To the Editor: We read with great interest the case report by Boesjes et al describing a presentation of recurrent, unilateral perniosis (chilblains) in a woman with prior trauma and reconstructive surgery to the affected site.1 Among the few documented cases of unilateral disease, one important similarity stands out—preceding neurological damage.1, 2, 3 This finding led Boesjes et al to propose a neurogenic component in disease pathogenesis. We report a case of unilateral chilblains which may further support this conclusion in an otherwise healthy 28-year-old Latino man with an extensive orthopedic surgery history.
Our patient presented to the emergency department with a 10-day history of redness and perceived coldness in the lower portion of his left leg. His medical history was notable for a left hip fracture sustained in an automobile accident 1.5 years prior, which was repaired by reduction and internal fixation shortly after the time of injury. The repair was later complicated by lumbosacral plexopathy and avascular necrosis necessitating arthroplasty, which he underwent 5 weeks prior to presentation. The patient was afebrile and felt well; he denied respiratory, neurologic, and cardiac symptoms. Physical examination revealed asymmetric edema and erythema of the left leg with intact peripheral pulses and neurologic function (Fig 1, A and B). Initial differential diagnosis included thromboembolic diseases versus cutaneous small vessel vasculitis.
Fig 1.
A, Dorsal feet demonstrating unilateral plethora and edema of the left foot and ankle extending proximally to the knee. B, Distal portion of left foot at the time of admission, depicting nonblanching, nonpalpable purpuric macules, which were also evident on the lateral dorsal aspect. Note vesicular lesions on the base of purpura of the third toe.
On admission, computed tomography angiography and venous duplex ultrasonography failed to demonstrate occlusive disease. No valvular lesions were identified on echocardiography. Erythrocyte sedimentation rate and C-reactive protein were normal, and an extractable nuclear antigen panel was negative. Serum cryoglobulins were not obtained. A punch biopsy was performed of the left foot lesions, demonstrating dense superficial and deep perivascular and lichenoid lymphocytic infiltration consistent with chilblains (Fig 2). Given the negative workup and lack of cold exposure, the patient's symptoms were felt to be most likely related to dysautonomia secondary to his prior injury and surgeries. He reported resolution of symptoms within 4 weeks with conservative management.
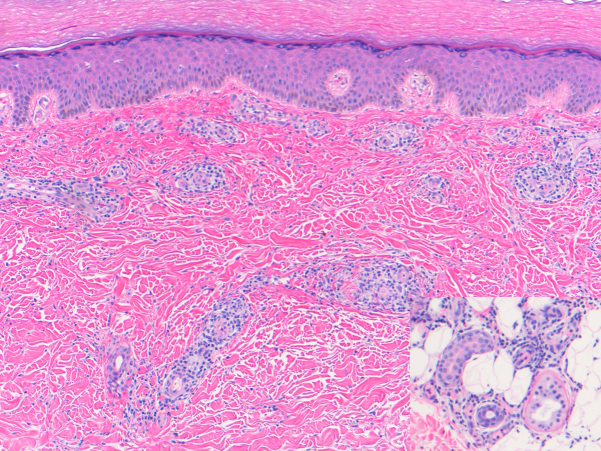
Fig 2.
Punch biopsy of dorsal left foot lesions using hematoxylin-eosin staining. Image: superficial and deep perivascular and peri-eccrine predominantly lymphocytic inflammatory cell infiltrate (original magnification: ×10.) Inset: lymphocytic infiltrate around eccrine glands (original magnification: ×20.)
Conflicts of interest
Dr Guzman discloses the receipt of travel reimbursement from Verrica Pharmaceuticals and has served as an advisory board participant for Johnson & Johnson. These do not pose any conflict of interest. Author Lally and Drs Balagula, Dewall, and Jacobson have no conflicts of interest to declare.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Boesjes C.M., van Rhijn B.D., van Dijk R., Sigurdsson V. Posttraumatic unilateral perniosis: a case report. JAAD Case Rep. 2019;5(10):909–911. doi: 10.1016/j.jdcr.2019.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klapman M.H., Johnston W.H. Localized recurrent postoperative pernio associated with leukocytoclastic vasculitis. J Am Acad Dermatol. 1991;24(5):811–813. doi: 10.1016/0190-9622(91)70119-m. [DOI] [PubMed] [Google Scholar]
- 3.Couture P., Moguelet P., Chasset F., Barbaud A., Senet P., Monfort J.B. Two cases of unilateral chilblains associated with monoparesis. Ann Dermatol Venerol. 2019;146(8-9):557–562. doi: 10.1016/j.annder.2019.01.022. [DOI] [PubMed] [Google Scholar]