Abstract
The human body is continuously threatened by pathogens, and the immune system must maintain a balance between fighting infection and becoming over-activated. Mucosal surfaces cover several anatomically diverse organs throughout the body, such as the respiratory and gastrointestinal tracts, and are directly exposed to the external environment. Various pathogens invade the body through mucosal surfaces, making the mucosa the frontline of immune defense. The immune systems of various mucosal tissues display distinctive features that reflect the tissues' anatomical and functional characteristics. This review discusses the cellular components that constitute the respiratory and gastrointestinal tracts; in particular, it highlights the complex interactions between epithelial and immune cells to induce Ag-specific immune responses in the lung and gut. This information on mucosal immunity may facilitate understanding of the defense mechanisms against infectious agents that invade mucosal surfaces, such as severe acute respiratory syndrome coronavirus 2, and provide insight into effective vaccine development.
Keywords: Gastrointestinal tract, Infection, Mucosal immunity, Respiratory tract
INTRODUCTION
The mucosal immune system consists of immune inductive and effector sites (1). Mucosal immune inductive sites include mucosa-associated lymphoid tissues (MALTs) and mucosa-draining lymph nodes (LNs). Examples of LNs include the mesenteric (MLNs) and cervical LNs (CLNs). MALTs are solitary organized structures containing T and B cell follicles; the gut-associated lymphoid tissue (GALT) and nasopharynx-associated lymphoid tissue (NALT) are typical examples of MALTs (Fig. 1). The lamina propria (LP) of the mucosa, which is an immune effector site, is situated within the subepithelial stroma of mucosal connective tissue and contains effector T cells, plasma cells, macrophages, and dendritic cells (DCs).
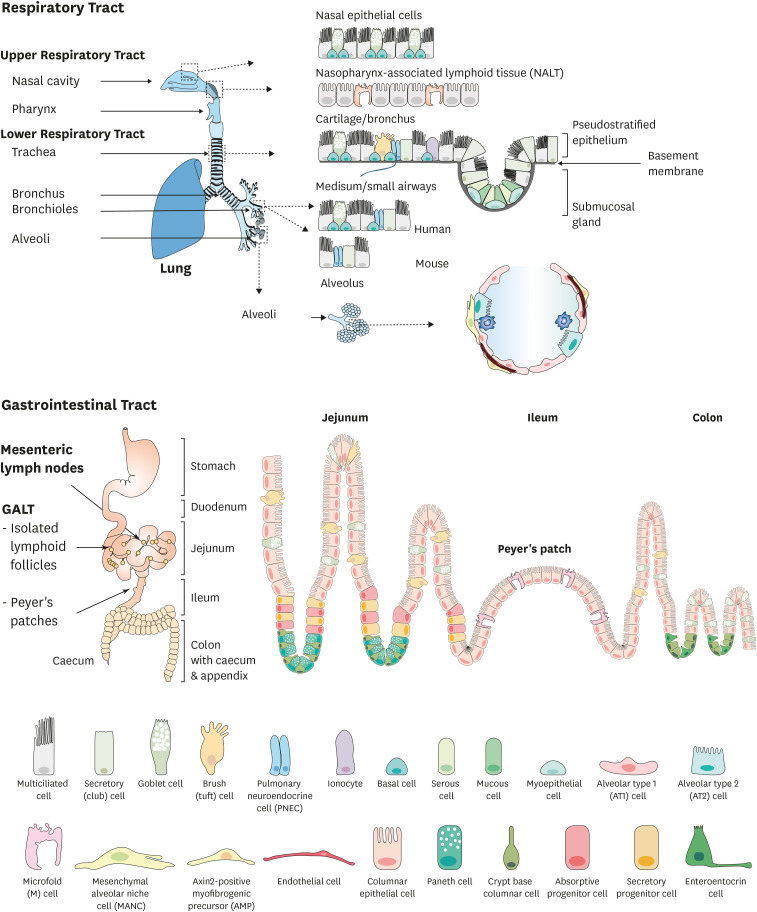
Figure 1.
Cellular composition of the respiratory and gastrointestinal tracts. (A) The respiratory tract consists of the upper (nasal cavity, pharynx) and lower (trachea, bronchus, bronchioles, alveoli) tracts. They are covered by a single layer of epithelial cells, such as multiciliated cells, club cells, goblet cells, basal cells, PNECs, tuft cells, ionocytes, serous cells, myoepithelial cells, AT1 and AT2 cells, mesenchymal alveolar niche cells, and AMPs. (B) The small and large intestines of the gastrointestinal tract are distinguished by the crypt-villus structure and are composed of columnar epithelial, microfold, Paneth, goblet, enteroendocrine, and tuft cells.
AMP, axin2-positive myofibrogenic precursor.
Igs are humoral immune effectors, of which secretory IgA (SIgA) is a primary humoral immune component of the mucosa (2). IgA, which is found in the LP, is produced by plasma cells in dimeric form, whereby two IgA components are linked together by a joining chain. The dimerization of IgA is necessary for its secretion, which is facilitated by the polymeric Ig receptor (pIgR); the secretory component of pIgR covalently interacts with dimeric IgA, completing the structure of the SIgA complex (3). The SIgA complex is transported by pIgR from the basolateral to the apical side of the membrane, then released from pIgR, and secreted to the mucosal surface. SIgA complexes are protected from proteolysis by N-glycosylation of the secretory component.
Alongside SIgA, secretory IgM (SIgM) is also present in mucosal secretions (4). Pentameric IgM is translocated to the apical side of the mucosal membrane following binding to pIgR via the joining chain. IgG levels are notably higher than SIgA levels in the lower respiratory lumen of human airways (5). IgG can be transported into the lumen via the neonatal Fc receptor (FcRn), which comprises MHC class I-like transmembrane protein and β2 microglobulin (6). FcRn also functions as an apical transporter. Although secretory IgD is present in mucosal secretions within aerodigestive mucosa, the basolateral transport mechanism for IgD is unclear (7). These Igs maintain mucosal homeostasis by controlling commensals and protecting against pathogens (8).
The secretory mechanisms of humoral effectors described above are common across various mucosal immune compartments. However, the immune systems of diverse mucosal tissues also exhibit unique characteristics reflecting their anatomical functions. In this review, we discuss the diverse characteristics of regional cellular components in the mucosal immune system of the respiratory and gastrointestinal tracts. In particular, we focus on the mucosal immune response in the humoral defense network of the lung and gut.
CELLULAR COMPONENTS OF THE RESPIRATORY AND GASTROINTESTINAL TRACTS
Respiratory and gastrointestinal epithelia exhibit distinct characteristics but likewise share some anatomical similarities. Both epithelia are lined with columnar epithelial cells with cilia (respiratory tract) or microvilli (gastrointestinal tract), which they produce a physical barrier between the inner body and the environment and act as sentinels for the immune system.
Cellular components of the respiratory system
Respiratory tissues span multiple organs, from the upper respiratory tract (nostrils, nasal cavity, and pharynx) to the lower respiratory tract (trachea, bronchi, bronchioles, and alveoli) (Fig. 1A) (9). The respiratory tract is wrapped with bands of smooth muscle, which supports to airway flow. In humans, a pseudostratified epithelium covers the trachea up to the distal bronchioles; however, in mice, the pseudostratified epithelium extends only to the distal intralobar bronchi (10). The pseudostratified epithelium is a single layer of epithelial cells comprising mainly multiciliated cells, club cells, goblet cells, and basal cells. Multiciliated cells have hundreds of motile cilia on their apical area and transport inhaled particulates and mucus out of the airways retrogradely (11). Club cells, with their dome-shaped apical surface, are primary secretory cells that specifically express uteroglobin (secretoglobin family 1A member 1), the most abundant protein in mucosal lung secretions, and contribute to homeostatic maintenance of the airways (12). Goblet cells secrete mucus, which blocks the influx of inhaled particulates. The secretion of mucus is regulated by IL-13, which is produced by type 2 innate lymphoid cells (ILC2s). Basal cells act as resident stem cells that are capable of long-term self-renewal and differentiation into basal, ciliated, and club cells during homeostasis and after injury (13). The fate of regenerated cells depends on Notch signaling (14).
The pseudostratified epithelium contains uncommon cell types, including pulmonary neuroendocrine cells (PNECs), tuft cells, and ionocytes (15). PNECs comprise approximately 1% of the airway epithelium, where they are the only innervated cell type. They manifest in clusters known as neuroepithelial bodies in mouse lungs. PNECs function as sensory cells by secreting neuropeptides (e.g., calcitonin gene-related peptide), neurotransmitters (e.g., serotonin), and bombesin-related peptides (e.g., neuromedin B) in response to changes in oxygen levels (16). PNECs also serve as a modulator in the immune responses to allergens and in tissue remodeling (16). Tuft cells are referred to by different names, depending on the organs in which they are present: brush cells in the airway, microvillous cells in the nasopharyngeal cavity, and multivesicular caveolated cells in the intestine (17). Tuft cells found in the lung specifically express type II taste receptors and bitter taste receptors; activation of the former promotes the release of antimicrobial peptides from neighboring ciliated cells by modulating Ca2+ influx. Ionocytes are major expressers of cystic fibrosis transmembrane conductor regulator and contribute to the regulation of mucus production (18). Submucosal glands and cartilaginous rings control airway function in the lower respiratory tract (15). Various cell types line the submucosal glands, including ciliated, goblet, serous, and myoepithelial cells; these cells secrete mucus and host defense proteins in response to pathogens and toxic substances.
The distal region of the small airways contains the alveolar sacs, where oxygen–carbon dioxide exchange occurs, and is hence referred to as the respiratory zone. The alveolar epithelium comprises two major epithelial lineages: alveolar type (AT) 1 and 2 cells. AT1 cells are thin and elongated and cover >95% of the alveolar surface of the adult lung (19). AT1 cells are associated with pulmonary capillary epithelial cells and mesenchymal cells to form a thin, diffusible gas exchange interface. AT2 cells are cuboidal epithelial cells and can be distinguished by their lipid-rich lamellar bodies containing surfactant proteins (SPs), such as ATP-binding cassette class A3 and SPs A–D (20). SPs reduce the surface tension of the epithelium and prevent atelectasis during respiration. AT2 cells act as alveolar epithelial progenitors when they detect the Wnt signal released from fibroblasts; in a steady-state condition, Wnt-responsive AT2 cells can self-renew and differentiate into AT1 cells, a process that is regulated by bone morphogenetic protein signaling (21). The alveolar structure is supported by the extracellular matrix produced from interstitial fibroblasts, such as Axin2-positive myogenic precursors, Wnt2-expressing platelet-derived growth factor-α-positive cells, and mesenchymal alveolar niche cells.
Cellular components of the gastrointestinal system
The gastrointestinal tract has a continuous tube structure and, unlike the respiratory tract, displays regionally distinctive anatomical features, such as in the mouth, pharynx, esophagus, stomach, small intestine, large intestine, and anus (Fig. 1B). The gastrointestinal tract is organized with crypt-villus structures; villi are the finger-like projections found within the intestinal wall, and crypts comprise the invaginated structures between villi (22). Villi extend along the surface area of the digestively active epithelium, mainly in the small intestine. The length of the villi decreases along the small intestinal tract, and the small intestine is subdivided into three segments according to villus length: the duodenum, jejunum, and ileum, in descending order. In contrast, the large intestine has a flat epithelial surface interspaced by crypts. The large intestine is subdivided into the caecum, proximal colon, transverse colon, distal colon, and rectum, in descending order (22).
The layers of intestinal epithelial cells (IECs) can be categorized by their primary functions; columnar epithelial and microfold (M) cells are primarily involved in absorption, whereas Paneth, goblet, enteroendocrine, and tuft cells are involved in secretion. All IECs are derived from crypt base columnar (CBC) cells, known as intestinal stem cells, for which Lgr5 is a specific marker (23). The Lgr5+ CBC cells located inside the crypt differentiate into multiple lineages of cells and self-renew for long-term maintenance (24). Notch signals promote the differentiation of CBC cells into absorptive progenitor cells, which rapidly proliferate and maturate to enterocytes and M cells, as induced by bone morphogenetic protein and receptor activator of NF-κB ligand signaling, respectively (25,26). Columnar epithelial cells, known as enterocytes, are the predominant cell type that absorbs digested nutrients in the small intestine. Enterocytes also play an essential role in maintaining mucosal homeostasis by regulating mucosal integrity and crosstalk among immune cells, including DCs and intraepithelial lymphocytes (27). The M cells located in the follicle-associated epithelium (FAE) of GALTs are specialized in the uptake of luminal Ags (28). M cells are recognized by their unique morphology, which constitutes short, irregular microvilli and an intraepithelial pocket containing various leukocytes (29). M cells can also be identified by monoclonal Abs specific to α (1,2)-fucose-containing carbohydrate moieties or by proteins expressed specifically on the apical surface of M cells, such as glycosylphosphatidylinositol-anchor protein 2 (GP2) and complement C5a receptor (C5aR) (30,31). M cells take up luminal Ags but are also utilized as an infection route by many pathogens, such as Salmonella typhimurium, Yersinia enterocolitica, and Listeria monocytogenes (29).
Secretory progenitor cells mature into Paneth, goblet, enteroendocrine, and tuft cells when they detect Wnt and other unidentified signals (23). Paneth cells are observed only in the small intestine and are concentrated mainly within the crypts of the terminal ileum. Paneth cells secrete various antimicrobial proteins, such as α-defensin, lysozymes, and C-type lectins (32). Additionally, they control crypt stem cell activity by secreting epidermal growth factor and Wnt3 and by expressing Notch ligand Delta-like 4 (33). Unlike Paneth cells, the frequency of mucin-secreting goblet cells in the lower tract increases towards the colon (34). The small intestine is covered by a loose layer of mucus known as glycocalyx; the colon also contains glycocalyx, as well as a denser mucosal layer underneath. The major component of intestinal mucus is mucin 2, a lack of which induces spontaneous colitis by allowing direct contact of IECs with bacteria (35). Another secretory product of goblet cell is small protease-resistant trefoil factor 3, which binds to the cysteine-rich domain of mucin 2 and influences the viscosity of mucus (36).
Hormone-producing enteroendocrine cells are distributed throughout the gut mucosa in the crypts and villi, but they only constitute 1% of the total gut epithelial cell population (37). Enteroendocrine cells comprise several subgroups showing regional differences, and their primary function is to orchestrate responses to ingested nutrients by secreting individual hormone peptides in the gut mucosa (38). I and K cells present in the jejunum secrete cholecystokinin and gastric inhibitory peptide, respectively, along with 5-hydroxytryptamine (5-HT, serotonin). L cells are present in the ileum and colon, where they secrete glucagon-like peptides 1 and 2 and polypeptide YY. Enterochromaffin cells, the most abundant enteroendocrine cell type, are distributed throughout both the small and large intestines and secrete 5-HT. Enteroendocrine cells play an essential role in gut sensing via the expression of various receptors, such as G protein-coupled receptors 40, 41, and 43, TLRs 1, 2, and 4, and taste receptors (types I and II). Tuft cells comprise approximately 0.4% of IECs and are characterized by their bottle-shaped morphology, apical microvilli, and the expression of transient receptor potential cation channel subfamily M member 5 (39). Tuft cells are the sole producers of IL-25, which promotes type 2 immune responses and intestinal remodeling via the activation of ILC2s (40). Collectively, these epithelial cells actively produce a mucosal barrier to block the invasion of luminal Ags and pathogens.
Cellular crosstalk between epithelial cells and immune cells in the lung and gut
Under steady-state conditions, AT2 cells are the primary source of colony-stimulating factor 2 (CSF2) and IL-33 in the lung, which play critical roles in lung-specific imprinting of pulmonary basophils and in stimulating ILC2s to produce CSF2 and IL-13 (41). CSF2 is a critical modulator of differentiation and/or maturation of alveolar macrophages (AMs) from fetal liver embryonic precursors or immature AMs (42). AMs reside in the alveolar lumen, where they clear surfactants and act as immune modulators. CSF2 signaling regulates tissue-specific differentiation of AMs by inducing the master transcription factor peroxisome proliferator-activated receptor gamma, which is a key regulator of lipid metabolism (43). AMs express TGF-β, which prevents unnecessary immune activation (44). Human AMs share common surface markers with lung macrophages, such as HLA-DR, CD11b, CD11c, and CD64; they can be distinguished from lung macrophages by examining autofluorescence and detecting the expression of CD206, CD169, and MARCO (45). Interstitial macrophages reside in the space between the lung epithelium and capillaries. They consist of two main populations: LYVE-1lowMHC IIhigh and LYVE-1highMHC IIlow cells. LYVE-1lowMHC IIhigh cells are located close to neurons and are specialized in Ag presentation (46). LYVE-1highMHC IIlow perivascular macrophages are functionally involved in wound healing and tissue repair.
Under steady-state conditions, myeloid cells in the small intestine express IL-1β, IL-6, and IL-23 (47). The adhesion of segmented filamentous bacteria to IECs induces the release of serum amyloid A, which triggers the expression of IL-1β and IL-23 in DCs (48). These cytokines promote Th17 cell differentiation and activation of group 3 innate lymphoid cells. Regenerating islet-derived protein 3γ also promotes IEC repair (49). Mucin production in goblet cells is increased via the IL-22-signal transducer and activator of transcription 3 axis (50). Tuft cells constitutively express IL-25, which induces ILC2 activation, resulting in IL-5, IL-9, and IL-13 secretion. IL-13 triggers the differentiation of epithelial cells into goblet and tuft cells, causing a feedback loop (40). In the large intestine, enteroendocrine L cells express glucagon-like peptide-2, which inhibits colonic crypt cell apoptosis and increases crypt depth and colon length (51). In addition, bacterial metabolites, including butyrate, trigger the release of 5-HT, which plays critical roles in enteric nervous system development, gut motility, T cell activation, and eosinophil migration (52).
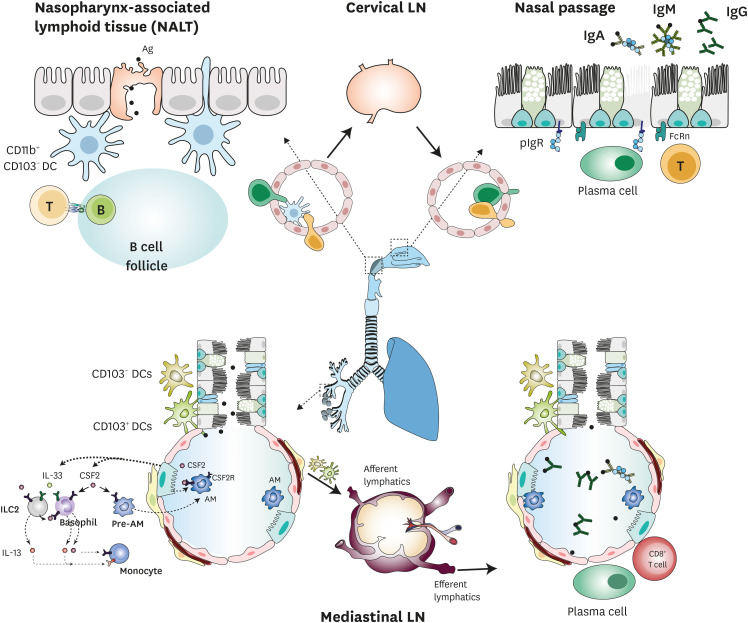
INDUCTION AND REGULATION OF MUCOSAL IMMUNE RESPONSES IN THE RESPIRATORY SYSTEM
IgA is the most abundant Ab in the upper respiratory tract, whereas IgG is dominant in the lower respiratory tract (53). NALT is a mucosal immune inductive site in the upper respiratory tract that is composed of several cell types and structures, including FAE cells, M cells, B cell follicles containing uncommitted (IgD+ and IgM+) B cells, T cell areas with DC enrichment, and high endothelial venules (54). Following initial Ag exposure in NALT, the germinal center (GC) is induced; nasal DCs take up Ags and migrate into CLNs, which are also immune inductive sites (Fig. 2). Nasal DCs encounter Ags via their dendrites or M cells, which are specialized epithelial cells that take up luminal Ags via pinocytosis and endocytosis. Effector cells, including Ag-specific IgA+ B cells, move to the nasal passage, which is a mucosal effector site. The nasal passage epithelium consists of multiciliated cells and mucus-producing goblet cells (55). In the nasal passage, mucosal Abs, including SIgA and IgG, are secreted via specific receptors, pIgR and FcRn, respectively. IgM−IgD+ plasma cells undergo IgM-to-IgD class switch recombination (CSR) in NALT; this process is rare or absent in systemic lymphoid tissues (8,56).
Figure 2.
Induction of mucosal immune responses in the respiratory tract. In the NALT, nasal DCs take up Ags via M cells and their dendrites, and then migrate to B cell follicles and CLNs. Ag-specific effector cells are recruited to the nasal passage, where they secrete Ag-specific IgG, IgA, and IgM. In the lower respiratory tract, Ag-stimulated DCs migrate to mediastinal LNs and initiate the Ag-specific immune response via activation of naïve T cells. Effector cells then home to alveolar sacs.
Under steady-state conditions, murine nasal DCs consist of CD11c+MHCII+CD103+CD11b+ (CD103+CD11b+), CD11c+MHCII+CD103-CD11b+ (CD103−CD11b+), and CD11c+MHCII+CD103+CD11b− (CD103+ CD11b−) cells. CD103+CD11b+ DCs predominantly reside in the nasal passage, whereas CD103−CD11b+ DCs are located mostly in the FAE of NALT (57). After nasal immunization or pathogenic infection, nasal DCs, especially CD103−CD11b+ cells, rapidly migrate into CLNs and induce T cell priming (54,58). Under steady-state conditions, the DCs of human nasopharyngeal tissue are composed of both major BDCA-1+ cells and minor BDCA-3high cells; reduced levels of these cells are found in patients with chronic rhinosinusitis (57).
In the lower respiratory tract, immunological events occur mainly in bronchi and bronchioles, in which the interstitium contains various immune cells such as DCs, mast cells, and ILCs. Conventional DCs (cDCs) in the lung consist of CD11bhighCD103−CD11c+SIRPα+ cells (cDC2) and CD11b−CD11c+Langerin+CD103+ cells (cDC1), which are primed for Ag uptake due to their immature states (59). CD103+ DCs located below the bronchial epithelium extend their dendrites into the airway lumen via formation of tight junctions with epithelial cells (60). Following the uptake of inhaled Ags, CD103+ DCs are stimulated by alarmins, including thymic stromal lymphopoietin and IL-25. Maturated CD103+ DCs then migrate to mediastinal LNs and initiate Ag-specific immune responses via activation of naïve T cells. CD11bhighCD103− cells are required for the induction of Ag-specific CD8+ T cell priming (61). For example, during an influenza infection, only CD11bhighCD103- cells can efficiently process and present Ags to MHC class I receptors in the lung. After migration, CD11bhighCD103- cells then cross-prime CD8+ T cells in the mediastinal LN. In the conducting airways, plasmacytoid DCs, defined by the expression of CD11c, B220, and plasmacytoid DC Ag-1, produce type I IFNs in response to viral infection and modulate regulatory T cells for lung homeostatic maintenance (62).
INDUCTION AND REGULATION OF MUCOSAL ABS IN THE GASTROINTESTINAL SYSTEM
Introduction of luminal Ags into the gastrointestinal immune system
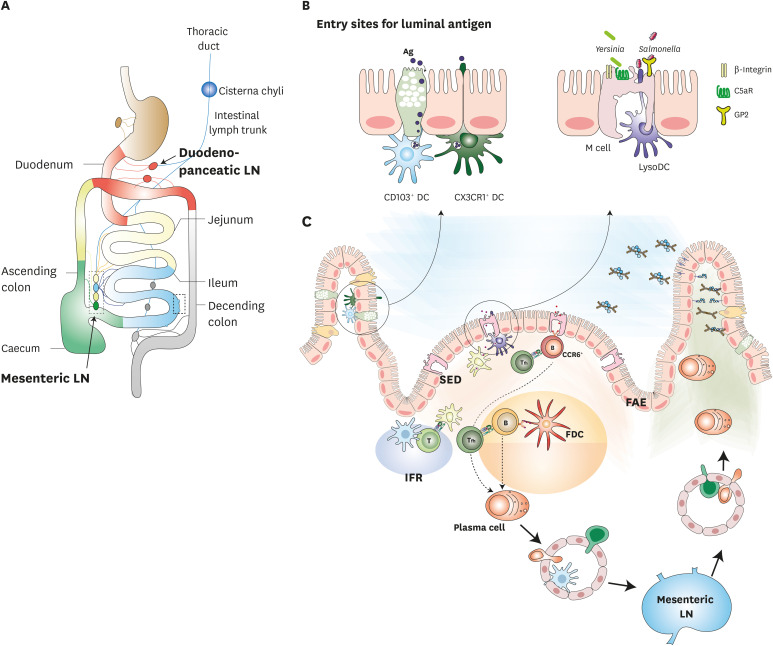
The gastrointestinal immune system consists of GALT and LP. Since luminal Ag influx is tightly regulated by IECs, introduction of luminal Ags for priming Ag-specific adaptive immunity occurs primarily in M-cell-containing GALTs (27). Examples of GALTs include Peyer's patches (PPs), solitary isolated lymphoid tissues (SILTs), cecal patches, and colonic patches (1,22). These lymphoid tissues have different distributions across the gut segments; PPs are abundant in the terminal ileum but scarce in the duodenum. In the large intestine, cecal patches and colonic patches, which are lymphoid structures similar to PPs, are found in the appendix and in the colon and rectum, respectively (63). SILTs observed throughout the intestine contain cryptopatches, in which isolated lymphoid follicles mature (64). The distribution of mature SILTs is correlated with bacterial burden; in humans, isolated lymphoid follicles are concentrated in the ileum and rectosigmoid colon (65). Each regional lymph of the gastrointestinal mucosa, including regional GALT, drains along the length of the mucosa and flows through the thoracic duct into the blood circulation (22). For example, lymph from the duodenum of the small intestine and the traverse colon drains into duodenopancreatic LNs embedded in pancreatic tissue; lymph from the jejunum drains to the middle MLNs, and lymph from the ileum, caecum, and ascending colon collects in the distal segments of the MLNs (Fig. 3A). Given the differences in cellular components and environment along the length of the intestine, each draining LN conducts regional tissue-specific adaptive immune responses.
Figure 3.
Induction of mucosal immune responses in the gastrointestinal tract. (A) Lymph from mucosal lymphatics collects for transport to the draining LNs. (B) Luminal Ags and pathogens, such as Yersinia and Salmonella, can be delivered to PP by M cells. This is facilitated by GP2, C5aR, and integrin β1. Close to the M cells, Ags encounter lysozyme-expressing DCs. Luminal soluble Ags can be also transported into the LP via both the goblet cell-associated Ag passages of goblet cells and extending dendrites from CX3CR1+ cells. (C) In PPs, the Ag-specific immune response was initiated in the GC, SED of PPs, and MLNs. Ag-specific effector cells then home to LP.
PPs are the best-characterized GALTs (66). PPs are separated from the lumen by FAE, which contains a limited number of goblet and Paneth cells and creates a thin mucus layer containing antimicrobial peptides. In the subepithelial dome (SED), MHChighCD11highCD11b+CD8a− cells inhibit the expression of Axin2-positive myogenic precursor by secreting IL-22 binding protein, which reduces the level of circulating IL-22 (67,68). This environment allows luminal Ags to access M-cell-containing FAE. In the M cells, the transport of luminal Ags is facilitated by transport receptors, such as GP2, C5aR, integrin β1, and CD155 poliovirus receptor; these receptors are capable of binding whole luminal bacteria and soluble Ags (Fig. 3B) (27,31,69,70). For example, GP2 interacts with FimH of type I piliated bacteria, such as Escherichia coli and S. typhimurium, and can transport them into PPs (31). C5aR interacts with outer membrane protein H of Y. enterocolitica (69). Ags conjugated to M-cell-specific Ab (NKM 16-2-4), anti-GP2 Ab, or C5aR ligand are transcytosed via M cells, which can then induce Ag-specific immune responses (71,72). Lysozyme-expressing DCs that are localized to M cells extend their dendrites through M-cell-specific transcellular pores to the lumen, where they can take up luminal pathogens such as S. typhimurium (73).
In other LNs, Ags and soluble molecules flow from the afferent lymphatics into the LN parenchyma through a conduit network consisting of fibroblastic reticular cells and their specialized collagen fibers (74). However, Ag influx into PPs mainly depends on M cells because PPs do not contain afferent lymphatics (27). Interestingly, a recent study reported a specialized conduit system in PPs (75). Intestinal fluid absorption occurs due to the local osmotic gradient via ion channels, after which the fluid flows from SED to the follicle and interfollicular regions (IFRs) of PPs. In this study, 14 kDa hen egg lysozyme labeled with Alexa Fluor 488 was shown to rapidly penetrate PPs and flow along the conduit network in explanted intestinal loops. Although the mechanistic link between conduit flow and immune induction remains unknown, disruption of the conduit flow has been linked to an impaired mucosal Ab response. Therefore, these observations suggest that regulation of Ag delivery within PPs is closely related to Ag-specific mucosal immune induction.
The LP underlying the intestinal villi is an immune effector site. Soluble Ags from the lumen can be delivered into the LP via goblet-cell-associated Ag passages and the extended dendrites of CX3CR1+ cells (Fig. 3B) (76). In the LP, the Ags encounter CD103+ DCs either directly or via connexin 43-expressing gap junctions. CD103+ DCs that have taken up Ags migrate to MLNs in a CCR7-dependent manner to induce tolerance to the Ags (77).
Induction of IgA responses in the gastrointestinal tract
Once Ags have translocated into PPs, they encounter the SED environment, which is a niche located between the FAE and B cell follicles. The SED contains double-negative cDCs, lysozyme-expressing DCs, macrophages, T cells, and B cells (78). Current evidence suggests that T-cell-dependent IgA induction is initiated following the cognate interaction between DCs and follicular helper T (Tfh) cells in the IFR of PPs (Fig. 3C). SED-localized DCs likely drive the initiation of Ag-specific immune responses, because their primary function is to capture translocated luminal bacteria, such as E. coli, SIgA-coated Shigella flexneri, and S. typhimurium (79). In addition, DCs bearing Ags or DCs stimulated by TLR7 ligands were reported to move from the SED into the IFR of PPs (80). Nevertheless, the mechanism by which Ags move from the SED to B cell follicles is poorly understood.
Recent studies showed that the early IgA response occurs without clonal selection in CCR6+ B cells of the SED. This is in contrast to other LNs, in which B cell clones that exhibit low affinity to Ags fail to survive, and high-affinity Ag receptor-expressing B cell clones are preferentially selected for differentiation into early plasmablasts in GCs (81,82). CCR6+ B cells localized to the SED generally encounter Ags that have been transcytosed by M cells. They then initiate CSR to IgA in response to cognate Ag stimulation without clonal selection; this process occurs after the expression of activation-induced cytidine deaminases in CCR6+ B cells. Furthermore, low-affinity B cell clones extensively proliferate without any competition in a T-cell-dependent manner within the SED, even though some CD4+ T cells in the SED are Tfh cells related to B cell clonal selection via T cell receptor–peptide–MHC class II interactions (83,84). However, low-affinity B cell clones fail to enter the pre-existing GCs; only high-affinity B cell clones are preferentially selected, after which they expand and undergo somatic hypermutation in pre-existing GCs of PPs.
PP GCs spontaneously arise during homeostatic response and continuously exist (85). In the GCs of peripheral LNs, follicular DCs (FDCs) present Ags as part of immune complexes to select for high-affinity B cells (86). It is currently unclear whether FDCs are necessary for the selection of high-affinity IgA-expressing B cell clones in PPs. FDCs are likely involved in the IgA response during GC reactions, as reports have shown that IgA deposition follows the distribution of the FDC network. In steady-state PPs, FDCs that have been stimulated by TLR and retinoic acid receptor signaling express chemokines and survival factors, which facilitate IgA B cell differentiation (78,87). In addition, a cathelin-related antimicrobial peptide contributes to FDC stimulation, which in turn enhances IgA B cell differentiation (88). Following GC reactions, selected plasma precursor cells migrate through the lymph, which drains along the length of the mucosa into specific draining LNs. The plasma precursor cells then flow through the thoracic lymph duct into the blood circulation, after which they can home to the LP of the small and large intestines (8). This homing process is regulated by specific receptors. The microenvironment of PPs induces plasmablasts to express α4β7, CCR9, and CCR10, which target the plasmablasts to the small and large intestine (89). In addition, mucosal memory cells and long-lived plasma cells were found in mice after infection and oral immunization. IgA+ memory B cells can be characterized by their expression of IL-17 receptor C, IL-22 receptor subunit α2, α4β7, CCR9, and CCR10 (90). However, the generation and maintenance of IgA+ memory B cells are not clearly understood. In addition to the T-dependent pathway, gut IgA can be generated by the T-independent pathway. The T-independent pathway is induced by the innate signaling of TLR ligands, a proliferation-inducing ligand, and B cell activation factor. A recent study reported that intestinal epithelial endoplasmic reticulum stress induces peritoneal B1b cells to differentiate into gut-homing IgA+ plasma cells (91). These findings suggest that B cell responses induced by T-cell-dependent and -independent pathways may differ in their origin and activation signals.
Other Ab responses in the gastrointestinal tract
Cooperation between SIgM and SIgA improves the prevention of bacterial dissemination (8). For example, the oral administration of S. typhimurium coated with SIgM and SIgA reduces mucosal infection and systemic dissemination of the pathogen. IgM-secreting plasma cells are observed mainly in the terminal ileum of humans, where they constitute 10%–20% of total plasma cells. In the gut, IgM+IgD−CD27+ memory B cells can undergo IgA CSR in response to T-cell-dependent and -independent pathways; this strategy enables a rapid response to microbial infection. Additionally, commensal microbe-specific IgG is detected in intestinal mucosa and peripheral blood. The presence of the commensal bacterium Akkermansia muciniphila in mucus can activate bacteria-specific Tfh cells, resulting in the production of specific IgG1 in the gut (92). Furthermore, highly protective levels of IgG were identified in mice infected with Citrobacter rodentium (93). Pathogen-specific IgG, but not IgA or IgM, is necessary to eliminate pathogens from the intestinal mucosa, as IgG-coated pathogens are subsequently killed by neutrophils in the intestinal lumen.
HOMEOSTATIC MAINTENANCE AND BREAKDOWN OF MUCOSAL FIREWALLS
Respiratory pathogen infections vary in their severity, from mild common colds to deadly pandemics. Recently, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused a global pandemic, known as coronavirus disease 2019 (COVID-19) (94). SARS-CoV-2 utilizes host receptors to enter into cells, namely human angiotensin-converting enzyme 2 (ACE2) and type II transmembrane serine protease (TMPRSS2). Several single-cell RNA sequencing reports suggest that ACE2+TMPRSS2+ cells include ciliated and goblet cells in the nasal epithelium, AT2 cells in alveoli, and enterocytes in the ileum and colon (95,96). In addition, SARS-CoV-2 infection was detected in ciliated cells and AT2 cells in autopsied lungs using RNA in situ hybridization. Given that the role of AT2 cells is closely associated with alveolar regeneration, damage to AT2 cells by viral infection may lead to acute alveolar damage (97). Although the immune response to SARS-CoV-2 has not yet been fully elucidated, it can be modelled using studies from other respiratory viruses, including SARS-CoV (Fig. 4). In the alveoli, SARS-CoV-2 infection in AT2 cells induces pyroptosis, which triggers the generation of pro-inflammatory cytokines from neighboring epithelial cells, endothelial cells, and AMs. The cytokines promote the recruitment of monocytes, macrophages, and T cells to the infected area, which then cause further inflammation. The attraction of virus-specific CD8+ T cells facilitates the elimination of virus-infected cells, thus blocking further spread of the virus. Neutralizing Abs also inhibit viral infection and trigger AM phagocytosis of neutralized viral particles. These immune responses can clear the virus while causing only mild lung damage. Consequently, the level of adaptive immunity determines the severity of the disease. In contrast, hyperaccumulation of immune cells promotes excessive infiltration of mononuclear phagocytes, which can in turn induce a systemic cytokine storm, pulmonary edema, and pneumonia; the result is widespread inflammation and multi-organ damage.
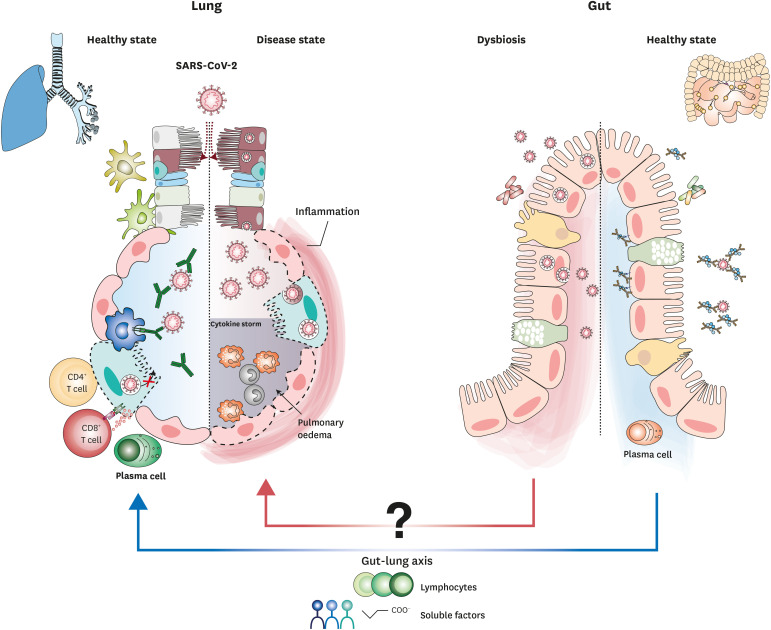
Figure 4.
Hypothetical immunity in the lung and gut during SARS-CoV-2 infection. SARS-CoV-2 infects both ACE2- and TMPRSS2-expressing epithelial cells, including ciliated cells, AT2 cells, and enterocytes. In mucosal compartments, induction of the adaptive immune response can promote viral clearance.
In addition to severe respiratory symptoms, some COVID-19 patients also develop gastrointestinal symptoms (94). Recent data suggest that SARS-CoV-2 targets ACE2+TMPRSS2+ enterocytes, which also reside in the intestine; thus, the gut is likely to be a target organ for SARS-CoV-2 infection. SARS-CoV-2 has been shown to infect, replicate, and produce infectious viral particles in human epithelial cells and human small intestinal organoids (98). Given that ACE2 expression is decreased upon SARS-CoV binding, reduced ACE2 expression is also expected during SARS-CoV-2 infection. ACE2 dysfunction caused by decreased ACE2 expression may also affect the composition of the gut microbiota by suppressing the expression of neutral amino acid transporters in IECs, thereby decreasing nicotinamide levels (99). Therefore, ACE2 dysfunction during SARS-CoV-2 infection may be sufficient to alter the composition of the gut microbiota, as COVID-19 patients show a change in gut microbiota composition to increased opportunistic pathogens and often have decreased levels of butyrate-producing bacteria (99,100). While the impact of COVID-19 on gut disorders remains unclear, evidence suggests that COVID-19 influences the systemic dissemination of bacteria, endotoxins, and microbial metabolites. Additionally, it may trigger a systemic cytokine storm and multiorgan dysfunction. Therefore, we hypothesize that the effects of the gut microbiota on lung immunity may mediate the effects of COVID-19 on the gut-lung axis (Fig. 4). Additionally, we suggest that protective immune response against SARS-CoV-2 in the gut may be able to play an important role in controlling the pathogenesis of COVID-19.
CONCLUDING REMARKS
In this review, we summarize the cellular components of the lung and gut. We also describe their crosstalk in Ag-specific immune responses, and the implications thereof for vaccine development in terms of the route of vaccine administration. Ag-specific immune responses in the mucosal compartment are particularly important for protecting against mucosal pathogens, including SARS-CoV-2, since Ab can block viral entry to the mucosal compartment. Although parenteral vaccination can induce protective IgG at the respiratory mucosa, mucosal immunization through the nasopharyngeal route can induce potent T cell and IgA responses in mucosal compartments, including the upper respiratory tract. Given that the currently available mucosal vaccines contain live-attenuated viruses, the development of a mucosal vaccine for COVID-19 may be challenging. Furthermore, weakly immunogenic vaccines, such as protein subunit vaccines, cannot be administered via the nasopharyngeal route due to the lack of safe adjuvants. Therefore, future studies are required to optimize currently available live-attenuated vaccines and mucosal adjuvants.
ACKNOWLEDGEMENTS
This study was supported by grants from the Basic Science Research Programs (NRF-2019R1A2C2004711) through the National Research Foundation, funded by Korean Ministry of Science and ICT, and by the Basic Science Research Program through the NRF, funded by the Ministry of Education (2017R1A6A1A03015876). Dr. Yong-Suk Jang was supported by the Research Base Construction Fund Support Program funded by Jeonbuk National University in 2020.
Abbreviations
- ACE2
angiotensin-converting enzyme 2
- AM
alveolar macrophage
- AT
alveolar type
- C5aR
complement C5a receptor
- CBC
crypt base columnar
- cDC
conventional dendritic cell
- CLN
cervical lymph node
- COVID-19
coronavirus disease 2019
- CSF2
colony-stimulating factor 2
- CSR
class switch recombination
- DC
dendritic cell
- FAE
follicle-associated epithelium
- FcRn
neonatal Fc receptor
- FDC
follicular dendritic cell
- GALT
gut-associated lymphoid tissue
- GC
germinal center
- GP2
glycosylphosphatidylinositol-anchor protein 2
- 5-HT
5-hydroxytryptamine
- IEC
intestinal epithelial cell
- IFR
interfollicular region
- ILC2
type 2 innate lymphoid cell
- LN
lymph node
- LP
lamina propria
- M
microfold
- MALT
mucosa-associated lymphoid tissue
- MLN
mesenteric lymph node
- NALT
nasopharynx-associated lymphoid tissue
- pIgR
polymeric Ig receptor
- PNEC
pulmonary neuroendocrine cell
- PP
Peyer's patch
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2
- SED
subepithelial dome
- SIgA
secretory IgA
- SIgM
secretory IgM
- SILT
solitary isolated lymphoid tissue
- SMG
submucosal gland
- SP
surfactant protein
- Tfh
follicular helper T
- TMPRSS2
type II transmembrane serine protease
Footnotes
Conflict of Interest: The authors declare no potential conflicts of interest.
- Conceptualization: Jang YS, Kim SH.
- Data curation: Kim SH, Jang YS.
- Formal analysis: Jang YS, Kim SH.
- Funding acquisition: Jang YS.
- Investigation: Kim SH, Jang YS.
- Project administration: Jang YS.
- Supervision: Jang YS.
- Validation: Jang YS.
- Visualization: Kim SH, Jang YS.
- Writing - original draft: Kim SH.
- Writing - review & editing: Jang YS.
References
- 1.Brandtzaeg P, Kiyono H, Pabst R, Russell MW. Terminology: nomenclature of mucosa-associated lymphoid tissue. Mucosal Immunol. 2008;1:31–37. doi: 10.1038/mi.2007.9. [DOI] [PubMed] [Google Scholar]
- 2.Macpherson AJ, McCoy KD, Johansen FE, Brandtzaeg P. The immune geography of IgA induction and function. Mucosal Immunol. 2008;1:11–22. doi: 10.1038/mi.2007.6. [DOI] [PubMed] [Google Scholar]
- 3.Phalipon A, Corthésy B. Novel functions of the polymeric Ig receptor: well beyond transport of immunoglobulins. Trends Immunol. 2003;24:55–58. doi: 10.1016/s1471-4906(02)00031-5. [DOI] [PubMed] [Google Scholar]
- 4.Michaud E, Mastrandrea C, Rochereau N, Paul S. Human secretory IgM: an elusive player in mucosal immunity. Trends Immunol. 2020;41:141–156. doi: 10.1016/j.it.2019.12.005. [DOI] [PubMed] [Google Scholar]
- 5.Heron M, Grutters JC, ten Dam-Molenkamp KM, Hijdra D, van Heugten-Roeling A, Claessen AM, Ruven HJ, van den Bosch JM, van Velzen-Blad H. Bronchoalveolar lavage cell pattern from healthy human lung. Clin Exp Immunol. 2012;167:523–531. doi: 10.1111/j.1365-2249.2011.04529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pyzik M, Sand KMK, Hubbard JJ, Andersen JT, Sandlie I, Blumberg RS. The neonatal Fc receptor (FcRn): a misnomer? Front Immunol. 2019;10:1540. doi: 10.3389/fimmu.2019.01540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen K, Cerutti A. New insights into the enigma of immunoglobulin D. Immunol Rev. 2010;237:160–179. doi: 10.1111/j.1600-065X.2010.00929.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen K, Magri G, Grasset EK, Cerutti A. Rethinking mucosal antibody responses: IgM, IgG and IgD join IgA. Nat Rev Immunol. 2020;20:427–441. doi: 10.1038/s41577-019-0261-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Man WH, de Steenhuijsen Piters WA, Bogaert D. The microbiota of the respiratory tract: gatekeeper to respiratory health. Nat Rev Microbiol. 2017;15:259–270. doi: 10.1038/nrmicro.2017.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rackley CR, Stripp BR. Building and maintaining the epithelium of the lung. J Clin Invest. 2012;122:2724–2730. doi: 10.1172/JCI60519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nanjundappa R, Kong D, Shim K, Stearns T, Brody SL, Loncarek J, Mahjoub MR. Regulation of cilia abundance in multiciliated cells. Elife. 2019;8:e44039. doi: 10.7554/eLife.44039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stripp BR, Reynolds SD, Boe IM, Lund J, Power JH, Coppens JT, Wong V, Reynolds PR, Plopper CG. Clara cell secretory protein deficiency alters Clara cell secretory apparatus and the protein composition of airway lining fluid. Am J Respir Cell Mol Biol. 2002;27:170–178. doi: 10.1165/ajrcmb.27.2.200200270c. [DOI] [PubMed] [Google Scholar]
- 13.Rock JR, Onaitis MW, Rawlins EL, Lu Y, Clark CP, Xue Y, Randell SH, Hogan BL. Basal cells as stem cells of the mouse trachea and human airway epithelium. Proc Natl Acad Sci U S A. 2009;106:12771–12775. doi: 10.1073/pnas.0906850106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rock JR, Gao X, Xue Y, Randell SH, Kong YY, Hogan BL. Notch-dependent differentiation of adult airway basal stem cells. Cell Stem Cell. 2011;8:639–648. doi: 10.1016/j.stem.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zepp JA, Morrisey EE. Cellular crosstalk in the development and regeneration of the respiratory system. Nat Rev Mol Cell Biol. 2019;20:551–566. doi: 10.1038/s41580-019-0141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Branchfield K, Nantie L, Verheyden JM, Sui P, Wienhold MD, Sun X. Pulmonary neuroendocrine cells function as airway sensors to control lung immune response. Science. 2016;351:707–710. doi: 10.1126/science.aad7969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schneider C, O'Leary CE, Locksley RM. Regulation of immune responses by tuft cells. Nat Rev Immunol. 2019;19:584–593. doi: 10.1038/s41577-019-0176-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Plasschaert LW, Žilionis R, Choo-Wing R, Savova V, Knehr J, Roma G, Klein AM, Jaffe AB. A single-cell atlas of the airway epithelium reveals the CFTR-rich pulmonary ionocyte. Nature. 2018;560:377–381. doi: 10.1038/s41586-018-0394-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whitsett JA, Alenghat T. Respiratory epithelial cells orchestrate pulmonary innate immunity. Nat Immunol. 2015;16:27–35. doi: 10.1038/ni.3045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walker SR, Williams MC, Benson B. Immunocytochemical localization of the major surfactant apoproteins in type II cells, Clara cells, and alveolar macrophages of rat lung. J Histochem Cytochem. 1986;34:1137–1148. doi: 10.1177/34.9.2426341. [DOI] [PubMed] [Google Scholar]
- 21.Barkauskas CE, Cronce MJ, Rackley CR, Bowie EJ, Keene DR, Stripp BR, Randell SH, Noble PW, Hogan BL. Type 2 alveolar cells are stem cells in adult lung. J Clin Invest. 2013;123:3025–3036. doi: 10.1172/JCI68782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mowat AM, Agace WW. Regional specialization within the intestinal immune system. Nat Rev Immunol. 2014;14:667–685. doi: 10.1038/nri3738. [DOI] [PubMed] [Google Scholar]
- 23.Gehart H, Clevers H. Tales from the crypt: new insights into intestinal stem cells. Nat Rev Gastroenterol Hepatol. 2019;16:19–34. doi: 10.1038/s41575-018-0081-y. [DOI] [PubMed] [Google Scholar]
- 24.Barker N, van Es JH, Kuipers J, Kujala P, van den Born M, Cozijnsen M, Haegebarth A, Korving J, Begthel H, Peters PJ, et al. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature. 2007;449:1003–1007. doi: 10.1038/nature06196. [DOI] [PubMed] [Google Scholar]
- 25.Shroyer NF, Helmrath MA, Wang VY, Antalffy B, Henning SJ, Zoghbi HY. Intestine-specific ablation of mouse atonal homolog 1 (Math1) reveals a role in cellular homeostasis. Gastroenterology. 2007;132:2478–2488. doi: 10.1053/j.gastro.2007.03.047. [DOI] [PubMed] [Google Scholar]
- 26.Knoop KA, Kumar N, Butler BR, Sakthivel SK, Taylor RT, Nochi T, Akiba H, Yagita H, Kiyono H, Williams IR. RANKL is necessary and sufficient to initiate development of antigen-sampling M cells in the intestinal epithelium. J Immunol. 2009;183:5738–5747. doi: 10.4049/jimmunol.0901563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kurashima Y, Kiyono H. Mucosal ecological network of epithelium and immune cells for gut homeostasis and tissue healing. Annu Rev Immunol. 2017;35:119–147. doi: 10.1146/annurev-immunol-051116-052424. [DOI] [PubMed] [Google Scholar]
- 28.Owen RL, Jones AL. Epithelial cell specialization within human Peyer's patches: an ultrastructural study of intestinal lymphoid follicles. Gastroenterology. 1974;66:189–203. [PubMed] [Google Scholar]
- 29.Mabbott NA, Donaldson DS, Ohno H, Williams IR, Mahajan A. Microfold (M) cells: important immunosurveillance posts in the intestinal epithelium. Mucosal Immunol. 2013;6:666–677. doi: 10.1038/mi.2013.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim SH, Seo KW, Kim J, Lee KY, Jang YS. The M cell-targeting ligand promotes antigen delivery and induces antigen-specific immune responses in mucosal vaccination. J Immunol. 2010;185:5787–5795. doi: 10.4049/jimmunol.0903184. [DOI] [PubMed] [Google Scholar]
- 31.Hase K, Kawano K, Nochi T, Pontes GS, Fukuda S, Ebisawa M, Kadokura K, Tobe T, Fujimura Y, Kawano S, et al. Uptake through glycoprotein 2 of FimH(+) bacteria by M cells initiates mucosal immune response. Nature. 2009;462:226–230. doi: 10.1038/nature08529. [DOI] [PubMed] [Google Scholar]
- 32.Clevers HC, Bevins CL. Paneth cells: maestros of the small intestinal crypts. Annu Rev Physiol. 2013;75:289–311. doi: 10.1146/annurev-physiol-030212-183744. [DOI] [PubMed] [Google Scholar]
- 33.Pellegrinet L, Rodilla V, Liu Z, Chen S, Koch U, Espinosa L, Kaestner KH, Kopan R, Lewis J, Radtke F. Dll1- and Dll4-mediated notch signaling are required for homeostasis of intestinal stem cells. Gastroenterology. 2011;140:1230–1240.e1-7. doi: 10.1053/j.gastro.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Birchenough GM, Johansson ME, Gustafsson JK, Bergström JH, Hansson GC. New developments in goblet cell mucus secretion and function. Mucosal Immunol. 2015;8:712–719. doi: 10.1038/mi.2015.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johansson ME, Phillipson M, Petersson J, Velcich A, Holm L, Hansson GC. The inner of the two Muc2 mucin-dependent mucus layers in colon is devoid of bacteria. Proc Natl Acad Sci U S A. 2008;105:15064–15069. doi: 10.1073/pnas.0803124105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Suemori S, Lynch-Devaney K, Podolsky DK. Identification and characterization of rat intestinal trefoil factor: tissue- and cell-specific member of the trefoil protein family. Proc Natl Acad Sci U S A. 1991;88:11017–11021. doi: 10.1073/pnas.88.24.11017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yu Y, Yang W, Li Y, Cong Y. Enteroendocrine cells: Sensing gut microbiota and regulating inflammatory bowel diseases. Inflamm Bowel Dis. 2020;26:11–20. doi: 10.1093/ibd/izz217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Latorre R, Sternini C, De Giorgio R, Greenwood-Van Meerveld B. Enteroendocrine cells: a review of their role in brain-gut communication. Neurogastroenterol Motil. 2016;28:620–630. doi: 10.1111/nmo.12754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ting HA, von Moltke J. The immune function of tuft cells at gut mucosal surfaces and beyond. J Immunol. 2019;202:1321–1329. doi: 10.4049/jimmunol.1801069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.von Moltke J, Ji M, Liang HE, Locksley RM. Tuft-cell-derived IL-25 regulates an intestinal ILC2-epithelial response circuit. Nature. 2016;529:221–225. doi: 10.1038/nature16161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scott CL, Guilliams M. Tissue unit-ed: lung cells team up to drive alveolar macrophage development. Cell. 2018;175:898–900. doi: 10.1016/j.cell.2018.10.031. [DOI] [PubMed] [Google Scholar]
- 42.Rossi RL, Soeldner JS, Braasch JW, Heiss FW, Shea JA, Watkins E, Jr, Silverman ML. Long-term results of pancreatic resection and segmental pancreatic autotransplantation for chronic pancreatitis. Am J Surg. 1990;159:51–57. doi: 10.1016/s0002-9610(05)80606-3. [DOI] [PubMed] [Google Scholar]
- 43.Schneider C, Nobs SP, Kurrer M, Rehrauer H, Thiele C, Kopf M. Induction of the nuclear receptor PPAR-γ by the cytokine GM-CSF is critical for the differentiation of fetal monocytes into alveolar macrophages. Nat Immunol. 2014;15:1026–1037. doi: 10.1038/ni.3005. [DOI] [PubMed] [Google Scholar]
- 44.Khalil N, Whitman C, Zuo L, Danielpour D, Greenberg A. Regulation of alveolar macrophage transforming growth factor-β secretion by corticosteroids in bleomycin-induced pulmonary inflammation in the rat. J Clin Invest. 1993;92:1812–1818. doi: 10.1172/JCI116771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mitsi E, Kamng'ona R, Rylance J, Solórzano C, Jesus Reiné J, Mwandumba HC, Ferreira DM, Jambo KC. Human alveolar macrophages predominately express combined classical M1 and M2 surface markers in steady state. Respir Res. 2018;19:66. doi: 10.1186/s12931-018-0777-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chakarov S, Lim HY, Tan L, Lim SY, See P, Lum J, Zhang XM, Foo S, Nakamizo S, Duan K, et al. Two distinct interstitial macrophage populations coexist across tissues in specific subtissular niches. Science. 2019;363:eaau0964. doi: 10.1126/science.aau0964. [DOI] [PubMed] [Google Scholar]
- 47.Won HY, Lee JY, Ryu D, Kim HT, Chang SY. The role of plasmacytoid dendritic cells in gut health. Immune Netw. 2019;19:e6. doi: 10.4110/in.2019.19.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ivanov II, Atarashi K, Manel N, Brodie EL, Shima T, Karaoz U, Wei D, Goldfarb KC, Santee CA, Lynch SV, et al. Induction of intestinal Th17 cells by segmented filamentous bacteria. Cell. 2009;139:485–498. doi: 10.1016/j.cell.2009.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zheng Y, Valdez PA, Danilenko DM, Hu Y, Sa SM, Gong Q, Abbas AR, Modrusan Z, Ghilardi N, de Sauvage FJ, et al. Interleukin-22 mediates early host defense against attaching and effacing bacterial pathogens. Nat Med. 2008;14:282–289. doi: 10.1038/nm1720. [DOI] [PubMed] [Google Scholar]
- 50.Sugimoto K, Ogawa A, Mizoguchi E, Shimomura Y, Andoh A, Bhan AK, Blumberg RS, Xavier RJ, Mizoguchi A. IL-22 ameliorates intestinal inflammation in a mouse model of ulcerative colitis. J Clin Invest. 2008;118:534–544. doi: 10.1172/JCI33194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tsai CH, Hill M, Asa SL, Brubaker PL, Drucker DJ. Intestinal growth-promoting properties of glucagon-like peptide-2 in mice. Am J Physiol. 1997;273:E77–E84. doi: 10.1152/ajpendo.1997.273.1.E77. [DOI] [PubMed] [Google Scholar]
- 52.Silva YP, Bernardi A, Frozza RL. The role of short-chain fatty acids from gut microbiota in gut-brain communication. Front Endocrinol (Lausanne) 2020;11:25. doi: 10.3389/fendo.2020.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ko YT, Alsford T, Miller J. Inhibitory effects on response force in the stop-signal paradigm. J Exp Psychol Hum Percept Perform. 2012;38:465–477. doi: 10.1037/a0027034. [DOI] [PubMed] [Google Scholar]
- 54.Kiyono H, Fukuyama S. NALT- versus Peyer's-patch-mediated mucosal immunity. Nat Rev Immunol. 2004;4:699–710. doi: 10.1038/nri1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Scherzad A, Hagen R, Hackenberg S. Current understanding of nasal epithelial cell mis-differentiation. J Inflamm Res. 2019;12:309–317. doi: 10.2147/JIR.S180853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chen K, Xu W, Wilson M, He B, Miller NW, Bengtén E, Edholm ES, Santini PA, Rath P, Chiu A, et al. Immunoglobulin D enhances immune surveillance by activating antimicrobial, proinflammatory and B cell-stimulating programs in basophils. Nat Immunol. 2009;10:889–898. doi: 10.1038/ni.1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee H, Ruane D, Law K, Ho Y, Garg A, Rahman A, Esterházy D, Cheong C, Goljo E, Sikora AG, et al. Phenotype and function of nasal dendritic cells. Mucosal Immunol. 2015;8:1083–1098. doi: 10.1038/mi.2014.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pizzolla A, Wang Z, Groom JR, Kedzierska K, Brooks AG, Reading PC, Wakim LM. Nasal-associated lymphoid tissues (NALTs) support the recall but not priming of influenza virus-specific cytotoxic T cells. Proc Natl Acad Sci U S A. 2017;114:5225–5230. doi: 10.1073/pnas.1620194114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Condon TV, Sawyer RT, Fenton MJ, Riches DW. Lung dendritic cells at the innate-adaptive immune interface. J Leukoc Biol. 2011;90:883–895. doi: 10.1189/jlb.0311134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Guilliams M, Lambrecht BN, Hammad H. Division of labor between lung dendritic cells and macrophages in the defense against pulmonary infections. Mucosal Immunol. 2013;6:464–473. doi: 10.1038/mi.2013.14. [DOI] [PubMed] [Google Scholar]
- 61.Ballesteros-Tato A, León B, Lund FE, Randall TD. Temporal changes in dendritic cell subsets, cross-priming and costimulation via CD70 control CD8(+) T cell responses to influenza. Nat Immunol. 2010;11:216–224. doi: 10.1038/ni.1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.de Heer HJ, Hammad H, Soullié T, Hijdra D, Vos N, Willart MA, Hoogsteden HC, Lambrecht BN. Essential role of lung plasmacytoid dendritic cells in preventing asthmatic reactions to harmless inhaled antigen. J Exp Med. 2004;200:89–98. doi: 10.1084/jem.20040035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kimura S, Yamakami-Kimura M, Obata Y, Hase K, Kitamura H, Ohno H, Iwanaga T. Visualization of the entire differentiation process of murine M cells: suppression of their maturation in cecal patches. Mucosal Immunol. 2015;8:650–660. doi: 10.1038/mi.2014.99. [DOI] [PubMed] [Google Scholar]
- 64.Lorenz RG, Newberry RD. Isolated lymphoid follicles can function as sites for induction of mucosal immune responses. Ann N Y Acad Sci. 2004;1029:44–57. doi: 10.1196/annals.1309.006. [DOI] [PubMed] [Google Scholar]
- 65.Bouskra D, Brézillon C, Bérard M, Werts C, Varona R, Boneca IG, Eberl G. Lymphoid tissue genesis induced by commensals through NOD1 regulates intestinal homeostasis. Nature. 2008;456:507–510. doi: 10.1038/nature07450. [DOI] [PubMed] [Google Scholar]
- 66.Jung C, Hugot JP, Barreau F. Peyer's patches: The immune sensors of the intestine. Int J Inflamm. 2010;2010:823710. doi: 10.4061/2010/823710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kobayashi N, Takahashi D, Takano S, Kimura S, Hase K. The roles of Peyer's patches and microfold cells in the gut immune system: relevance to autoimmune diseases. Front Immunol. 2019;10:2345. doi: 10.3389/fimmu.2019.02345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jinnohara T, Kanaya T, Hase K, Sakakibara S, Kato T, Tachibana N, Sasaki T, Hashimoto Y, Sato T, Watarai H, et al. IL-22BP dictates characteristics of Peyer's patch follicle-associated epithelium for antigen uptake. J Exp Med. 2017;214:1607–1618. doi: 10.1084/jem.20160770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kim SH, Jung DI, Yang IY, Kim J, Lee KY, Nochi T, Kiyono H, Jang YS. M cells expressing the complement C5a receptor are efficient targets for mucosal vaccine delivery. Eur J Immunol. 2011;41:3219–3229. doi: 10.1002/eji.201141592. [DOI] [PubMed] [Google Scholar]
- 70.Iwasaki A, Welker R, Mueller S, Linehan M, Nomoto A, Wimmer E. Immunofluorescence analysis of poliovirus receptor expression in Peyer's patches of humans, primates, and CD155 transgenic mice: implications for poliovirus infection. J Infect Dis. 2002;186:585–592. doi: 10.1086/342682. [DOI] [PubMed] [Google Scholar]
- 71.Shima H, Watanabe T, Fukuda S, Fukuoka S, Ohara O, Ohno H. A novel mucosal vaccine targeting Peyer's patch M cells induces protective antigen-specific IgA responses. Int Immunol. 2014;26:619–625. doi: 10.1093/intimm/dxu061. [DOI] [PubMed] [Google Scholar]
- 72.Kim SH, Kim YN, Kim J, Jang YS. C5a receptor targeting of partial non-structural protein 3 of dengue virus promotes antigen-specific IFN-γ-producing T-cell responses in a mucosal dengue vaccine model. Cell Immunol. 2018;325:41–47. doi: 10.1016/j.cellimm.2018.01.016. [DOI] [PubMed] [Google Scholar]
- 73.Lelouard H, Fallet M, de Bovis B, Meresse S, Gorvel JP. Peyer's patch dendritic cells sample antigens by extending dendrites through M cell-specific transcellular pores. Gastroenterology. 2012;142:592–601.e3. doi: 10.1053/j.gastro.2011.11.039. [DOI] [PubMed] [Google Scholar]
- 74.Cyster JG, Allen CD. B cell responses: cell interaction dynamics and decisions. Cell. 2019;177:524–540. doi: 10.1016/j.cell.2019.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chang JE, Buechler MB, Gressier E, Turley SJ, Carroll MC. Mechanosensing by Peyer's patch stroma regulates lymphocyte migration and mucosal antibody responses. Nat Immunol. 2019;20:1506–1516. doi: 10.1038/s41590-019-0505-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.McDole JR, Wheeler LW, McDonald KG, Wang B, Konjufca V, Knoop KA, Newberry RD, Miller MJ. Goblet cells deliver luminal antigen to CD103+ dendritic cells in the small intestine. Nature. 2012;483:345–349. doi: 10.1038/nature10863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mazzini E, Massimiliano L, Penna G, Rescigno M. Oral tolerance can be established via gap junction transfer of fed antigens from CX3CR1+ macrophages to CD103+ dendritic cells. Immunity. 2014;40:248–261. doi: 10.1016/j.immuni.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 78.Reboldi A, Cyster JG. Peyer's patches: organizing B-cell responses at the intestinal frontier. Immunol Rev. 2016;271:230–245. doi: 10.1111/imr.12400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Da Silva C, Wagner C, Bonnardel J, Gorvel JP, Lelouard H. The Peyer's patch mononuclear phagocyte system at steady state and during infection. Front Immunol. 2017;8:1254. doi: 10.3389/fimmu.2017.01254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bonnardel J, Da Silva C, Wagner C, Bonifay R, Chasson L, Masse M, Pollet E, Dalod M, Gorvel JP, Lelouard H. Distribution, location, and transcriptional profile of Peyer's patch conventional DC subsets at steady state and under TLR7 ligand stimulation. Mucosal Immunol. 2017;10:1412–1430. doi: 10.1038/mi.2017.30. [DOI] [PubMed] [Google Scholar]
- 81.Komban RJ, Strömberg A, Biram A, Cervin J, Lebrero-Fernández C, Mabbott N, Yrlid U, Shulman Z, Bemark M, Lycke N. Activated Peyer's patch B cells sample antigen directly from M cells in the subepithelial dome. Nat Commun. 2019;10:2423. doi: 10.1038/s41467-019-10144-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Biram A, Strömberg A, Winter E, Stoler-Barak L, Salomon R, Addadi Y, Dahan R, Yaari G, Bemark M, Shulman Z. BCR affinity differentially regulates colonization of the subepithelial dome and infiltration into germinal centers within Peyer's patches. Nat Immunol. 2019;20:482–492. doi: 10.1038/s41590-019-0325-1. [DOI] [PubMed] [Google Scholar]
- 83.Schwickert TA, Victora GD, Fooksman DR, Kamphorst AO, Mugnier MR, Gitlin AD, Dustin ML, Nussenzweig MC. A dynamic T cell-limited checkpoint regulates affinity-dependent B cell entry into the germinal center. J Exp Med. 2011;208:1243–1252. doi: 10.1084/jem.20102477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Biram A, Shulman Z. T cell help to B cells: cognate and atypical interactions in peripheral and intestinal lymphoid tissues. Immunol Rev. 2020;296:36–47. doi: 10.1111/imr.12890. [DOI] [PubMed] [Google Scholar]
- 85.Bergqvist P, Stensson A, Hazanov L, Holmberg A, Mattsson J, Mehr R, Bemark M, Lycke NY. Re-utilization of germinal centers in multiple Peyer's patches results in highly synchronized, oligoclonal, and affinity-matured gut IgA responses. Mucosal Immunol. 2013;6:122–135. doi: 10.1038/mi.2012.56. [DOI] [PubMed] [Google Scholar]
- 86.Heesters BA, Myers RC, Carroll MC. Follicular dendritic cells: dynamic antigen libraries. Nat Rev Immunol. 2014;14:495–504. doi: 10.1038/nri3689. [DOI] [PubMed] [Google Scholar]
- 87.Suzuki K, Maruya M, Kawamoto S, Sitnik K, Kitamura H, Agace WW, Fagarasan S. The sensing of environmental stimuli by follicular dendritic cells promotes immunoglobulin A generation in the gut. Immunity. 2010;33:71–83. doi: 10.1016/j.immuni.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 88.Kim SH, Kim YN, Jang YS. Cutting edge: LL-37-mediated formyl peptide receptor-2 signaling in follicular dendritic cells contributes to B cell activation in Peyer's patch germinal centers. J Immunol. 2017;198:629–633. doi: 10.4049/jimmunol.1600886. [DOI] [PubMed] [Google Scholar]
- 89.Mora JR, von Andrian UH. Differentiation and homing of IgA-secreting cells. Mucosal Immunol. 2008;1:96–109. doi: 10.1038/mi.2007.14. [DOI] [PubMed] [Google Scholar]
- 90.Wang NS, McHeyzer-Williams LJ, Okitsu SL, Burris TP, Reiner SL, McHeyzer-Williams MG. Divergent transcriptional programming of class-specific B cell memory by T-bet and RORα. Nat Immunol. 2012;13:604–611. doi: 10.1038/ni.2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Grootjans J, Krupka N, Hosomi S, Matute JD, Hanley T, Saveljeva S, Gensollen T, Heijmans J, Li H, Limenitakis JP, et al. Epithelial endoplasmic reticulum stress orchestrates a protective IgA response. Science. 2019;363:993–998. doi: 10.1126/science.aat7186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ansaldo E, Slayden LC, Ching KL, Koch MA, Wolf NK, Plichta DR, Brown EM, Graham DB, Xavier RJ, Moon JJ, et al. Akkermansia muciniphila induces intestinal adaptive immune responses during homeostasis. Science. 2019;364:1179–1184. doi: 10.1126/science.aaw7479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Maaser C, Housley MP, Iimura M, Smith JR, Vallance BA, Finlay BB, Schreiber JR, Varki NM, Kagnoff MF, Eckmann L. Clearance of Citrobacter rodentium requires B cells but not secretory immunoglobulin A (IgA) or IgM antibodies. Infect Immun. 2004;72:3315–3324. doi: 10.1128/IAI.72.6.3315-3324.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lee P, Kim DJ. Newly emerging human coronaviruses: animal models and vaccine research for sars, mers, and COVID-19. Immune Netw. 2020;20:e28. doi: 10.4110/in.2020.20.e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ziegler CGK, Allon SJ, Nyquist SK, Mbano IM, Miao VN, Tzouanas CN, Cao Y, Yousif AS, Bals J, Hauser BM, et al. SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell. 2020;181:1016–1035.e19. doi: 10.1016/j.cell.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sungnak W, Huang N, Bécavin C, Berg M, Queen R, Litvinukova M, Talavera-López C, Maatz H, Reichart D, Sampaziotis F, et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. 2020;26:681–687. doi: 10.1038/s41591-020-0868-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LF. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20:363–374. doi: 10.1038/s41577-020-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Stanifer ML, Kee C, Cortese M, Zumaran CM, Triana S, Mukenhirn M, Kraeusslich HG, Alexandrov T, Bartenschlager R, Boulant S. Critical role of type III interferon in controlling SARS-CoV-2 infection in human intestinal epithelial cells. Cell Reports. 2020;32:107863. doi: 10.1016/j.celrep.2020.107863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Trottein F, Sokol H. Potential causes and consequences of gastrointestinal disorders during a SARS-CoV-2 infection. Cell Reports. 2020;32:107915. doi: 10.1016/j.celrep.2020.107915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gu S, Chen Y, Wu Z, Chen Y, Gao H, Lv L, Guo F, Zhang X, Luo R, Huang C, et al. Alterations of the gut microbiota in patients with COVID-19 or H1N1 influenza. Clin Infect Dis. 2020:ciaa709. doi: 10.1093/cid/ciaa709. [DOI] [PMC free article] [PubMed] [Google Scholar]