradual stress distribution on the bone due to the rotating hinge.26
1.4.4. Bone loss and choice of constraint
The primary choice of constraint is dependent on the soft tissue envelope surrounding the knee, however, a school of thought feels that bone defect has a role to play in the decision making as well. Vasso et al. gave an algorithm for the use of constraint in revision TKR according to the state of ligaments and the bone defects as per the Anderson Orthopaedic Research Institute (AORI) Classification.27 They describe use of PS implants for intact ligaments and AORI type 1 defects, use of VVC implants in AORI Type 2 defects with ligament insufficiency, and use RHK for AORI type 2 & 3 with insufficient ligaments. Tumor prosthesis for a massive bone loss. Another study by Lee at al comparing revision TKR using a PS and a VVC implant found that the femoral bone defect was an important factor for choosing a prosthesis in addition to the ligament laxity. This could be that the correct femoral implant position governs the flexion stability, which is the key to choosing between PS and VVC implant.28 Morgan-Jones et al. described the anatomical zone of fixation in a revision TKR setting which helps us to predict the modular assembly of the revision components according to the degree of bone damage in the epiphysis, metaphysis, and diaphysis.29
However, the author feels that AORI type 1 & 2 bone defects should not define the choice of constraint in revision TKR. The bone defects should be built up with either augments or bone graft and then after trialing usually you find that a horrible looking knee can be balanced well with a PS type knee with stem augmentation (Fig. 7a and b). The whole concept being to reconstruct the joint line at the normal level and getting adequate balance and tension in the ligaments. Even in certain AORI type 3 defects with the use of cones and sleeves we can build the joint line to an adequate level and use the least amount of constraint needed unless the collateral attachment is completely missing then a hinged implant is required.Table 1
Fig. 7a.
Pre op Infected TKR with static antibiotic loaded spacer insitu.
Fig. 7b.
Post op showing that only build up was required and since ligaments were intact a PS articulation was used.
Table 1.
Authors algorithm.
| Constraint level increasing | Prosthesis | MCL | LCL | PCL |
|---|---|---|---|---|
| Least | PCL Retaining | + | + | + |
| Deep Dish | + | + | – | |
| Posterior Stabilised | + | + | – | |
| Constrained Condylar | +- | + | – | |
| Most | Rotating Hinge | – | – | – |
| Most | Rigid Hinge (used in Neurological or Tumors only) | – | – | – |
2. Authors algorithm
-
-
Use the least constraint possible (Table 1).
-
-
In case of bone defect build the defect with graft, wedges or sleeves and cones then assess the balance of flexion-extension gaps to choose the constraint.
-
-
In case where the osseous attachment of ligaments is in doubt (Tumor, septic revision or re-revision) RHK implant to be kept handy but final assessment on table
-
-
Comminuted periprosthetic fractures with loose femoral implants in elderly patients, a distal femur replacement with a rotating hinge should be considered.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Babis G.C., Trousdale R.T., Morrey B.F. The effectiveness of isolated tibial insert exchange in revision total knee arthroplasty. J Bone Joint Surg Am. 2002;84-A(1):64. doi: 10.2106/00004623-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Fitzpatrick C.K., Clary C.W., Cyr A.J., Maletsky L.P., Rullkoetter P.J. Mechanics of post-cam engagement during simulated dynamic activity. J Orthop Res. 2013;31(9):1438–1446. doi: 10.1002/jor.22366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jo A.R., Song E.K., Lee K.B., Seo H.Y., Kim S.K., Seon J.K. A comparison of stability and clinical outcomes in single-radius versus multi-radius femoral design for total knee arthroplasty. J Arthroplasty. 2014;29:2402–2406. doi: 10.1016/j.arth.2014.03.033. [DOI] [PubMed] [Google Scholar]
- 4.Adravanti P., Vasta S. Varus-valgus constrained implants in total knee arthroplasty: indications and technique. Acta Biomed. 2017;88(2S):112–117. doi: 10.23750/abm.v88i2-S.6521. Published 2017 Jun 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park C.H., Bae J.K., Song S.J. Factors affecting the choice of constrained prostheses when performing revision total knee arthroplasty. Int Orthop. 2019;43(8):1831–1840. doi: 10.1007/s00264-018-4200-8. [DOI] [PubMed] [Google Scholar]
- 6.Barrack R.L. Evolution of the rotating hinge for complex total knee arthroplasty. Clin Orthop Relat Res. 2001;392:292–299. doi: 10.1097/00003086-200111000-00038. [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez J.A. Does the total condylar 3 constrained knee prosthesis predispose to failure of revision total knee replacement? J Bone Joint Surg Am. 2003;85-A(suppl 4):153–156. doi: 10.2106/00004623-200300004-00021. [DOI] [PubMed] [Google Scholar]
- 8.Hartford J.M. Complex primary and revision total knee arthroplasty using the condylar constrained pros- thesis: an average 5-year follow-up. J Arthroplasty. 1998;13(4):380–387. doi: 10.1016/s0883-5403(98)90002-x. [DOI] [PubMed] [Google Scholar]
- 9.Arden GP. Total knee replacement. Clin Orthop. 1973;94: 92–103. [DOI] [PubMed]
- 10.Küsswetter W., Baumann D. Totaler Kniegelenksersatz durch die Walldius-Prothese [Total knee replacement using the Walldius hinge joint (author's transl)] Arch Orthop Unfall-Chir. 1977;88(2):199–215. doi: 10.1007/BF00415100. [DOI] [PubMed] [Google Scholar]
- 11.LeNobel J, Patterson FP. Guepar total knee prosthesis. J Bone Joint Surg Br. 1981;63B:257–260. [DOI] [PubMed]
- 12.Jones E.C., Insall J.N., Inglis A.E. GUEPAR knee arthroplasty results and late complications. Clin Orthop Relat Res. 1979;140:145–152. [PubMed] [Google Scholar]
- 13.Grimer R.J., Aydin B.K., Wafa H. Very long-term outcomes after endoprosthetic replacement for malignant tumours of bone. Bone Joint Lett J. 2016;98-B:857–864. doi: 10.1302/0301-620X.98B6.37417. [DOI] [PubMed] [Google Scholar]
- 14.Knutson K.A.J., Lindstrand A., Lindgren L. Survival of knee arthroplasties: a nation-wide multicenter investigation of 8000 cases. J Bone Joint Surg Br. 1986;68B:795–803. doi: 10.1302/0301-620X.68B5.3782249. [DOI] [PubMed] [Google Scholar]
- 15.Pala E., Trovarelli G., Angelini A., Maraldi M., Berizzi A., Ruggieri P. Megaprosthesis of the knee in tumor and revision surgery. Acta Biomed. 2017;88(2S):129–138. doi: 10.23750/abm.v88i2-S.6523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manning D.W., Chiang P.P., Freiberg A.A. Hinge implants. In: Bono J.V., Scott R.D., editors. Revision Total Knee Arthroplasty. Springer; New York, NY: 2005. [Google Scholar]
- 17.Barrack R.L., Lyons T.R., Ingraham R.Q. The use of a modular rotating hinge component in salvage revision total knee arthroplasty. J Arthroplasty. 2000;15:158–166. doi: 10.1054/arth.2000.9056. [DOI] [PubMed] [Google Scholar]
- 18.Joshi N., Navarro-Quilis A. Is there a place for rotating-hinge arthroplasty in knee revision surgery for aseptic loosening? J Arthroplasty. 2008;23:1204–1211. doi: 10.1016/j.arth.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 19.Cottino U., Abdel M.P., Perry K.I. Long-term results after total knee arthroplasty with contemporary rotating-hinge prostheses. J Bone Joint Surg Am. 2017;99:324–330. doi: 10.2106/JBJS.16.00307. [DOI] [PubMed] [Google Scholar]
- 20.Pala E., Trovarelli G., Calabrò T., Angelini A., Abati C.N., Ruggieri P. Survival of modern knee tumor megaprostheses: failures, functional results, and a comparative statistical analysis. Clin Orthop Relat Res. 2015;473(3):891–899. doi: 10.1007/s11999-014-3699-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Myers G.J.C., Abudu A.T., Carter S.R., Tillman R.M., Grimer R.J. The long-term results of endoprosthetic replacement of the proximal tibia for bone tumours. J Bone Joint Surg [Br] 2007;89-B:1632–1637. doi: 10.1302/0301-620X.89B12.19481. [DOI] [PubMed] [Google Scholar]
- 22.Haidukewych G.J. Role of distal femoral replacement for periprosthetic fractures above a total knee arthroplasty: when and how? J Orthop Trauma. 2019;33(Suppl 6):S33–S35. doi: 10.1097/BOT.0000000000001566. [DOI] [PubMed] [Google Scholar]
- 23.Mortazavi S.M., Kurd M.F., Bender B., Post Z., Parvizi J., Purtill J.J. Distal femoral arthroplasty for the treatment of periprosthetic fractures after total knee arthroplasty. J Arthroplasty. 2010;25(5):775–780. doi: 10.1016/j.arth.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 24.Kang S.G., Park C.H., Song S.J. Stem fixation in revision total knee arthroplasty: indications, stem dimensions, and fixation methods. Knee Surg Relat Res. 2018;30(3):187–192. doi: 10.5792/ksrr.18.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.El-Zayat B.F., Heyse T.J., Fanciullacci N. Fixation techniques and stem dimensions in hinged total knee arthroplasty: a finite element study. Arch Orthop Trauma Surg. 2016;136:1741–1752. doi: 10.1007/s00402-016-2571-0. [DOI] [PubMed] [Google Scholar]
- 26.Andreani L., Pianigiani S., Bori E., Lisanti M., Innocenti B. Analysis of biomechanical differences between condylar constrained knee and rotating hinged implants: a numerical study. J Arthroplasty. 2020;35(1):278–284. doi: 10.1016/j.arth.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 27.Vasso M., Beaufils P., Schiavone Panni A. Constraint choice in revision knee arthroplasty. Int Orthop. 2013;37(7):1279–1284. doi: 10.1007/s00264-013-1929-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee J.K., Lee S., Kim D. Revision total knee arthroplasty with varus-valgus constrained prosthesis versus posterior stabilized prosthesis. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):620–628. doi: 10.1007/s00167-012-1998-2. [DOI] [PubMed] [Google Scholar]
- 29.Morgan-Jones R., Oussedik S.I., Graichen H., Haddad F.S. Zonal fixation in revision total knee arthroplasty. Bone Joint Lett J. 2015;97-B(2):147–149. doi: 10.1302/0301-620X.97B2.34144. [DOI] [PubMed] [Google Scholar]