Abstract
IL-9 has been reported to play dual roles in the pathogenesis of autoimmune disorders and cancers. The collaboration of IL-9 with microenvironmental factors including the broader cytokine milieu and other cellular components may provide important keys to explain its conflicting effects in chronic conditions. In this review, we summarize recent findings on the cellular sources of, and immunological responders to IL-9, in order to interpret the role of IL-9 in the regulation of immune responses. This knowledge will provide new perspectives to improve clinical benefits and limit adverse effects of IL-9 when treating pathologic conditions.
Keywords: Interleukin-9; Autoimmune diseases; Allergy; Cancer, Adaptive immunity; Innate immunity
INTRODUCTION
IL-9, initially termed P40, is a single chain glycoprotein with molecular weight between 32 and 39 kDa (1). Without N-linked glycosylation IL-9 is 14 kDa. IL-9 was first found to support the long-term growth of antigen-independent Th cell lines (1). Unlike other growth factors of T cells, IL-9 did not stimulate the proliferation of cytotoxic T cells (Tc) (1). The Il9 gene loci of both human and mouse shares 55% amino acid homology at the protein level (2). Intriguingly, murine IL-9 can function on human cells, but human IL-9 is inactive on mouse cells. The IL-9 receptor complex consists of the cytokine-specific IL-9 receptor α-chain (IL-9Rα) and the γc-chain (2) and therefore IL-9 is a member of the common γc receptor family which includes IL-2, IL-4, IL-7, IL-15, and IL-21 (3). Binding of IL-9 to the ligand-binding subunit IL-9Rα results in formation of the IL-9R heterocomplex, which undergoes a conformational change to allow binding of JAK1 and JAK3. Phosphorylated JAK1 and JAK3 then mediate the phosphorylation of receptor tyrosine residues (4). In turn, the phosphorylation of tyrosine residues induces activation of transcription factors belonging to the STAT family, insulin receptor substrates (IRSs), and MAP kinase pathway (4). The activation of STAT family including STAT1, STAT3, and/or STAT5 is crucial for IL-9 to mediate its anti-apoptotic and growth regulatory effects (4). In various hematopoietic cells, JAK kinases also mediate the phosphorylation of IRS1/2 which in turn, activates PI3K signaling pathways to induce cell proliferation and prevent caspase-mediated apoptosis (4,5). The MAP kinase pathway also contributes to the extent IL-9 signaling in several lymphoid and hematopoietic cells lines (6).
Although the innate and adaptive components of the immune system are 2 arms of the host responses, they work together intimately to induce effective immune responses. Proinflammatory cytokines play important roles in the interaction between innate and adaptive immune cells. IL-9 has been reported to induce the development of a number of autoimmune diseases such as inflammatory bowel diseases (IBD), multiple sclerosis (MS), psoriasis, rheumatoid arthritis (RA), and systemic lupus erythematosus (SLE) (7,8,9). However, there are also somewhat conflicting reports in which IL-9 was found to suppress experimental autoimmune encephalomyelitis (EAE) in mice (10,11). IL-9 contributes to the pathophysiology of allergic diseases like food allergy, dermatitis or asthma through its autocrine or paracrine effect on T cells, B cells, innate lymphoid cells, mast cells, eosinophils, and neutrophils (12,13,14,15,16,17). Besides the gathering evidence of proinflammatory functions of IL-9, early studies also showed the effect of IL-9 in inducing immune tolerance in tolerant allografts and in inflammatory disease models (18,19). In the context of cancer, many studies have reported pro-tumor effects of IL-9 on hematological tumors and solid tumors (20,21). Nevertheless, more recent evidence suggests IL-9 and IL-9-producing cells may have anti-tumor effects particularly in melanoma, and these data have implied a role for anti-cancer immune responses (20,21). Therefore, the functional role of IL-9 in the pathology of various diseases remains controversial. The apparently conflicting outcomes in different systems implies that it is necessary to clarify the pleiotropic immunological functions of IL-9 in immune-originating cells such as hematopoietic progenitor, myeloid and lymphoid cells but also in non-immune cells such as airway smooth muscle and epithelial cells. Noelle and Nowak (3) have summarized the cellular sources and immune functions of IL-9. However, with a plethora of new findings about the sources and immunological functions of IL-9, a fresh summarizing and detailed interpretation may be very useful. In this review, we focus on clarifying the immune-originated sources of IL-9 and the feedback loop between IL-9 producers and IL-9 responders.
IL-9 ON ADAPTIVE IMMUNE CELLS
Th9 cells
Th9 cells are the subset of Th cells specialized for secreting IL-9. Classic Th9 cells become polarized after originating from naïve T cells, Th2, Th17 or Treg cells in the presence of TGF-β and IL-4 (22,23,24,25). TGF-β induces PU.1, an ETS-family transcription factor, expression while IL-4 triggers the STAT6 pathway followed by induction of IRF4 transcription factor. PU.1 and IRF4 together promote Th9 polarization (24). ETV5 transcription factor, another member of the ETS family, can also induce IL-9 production in Th9 cells in a PU.1 independent manner (24,26). In addition to IL-9, Th9 cells also secrete IL-10 and IL-21 (27) (Fig. 1). The IL-9 secretory capability of Th9 cells does not last for long. These cells lose IL-9 expression gradually during several rounds of differentiation, due to activation of the STAT3 pathway (28). Notably, treatment with retinoic acid, IFN-γ or IL-27 all inhibited IL-9 production from Th9 cells (29,30). Recently, an alternative pathway was reported, in which IL-1β+IL-4 could polarize Th9 from naïve T cells through NF-κB signaling and induce the expression of IL-9 and IL-10 at a comparable level to that induced by the classical pathway (31). In addition, an agonistic antibody of GITR, a TNF receptor family protein, enhanced the differentiation to Th9 cells via TRAF6 and NF-κB pathway in an IL-4 dependent manner (32). Whether IL-9 exerts direct effects on Th9 cell development is still elusive. However, absence of IL-9R signaling in Il9R−/− mice significantly reduced the frequency of Th9 cells in vivo and in vitro compared to the control groups (33).
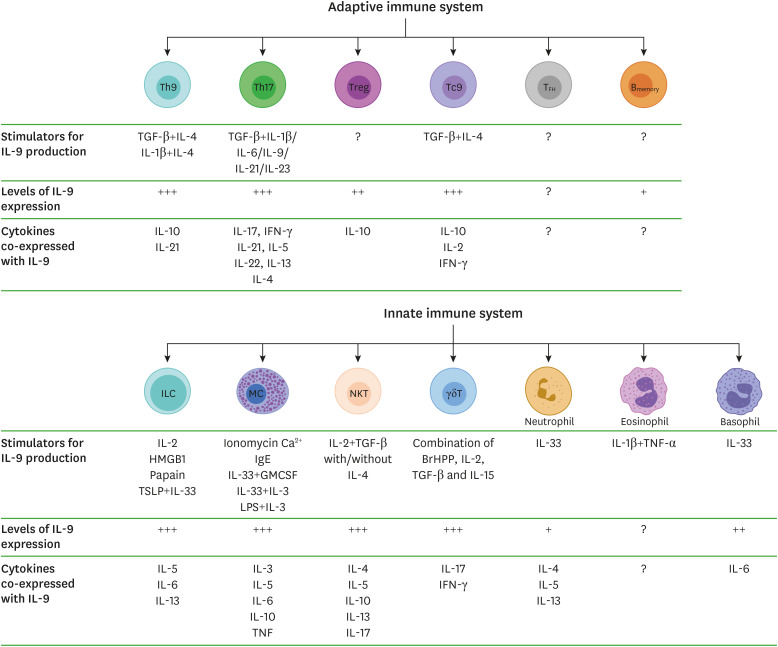
Figure 1. Conditions in which IL-9 is produced by immune cells.
IL-9 can be produced by cellular components from both the adaptive and innate immune systems. After stimulation by the indicated conditions, Th9, Th17, IL-9 producing CD8+ T (Tc9), NKT cells, ILCs, MCs, and γδ T cells express IL-9 at high levels (+++), while Treg and basophils produce IL-9 at moderate levels (++). Memory B cells and neutrophils produce IL-9 at a low level (+). IL-9 expression by TFH cells and eosinophils have not yet been analyzed by ELISA. Cytokines co-expressed with IL-9 after stimulation are listed.
Th17 cells
Th17 cells are defined as a subset of T helper cells releasing IL-17A (34). Although secretion of IL-9 is mainly attributed to the Th9 subset, IL-9 can also be secreted by Th17 (35,36,37). The production of IL-9 by Th17 cells is positively regulated by combinations of TGF-β with any of IL-1β, IL-6, IL-21, or IL-23 (35,37) and is negatively regulated by IL-23 alone (36) (Fig. 1). Recently, TL1A, a member of the TNF superfamily, was reported as a new stimulator for IL-17 secretion from memory CD4+ T cells (38). TL1A alone or together with IL-6/TGF-β can trigger memory Th17 to release a large amount of IL-17, IL-22, IFN-γ, and IL-9 (38) (Fig. 1). The secretion of IL-22 by TL1A-stimulated Th17 cells was dependent on the IL-9 signaling pathway since treatment with anti-IL-9R antibody inhibited IL-22 production (38). In some allergic conditions, in addition to IL-9, Th17 cells also expressed IL-4, IL-5, IL-8, IL-13, IL-21, and IL-22 (39). Notably, IL-9 secretion depends on the differentiation stage of Th17 cells. Newly polarized Th17 from naïve CD4+ T cells did not express IL-9. The capability for IL-9 expression was acquired after several rounds of polarization under Th17-polarizing conditions in vitro (35). Memory Th17 cells play an important part in IL-9 release (35,38). IFN-γ or IL-27 supplementation significantly inhibited IL-9, IL-17 and ROR-γt expression in Th17 cells (30).
As more than a cytokine secreted by Th17 cells, IL-9 plays important roles in Th17 differentiation and proliferation through autocrine and paracrine stimulation. Combinations of IL-9 and TGF-β differentiated naïve CD4+ T cells into Th17 cells to express IL-17 through STAT1 and STAT3 activation in both human and mouse (8,36,40) (Fig. 2). Treatment with IL-9 neutralizing antibody partially attenuated the secretion of IL-17 from Th17 cells that were polarized by treatment with IL-6 or IL-21 in the presence of TGF-β (36). Exogenous IL-9 failed to enhance IL-17 production in CD4+ T cells from STAT1−/− or STAT3−/− mice (8).
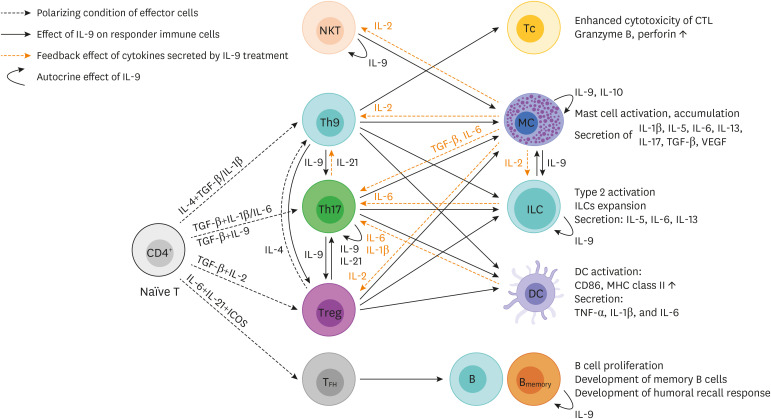
Figure 2. Proposed model of crosstalk between producers and immune targets of IL-9.
IL-9 can exert various effects on both adaptive and innate immune cells. These effects include stimulating the differentiation and proliferation of Th17, promoting suppressive functions of Treg cells, enhancing cytotoxicity of cytotoxic T lymphocytes (Tc, CTL), inducing activation and accumulation of MCs, activating and maintaining ILCs, activating DCs, regulating memory B cell development and antibody recall response. After being stimulated by IL-9, IL-9 responders secrete cytokines which, in turn, exert their biological effects on IL-9 producing cells. There are also significant autocrine effects of IL-9 in Th17, NKT, MC, ILC and memory B cells. Indirect effects of IL-9 on Th1 and Th2 are not included in this illustration.
The close relationship between IL-9 and Th17 cells has been notably revealed in autoimmune disease. Myelin-specific Th1 and/or Th17 cells are known to cause EAE through damage to the blood-brain barrier (41). Mechanistically, IL-9 promoted Th17 migration into the CNS by inducing CCL-20 from astrocytes (25) while IL-9 neutralization or IL-9R deficiency reduced Th17 migration and attenuated the EAE phenotype (25,42). Furthermore, Il9−/− mice developed significantly less severe EAE, accompanied by lower levels of IL-17 (8). In the EAE resistant Il9−/− mice, the expression of C-C chemokine receptors including CCR2, CCR5 and CCR6 were reduced in memory/activated T cells and that may have contributed to the reduced migration of Th17 cells into CNS (8). IL-9 secretion by memory Th17 cells was also shown to be increased in patients with autoimmune diabetes (35). In K5.hTGF-β1 transgenic mice, a psoriasis model, intradermal IL-9 injection triggered Th17-related inflammation and further treatment with anti-IL-17 antibody reduced the inflammation (40). In psoriasis patients, IL-9R expression was shown to be elevated in samples of lesional skin, and IL-9 treatment increased the number of Th17 cells and hence IL-17 secretion more in peripheral blood mononuclear cells (PBMCs) from psoriasis patients than those from normal healthy controls (40). In the cancer context, subcutaneous implantation of IL-9 expressing CT26 colon cancer cells clearly showed elevated levels of IL-17 in both blood serum and tumor masses (43). In this system, although IL-9 definitely reduced colon cancer growth, the survival of mice was not improved. It was proposed that IL-17-related inflammation may counteract prolonged survival of mice injected with IL-9 secreting cancer cells. In another study, deficiencies in Th17 pathways (ROR-γ−/− or IL-23−/−) enhanced IL-9 producing T cells, and this was accompanied by delays in B16F10 tumor growth in mice. Further analysis of tumor infiltrating lymphocytes confirmed the anti-tumor effect of tumor-antigen-specific Th9 in this system (44).
Tregs
The role of Tregs has been extensively investigated in the areas of immune tolerance and graft rejection. Two classes of Treg exist: natural Treg (nTreg, CD4+CD25+Foxp3+) originating from the thymus while induced Treg (iTreg, CD4+CD25−) are derived from mature T cells in the peripheral system (45,46). Both nTreg and iTreg cells are known to produce IL-9 (19) (Fig. 1). The positive role of IL-9 on the immunosuppressive function of Tregs was first reported by Noelle and colleagues (19). They found that both Tregs and mast cells (MCs) play important roles in the induction of immunosuppression in long-lived allografts. Given that IL-9 is highly expressed by Tregs and plays dominant roles in activation and accumulation of MCs, they proposed IL-9 as a key cytokine secreted from Tregs that functions to recruit and activate MCs for inducing local tolerance. Neutralizing IL-9 greatly accelerates allograft rejection in Rag−/− mice adoptively transferred with Tc and Tregs, and abolished the protective effect of adoptive Treg therapy in mice suffering acute nephrotoxic serum nephritis (18,19,36). IL-9 is also a key mediator of Tregs and MCs in suppressing the immune system in a lymphoma model. Inhibition of IL-9-signaling down-regulated expression of Treg-related gene (Foxp3), mast cell-related genes (CD117, Mcpt1, Mcpt5) and monocyte-related gene (Fcer1a) in tumor draining lymph nodes, and delayed tumor growth in mice (47,48). In an EAE model, the absence of IL-9 signaling in Il9R−/− mice weakened the suppressive activity of nTregs in vivo and worsened symptoms of EAE compared to wild type mice (36).
Notably, IL-9 emerged as an important cytokine to balance the Th9/Th17/Treg cell populations. IL-9 from Th9 promotes the expansion of Th17, and Th17-derived IL-21 is involved in the differentiation of Th9 (Fig. 2). STAT3 and STAT5, (IL-9 downstream signaling factors), play opposing roles in regulating the polarization of Th17 and Treg (36,49,50). Moreover, in an IL-4 rich setting, Tregs can be converted to Th9 phenotype (23).
Th1 and Th2 cells
Th1 is known to express very low IL-9R (42). However, IL-9 can indirectly regulate Th1 polarization through modulating the expression of other cytokines, such as IL-12 and IFN-γ, which are crucial stimulatory cytokines for initiating Th1 polarization (51). Exogenous IL-9 reduced IL-12 and IFN-γ expression from PBMCs leading to negative effects on Th1 polarization (15,52). The serum level of IFN-γ was significantly elevated in Il9−/− mice compared with wild type mice (15) and ectopic implantation of IL-9-expressing tumor cells reduced IFN-γ concentration in both blood and tumor masses (43). Th2 cells were found to express IL-9R at levels as high as Th17 cells (42), but there is little evidence for direct effects of IL-9 on Th2 cells. However, IL-9 can support Th2 polarization by its ability to regulate the production of IL-4. Absence of IL-9R signaling in Il9R−/− mice significantly reduced the frequency of Th2 cells induced by Aspergillus fumigatus infection (33). The serum concentration of IL-4 in Il9−/− mice is lower than wild type and treatment with IL-9 induced IL-4 secretion in PBMCs (15,52).
Cytotoxic CD8+ T cells
Tc9 cells are defined as IL-9 producing cytotoxic CD8+ T cells, which differentiate from naïve CD8+ cells under Th9-polarizing conditions, such as in the presence of IL-4 and TGF-β (53,54). Tc9 differentiation can also be prompted by dendritic cells (DCs) in an IL-33 rich environment or by resident CXCR1+ DCs (55,56). Unlike conventional cytotoxic CD8+ T cells (Tc1 cells), Tc9 cells express high levels of transcription factors PU.1 and IRF4, and low levels of Eomes and Tbx21 (53,54). In cytokine profile, Tc9 expresses high levels of IL-2, IL-9, IL-10 and low levels of IFN-γ, granzyme and perforin (53,54,55) (Fig. 1). Therefore, Tc9 cells were expected to have lower cytolytic activity than Tc1. However, Tc9 cells were less exhausted and converted to an IFN-γ positive Tc1-like phenotype after up to 14 days of the adoptive transfer. As a consequence, adoptive transfer of tumor specific Tc9 generated cytolytic activities 2-fold greater than Tc1 cells in experiments using B16 melanoma (53). Tc9 consistently showed significantly lower levels of exhaustion markers including KLRG-1, PD-1, LAG-3 and 2B4 (53,55,57). Treatment with IL-9 up-regulated the expression of IL-9 and IL-9R in Tc9 cells but not in other CD8+ T cells (57). In other cases, Tc9 cells promoted Th2-mediated airway inflammation in allergic airway disease, and Foxp3 or cholesterol derivatives inhibited IL-9 production in Tc9 cells (54,58).
The anti-tumor effects of Th9 are primarily attributable to the immunostimulatory function of IL-9 on cytotoxic CD8+ T cells as has been shown against breast cancer, colorectal cancer, and melanoma. The CD8+ population of T cells was expanded in the presence of Th9 cells and the addition of anti-IL-9 antibodies partially blocked CD8+ T cell-mediated cytotoxicity (27,59). Blocking IL-9 signaling by neutralizing antibody reduced the production of granzyme B and perforin by CD8+ T cells but the same did not occur in NK cells. And vice versa, treatment with recombinant IL-9 accelerated cytotoxicity of tumor specific CD8+ T cells in mice by inducing granzyme and perforin expression (60). In addition, IL-9 can stimulate tumor specific CTL responses by enhancing the function of DCs (32).
B cells
IL-9R was found to be expressed in B cells of follicles, the marginal zone and germinal center of spleen, and is especially induced in memory B cells (16,61,62). It is also expressed in diffuse large B cell lymphoma (DLBCL) cell lines such as LY1 and LY8 (63). IL-9R expression was stimulated by CD40L alone, or in combination with BAFF, and inhibited by treatment with IL-4 or IL-21 (16,62). IL-9 is also selectively expressed in memory B cells, and the autocrine or parcrine manner of IL-9 signaling is important for memory B cell develoment (62). The first evidence of the effects of IL-9 on B cells was obtained in experiments using IL-9 transgenic mice. In those mice, the serum concentrations of IgM, IgG1, IgG2a, IgG2b, IgG3, and IgE were enhanced after immunization with antigens, compared with control mice (64). The level of IgG antibodies were even higher after secondary immunization (64). Treatment with exogenous IL-9 promoted the proliferation of DLBCL cells and protected them from induced apoptosis (63). In tonsillar B cells, IL-9 triggered IL-4-mediated IgE production through the activation of STAT3, and STAT5 (16).
The mechanisms underlying the generation and activation of memory B cells is necessary to completely understand the humoral immune response. Wang et al. (61) used Il9R−/− mice to show that IL-9 is required for germinal center development of memory B cells and also found that follicular helper T (TFH) cells supply IL-9 for optimum development of memory B cells (61) (Fig. 2). Takatsuka et al. (62) also reported IL-9 promotes the proliferation and differentiation of ex vivo-cultured B cells by inducing phosphorylation of STAT3 and STAT5. Furthermore, they showed that IL-9-IL-9R signaling may initiate memory B cell develoment. Treatment with IL-9 significantly downregulated ICOSL, a co-stimulatory molecule for germinal center formation, on memory B cells, implying that the cytokine facilitated plasma cell-differentiation from memory B cells rather than keeping them in germinal centers (62). Although the primary IgG1 response was not affected by the lack of IL-9R, the secondary IgG1 and IgG2b responses following the booster dose was diminished in Il9R−/− mice (62).
IL-9 ON INNATE IMMUNE CELLS
DCs
DCs themselves may not secrete IL-9 but can function to either stimulate or inhibit T cells with respect to IL-9 secretion. Dectin-1-activated DCs induced proliferation and IL-9 expression of Th9 cells via IL-33 signaling pathway (65,66,67). On the other hand, retinoic acid-monocyte-derived DC inhibited IL-9 production from Th9 and Th17 cells (29). The expression of IL-9R was strongly detected on the surface of bone marrow derived dendritic cells (BMDCs), myeloid DCs, and plasmacytoid DCs (12,68). Treatment with IL-9 did not alter the proliferation of BMDCs, but it stimulated the activation of BMDCs by inducing phosphorylation of JAK1, JAK3, STAT3, and NF-κB (12,69) (Fig. 2). After stimulation with IL-9, activated BMDCs expressed more surface CD86 and MHC class II molecules and secreted more TNF-α, IL-1β, and IL-6 (12,70). In IL-9 transgenic mice, IL-9-activated DCs can stimulate proliferation of CD4+ T cells and induce differentiation into Th2 subclass. Co-culturing of IL-9-activated BMDCs and naïve T cells led to an inhibition of Th1 differentiation (IFN-γ+CD4+ T cells) and facilitated Th2 polarization (IL-4+GATA3+CD4+ T cells). IL-9-activated BMDCs did not alter the frequency of Th17 and Tregs in vitro (12,70). In contrast, in an EAE model, splenic DC from Il9−/− mice were found to express more IL-1β, IL-6, IL-23A and less IL-27, and they induced naïve CD4+ T cells to produce more IFN-γ compared with control mice (10).
Innate lymphoid cells (ILCs)
ILCs are a heterogeneous population of lymphocytes lacking antigen specific B or T cell receptors (71). Based on expression profiles of transcription factors and cytokines, ILCs are categorized into three groups, ILC1, ILC2 and ILC3. Since ILCs are tissue resident cells, they act early in the immune response and process target antigens to stimulate T cells (72). Intriguingly, ILCs, especially type 2 (ILC2), have been shown to be a major producer of IL-9 (33,73,74,75). In mice, IL-9-expressing ILCs far outnumbered IL-9 expressing T cells and produced more IL-9 than T cell counterparts at the cellular level (75). However, resting ILCs did not express IL-9, but only started to produce it after being treated with IL-2 or after prolonged stimulation with any of HMGB1, papain, or TSLP + IL-33 (12,73,74). IL-2 is an essential signal for IL-9 production by ILCs. The main IL-2 sources for eliciting IL-9 expression by ILCs are adaptive immune cells (Fig. 2). In fact, IL-9 concentration was dramatically reduced in the lungs of Rag1−/− mice compared to those from wild type mice and declined completely in Rag2−/−Il2Rg−/− mice (73). IL-9 production from Rag1−/− ILCs was recovered after overnight stimulation with IL-2, but this did not occur in Rag2−/−Il2Rg−/− ILCs (73). Notably, the expression of IL-9 from stimulated ILCs did not last for long. Around 24 hour after stimulation, the level of IL-9 expression dropped significantly and those cells began to express IL-5, IL-6, and IL-13 instead (73) (Fig. 1). Production of IL-9 by activated ILCs required transcription factor IRF4 (74). Irf4−/− ILC2 cells did not express IL-9, and further, downstream cytokines, IL-5 and IL-13, were also not produced. Expression of IL-5 and IL-13 by Irf4−/− ILC2 were however rescued by treatment with IL-9 (74). ST2, suppressor of tumorigenicity 2, is an IL-33 receptor and a negative regulator of IL-9 production in ILC2s. The number of IL-9+ ILC2 cells and the secretion level of IL-9 were increased in ST2−/− mice (13).
Both naïve and activated ILCs express high levels of IL-9R (73,74,75,76,77) and early exposure to IL-9 is important for rapid and complete activation of effector ILCs (Fig. 2). The total number of CD25+Sca-1+ILCs, and GATA3+ ILC2s, were significantly attenuated in IL-9 signaling deficient mice (73,75). Implantation of bone marrow from wild type or Il9R−/− mice into irradiated CD45.1+Rag1−/− mice revealed that the survival of IL-5+IL-13+ ILC2s depends on their natural ability to respond to IL-9 (75). Based on these lines of evidence, autocrine or paracrine signaling of IL-9 may play crucial roles in maintenance and expansion of ILC2s (Fig.2). IL-9 exerted direct effects on protecting ILC2s from apoptotic cell death by upregulation of survival factor BCL3 (75). IL-9 also exerted its indirect effect on promoting the expansion of IL-25+ ILC2s by inducing IL-2 expression in MCs (33,77,78) (Fig.2).
Mast cells
Mast cells (MCs) can be stimulated by Ca2+-ionophore ionomycin, cross-linkage of antigen specific IgE (IgE/Ag), IL-33+GM-CSF, IL-33+IL3, or LPS+IL-3 (Fig. 1). These activated MCs secrete large amounts of IL-9 (79,80). Together with IL-9, the up-regulated production of several Th2-related cytokines including IL-3, IL-5, IL-6, IL-10 and TNF were observed in MCs activated by ionomycin or IgE/Ag (79,81). Furthermore, the presence of IL-1 alone or in combination with IL-10 or stem cell factor (SCF), significantly increased IL-9 production from activated MCs by enhancing the stability of IL-9 mRNA (79). Activated MCs expressed high amount of endogenous IL-10 which, in turn, exerted autocrine effects on MCs to amplify IL-9 production (79) (Fig. 2). STAT5 and GATA1 transcription factors are necessary for IL-9 production in MCs (82). The secretion of IL-9 from activated MCs is partially inhibited by treatment with SGC-CBP300, a bromodomain inhibitor (80).
MCs are a major target group of IL-9 as they express significant levels of IL-9R (42). Hematopoietic cells including activated Tregs, Th9, ILC2, and NKT cells are the main sources of IL-9 for in situ accumulation of MCs (19,83,84) (Fig 2). Recent in vivo evidence suggests that IL-9 serves as a chemoattractant to recruit activated MCs. In ST2−/− mice, elevations in IL-9 led to the accumulation of intraepithelial MCs and enhancement of their effector function (13). In IL-9 or IL-9R deficient mice, the number of MCs and MC precursors in bone marrow, peritoneal cavity, lung and intestine were significantly reduced compared to control mice (33,80,84,85). In IL9∆CNS-25 mice lacking the CNS-25 element (which is 25 kb upstream from the IL9 gene, and has IL9-enhancer characteristics), IL-9 production was significantly impaired and the functioning of MCs was reduced, as evidenced by a reduced temperature drop and lower plasma IL-6 concentration, in response to IgE and BSA injection (80). Blockage of IL-9 signaling by anti-IL-9 antibody decreased MC infiltration into the central nervous system in EAE mice (86). Furthermore, IL-9 signaling plays key roles in the activation of MCs (Fig 2). Treatment with IL-9 significantly increased production of IL-1β, IL-2, IL-4, IL-5, IL-6, IL-9, IL-10, IL-13, IL-17, TGF-β, VEGF and MIF by MCs (33,87,88,89). In IL-9 or IL-9R deficient mice, the activation of MCs was attenuated and the effector function of MCs characterized by mastocytosis was diminished (17,85). MCs play a vital role in elimination of Strongyloides ratti in mice as IL-9R deficiency increased intestinal parasite burden and prolonged the infection (83). The serum concentrations of MCP1, a mast cell degranulation marker, and IgE were drastically reduced in Il9R−/− mice compared with control mice after Strongyloides ratti-infection (83). In addition, IL-9 plays key roles in MC-mediated allergic responses. For example, in OVA-sensitized mice, food allergy was induced by the recruitment of IL-9 producing MCs in the intestinal area and in lung (84,85,90). In contrast, the development of food allergy was inhibited in OVA-sensitized Il9−/− or Il9R−/− mice (85).
Notably, there is no direct evidence indicating that IL-9 alone can promote proliferation of MCs in vitro since weakening of IL-9 signaling did not change the number of MCs in IL9∆CNS-25 mice (80). However, synergistic activity resulting from combined IL-9 and SCF treatment promoted mast cell growth in vitro (91).
NKT cells
Invariant NKT cells (iNKT), a major subset of NKT cells, are a CD1d-restricted T cell population. Naïve iNKT cells do not express IL-9 (92), but iNKT cells stimulated with a combination of IL-2, TGF-β and IL-4, produced large amounts of IL-9 under control of IRF4 transcription factor (84,92) (Fig. 1). In addition, NKT cells secreting large amounts of IL-9 were detected in biopsies from 8 out of 12 patients suffering nasal NKT lymphomas (93). IL-9 and IL-9R were also found to be expressed by nasal NKT lymphoma cell lines, SNK-6 and SNT-8, and accordingly, IL-9 is an autocrine growth factor for nasal NKT lymphoma cell lines. Treatment with IL-9 stimulated the in vitro proliferation of SNK-6 and SNT-8 cells and neutralization with anti-IL-9 antibody lowered the in vitro viability of those cell lines (93). IL-9-secreted from iNKT cells is also known for its role in allergic inflammation through MC accumulation (Fig. 2). Intratracheal adoptive transfer of IL-9-secreting iNKT cells led to recruitment of eosinophils and MCs in the airways of recipient mice. The accumulation of eosinophils and MCs was abolished by IL-9 signaling neutralization with anti-IL-9 antibody (92). Interestingly, the lack of iNKT cells also reduced the number of pulmonary MCs by up to 65% in CD1d-deficient mice with allergic airway inflammation (84). Anti-CD1d treatment of IL-9-deficient mice or anti-IL-9 treatment of CD1d-deficient mice did not further lessen the impairment of MC recruitment, implicating iNKT cells as an important source of IL-9 for MC accumulation.
γδ T cells, granulocytes, and macrophages
Vγ9Vδ2 T cells are the dominant γδ T-cell subset in human peripheral blood and the peripheral blood Vγ9Vδ2 T cell is one of the major sources of IL-9 in humans (94). Vγ9Vδ2 T cells secreted large amount of IL-9 after in vitro stimulation with a combination of phosphoantigen (bromohydrin pyrophosphate, BrHPP), IL-2, TGF-β and IL-15 (94) (Fig. 1). The expression of IL-9R on Vγ9Vδ2 T cells was significantly increased in patients with psoriatic arthritis (PsA) inflammatory disease. Treatment with IL-9 strongly promoted expression of IL-17 and IFN-γ from Vγ9Vδ2 T cells in PsA patients (95).
Neutrophils, eosinophils and basophils can express small amounts of IL-9 under some circumstances (14,80,82,96) (Fig. 1). Although the effect of IL-9 on eosinophils has not been clarified yet, the significant reduction of eosinophils in lungs of Il9R−/− mice in response to Nippostrongylus brasiliensis infection implied a potential function for IL-9 in this subset of immune cells (75). Monocytes and macrophages were found to express high levels of IL-9R (12,68). IL-9 treatment induced phosphorylation of STAT1, 3, and 5 in blood monocytes and reduced the expression of activation markers including CD45, CD11b, CD68 and CD14 in inflammatory macrophages (68). In the context of B16 lung metastasis, IL-9 stimulated the accumulation of M1-like macrophages in lung and induced cytotoxic function of the macrophages in vitro (97).
CONCLUSION AND FUTURE PERSPECTIVES
IL-9 is produced by a wide variety of immune cells including CD4+ T cells, CD8+ T cells, B cells, NKT cells, ILCs, MCs, γδ T cells, and granulocytes. Among them, the primary producers of IL-9 seem to be Th9, ILC2, and MCs (Fig. 1). Under conditions stimulatory for IL-9 secretion, almost all of the IL-9 producers also expressed either IL-5, IL-13 and/or IL-10. These co-expressing cytokines may contribute to shifting the nature of immune responses to type 2 or to immune suppression. In our proposed model of Fig. 2, IL-9 can exert various effects on both adaptive and innate immune cells. These effects include 1) stimulating the differentiation and proliferation of Th17 cells, 2) promoting immune suppressive functions of Tregs, 3) enhancing cytotoxicity of Tc cells, 4) inducing activation and accumulation of MCs, 5) activating and maintaining ILCs, 6) activating DCs toward type 2 responses, 7) promoting allergic inflammation of NKT cells, and 8) regulating memory B cell development. After being stimulated by IL-9, the immune cells secrete cytokines that, in turn, may also act as feedback responses to promote the expansion of IL-9-producing cells (Fig. 2). For example, IL-2 produced from MC can stimulate the polarization and proliferation of various types of effector cells including Th9, Th17, Treg, NKT cells and ILC2. In addition, MC-, ILC2-, or DC-derived IL-1β, IL-6 or TGF-β are important for the development of Th17 cells (78,98,99). Remarkably, IL-9 exhibits important roles in maintaining the balance of Th9, Th17 and Tregs. IL-9 secreted from Th9 can promote the expansion of Th17 cells and enhance the immunosuppressive function of Tregs. Furthermore, Th17-derived IL-21 and Treg-derived IL-4 are involved in the differentiation of Th9. There are also significant autocrine effects of IL-9 in Th17, NKT, MC, ILC and memory B cells. Collectively, we can conclude that the crosstalk between the producers and immune targets of IL-9 derive various cytokine networks and regulate immune cell activities.
Recent studies on IL-9 have significantly expanded our understanding of its effects on diverse immune cells and particularly on memory B cells, Tc cells, DCs, and ILCs. Further dissection of biological function mediated by IL-9 on Th2, Treg, NKTs, γδ T-cells, granulocytes and macrophages will provide a more complete view on how IL-9 exerts its anti-inflammatory or pro-inflammatory function in a given physiological setting. In particular, the specific conditions for, and the clinical consequences of, the conversions between the IL-9-producing CD4+ T cell subsets need to be further clarified. In chronic disease contexts, IL-9 exerts either pro-inflammatory or anti-inflammatory effects depending on the overall cytokine milieu and other cellular components in the microenvironment. Further studies are required to delineate the cooperative interactions between IL-9 and microenvironmental factors in the pathogenesis of autoimmune disease, allergy, and cancer.
ACKNOWLEDGeMENTS
This research was supported by the National Research Foundation of Korea (NRF) (NRF-2017M3A9F6029753) and by a grant from Chungnam National University.
Abbreviations
- BMDC
bone marrow derived dendritic cells
- BrHPP
bromohydrin pyrophosphate
- DC
dendritic cell
- DLBCL
diffuse large B cell lymphoma
- EAE
experimental autoimmune encephalomyelitis
- IBD
inflammatory bowel disease
- IL-9R
IL-9 receptor
- ILC
innate lymphoid cells
- iNKT
Invariant NKT cells
- IRS
insulin receptor substrate
- iTreg
induced Treg
- MC
mast cell
- MS
multiple sclerosis
- nTreg
natural Treg
- PsA
psoriatic arthritis
- RA
rheumatoid arthritis
- SLE
systemic lupus erythematosus
- Tc
cytotoxic T
- TFH
follicular helper T
Footnotes
Conflict of Interest: The authors declare no potential conflicts of interest.
- Conceptualization: Kim YS, Lee H.
- Formal analysis: Lee H, Do-Thi VA.
- Funding acquisition: Kim YS, Lee JO.
- Writing - original draft: Lee H, Do-Thi VA.
- Writing - review & editing: Kim YS, Lee JO, Lee H, Do-Thi VA.
References
- 1.Uyttenhove C, Simpson RJ, Van Snick J. Functional and structural characterization of P40, a mouse glycoprotein with T-cell growth factor activity. Proc Natl Acad Sci U S A. 1988;85:6934–6938. doi: 10.1073/pnas.85.18.6934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Renauld JC, Druez C, Kermouni A, Houssiau F, Uyttenhove C, Van Roost E, Van Snick J. Expression cloning of the murine and human interleukin 9 receptor cDNAs. Proc Natl Acad Sci U S A. 1992;89:5690–5694. doi: 10.1073/pnas.89.12.5690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Noelle RJ, Nowak EC. Cellular sources and immune functions of interleukin-9. Nat Rev Immunol. 2010;10:683–687. doi: 10.1038/nri2848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chakraborty S, Kubatzky KF, Mitra DK. An update on interleukin-9: from its cellular source and signal transduction to its role in immunopathogenesis. Int J Mol Sci. 2019;20:2113. doi: 10.3390/ijms20092113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Demoulin JB, Grasso L, Atkins JM, Stevens M, Louahed J, Levitt RC, Nicolaides NC, Renauld JC. Role of insulin receptor substrate-2 in interleukin-9-dependent proliferation. FEBS Lett. 2000;482:200–204. doi: 10.1016/s0014-5793(00)02059-7. [DOI] [PubMed] [Google Scholar]
- 6.Demoulin JB, Louahed J, Dumoutier L, Stevens M, Renauld JC. MAP kinase activation by interleukin-9 in lymphoid and mast cell lines. Oncogene. 2003;22:1763–1770. doi: 10.1038/sj.onc.1206253. [DOI] [PubMed] [Google Scholar]
- 7.Ciccia F, Guggino G, Rizzo A, Manzo A, Vitolo B, La Manna MP, Giardina G, Sireci G, Dieli F, Montecucco CM, et al. Potential involvement of IL-9 and Th9 cells in the pathogenesis of rheumatoid arthritis. Rheumatology (Oxford) 2015;54:2264–2272. doi: 10.1093/rheumatology/kev252. [DOI] [PubMed] [Google Scholar]
- 8.Li H, Nourbakhsh B, Cullimore M, Zhang GX, Rostami A. IL-9 is important for T-cell activation and differentiation in autoimmune inflammation of the central nervous system. Eur J Immunol. 2011;41:2197–2206. doi: 10.1002/eji.201041125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deng Y, Wang Z, Chang C, Lu L, Lau CS, Lu Q. Th9 cells and IL-9 in autoimmune disorders: pathogenesis and therapeutic potentials. Hum Immunol. 2017;78:120–128. doi: 10.1016/j.humimm.2016.12.010. [DOI] [PubMed] [Google Scholar]
- 10.Yoshimura S, Thome R, Konno S, Mari ER, Rasouli J, Hwang D, Boehm A, Li Y, Zhang GX, Ciric B, et al. IL-9 controls central nervous system autoimmunity by suppressing GM-CSF production. J Immunol. 2020;204:531–539. doi: 10.4049/jimmunol.1801113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elyaman W, Bassil R, Bradshaw EM, Orent W, Lahoud Y, Zhu B, Radtke F, Yagita H, Khoury SJ. Notch receptors and Smad3 signaling cooperate in the induction of interleukin-9-producing T cells. Immunity. 2012;36:623–634. doi: 10.1016/j.immuni.2012.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wan J, Huang L, Ji X, Yao S, Hamed Abdelaziz M, Cai W, Wang H, Cheng J, Dineshkumar K, Aparna V, et al. HMGB1-induced ILC2s activate dendritic cells by producing IL-9 in asthmatic mouse model. Cell Immunol. 2020;352:104085. doi: 10.1016/j.cellimm.2020.104085. [DOI] [PubMed] [Google Scholar]
- 13.Verma M, Liu S, Michalec L, Sripada A, Gorska MM, Alam R. Experimental asthma persists in IL-33 receptor knockout mice because of the emergence of thymic stromal lymphopoietin-driven IL-9+ and IL-13+ type 2 innate lymphoid cell subpopulations. J Allergy Clin Immunol. 2018;142:793–803.e8. doi: 10.1016/j.jaci.2017.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sun B, Zhu L, Tao Y, Sun HX, Li Y, Wang P, Hou Y, Zhao Y, Zhang X, Zhang L, et al. Characterization and allergic role of IL-33-induced neutrophil polarization. Cell Mol Immunol. 2018;15:782–793. doi: 10.1038/cmi.2017.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu J, Harberts E, Tammaro A, Girardi N, Filler RB, Fishelevich R, Temann A, Licona-Limón P, Girardi M, Flavell RA, et al. IL-9 regulates allergen-specific Th1 responses in allergic contact dermatitis. J Invest Dermatol. 2014;134:1903–1911. doi: 10.1038/jid.2014.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fawaz LM, Sharif-Askari E, Hajoui O, Soussi-Gounni A, Hamid Q, Mazer BD. Expression of IL-9 receptor α chain on human germinal center B cells modulates IgE secretion. J Allergy Clin Immunol. 2007;120:1208–1215. doi: 10.1016/j.jaci.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 17.Townsend JM, Fallon GP, Matthews JD, Smith P, Jolin EH, McKenzie NA. IL-9-deficient mice establish fundamental roles for IL-9 in pulmonary mastocytosis and goblet cell hyperplasia but not T cell development. Immunity. 2000;13:573–583. doi: 10.1016/s1074-7613(00)00056-x. [DOI] [PubMed] [Google Scholar]
- 18.Eller K, Wolf D, Huber JM, Metz M, Mayer G, McKenzie AN, Maurer M, Rosenkranz AR, Wolf AM. IL-9 production by regulatory T cells recruits mast cells that are essential for regulatory T cell-induced immune suppression. J Immunol. 2011;186:83–91. doi: 10.4049/jimmunol.1001183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lu LF, Lind EF, Gondek DC, Bennett KA, Gleeson MW, Pino-Lagos K, Scott ZA, Coyle AJ, Reed JL, Van Snick J, et al. Mast cells are essential intermediaries in regulatory T-cell tolerance. Nature. 2006;442:997–1002. doi: 10.1038/nature05010. [DOI] [PubMed] [Google Scholar]
- 20.Lee JE, Zhu Z, Bai Q, Brady TJ, Xiao H, Wakefield MR, Fang Y. The role of interleukin-9 in cancer. Pathol Oncol Res. 2020;26:2017–2022. doi: 10.1007/s12253-019-00665-6. [DOI] [PubMed] [Google Scholar]
- 21.Wan J, Wu Y, Ji X, Huang L, Cai W, Su Z, Wang S, Xu H. IL-9 and IL-9-producing cells in tumor immunity. Cell Commun Signal. 2020;18:50. doi: 10.1186/s12964-020-00538-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Veldhoen M, Uyttenhove C, van Snick J, Helmby H, Westendorf A, Buer J, Martin B, Wilhelm C, Stockinger B. Transforming growth factor-β ‘reprograms’ the differentiation of T helper 2 cells and promotes an interleukin 9-producing subset. Nat Immunol. 2008;9:1341–1346. doi: 10.1038/ni.1659. [DOI] [PubMed] [Google Scholar]
- 23.Dardalhon V, Awasthi A, Kwon H, Galileos G, Gao W, Sobel RA, Mitsdoerffer M, Strom TB, Elyaman W, Ho IC, et al. IL-4 inhibits TGF-β-induced Foxp3+ T cells and, together with TGF-β, generates IL-9+ IL-10+ Foxp3− effector T cells. Nat Immunol. 2008;9:1347–1355. doi: 10.1038/ni.1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaplan MH. The transcription factor network in Th9 cells. Semin Immunopathol. 2017;39:11–20. doi: 10.1007/s00281-016-0600-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou Y, Sonobe Y, Akahori T, Jin S, Kawanokuchi J, Noda M, Iwakura Y, Mizuno T, Suzumura A. IL-9 promotes Th17 cell migration into the central nervous system via CC chemokine ligand-20 produced by astrocytes. J Immunol. 2011;186:4415–4421. doi: 10.4049/jimmunol.1003307. [DOI] [PubMed] [Google Scholar]
- 26.Koh B, Hufford MM, Pham D, Olson MR, Wu T, Jabeen R, Sun X, Kaplan MH. The ETS family transcription factors ETV5 and PU.1 function in parallel to promote Th9 cell development. J Immunol. 2016;197:2465–2472. doi: 10.4049/jimmunol.1502383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.You FP, Zhang J, Cui T, Zhu R, Lv CQ, Tang HT, Sun DW. Th9 cells promote antitumor immunity via IL-9 and IL-21 and demonstrate atypical cytokine expression in breast cancer. Int Immunopharmacol. 2017;52:163–167. doi: 10.1016/j.intimp.2017.08.031. [DOI] [PubMed] [Google Scholar]
- 28.Ulrich BJ, Verdan FF, McKenzie AN, Kaplan MH, Olson MR. STAT3 activation impairs the stability of Th9 cells. J Immunol. 2017;198:2302–2309. doi: 10.4049/jimmunol.1601624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rampal R, Awasthi A, Ahuja V. Retinoic acid-primed human dendritic cells inhibit Th9 cells and induce Th1/Th17 cell differentiation. J Leukoc Biol. 2016;100:111–120. doi: 10.1189/jlb.3VMA1015-476R. [DOI] [PubMed] [Google Scholar]
- 30.Murugaiyan G, Beynon V, Pires Da Cunha A, Joller N, Weiner HL. IFN-γ limits Th9-mediated autoimmune inflammation through dendritic cell modulation of IL-27. J Immunol. 2012;189:5277–5283. doi: 10.4049/jimmunol.1200808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xue G, Jin G, Fang J, Lu Y. IL-4 together with IL-1β induces antitumor Th9 cell differentiation in the absence of TGF-β signaling. Nat Commun. 2019;10:1376. doi: 10.1038/s41467-019-09401-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim IK, Kim BS, Koh CH, Seok JW, Park JS, Shin KS, Bae EA, Lee GE, Jeon H, Cho J, et al. Glucocorticoid-induced tumor necrosis factor receptor-related protein co-stimulation facilitates tumor regression by inducing IL-9-producing helper T cells. Nat Med. 2015;21:1010–1017. doi: 10.1038/nm.3922. [DOI] [PubMed] [Google Scholar]
- 33.Moretti S, Renga G, Oikonomou V, Galosi C, Pariano M, Iannitti RG, Borghi M, Puccetti M, De Zuani M, Pucillo CE, et al. A mast cell-ILC2-Th9 pathway promotes lung inflammation in cystic fibrosis. Nat Commun. 2017;8:14017. doi: 10.1038/ncomms14017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tesmer LA, Lundy SK, Sarkar S, Fox DA. Th17 cells in human disease. Immunol Rev. 2008;223:87–113. doi: 10.1111/j.1600-065X.2008.00628.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beriou G, Bradshaw EM, Lozano E, Costantino CM, Hastings WD, Orban T, Elyaman W, Khoury SJ, Kuchroo VK, Baecher-Allan C, et al. TGF-β induces IL-9 production from human Th17 cells. J Immunol. 2010;185:46–54. doi: 10.4049/jimmunol.1000356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Elyaman W, Bradshaw EM, Uyttenhove C, Dardalhon V, Awasthi A, Imitola J, Bettelli E, Oukka M, van Snick J, Renauld JC, et al. IL-9 induces differentiation of TH17 cells and enhances function of FoxP3+ natural regulatory T cells. Proc Natl Acad Sci U S A. 2009;106:12885–12890. doi: 10.1073/pnas.0812530106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nowak EC, Noelle RJ. Interleukin-9 as a T helper type 17 cytokine. Immunology. 2010;131:169–173. doi: 10.1111/j.1365-2567.2010.03332.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thomas LS, Targan SR, Tsuda M, Yu QT, Salumbides BC, Haritunians T, Mengesha E, McGovern DP, Michelsen KS. The TNF family member TL1A induces IL-22 secretion in committed human Th17 cells via IL-9 induction. J Leukoc Biol. 2017;101:727–737. doi: 10.1189/jlb.3A0316-129R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cosmi L, Maggi L, Santarlasci V, Capone M, Cardilicchia E, Frosali F, Querci V, Angeli R, Matucci A, Fambrini M, et al. Identification of a novel subset of human circulating memory CD4+ T cells that produce both IL-17A and IL-4. J Allergy Clin Immunol. 2010;125:222–230.e1. doi: 10.1016/j.jaci.2009.10.012. [DOI] [PubMed] [Google Scholar]
- 40.Singh TP, Schön MP, Wallbrecht K, Gruber-Wackernagel A, Wang XJ, Wolf P. Involvement of IL-9 in Th17-associated inflammation and angiogenesis of psoriasis. PLoS One. 2013;8:e51752. doi: 10.1371/journal.pone.0051752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kebir H, Kreymborg K, Ifergan I, Dodelet-Devillers A, Cayrol R, Bernard M, Giuliani F, Arbour N, Becher B, Prat A. Human TH17 lymphocytes promote blood-brain barrier disruption and central nervous system inflammation. Nat Med. 2007;13:1173–1175. doi: 10.1038/nm1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nowak EC, Weaver CT, Turner H, Begum-Haque S, Becher B, Schreiner B, Coyle AJ, Kasper LH, Noelle RJ. IL-9 as a mediator of Th17-driven inflammatory disease. J Exp Med. 2009;206:1653–1660. doi: 10.1084/jem.20090246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Do Thi VA, Park SM, Lee H, Kim YS. Ectopically expressed membrane-bound form of IL-9 exerts immune-stimulatory effect on CT26 colon carcinoma cells. Immune Netw. 2018;18:e12. doi: 10.4110/in.2018.18.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Purwar R, Schlapbach C, Xiao S, Kang HS, Elyaman W, Jiang X, Jetten AM, Khoury SJ, Fuhlbrigge RC, Kuchroo VK, et al. Robust tumor immunity to melanoma mediated by interleukin-9-producing T cells. Nat Med. 2012;18:1248–1253. doi: 10.1038/nm.2856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Adeegbe DO, Nishikawa H. Natural and induced T regulatory cells in cancer. Front Immunol. 2013;4:190. doi: 10.3389/fimmu.2013.00190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Whiteside TL, Schuler P, Schilling B. Induced and natural regulatory T cells in human cancer. Expert Opin Biol Ther. 2012;12:1383–1397. doi: 10.1517/14712598.2012.707184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Feng LL, Gao JM, Li PP, Wang X. IL-9 contributes to immunosuppression mediated by regulatory T cells and mast cells in B-cell non-hodgkin's lymphoma. J Clin Immunol. 2011;31:1084–1094. doi: 10.1007/s10875-011-9584-9. [DOI] [PubMed] [Google Scholar]
- 48.Smith SE, Hoelzinger DB, Dominguez AL, Van Snick J, Lustgarten J. Signals through 4-1BB inhibit T regulatory cells by blocking IL-9 production enhancing antitumor responses. Cancer Immunol Immunother. 2011;60:1775–1787. doi: 10.1007/s00262-011-1075-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yao Z, Kanno Y, Kerenyi M, Stephens G, Durant L, Watford WT, Laurence A, Robinson GW, Shevach EM, Moriggl R, et al. Nonredundant roles for Stat5a/b in directly regulating Foxp3. Blood. 2007;109:4368–4375. doi: 10.1182/blood-2006-11-055756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Laurence A, Tato CM, Davidson TS, Kanno Y, Chen Z, Yao Z, Blank RB, Meylan F, Siegel R, Hennighausen L, et al. Interleukin-2 signaling via STAT5 constrains T helper 17 cell generation. Immunity. 2007;26:371–381. doi: 10.1016/j.immuni.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 51.Jacobson NG, Szabo SJ, Weber-Nordt RM, Zhong Z, Schreiber RD, Darnell JE, Jr, Murphy KM. Interleukin 12 signaling in T helper type 1 (Th1) cells involves tyrosine phosphorylation of signal transducer and activator of transcription (Stat)3 and Stat4. J Exp Med. 1995;181:1755–1762. doi: 10.1084/jem.181.5.1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wu B, Huang C, Kato-Maeda M, Hopewell PC, Daley CL, Krensky AM, Clayberger C. IL-9 is associated with an impaired Th1 immune response in patients with tuberculosis. Clin Immunol. 2008;126:202–210. doi: 10.1016/j.clim.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 53.Lu Y, Hong B, Li H, Zheng Y, Zhang M, Wang S, Qian J, Yi Q. Tumor-specific IL-9-producing CD8+ Tc9 cells are superior effector than type-I cytotoxic Tc1 cells for adoptive immunotherapy of cancers. Proc Natl Acad Sci U S A. 2014;111:2265–2270. doi: 10.1073/pnas.1317431111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Visekruna A, Ritter J, Scholz T, Campos L, Guralnik A, Poncette L, Raifer H, Hagner S, Garn H, Staudt V, et al. Tc9 cells, a new subset of CD8(+) T cells, support Th2-mediated airway inflammation. Eur J Immunol. 2013;43:606–618. doi: 10.1002/eji.201242825. [DOI] [PubMed] [Google Scholar]
- 55.Liu N, Jiang Y, Chen J, Nan H, Zhao Y, Chu X, Wang A, Wang D, Qin T, Gao S, et al. IL-33 drives the antitumor effects of dendritic cells via the induction of Tc9 cells. Cell Mol Immunol. 2019;16:644–651. doi: 10.1038/s41423-018-0166-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chang SY, Song JH, Guleng B, Cotoner CA, Arihiro S, Zhao Y, Chiang HS, O'Keeffe M, Liao G, Karp CL, et al. Circulatory antigen processing by mucosal dendritic cells controls CD8(+) T cell activation. Immunity. 2013;38:153–165. doi: 10.1016/j.immuni.2012.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ding P, Zhu R, Cai B, Zhang J, Bu Q, Sun DW. IL-9-producing CD8+ T cells represent a distinctive subset with different transcriptional characteristics from conventional CD8+ T cells, and partially infiltrate breast tumors. Int J Biochem Cell Biol. 2019;115:105576. doi: 10.1016/j.biocel.2019.105576. [DOI] [PubMed] [Google Scholar]
- 58.Ma X, Bi E, Huang C, Lu Y, Xue G, Guo X, Wang A, Yang M, Qian J, Dong C, et al. Cholesterol negatively regulates IL-9-producing CD8+ T cell differentiation and antitumor activity. J Exp Med. 2018;215:1555–1569. doi: 10.1084/jem.20171576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang C, Lu Y, Chen L, Gao T, Yang Q, Zhu C, Chen Y. Th9 cells are subjected to PD-1/PD-L1-mediated inhibition and are capable of promoting CD8 T cell expansion through IL-9R in colorectal cancer. Int Immunopharmacol. 2020;78:106019. doi: 10.1016/j.intimp.2019.106019. [DOI] [PubMed] [Google Scholar]
- 60.Nonomura Y, Otsuka A, Nakashima C, Seidel JA, Kitoh A, Dainichi T, Nakajima S, Sawada Y, Matsushita S, Aoki M, et al. Peripheral blood Th9 cells are a possible pharmacodynamic biomarker of nivolumab treatment efficacy in metastatic melanoma patients. OncoImmunology. 2016;5:e1248327. doi: 10.1080/2162402X.2016.1248327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wang Y, Shi J, Yan J, Xiao Z, Hou X, Lu P, Hou S, Mao T, Liu W, Ma Y, et al. Germinal-center development of memory B cells driven by IL-9 from follicular helper T cells. Nat Immunol. 2017;18:921–930. doi: 10.1038/ni.3788. [DOI] [PubMed] [Google Scholar]
- 62.Takatsuka S, Yamada H, Haniuda K, Saruwatari H, Ichihashi M, Renauld JC, Kitamura D. IL-9 receptor signaling in memory B cells regulates humoral recall responses. Nat Immunol. 2018;19:1025–1034. doi: 10.1038/s41590-018-0177-0. [DOI] [PubMed] [Google Scholar]
- 63.Lv X, Feng L, Ge X, Lu K, Wang X. Interleukin-9 promotes cell survival and drug resistance in diffuse large B-cell lymphoma. J Exp Clin Cancer Res. 2016;35:106. doi: 10.1186/s13046-016-0374-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vink A, Warnier G, Brombacher F, Renauld JC. Interleukin 9-induced in vivo expansion of the B-1 lymphocyte population. J Exp Med. 1999;189:1413–1423. doi: 10.1084/jem.189.9.1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chen J, Zhao Y, Chu X, Lu Y, Wang S, Yi Q. Dectin-1-activated dendritic cells: a potent Th9 cell inducer for tumor immunotherapy. OncoImmunology. 2016;5:e1238558. doi: 10.1080/2162402X.2016.1238558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen J, Zhao Y, Jiang Y, Gao S, Wang Y, Wang D, Wang A, Yi H, Gu R, Yi Q, et al. Interleukin-33 contributes to the induction of Th9 cells and antitumor efficacy by dectin-1-activated dendritic cells. Front Immunol. 2018;9:1787. doi: 10.3389/fimmu.2018.01787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhao Y, Chu X, Chen J, Wang Y, Gao S, Jiang Y, Zhu X, Tan G, Zhao W, Yi H, et al. Dectin-1-activated dendritic cells trigger potent antitumour immunity through the induction of Th9 cells. Nat Commun. 2016;7:12368. doi: 10.1038/ncomms12368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Donninelli G, Saraf-Sinik I, Mazziotti V, Capone A, Grasso MG, Battistini L, Reynolds R, Magliozzi R, Volpe E. Interleukin-9 regulates macrophage activation in the progressive multiple sclerosis brain. J Neuroinflammation. 2020;17:149. doi: 10.1186/s12974-020-01770-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Park J, Li H, Zhang M, Lu Y, Hong B, Zheng Y, He J, Yang J, Qian J, Yi Q. Murine Th9 cells promote the survival of myeloid dendritic cells in cancer immunotherapy. Cancer Immunol Immunother. 2014;63:835–845. doi: 10.1007/s00262-014-1557-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Leech MD, Grencis RK. Induction of enhanced immunity to intestinal nematodes using IL-9-producing dendritic cells. J Immunol. 2006;176:2505–2511. doi: 10.4049/jimmunol.176.4.2505. [DOI] [PubMed] [Google Scholar]
- 71.Spits H, Cupedo T. Innate lymphoid cells: emerging insights in development, lineage relationships, and function. Annu Rev Immunol. 2012;30:647–675. doi: 10.1146/annurev-immunol-020711-075053. [DOI] [PubMed] [Google Scholar]
- 72.Vivier E, Artis D, Colonna M, Diefenbach A, Di Santo JP, Eberl G, Koyasu S, Locksley RM, McKenzie AN, Mebius RE, et al. Innate lymphoid cells: 10 years on. Cell. 2018;174:1054–1066. doi: 10.1016/j.cell.2018.07.017. [DOI] [PubMed] [Google Scholar]
- 73.Wilhelm C, Hirota K, Stieglitz B, Van Snick J, Tolaini M, Lahl K, Sparwasser T, Helmby H, Stockinger B. An IL-9 fate reporter demonstrates the induction of an innate IL-9 response in lung inflammation. Nat Immunol. 2011;12:1071–1077. doi: 10.1038/ni.2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mohapatra A, Van Dyken SJ, Schneider C, Nussbaum JC, Liang HE, Locksley RM. Group 2 innate lymphoid cells utilize the IRF4-IL-9 module to coordinate epithelial cell maintenance of lung homeostasis. Mucosal Immunol. 2016;9:275–286. doi: 10.1038/mi.2015.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Turner JE, Morrison PJ, Wilhelm C, Wilson M, Ahlfors H, Renauld JC, Panzer U, Helmby H, Stockinger B. IL-9-mediated survival of type 2 innate lymphoid cells promotes damage control in helminth-induced lung inflammation. J Exp Med. 2013;210:2951–2965. doi: 10.1084/jem.20130071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Price AE, Liang HE, Sullivan BM, Reinhardt RL, Eisley CJ, Erle DJ, Locksley RM. Systemically dispersed innate IL-13-expressing cells in type 2 immunity. Proc Natl Acad Sci U S A. 2010;107:11489–11494. doi: 10.1073/pnas.1003988107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hoyler T, Klose CS, Souabni A, Turqueti-Neves A, Pfeifer D, Rawlins EL, Voehringer D, Busslinger M, Diefenbach A. The transcription factor GATA-3 controls cell fate and maintenance of type 2 innate lymphoid cells. Immunity. 2012;37:634–648. doi: 10.1016/j.immuni.2012.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Roediger B, Kyle R, Tay SS, Mitchell AJ, Bolton HA, Guy TV, Tan SY, Forbes-Blom E, Tong PL, Köller Y, et al. IL-2 is a critical regulator of group 2 innate lymphoid cell function during pulmonary inflammation. J Allergy Clin Immunol. 2015;136:1653–1663.e7. doi: 10.1016/j.jaci.2015.03.043. [DOI] [PubMed] [Google Scholar]
- 79.Stassen M, Arnold M, Hültner L, Müller C, Neudörfl C, Reineke T, Schmitt E. Murine bone marrow-derived mast cells as potent producers of IL-9: costimulatory function of IL-10 and kit ligand in the presence of IL-1. J Immunol. 2000;164:5549–5555. doi: 10.4049/jimmunol.164.11.5549. [DOI] [PubMed] [Google Scholar]
- 80.Koh B, Abdul Qayum A, Srivastava R, Fu Y, Ulrich BJ, Janga SC, Kaplan MH. A conserved enhancer regulates Il9 expression in multiple lineages. Nat Commun. 2018;9:4803. doi: 10.1038/s41467-018-07202-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hültner L, Kölsch S, Stassen M, Kaspers U, Kremer JP, Mailhammer R, Moeller J, Broszeit H, Schmitt E. In activated mast cells, IL-1 up-regulates the production of several Th2-related cytokines including IL-9. J Immunol. 2000;164:5556–5563. doi: 10.4049/jimmunol.164.11.5556. [DOI] [PubMed] [Google Scholar]
- 82.Abdul Qayum A, Koh B, Martin RK, Kenworthy BT, Kharwadkar R, Fu Y, Wu W, Conrad DH, Kaplan MH. The IL9 CNS-25 regulatory element controls mast cell and basophil IL-9 production. J Immunol. 2019;203:1111–1121. doi: 10.4049/jimmunol.1900272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Reitz M, Hartmann W, Rüdiger N, Orinska Z, Brunn ML, Breloer M. Interleukin-9 promotes early mast cell-mediated expulsion of Strongyloides ratti but is dispensable for generation of protective memory. Sci Rep. 2018;8:8636. doi: 10.1038/s41598-018-26907-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jones TG, Hallgren J, Humbles A, Burwell T, Finkelman FD, Alcaide P, Austen KF, Gurish MF. Antigen-induced increases in pulmonary mast cell progenitor numbers depend on IL-9 and CD1d-restricted NKT cells. J Immunol. 2009;183:5251–5260. doi: 10.4049/jimmunol.0901471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chen CY, Lee JB, Liu B, Ohta S, Wang PY, Kartashov AV, Mugge L, Abonia JP, Barski A, Izuhara K, et al. Induction of interleukin-9-producing mucosal mast cells promotes susceptibility to IgE-mediated experimental food allergy. Immunity. 2015;43:788–802. doi: 10.1016/j.immuni.2015.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yin JJ, Hu XQ, Mao ZF, Bao J, Qiu W, Lu ZQ, Wu HT, Zhong XN. Neutralization of interleukin-9 decreasing mast cells infiltration in experimental autoimmune encephalomyelitis. Chin Med J (Engl) 2017;130:964–971. doi: 10.4103/0366-6999.204110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wiener Z, Falus A, Toth S. IL-9 increases the expression of several cytokines in activated mast cells, while the IL-9-induced IL-9 production is inhibited in mast cells of histamine-free transgenic mice. Cytokine. 2004;26:122–130. doi: 10.1016/j.cyto.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 88.Renga G, Moretti S, Oikonomou V, Borghi M, Zelante T, Paolicelli G, Costantini C, De Zuani M, Villella VR, Raia V, et al. IL-9 and mast cells are key players of candida albicans commensalism and pathogenesis in the gut. Cell Reports. 2018;23:1767–1778. doi: 10.1016/j.celrep.2018.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tete S, Saggini A, Maccauro G, Rosati M, Conti F, Cianchetti E, Tripodi D, Toniato E, Fulcheri M, Salini V, et al. Interleukin-9 and mast cells. J Biol Regul Homeost Agents. 2012;26:319–326. [PubMed] [Google Scholar]
- 90.Lee JB. Regulation of IgE-mediated food allergy by IL-9 producing mucosal mast cells and type 2 innate lymphoid cells. Immune Netw. 2016;16:211–218. doi: 10.4110/in.2016.16.4.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Godfraind C, Louahed J, Faulkner H, Vink A, Warnier G, Grencis R, Renauld JC. Intraepithelial infiltration by mast cells with both connective tissue-type and mucosal-type characteristics in gut, trachea, and kidneys of IL-9 transgenic mice. J Immunol. 1998;160:3989–3996. [PubMed] [Google Scholar]
- 92.Monteiro M, Agua-Doce A, Almeida CF, Fonseca-Pereira D, Veiga-Fernandes H, Graca L. IL-9 expression by invariant NKT cells is not imprinted during thymic development. J Immunol. 2015;195:3463–3471. doi: 10.4049/jimmunol.1403170. [DOI] [PubMed] [Google Scholar]
- 93.Nagato T, Kobayashi H, Kishibe K, Takahara M, Ogino T, Ishii H, Oikawa K, Aoki N, Sato K, Kimura S, et al. Expression of interleukin-9 in nasal natural killer/T-cell lymphoma cell lines and patients. Clin Cancer Res. 2005;11:8250–8257. doi: 10.1158/1078-0432.CCR-05-1426. [DOI] [PubMed] [Google Scholar]
- 94.Peters C, Häsler R, Wesch D, Kabelitz D. Human Vδ2 T cells are a major source of interleukin-9. Proc Natl Acad Sci U S A. 2016;113:12520–12525. doi: 10.1073/pnas.1607136113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Guggino G, Ciccia F, Di Liberto D, Lo Pizzo M, Ruscitti P, Cipriani P, Ferrante A, Sireci G, Dieli F, Fourniè JJ, et al. Interleukin (IL)-9/IL-9R axis drives γδ T cells activation in psoriatic arthritis patients. Clin Exp Immunol. 2016;186:277–283. doi: 10.1111/cei.12853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gounni AS, Nutku E, Koussih L, Aris F, Louahed J, Levitt RC, Nicolaides NC, Hamid Q. IL-9 expression by human eosinophils: regulation by IL-1β and TNF-α. J Allergy Clin Immunol. 2000;106:460–466. doi: 10.1067/mai.2000.109172. [DOI] [PubMed] [Google Scholar]
- 97.Park SM, Do-Thi VA, Lee JO, Lee H, Kim YS. Interleukin-9 inhibits lung metastasis of melanoma through stimulating anti-tumor M1 macrophages. Mol Cells. 2020;43:479–490. doi: 10.14348/molcells.2020.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ross SH, Cantrell DA. Signaling and function of interleukin-2 in T lymphocytes. Annu Rev Immunol. 2018;36:411–433. doi: 10.1146/annurev-immunol-042617-053352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bachmann MF, Oxenius A. Interleukin 2: from immunostimulation to immunoregulation and back again. EMBO Rep. 2007;8:1142–1148. doi: 10.1038/sj.embor.7401099. [DOI] [PMC free article] [PubMed] [Google Scholar]