Abstract
Background
The shifting of medical tasks (MT) to Qualified Medical Practice Assistants (MPA) is an option that can be pursued to ensure adequate health care in Germany despite the increasing scarcity of physicians. The goal of this study was to determine the acceptability of medical task-shifting to MPA among the general population.
Methods
In a nationwide, representative telephone survey, 6105 persons aged 18 or older were asked whether they would be willing to receive care from a specially trained MPA at a physician’s office. Their responses were tested for correlations with sociodemographic characteristics by means of bivariate (chi-squared test, Mann–Whitney U test) and multivariable statistics (logistic regression).
Results
Of the respondents, 67.2% expressed willingness to accept the shifting of MT to an MPA for the treatment of a minor illness, and 51.8% for a chronic illness. Rejection of task-shifting was associated with old age, residence in western Germany, and citizenship of a country other than Germany. For example, non-Germans rejected task-shifting more commonly than Germans, for both minor illnesses (odds ratio [OR] 2.96; 95% confidence interval [2.28; 3.85]) and chronic illnesses (OR 1.61; [1.24; 2.10]).
Conclusion
Further studies are needed to investigate the motives for rejection of medical task-shifting to MPA in order to assess the likelihood of successful nationwide introduction of a uniform delegation model.
Task-shifting from doctors to members of various non-medical specialized professions is routine practice in the Anglo-Saxon countries and Scandinavia (1, 2). In Germany only narrowly defined medical tasks (MT) are delegated, mostly to Qualified Medical Practice Assistants (MPA) (ebox) (3, 4). Although the concept of redistributing certain medical activities has existed since 1975 (5), the requirements, as well as the services eligible for delegation, were first defined in 2013 (6). The prerequisite of delegating tasks is supervision by the physician who has the authority to issue instructions. She or he has the duty of selection, instruction, and supervision (5) and retains full responsibility.
eBOX. Examples of general medical tasks that can be delegated*.
-
Administrative tasks (examples)
Data collection and documentation of examination findings and treatment success
Supporting the doctor in compilation of written communications and reports\
-
Preparation of medical history
Standardized history taking
-
Preparation/provision of information materials
Support in imparting and explaining standardized information
-
Screening services
In adults: laboratory tests (fecal occult blood) in the context of cancer screening
Home visits
-
Injections
Intramuscular and subcutaneous (also vaccinations)
-
Laboratory diagnostic evaluation
General laboratory services (for example, blood glucose measurement)
Technical work-up and assessment of sample materials
-
Supporting measures for diagnostic evaluation/monitoring
Blood sampling (capillary and venous)
(Long-term) blood pressure measurement
(Long-term) electrocardiogram
Lung function test/spirography
Pulse oximetry
Blood gas analyses
Additional vital parameters
Wound care/changing dressings
*Kassenärztliche Bundesvereinigung: Vereinbarung über die Delegation ärztlicher Leistungen an nichtärztliches Personal.[Agreement on the delegation of medical tasks to non-medical personnel] Dtsch Arztebl Int 2013; 110: A-1757 / B-549 / C-525.
The reallocation of MT to MPA is considered a practicable strategy to counteract the consequences of demographic change and shortage of physicians, especially in rural areas. The aim is to create structures that make it possible to maintain the quality of care and simultaneously alleviate doctors’ workload (2, 7, 8).
In recent years in Germany, various training models have been used to qualify MPA to take over tasks eligible for delegation and equip them to carry out specific tasks (7, 9). In evaluating these projects the perspectives of the participating physicians, MPA, and patients on the delegation have been studied (7, 9– 18). Altogether the results show that delegation was broadly acceptable to all participants (15, 18, 19). Almost nothing is known, however, about attitudes in the general population, independently of previous experience.
For Germany, the results of two survey studies are currently available: Höppner’s purely descriptive study on the basis of a representative population survey carried out in 2007 shows that about half of the participants were prepared to consult an MPA instead of a physician for minor illnesses (e.g., colds, gastrointestinal problems, or headache) (20). Data from a nationwide survey of members of the National Association of Statutory Health Insurance Physicians (KBV, Kassenärztliche Bundesvereinigung) in 2017 indicate a greater readiness to be treated by an MPA for minor illnesses than for chronic disorders (21). The KBV survey was the first to ask participants explicitly whether shifting of MT to a specially trained MPA, without any direct contact with a doctor, was acceptable. To date the results of the KBV survey are available only in a descriptive format, rather than embedded in studies (21). The extent to which an expansion or nationwide introduction of such delegation models might be successful in Germany can be assessed only on the basis of more detailed insights into the population’s acceptance of the shifting of MT to MPA. Our aim was to study this aspect on the basis of the following specific questions:
Which population groups refuse the shifting of medical tasks to MPA in the event of a minor illness?
Which population groups refuse the shifting of medical tasks to MPA in the event of a chronic illness?
Methods
To answer these questions we conducted telephone interviews with German-speaking residents aged 18 or older during the period 15 May 2017 to 27 June 2017. The weighted sample is representative for this group and comprises 6105 persons (table 1). For the group of German speakers of non-German nationality, the representativeness is limited (eMethods). Study participants were asked whether they were prepared to receive healthcare from an MPA, for a minor or for a chronic illness, without contact with a doctor (eMethods).
Table 1. Sociodemographic baseline data.
| n | % | |
| Total | 6105 | |
|
Sex Male Female |
2875 3230 |
47.1 52.9 |
|
Age group 18–34 years 35–49 years 50–64 years 65–80+ years |
1178 1477 1637 1812 |
19.3 24.2 26.8 29.7 |
|
Educational attainment (highest qualification) General or intermediate secondary school leaving certificate University/university of applied sciences entrance qualification University/university of applied sciences degree |
4008 863 1111 |
65.6 14.1 18.2 |
|
Employment status Full time Part time/reduced hours In training Retired Unemployed Not in gainful employment/community service/parental leave |
2395 898 269 1999 106 352 |
39.2 14.7 4.4 32.7 1.7 5.8 |
|
Region Western Germany (including western Berlin) Eastern Germany (including eastern Berlin) |
5036 1069 |
82.5 17.5 |
|
Nationality German Other |
5814 291 |
95.2 4.8 |
|
Community size Rural (< 5000 population) Small town (< 20 000 population) Medium-sized town (< 100 000 population) Large city (> 100 000 population) |
1787 1263 1177 1381 |
29.3 20.7 19.3 22.6 |
|
Chronic illness Yes No |
3015 3040 |
49.4 49.8 |
|
Subjective state of health Excellent Very good Good Less than good Poor |
848 1355 2607 959 281 |
13.9 22.2 42.7 15.7 4.6 |
|
Health insurance Statutory Private Uninsured Other |
5266 772 8 33 |
86.3 12.6 0.1 0.5 |
Difference between sum and 6105 = no data
Results
Willingness to be treated by an MPA for a minor illness
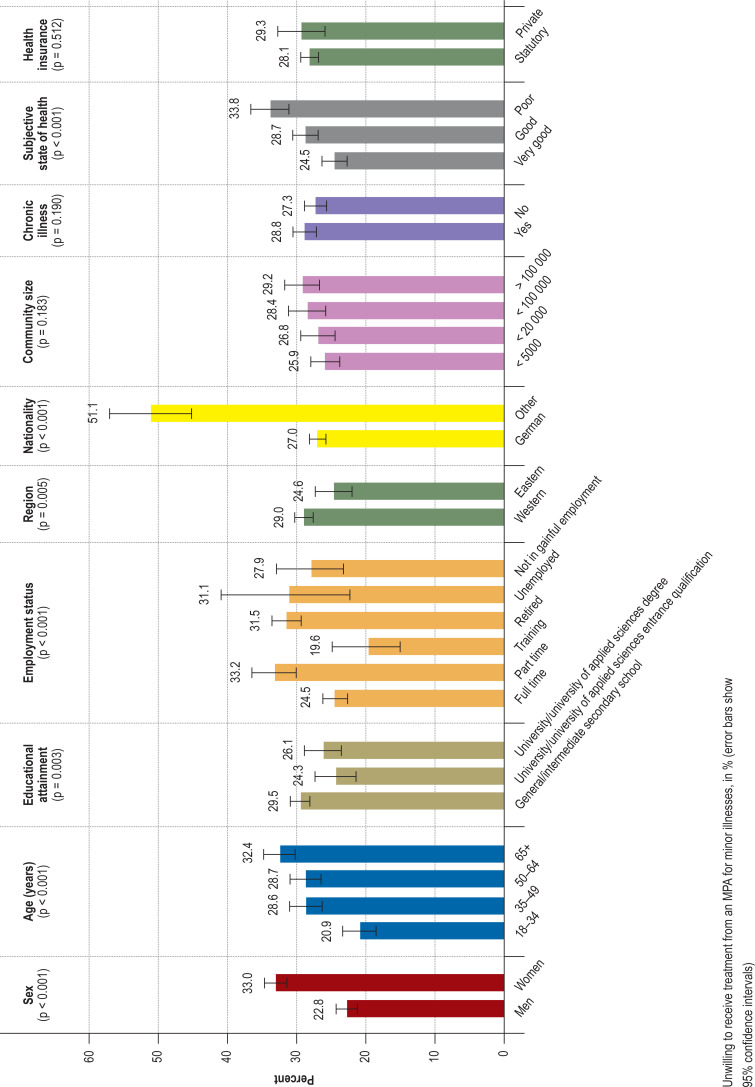
Two thirds of participants (67.2%; 95% confidence interval [66.02; 68.38]) would agree to receive care from an MPA for a minor illness, 27% would not do so, and 1.5% reported previous experience of receiving care from an MPA (21). In the bivariate analyses, sex, age, educational attainment, employment status, region, nationality, and subjective state of health were significantly associated with willingness to receive care from an MPA (figure 1). Persons without German nationality (“non-Germans”) were twice as likely as German nationals to refuse care from an MPA. Respondents aged 65 or older were unwilling to accept task-shifting to an MPA significantly more often than those in the 18–34 age group (figure 1).
Figure 1.
The multivariable analyses confirmed the following associations: non-Germans (odds ratio [OR] 2.96; [2.28; 3.85], those older than 65 (OR 1.76; [1.37; 2.55]), women (OR 1.53; [1.34; 1.74]), residents of western Germany (OR 1.26; [1.07; 1.48]), and persons in subjectively poor health (OR 1.37; [1.16; 1.63]) refused care from an MPA more frequently than the members of the respective reference groups, as defined in Table 2. Education-specific associations and association with employment status were not seen in the multivariable analyses.
Table 2. Multivariable regressions on rejection of task-shifting to an MPA (= unwilling to receive treatment from an MPA).
| Minor illnesses | Chronic illnesses | |||||
| OR | 95% CI | Significance | OR | 95% CI | Significance | |
|
Sex Male Female |
Ref 1.53 |
[1.34; 1.74] |
p < 0.001 |
Ref 1.06 |
[0.94; 1.19] |
p = 0.378 |
|
Age group 18–34 years 35–49 years 50–64 years 65–80+ years |
Ref 1.45 1.46 1.87 |
[1.18; 1.78] [1.18; 1.80] [1.37; 2.55] |
p < 0.001 p < 0.001 p < 0.001 |
Ref 0.94 1.08 1.64 |
[0.78; 1.13] [0.89; 1.30] [1.24; 2.18] |
p = 0.501 p = 0.433 p = 0.001 |
|
Educational attainment (highest certificate) General or intermediate secondary school leaving certificate University/university of applied sciences entrance qualification University/university of applied sciences degree |
1.14 1.01 Ref |
[0.97; 1.34] [0.81; 1.26] |
p = 0.106 p = 0.905 |
1.20 0.86 Ref |
[1.04; 1.39] [0.71; 1.06] |
p = 0.015 p = 0.163 |
|
Employment status Full time part time/reduced hours In training Retired Unemployed Not in gainful employment/community service/parental leave |
1.11 1.32 1.07 1.02 1.26 Ref |
[0.84; 1.45] [0.99; 1.75] [0.70; 1.62] [0.72; 1.45] [0.76; 2.09] |
p = 0.466 p = 0.059 p = 0.763 p = 0.888 p = 0.363 |
0.94 0.96 1.10 0.93 0.84 Ref |
[0.73; 1.20] [0.74; 1.26] [0.77; 1.57] [0.68; 1.29] [0.52; 1.37] |
p = 0.617 p = 0.801 p = 0.599 p = 0.678 p = 0.483 |
|
Region Western Germany (including western Berlin) Eastern Germany (including eastern Berlin) |
1.26 Ref |
[1.07; 1.48] |
p = 0.005 |
1.21 Ref |
[1.04; 1.40] |
p = 0.011 |
|
Nationality German Other |
Ref 2.96 |
[2.28; 3.85] |
p < 0.001 |
Ref 1.61 |
[1.24; 2.10] |
p < 0.001 |
|
Chronic illness Yes No |
/ | / | / |
0.98 Ref |
[0.87; 1.12] |
p = 0.746 |
|
Subjective health Excellent/very good Good Less than good/poor |
Ref 1.15 1.37 |
[1.00; 1.33] [1.16; 1.63] |
p = 0.046 p < 0.001 |
Ref 1.10 1.13 |
[0.96; 1.25] [0.95; 1.33] |
p = 0.159 p = 0.165 |
MPA, Qualified Medical Practice Assistants; CI, confidence interval; OR, odds ratio; Ref, reference category
Willingness to be treated by an MPA for a chronic illness
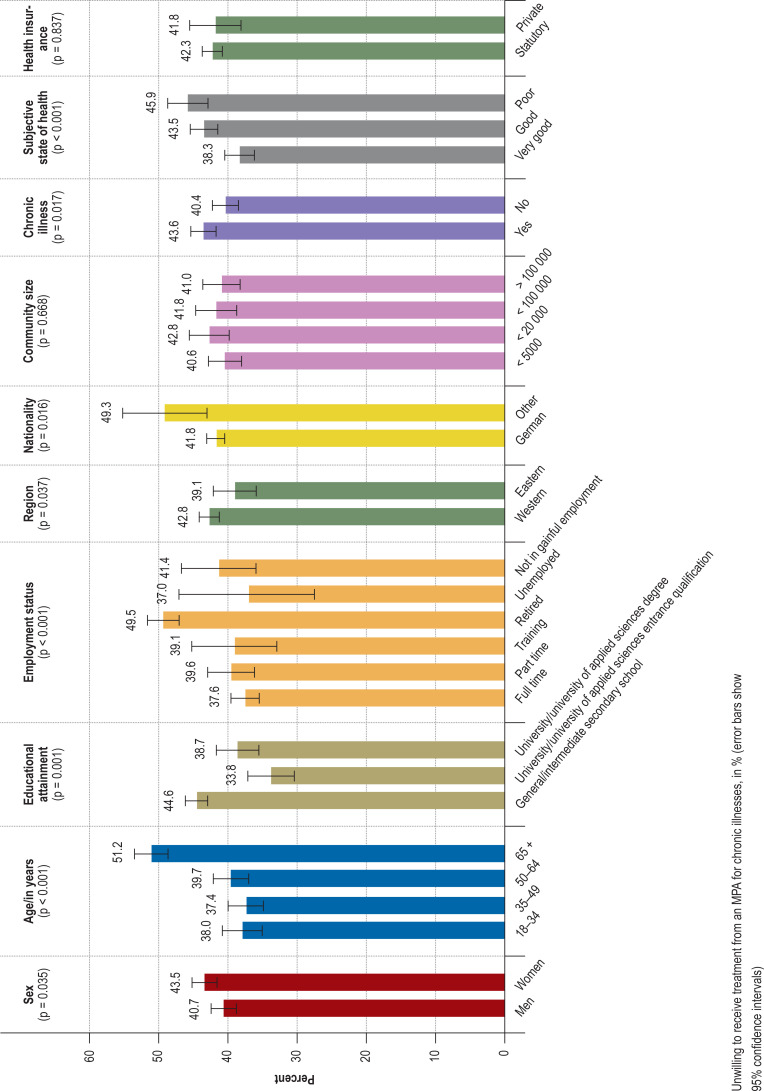
Of the participants with chronic illnesses, 51.8% [50.55; 53.05] were willing to receive care from an MPA, while 38.7% were unwilling. The proportion of participants who reported that they were already receiving care from an MPA for their chronic illness was 1.3% (21). Bivariate analysis of sociodemographic characteristics revealed that the following factors were significantly associated with the acceptance of task-shifting to MPA (figure 2):
Figure 2.
Sex
Age
Educational attainment
Employment status
Region
Nationality
Subjective state of health
Chronic illness
Similar to the question about task-shifting for minor illnesses, older age groups were more critical than younger people, and more non-Germans than German nationals refused to accept MPA performing MT. Those with limited formal education (general or intermediate secondary school leaving certificate) were more inclined to be critical towards task-shifting from doctors to MPA than those with a higher formal education. Persons with a pre-existing chronic illness were more likely to reject task-shifting to an MPA (figure 2). The associations between the acceptability of task-shifting to an MPA and age, nationality, region, and educational status persisted in the multivariable analyses. Persons older than 65 (OR 1.64; [1.24; 2.18]), non-Germans (OR 1.61; [1.24; 2.10]), residents of western Germany (OR 1.21; [1.04; 1.40]), and those with limited formal education (OR 1.20; [1.04; 1.39]) rejected task-shifting from physicians to MPA significantly more often than persons in the respective reference groups (table 2).
Discussion
The results show a mostly positive attitude among the population towards reallocation of MT from physicians to MPA. Two thirds of those questioned were willing to receive care from an MPA for minor illnesses, as were slightly more than half of those with chronic illnesses, in each case without contact with a doctor. It is difficult to compare these results with those of studies from other countries, because the healthcare and training systems in Germany differ greatly from those elsewhere. In the Anglo-Saxon countries and Scandinavia, for example, MPA have been well integrated into medical care for several decades (22, 23). In Germany to date—except in the study reported by Höppner (2008) (20)—only persons who had already agreed to delegation of MT have been studied (1, 14, 15, 18, 19, 24). The data confirm that such patients predominantly rated task-shifting as positive (1, 24).
Comparison of the study reported by Höppner with data from 2007 and the present survey from 2017 shows that the proportion of people in favor of task-shifting from physicians to MPA has notably increased over 10 years. While in Höppner’s study 51% of participants were willing to receive healthcare for minor illnesses from specially trained MPA instead of a doctor, in our survey the proportion was 67%. For chronic illness the proportion of persons in favor of task-shifting from doctors to MPA had more than doubled: in 2007, 20% of survey participants were willing to entertain the idea of receiving healthcare from specially trained MPA (20), by the time of the KBV survey in 2017 the figure had risen to 52%.
In the Höppner study men were more critical than women of task-shifting from physicians to MPA, whereas in the KBV survey more women objected. The question of whether these results related to changed attitudes between the sexes or methodological differences (telephone survey versus written questionnaire; bivariate and multivariable analyses versus descriptive analyses) cannot be answered at this point. An earlier study of ours on the most commonly articulated complaints of patients in the German healthcare system showed, however, that women were more critical about different aspects of healthcare services than men. Based on a quantitative content analysis, we studied 13 505 letters of complaint sent to the federal government’s patient representatives during the period from 2004 to 2007. The results revealed that women criticized individual areas of healthcare provision, e.g., the prescription of medical services or the doctor–patient relationship, significantly more often than men (25). In analogy to the Höppner study, in our 2017 survey too, those with limited formal education (general or intermediate secondary school leaving certificate) were more critical towards reallocation of MT to MPA than those with a higher level of formal education. After the multivariable analysis, however, those with a limited formal education objected to task-shifting from physicians to MPA significantly more often than those with a higher education level only in the chronic illness setting. The acceptance of task-shifting from physicians to MPA for minor illness was no longer significantly associated with educational status.
The additional stratified evaluations of the survey show that especially non-Germans, persons living in western Germany, and those over 65 years of age objected to task-shifting from physicians to MPA significantly more frequently than their counterparts in the respective reference groups. Possible reasons for this are cultural and age-related attitudes and preferences vis-à-vis the doctor–patient relationship. Different studies in German found a rather paternalistically determined perspective on this relationship in patients with a family background of immigration from Turkey (26) and in Russian-speaking immigrants (27, 28). It is plausible that redistribution of MT from physicians to MPA is regarded more critically among those who have internalized the idea of a paternalistic doctor–patient relationship to a greater extent. The rejection of task-shifting to MPA that was noted among older patients is consistent with the findings of the Höppner study (20). Here, too, the reason may be a more paternalistically determined concept of the doctor–patient relationship (29). A possible explanation for the positive attitude of people living in eastern Germany is that in the former German Democratic Republic (GDR), community nurses providing much of the patient care in rural areas had been part of the healthcare service since the 1950s, and this role was reintroduced by means of the AGnES project in 2005 (18, 30, 31). People who experienced life in the GDR can therefore be assumed to be more familiar with the delegation of MT from doctors to MPA, so general acceptance of the task-shift was greater in the present study.
While the focus of our study was on attitudes towards task-shifting among the general population, other studies in Germany have investigated the perspectives of primary-care physicians or MPA towards delegation. Here too, those questioned showed a predominantly positive attitude (32– 34).
Experience in other countries points towards a global trend away from the delegation of individual tasks towards more cooperative styles of working, but in Germany this process is currently still subject to delays because of traditional role concepts, legal frameworks, and the existing billing/reimbursement systems (35).
As regards the effect of and evidence for delegation models in primary medical care, a systematic review showed positive effects in terms of patient satisfaction and rates of hospital admission and mortality (36). Against this background and in view of the results presented here, it seems promising to press ahead with the transfer of MT to MPA. One way forward might be the development of a nationwide standardized delegation model that allows the allocation of treatment for minor illnesses to MPA. The scope and content of such tasks could be elaborated in an interprofessional workshop, as outlined by Egidi et al. (34). In that study, doctors and MPA jointly developed examples of treatment pathways for four consultation scenarios (flu-like infection, gastrointestinal infection, tick bite, request for prescription) that had previously been classified as “trivial” in a scored survey (34).
Limitations
Because the survey of the KBV was a cross-sectional study, only data on current attitudes could be collected and no deeper motivations could be researched.
A further limitation of our study lies in the fact that we investigated only the general willingness of the population as regards task-shifting from physicians to MPA, but did not differentiate in detail between the delegation and substitution of healthcare services. The questions captured only whether subjects would consent to receiving healthcare from an MPA without any further doctor–patient contact. We did not investigate whether the MPA consulted the doctor—that is, acted on the doctor’s instructions—or whether the doctor would have oversight and responsibility. It is therefore not clear whether subjects’ agreement to receiving healthcare from an MPA relates only to the situation where the ultimate oversight and responsibility lies with the physician (delegation) or whether it also relates to a scenario in which the MPA treat patients independently, without supervision, and on their own responsibility (substitution). Further studies are needed to answer this question.
The data were collected by telephone, and only people with a landline were contacted (21, 37). This meant that mainly older persons rather than younger ones were reached (38). Telephone surveys are also associated with a high degree of standardization. It was not defined, for example, what was meant by “minor illnesses” or which tasks the specially trained MPA were going to take over in treatment of minor or chronic illnesses at the physician’s office without any contact between doctor and patient.
A further limitation is that adequate proficiency in German was required in order to participate in the KBV survey; consequently, attitudes towards task-shifting from physicians to MPA among non-Germans with no knowledge of German remains unclear. Since our results show that it was primarily non-Germans who were critical towards task-shifting to MPA, we would, for future surveys, recommend formulating the questionnaires of the KBV surveys in different languages and with sensitivity to persons with a migration background.
In the present study, we were able to undertake regional analyses based on community size and location in eastern or western Germany. For future studies, one might consider linking the findings with structural data, e,g., employment or unemployment rate, in order to generate a regional index (39, 40) and thus arrive at even more meaningful regional results.
Conclusions
Our population showed a high degree of willingness to agree to the redistribution of MT to non-medically trained personnel, e.g., receiving treatment from MPA. It therefore seems worthwhile to develop a consistent nationwide delegation model that permits the treatment of patients with minor illnesses, e.g., coughs and colds, to be transferred to MPA. The feasibility, acceptance, and outcome of such a model could be tested in a pilot study. We recommend taking into consideration the results of the present study.
Particularly the reasons for rejection of task-shifting to MPA by older survey participants, non-Germans, and those with limited formal education should be researched further. The insights thus gained will help to shape the basic and advanced training of health professionals.
Supplementary Material
eMethods
Details of the survey study design and the study methods
Study design
Representatives from the National Association of Statutory Health Insurance Physicians, the Forschungsgruppe Wahlen Telefonfeld Mannheim (FGW), and the Institute of Medical Sociology and Rehabilitation Science at Charité–Universitätsmedizin Berlindeveloped a questionnaire on different aspects of outpatient healthcare services. Between 15 May and 27 June 2017, telephone interviews were conducted with members of the German-speaking residential population in private households who were at least 18 years old. The sample was drawn by the FGW. The FGW is a full-service institute for quantitative surveys in the fields of social and market research (www.forschungsgruppe.de/ueber_die_Forschungsgruppe/FGW_Telefonfeld_GmbH/).
The interviews for the survey in 2017 were conducted by 230 interviewers. For the sample, a regionally stratified random selection was carried out in two stages. Initially households were selected, then one person from each household. For the household sample at the first stage of the selection, telephone numbers were chosen at random from the totality of entries in the official telephone directory. In order also to capture households that had a landline connection but were ex-directory, the final three digits of the respective phone number was substituted by three digits randomly generated by means of the randomized last digit procedure. At the second stage of selection, the person in each household was selected whose birthday had been the most recent of all the members of the household (“last birthday method”). To achieve as high a response rate as possible, up to 15 attempts to contact a randomly selected household were made on different days and at different times of day.
The sample was weighted. First, the design-related differences (number of landline numbers for telephone calls in the household, number of target persons in the household) were corrected in the selection probabilities. On the one hand, this takes into consideration that the chance of a household being contacted depends on the number of landline numbers. On the other hand, the chance that a given person will be selected to participate in the survey depends on the number of target persons per household. In a second step, the failure was corrected by adjusting the sample structures to the structures of the population. The respective nominal distributions (distributions in the population) for sex, age, and education were taken from the official statistics and the microcensus. As no official statistics on sex, age, and education exist for German-speaking foreign nationals, they were allocated the design weight.
The weighted sample is representative for the German residential population ≥ 18 when considering the basics of probability theory. For the group of German-speaking foreign nationals that was included in the survey, a limited degree of representativeness applies because this group is not clearly delimited as a separate population in the official statistics. The case number, weighted and unweighted, is 6105 cases.
Measuring the target variables
The acceptability of task-shifting from doctors to medical practice assistants was determined on the basis of the following two questions:
1. “Would you be willing to be treated for minor illnesses by a specially trained medical practice assistant in the doctor’s office even without any contact with a doctor, or would you object?” (possible responses: would be willing to do so, would object, already doing so, no answer).
2. “And for treatment of a chronic illness in the practice—for example, diabetes, hypertension, or asthma—would you agree to receiving healthcare from a specially trained medical practice assistant even without any contact with a doctor, or would you object?” (possible responses: would be willing to do so, would object, already doing so, no answer). For the multivariable calculations, the response categories were dichotomized (0: willing/already doing, 1: objection).
Sociodemographic determinants
Sex, age, educational attainment, employment status, region, nationality, community size, and type of health insurance were included in the analysis as independent variables. Assuming that health-related characteristics may influence a person’s willingness to receive healthcare from an medical practice assistant, data on subjective state of health and a question about the presence of chronic illness were added to the models. The operationalization (scaling) of the individual variables is shown in Table 1 of the article.
Statistical analyses
Possible differences between groups with regard to the normally scaled variables (sex, gainful employment, region, nationality, chronic illness) were checked using the chi-squared test and between ordinally scaled variables (age, education, subjective health) by means of the Mann–Whitney U test. Exclusion of missing values was done listwise. In order to test whether the significant differences of the bivariate comparisons between groups persisted after controlling for further characteristics, we used multivariable, binary logistic analyses. Questions relating to the transfer of medical tasks to medical practice assistants formed the dependent variables, and odds ratios (OR) and 95% confidence intervals (CI) were calculated for rejection (not willing). Independent variables included in the analyses were those sociodemographic variables that had reached statistical significance in the bivariate analyses. We used the software package SPSS version 25.0 for our statistical evaluations. The significance level was set at 5%.
Key Messages.
The transfer of medical tasks (MT) to Qualified Medical Practice Assistants (MPA) is an option for alleviating the consequences of demographic change and the scarcity of doctors, especially in rural regions, and to support and relieve physicians.
The acceptability of such task-shifting to the general population was investigated on the basis of a nationwide representative survey of the National Association of Statutory Health Insurance Physicians in Germany.
Two thirds (67.2%) of the population would agree to receiving care from a specially trained MPA for minor illnesses, and about half (51.8%) for chronic illnesses, with no contact between doctor and patient.
The acceptance of task-shifting from doctors to MPA is associated in particular with age, region (eastern/western Germany), and nationality.
Further studies should investigate the clinical effects, feasibility, and acceptability of a delegation model that allows treatment for minor illnesses (e.g., colds) to be provided by MPA.
Acknowledgments
Translated from the original German by Birte Twisselmann, PhD.
Funding
The study is part of the NAVICARE project, which is funded by the Federal Ministry of Education and Research (BMBF) in the context of the focus on structural development in health services research (funding code 01GY1601).
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Ruggeri M, Drago C, Moramarco V, et al. New professional roles and patient satisfaction: Evidence from a European survey along three clinical pathways. Health Policy. 2018;122:1078–1084. doi: 10.1016/j.healthpol.2018.07.020. [DOI] [PubMed] [Google Scholar]
- 2.Kleinke S. Delegation ärztlicher Leistungen. J Asthet Chir. 2016;9:44–46. [Google Scholar]
- 3.Maier CB, Batenburg R, Birch S, Zander B, Elliott R, Busse R. Health workforce planning: which countries include nurse practitioners and physician assistants and to what effect? Health Policy. 2018;122:1085–1092. doi: 10.1016/j.healthpol.2018.07.016. [DOI] [PubMed] [Google Scholar]
- 4.Harries L, Tangermann U, Amelung VE. Arztentlastende Konzepte in schwer zu versorgenden Regionen in Deutschland: Ein Vergleich mit England und den Niederlanden. GuS. 2015;69:66–73. [Google Scholar]
- 5.Krull B. Delegation ärztlicher Leistungen an nicht ärztliches Personal: Möglichkeiten und Grenzen. Dtsch Arztebl. 2015;112 [2] [Google Scholar]
- 6.Kassenärztliche Bundesvereinigung. Vereinbarung über die Delegation ärztlicher Leistungen an nicht-ärztliches Personal. Dtsch Arztebl Int. 2013;10 A-1757. [Google Scholar]
- 7.Mergenthal K, Leifermann M, Beyer M, Gerlach FM, Guthlin C. Delegation hausärztlicher Tätigkeiten an qualifiziertes medizinisches Fachpersonal in Deutschland - eine Übersicht. Gesundheitswesen. 2015;78:e62–e68. doi: 10.1055/s-0035-1555948. [DOI] [PubMed] [Google Scholar]
- 8.Robert Koch-Institut. RKI. Berlin: 2015. Gesundheit in Deutschland. Gesundheitsberichterstattung des Bundes. Gemeinsam getragen von RKI und Destatis. [Google Scholar]
- 9.Mergenthal K, Güthlin C. Umsetzung von Delegationskonzepten - So klappt es in der Hausarztpraxis Management von Gesundheitsregionen IV. Wiesbaden: Springer Fachmedien. 2018:89–100. [Google Scholar]
- 10.Kalitzkus V, Schluckebier I, Wilm S. AGnES, EVA, VerAH und Co - Wer kann den Hausarzt unterstützen und wie? Experten diskutieren die Zukunft der Medizinischen Fachangestellten in der hausärztlichen Versorgung. Z Allgemeinmed. 2009;85:403–405. [Google Scholar]
- 11.Dini L, Gisbert Miralles J, Heintze C. Landeszentrum Gesundheit. Bochum: 2018. Delegation in der Hausarztpraxis: Ergebnisse einer Befragung von Hausärztinnen und Hausärzten in Nordrhein-Westfalen. [Google Scholar]
- 12.Mergenthal K, Beyer M, Guthlin C, Gerlach FM. Evaluation des VERAH-Einsatzes in der Hausarztzentrierten Versorgung in Baden-Württemberg. Z Evid Fortbild Qual Gesundhwes. 2013;107:386–393. doi: 10.1016/j.zefq.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 13.Schmiedhofer MH, Brandner S, Kuhlmey A. Delegation ärztlicher Leistungen an nichtärztliche Fachkräfte: Der Versorgungsansatz agnes zwei in Brandenburg - eine qualitative Akzeptanzanalyse. Gesundheitswesen. 2017;79:453–460. doi: 10.1055/s-0035-1555943. [DOI] [PubMed] [Google Scholar]
- 14.Schüler G, Weber I, Löttgen M, Klaes L, Andreßen C. Neue Tätigkeitsprofile für Arzthelferinnen und medizinische Fachangestellte (MFA) in der Versorgung älterer Menschen Bonn, Bad Segeberg. Bundesärztekammer. 2011 doi: 10.1055/s-0032-1321770. [DOI] [PubMed] [Google Scholar]
- 15.Mergenthal K, Guthlin C, Beyer M, Gerlach FM, Siebenhofer A. Wie bewerten und akzeptieren Patienten die Betreuung durch Medizinische Fachangestellte in der Hausarztpraxis? Ergebnisse einer Patienten-Befragung in der HzV in Baden-Württemberg. Gesundheitswesen. 2018;80:1077–1083. doi: 10.1055/s-0042-110402. [DOI] [PubMed] [Google Scholar]
- 16.Dini L, Sarganas G, Boostrom E, Ogawa S, Heintze C, Braun V. German GPs‘ willingness to expand roles of physician assistants: a regional survey of perceptions and informal practices influencing uptake of health reforms in primary health care. Fam Pract. 2012;29:448–454. doi: 10.1093/fampra/cmr127. [DOI] [PubMed] [Google Scholar]
- 17.Dini L, Sarganas G, Heintze C, Braun V. Home visit delegation in primary care: Acceptability to general practitioners in the State of Mecklenburg-Western Pomerania, Germany. Dtsch Arztebl Int. 2012;109 doi: 10.3238/arztebl.2012.0795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van den Berg N, Meinke C, Heymann R, et al. AGnES: supporting general practitioners with qualified medical practice personnel: model project evaluation regarding quality and acceptance. Dtsch Arztebl Int. 2009;106:3–9. doi: 10.3238/arztebl.2009.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schüler G. Neue Tätigkeitsprofile für Arzthelferinnen und medizinische Fachangestellte (MFA) in der Versorgung älterer Menschen (Projekt im Rahmen der Förderinitiative zur Versorgungsforschung der Bundesärztekammer) Gesundheitswesen. 2013:503–509. doi: 10.1055/s-0032-1321770. [DOI] [PubMed] [Google Scholar]
- 20.Höppner K. Böcken J, Braun B, Amhof R, editors. Neue Aufgabenverteilung zwischen Gesundheitsberufen in der Arztpraxis aus Patientensicht Gesundheitsmonitor. Gütersloh. BertelsmanStiftung. 2008:250–269. [Google Scholar]
- 21.Kassenärztliche Bundesvereinigung. Versichertenbefragung der Kassenärztlichen Bundesvereinigung. www.kbv.de/media/sp/Tabellenband_gesamt_KBV_Versichertenbefragung_2017.pdf (last accessed on 9 July 2019) 2017 [Google Scholar]
- 22.Hutchinson L, Marks T, Pittilo M. The physician assistant: would the US model meet the needs of the NHS? BMJ. 2001;323:1244–1247. doi: 10.1136/bmj.323.7323.1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Caldow J, Bond C, Ryan M, et al. Treatment of minor illness in primary care: a national survey of patient satisfaction, attitudes and preferences regarding a wider nursing role. Health Expect. 2007;10:30–45. doi: 10.1111/j.1369-7625.2006.00422.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuhlmann E, Groenewegen PP, Bond C, Burau V, Hunter DJ. Primary care workforce development in Europe: An overview of health system responses and stakeholder views. Health Policy. 2018;122:1055–1062. doi: 10.1016/j.healthpol.2018.07.021. [DOI] [PubMed] [Google Scholar]
- 25.Schnitzer S, Kuhlmey A, Adolph H, Holzhausen J, Schenk L. Complaints as indicators of health care shortcomings: which groups of patients are affected? Int J Qual Health Care. 2012;24:476–482. doi: 10.1093/intqhc/mzs036. [DOI] [PubMed] [Google Scholar]
- 26.Uslu S, Natanzon I, Joos S. The image of general practitioners from the perspective of patients with and without a Turkish migration background—a qualitative study. Gesundheitswesen. 2014;76:366–374. doi: 10.1055/s-0033-1357199. [DOI] [PubMed] [Google Scholar]
- 27.Ries Z, Frank F, Bermejo I, et al. Auf dem Weg zu kultursensitiven Patienteninformationsmaterialien: Ergebnisse einer Fokusgruppenuntersuchung. Psychother Psych Med. 2018;68:242–249. doi: 10.1055/s-0043-117773. [DOI] [PubMed] [Google Scholar]
- 28.Bachmann V, Völkner M, Bösner S, Donner-Banzhoff N. The experiences of Russian speaking migrants in primary care consultations. Dtsch Arztebl. 2014;111:871–876. doi: 10.3238/arztebl.2014.0871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kassenärztliche Bundesvereinigung. Versichertenbefragung der Kassenärztlichen Bundesvereinigung. www.kbv.de/media/sp/KBV_Tabellenband_2013_gesamt.pdf (last accessed on 8 August 2019) 2013 [Google Scholar]
- 30.Korzilius H, Rabbata S. Gemeindeschwestern: Geheimwaffe gegen Überlastung und Unterversorgung. Dtsch Arztebl. 2006;103 A-2926-28. [Google Scholar]
- 31.van den Berg N, Meinke C, Heymann R, et al. AGnES: Correspondenz: AGnES-supporting general practitioners with qualified medical practice personnel—model project evaluation regarding quality and acceptance: support for general practitioners is uncertain. Dtsch Arztebl Int. 2009;106:3–9. doi: 10.3238/arztebl.2009.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goetz K, Kornitzky A, Mahnkopf J, Steinhauser J. At the dawn of delegation? Experiences and attitudes of general practitioners in Germany—a questionnaire survey. BMC Fam Pract. 2017;18 doi: 10.1186/s12875-017-0697-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stumm J, Thierbach C, Peter L, et al. Coordination of care for multimorbid patients from the perspective of general practitioners—a qualitative study. BMC Fam Pract. 2019;20:160. doi: 10.1186/s12875-019-1048-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Egidi G, Bülders S, Diederichs-Egidi H, Mergenthal K. Könnte das nicht auch die MFA erledigen? Bericht über einen interprofessionellen Workshop. Z Allg Med. 2015;91 [Google Scholar]
- 35.Freund T, Everett C, Griffiths P, Hudon C, Naccarella L, Laurant M. Skill mix, roles and remuneration in the primary care workforce: who are the healthcare professionals in the primary care teams across the world? Int J Nurs Stud. 2015;52:727–743. doi: 10.1016/j.ijnurstu.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 36.Martínez-González NA, Djalali S, Tandjung R, et al. Substitution of physicians by nurses in primary care: a systematic review and meta-analysis. BMC Health Serv Res. 2014;14 doi: 10.1186/1472-6963-14-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tille F, Rottger J, Gibis B, Busse R, Kuhlmey A, Schnitzer S. Patients’ perceptions of health system responsiveness in ambulatory care in Germany. Patient Educ Couns. 2019;102:162–171. doi: 10.1016/j.pec.2018.08.020. [DOI] [PubMed] [Google Scholar]
- 38.Statistisches Bundesamt. 94 % der Privathaushalte besitzen ein Handy. www.destatis.de/DE/Presse/Pressemitteilungen/Zahl-der-Woche/2016/PD16_42_p002.html (last accessed on 29 March 2020) [Google Scholar]
- 39.Bauer H, Maier W. GIMD 2010 - Ein Update des „German Index of Multiple Deprivation“ München. Helmholtz Zentrum. 2010 [Google Scholar]
- 40.Kroll LE, Schumann M, Hoebel J, Lampert T. Robert Koch-Institut. Berlin: 2017. Regionale Unterschiede in der Gesundheit - Entwicklung eines sozioökonomischen Deprivationsindex für Deutschland Epidemiologie und Gesundheitsberichterstattung. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods
Details of the survey study design and the study methods
Study design
Representatives from the National Association of Statutory Health Insurance Physicians, the Forschungsgruppe Wahlen Telefonfeld Mannheim (FGW), and the Institute of Medical Sociology and Rehabilitation Science at Charité–Universitätsmedizin Berlindeveloped a questionnaire on different aspects of outpatient healthcare services. Between 15 May and 27 June 2017, telephone interviews were conducted with members of the German-speaking residential population in private households who were at least 18 years old. The sample was drawn by the FGW. The FGW is a full-service institute for quantitative surveys in the fields of social and market research (www.forschungsgruppe.de/ueber_die_Forschungsgruppe/FGW_Telefonfeld_GmbH/).
The interviews for the survey in 2017 were conducted by 230 interviewers. For the sample, a regionally stratified random selection was carried out in two stages. Initially households were selected, then one person from each household. For the household sample at the first stage of the selection, telephone numbers were chosen at random from the totality of entries in the official telephone directory. In order also to capture households that had a landline connection but were ex-directory, the final three digits of the respective phone number was substituted by three digits randomly generated by means of the randomized last digit procedure. At the second stage of selection, the person in each household was selected whose birthday had been the most recent of all the members of the household (“last birthday method”). To achieve as high a response rate as possible, up to 15 attempts to contact a randomly selected household were made on different days and at different times of day.
The sample was weighted. First, the design-related differences (number of landline numbers for telephone calls in the household, number of target persons in the household) were corrected in the selection probabilities. On the one hand, this takes into consideration that the chance of a household being contacted depends on the number of landline numbers. On the other hand, the chance that a given person will be selected to participate in the survey depends on the number of target persons per household. In a second step, the failure was corrected by adjusting the sample structures to the structures of the population. The respective nominal distributions (distributions in the population) for sex, age, and education were taken from the official statistics and the microcensus. As no official statistics on sex, age, and education exist for German-speaking foreign nationals, they were allocated the design weight.
The weighted sample is representative for the German residential population ≥ 18 when considering the basics of probability theory. For the group of German-speaking foreign nationals that was included in the survey, a limited degree of representativeness applies because this group is not clearly delimited as a separate population in the official statistics. The case number, weighted and unweighted, is 6105 cases.
Measuring the target variables
The acceptability of task-shifting from doctors to medical practice assistants was determined on the basis of the following two questions:
1. “Would you be willing to be treated for minor illnesses by a specially trained medical practice assistant in the doctor’s office even without any contact with a doctor, or would you object?” (possible responses: would be willing to do so, would object, already doing so, no answer).
2. “And for treatment of a chronic illness in the practice—for example, diabetes, hypertension, or asthma—would you agree to receiving healthcare from a specially trained medical practice assistant even without any contact with a doctor, or would you object?” (possible responses: would be willing to do so, would object, already doing so, no answer). For the multivariable calculations, the response categories were dichotomized (0: willing/already doing, 1: objection).
Sociodemographic determinants
Sex, age, educational attainment, employment status, region, nationality, community size, and type of health insurance were included in the analysis as independent variables. Assuming that health-related characteristics may influence a person’s willingness to receive healthcare from an medical practice assistant, data on subjective state of health and a question about the presence of chronic illness were added to the models. The operationalization (scaling) of the individual variables is shown in Table 1 of the article.
Statistical analyses
Possible differences between groups with regard to the normally scaled variables (sex, gainful employment, region, nationality, chronic illness) were checked using the chi-squared test and between ordinally scaled variables (age, education, subjective health) by means of the Mann–Whitney U test. Exclusion of missing values was done listwise. In order to test whether the significant differences of the bivariate comparisons between groups persisted after controlling for further characteristics, we used multivariable, binary logistic analyses. Questions relating to the transfer of medical tasks to medical practice assistants formed the dependent variables, and odds ratios (OR) and 95% confidence intervals (CI) were calculated for rejection (not willing). Independent variables included in the analyses were those sociodemographic variables that had reached statistical significance in the bivariate analyses. We used the software package SPSS version 25.0 for our statistical evaluations. The significance level was set at 5%.