Abstract
Since December 2019, COVID-19 has aroused global attention. Studies show the link between obesity and severe outcome of influenza and COVID-19. Thus, we aimed to compare the impacts of obesity on the severity and mortality of influenza and COVID-19 by performing a meta-analysis. A systematic search was performed in MEDLINE, EMASE, ClinicalTrials.gov, and Web of Science from January 2009 to July 2020. The protocol was registered onto PROSPERO (CRD42020201461). After selection, 46 studies were included in this meta-analysis. The pooled odds ratios (ORs) with 95% confidence intervals (CIs) were analyzed. We found obesity was a risk factor for the severity and mortality of influenza (ORsevere outcome = 1.56, CI: 1.28-1.90; ORmortality = 1.99, CI: 1.15-3.46). For COVID-19, obesity was a significant risk factor only for severe outcome (OR = 2.07, CI: 1.53-2.81) but not for mortality (OR = 1.57, CI: 0.85-2.90). Compared with obesity, morbid obesity was linked with a higher risk for the severity and mortality of both influenza (OR = 1.40, CI: 1.10-1.79) and COVID-19 (OR = 3.76, CI: 2.67-5.28). Thus, obesity should be recommended as a risk factor for the prognosis assessment of COVID-19. Special monitoring and earlier treatment should be implemented in patients with obesity and COVID-19.
Keywords: obesity, COVID-19, influenza, mortality, severe outcome
Introduction
Since December 2019, countries globally have been suffering from the spread of COVID-19, which is also known as SARS-CoV-2 (1, 2). The latest information indicates that there are more than 48 million COVID-19 cases around the world, according to the data on November 6, 2020. Based on the 1918 “Spanish” influenza pandemic and 2009 influenza A (H1N1) pandemic (3), studies show the close relationship between obesity and virus infection as well as mortality (4, 5). Significantly, special attention should be paid to obese patients. Due to the prolonged pandemic of COVID-19, tons of expenses have been spent on medical fields, which has influenced the social economy extremely (6). Thus, investigating the influencing factors and susceptible population are the most important things to prevent the pandemic of COVID-19. Evidence from previous influenza studies might provide referential and warning values for the understanding and control of COVID-19.
Obesity is one of the most important diseases affecting people’s health with dramatically increased morbidity year by year (7, 8). Studies indicate that obesity is linked with increased influenza infection. Because of the disturbed immune regulation and metabolic homeostasis, patients with obesity present higher risks for the severe outcome and mortality of influenza (9, 10). Similarly, the latest studies show that COVID-19 patients with obesity are more likely to be admitted to the intensive care unit (ICU), be on mechanical support, and have a severe outcome (11, 12). Although some reviews and meta-analyses have been published on the topic of obesity and severe outcome of COVID-19, the data are updated every minute (13). An available and timely meta-analysis is urgent. Moreover, the differences and comparisons of severity, outcome, and mortality between influenza and COVID-19 in patients with obesity are unknown so far. Thus, to compare the effect of obesity on influenza and COVID-19 is of great value and importance for us to learn about COVID-19.
In the present study, we aimed to systematically review and compare the effects of obesity on the infection, hospitalization, disease severity, and mortality of both influenza and COVID-19 based on the available evidence. In addition, we updated the meta-analysis by including the latest studies from other countries. We hope this meta-analysis provides more valuable information for the management of the COVID-19 pandemic.
Methods
Literature Search Strategy
A systematic search was conducted to identify papers available on MEDLINE, EMASE, ClinicalTrials.gov, and Web of Science for relevant studies from January 2009 to July 2020. The review protocol was registered onto PROSPERO (CRD42020201461). We developed a search strategy for MEDLINE based on medical subject heading (MeSH®) terms and text of target papers. Different possible variations and combinations of the following search terms were used: influenza, influenza A, influenza B, H1N1, H7N9, COVID-19, SARS-CoV-2, coronavirus, 2019 nCoV, obesity, obese, BMI, severity, outcome, and mortality. We also reviewed the reference lists of all included papers and relevant review papers to identify studies that the database searches might have missed. To minimize selection bias, two persons completed this work independently. Disagreements were resolved by consensus and by a third person. In the initial search, no filter for language preference was used. The literature search process is based on the PRISMA form (14).
Inclusion and Exclusion Criteria
Articles were included or excluded on the basis of full-text articles. The following inclusion criteria were applied: 1) For the diagnosis of obesity, BMI was applied for classification according to the American Endocrine Society Scientific Statement on obesity management (15): ①normal weight: 18.5 kg/m2 < BMI < 25 kg/m2; ②overweight: 25 kg/m2 ≤ BMI < 30 kg/m2; ③obesity: BMI ≥ 30 kg/m2; ④morbid obesity: BMI ≥ 35 kg/m2. 2) COVID-19 infection is diagnosed according to the criteria established by the China National Health Commission (16) based on laboratory examinations, such as nasopharyngeal and oropharyngeal swab tests. Detection tests for coronavirus include reverse-transcription polymerase chain reaction (RT-PCR), real-time RT-PCR (rRT-PCR), and reverse transcription loop-mediated isothermal amplification (RT-LAMP). To identify patients earlier, two one-step quantitative RT-PCR (qRT-PCR) assays were developed to detect two different regions (ORF1b and N) of the SARS-CoV-2 genome. For patients suffering from fever, sore throat, fatigue, coughing, or dyspnea coupled with recent exposure, COVID-19 infection should be diagnosed with typical chest computerized tomography (CT) characteristics despite negative RT-PCR results. 3) Influenza infection is diagnosed with clinical manifestations and laboratory tests (17). The RT-PCR test is the most traditional yet powerful approach for identification of influenza viruses in most diagnostic labs around the world. Rapid influenza diagnostic tests are also applied by many countries, using monoclonal antibodies that target the viral nucleoprotein and employ either an enzyme immunoassay or immunochromatographic techniques. 4) Included studies should present data that could be extracted straightforwardly, and detailed characteristics on the population and studies should be provided. 5) Severe outcome of influenza and COVID-19 refers to admission to the ICU, requiring mechanical support, hypoxia requiring oxygen therapy, and increased mortality and death. 6) Only papers published in English were included in the present study, but abstracts of non-English papers were also reviewed to prevent missing information.
Studies were excluded if subjects had diabetes or other fatal chronic diseases or medication history. Fatal chronic disease refers to disease that could induce the severity of COVID-19 or influenza besides obesity, which might make it difficult to discuss the role of obesity on the risk and outcome of COVID-19 or influenza. For instance, fatal chronic diseases include cancer, severe autoimmune disease, chronic kidney disease, diabetes, cirrhosis, liver failure, and so on. As for medication history, it does not mean all kinds of treatment are excluded. Only medications that could cause interference in the outcome or mortality of COVID-19 or influenza were excluded. Case reports, reviews, meta-analyses, conference abstracts, and letters to the editor were also excluded.
Data Extraction and Analysis
Both investigators (XZ and QH) initially screened all relevant titles and abstracts to confirm if the studies were related to the topics of present study. After the first round of reviewing, full-text articles were read by two persons. Data were extracted from studies meeting our inclusion criteria according to our self-made forms. Data on population characteristics, group descriptions, and odds ratio or relative risk (OR/RR) values were extracted. One investigator performed the data extraction (XZ), which was verified by a second investigator (QH). Data from influenza and COVID-19 studies were analyzed through meta-analysis guidelines. For influenza studies, we aimed to analyze the data on the influenza infection, hospitalization, disease severity, and mortality in patients with obesity or morbid obesity. For COVID-19 studies, we aimed to analyze the data on the disease severity and mortality in patients with obesity or morbid obesity. OR/RR and 95% confidence interval (95% CI) were presented as effect size for case control or cohort studies. Before data synthesis, heterogeneity was estimated using the Q test and I2 statistic. When P < 0.1 or I2>50%, indicating the existence of possible heterogeneity among studies, the random-effect model was applied. Sensitivity analyses were performed to explore the resources of heterogeneity in instances in which sufficient data were collected. The Begg’s test was used to evaluate publication biases. All analyses were completed with the software STATA 15.1 (StataCorp, College Station, TX, USA). All statistical tests were 2-tailed.
Methodological Quality Assessment
The 9-star Newcastle-Ottawa Scale (NOS) was applied to assess the quality of the studies (18). The methodologies of studies that achieved 6/9 or more were classified as high quality, whereas those that scored less than 5/9 were classified as low quality.
Results
Literature Search and Study Characteristics
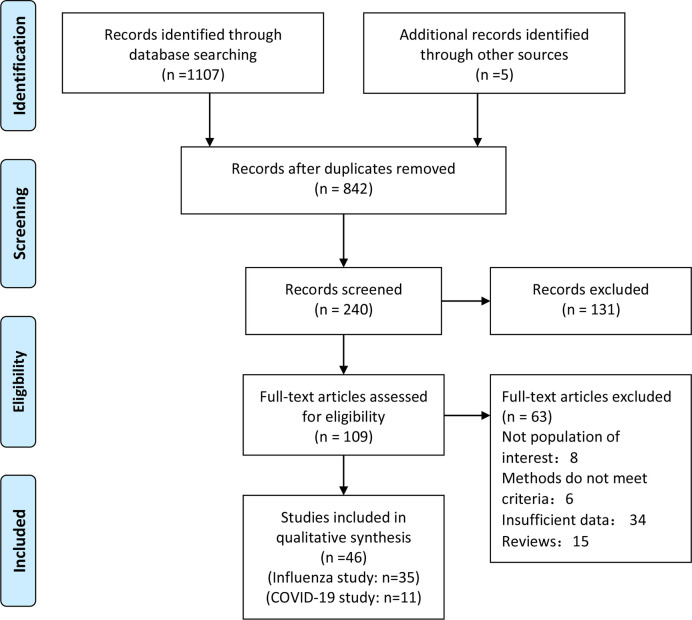
After careful selection, a total of 46 studies were included in the present meta-analysis; 11/46 studies were COVID-19 studies (11, 19–28), and 35/46 studies were influenza studies (29–61). A total of 4,023,895 patients were included for the studies on influenza, and 9,787 patients were included in the COVID-19 studies. The procedure of literature selection based on the PRISMA statement is shown in Figure 1. Details about the characteristics of the included studies are shown in Tables 1 and 2. The included studies were published between 2009 and 2020. Of the included COVID-19 studies, 4 were conducted in the United States, 3 were from China, and 1 each was from France, Singapore, Italy, and Mexico, respectively. Of the included influenza studies, 12 were conducted in the United States, 4 were from Spain, 6 were from China, 3 were from Canada, 2 were from UK, and 1 each was from the following countries: Mexico, Serbia, France, Iran, Romania, France, Brazil, Australia, and South Africa. The studies varied in sample size from 48 to 3,076,699. In addition, 41/46 studies enrolled both males and females, and 5 did not show the gender characteristic. Study quality assessment according to NOS is shown in Tables 1 and 2.
Figure 1.
Flowchart on the literature selection process in this meta-analysis.
Table 1.
Characteristics of included studies on the infection, hospitalization, severity, and mortality of influenza.
| Author | Country | Year | Number | Women (%) | Age | Groups | Disease outcome | OR or RR (95% CI) | NOS |
|---|---|---|---|---|---|---|---|---|---|
| Ren et al. (29) | China | 2013 | 686 | 48.40% | 5-60 | Overweight; Obesity |
Severe influenza manifestation | Overweight: 3.70(2.04, 6.72) Obesity: 35.61 (7.96, 159.21) |
7 |
| Maier et al. (30) | US | 2018 | 1783 | 74% | 0-92 | Obesity | Influenza | 2.04 (1.35, 3.09) | 6 |
| Segaloff et al. (31) | US | 2017 | 48 | 23% | 21-91 | Obesity Morbid obesity |
Severe influenza outcomes | Obesity: ICU: 2.9 (0.5, 20.9); LRD: 2.1 (0.5, 8.6) Morbid obesity: ICU: 7.9 (0.9, 87.1); LRD: 4.0 (0.6, 35.0) |
6 |
| Moser et al. (32) | Mexico | 2018 | 3248 | 64.25% | 41.2 ± 16.2 | Underweight; Obesity; morbid obesity | hospitalization | Underweight: 5.20 (1.67, 16.01) Obesity: 3.18 (1.73, 5.91) Morbid obesity: 18.4 (7.83, 47.4) |
5 |
| Neidich et al. (33) | US | 2017 | 1022 | 64.68% | 54 ± 15 | Obesity | Influenza risk | Obesity: 2.01 (1.12, 3.06) | 5 |
| Murphy et al. (34) | UK | 2016 | 6984 | 53.94% | 35-63 | Obesity | Influenza-like illness | Obesity: 1.16 (0.97, 1.38) | 6 |
| Yang et al. (35) | China | 2013 | 66820 | 65.75% | 65+ | Underweight; Overweight; Obesity; Morbid obesity |
influenza-associated mortality | Underweight: 1.081 (1.013, 1.154) Overweight: 0.981 (0.936, 1.028) Obesity: 1.018 (0.980, 1.058) Morbid obesity: 1.062 (0.972, 1.162) |
6 |
| Cocoros et al. (36) | US | 2014 | 8266 | 59.63% | 48+ | Overweight; Obesity |
Influenza-like illness | Overweight: 1.54 (0.56, 4.27) Obesity: 1.90 (0.68, 5.27) |
6 |
| Dragana et al. (37) | Serbia | 2017 | 777 | 48.26% | 65+ | Obesity | Admission to ICU | Obesity: 3.32 (1.36, 8.14) | 6 |
| Charland et al. (38) | US | 2012 | 3076699 | N/A | 0-80+ | Obesity | Hospitalization | Obesity: 1.12 (1.07, 1.17) | 6 |
| Braun et al. (39) | US | 2015 | 9048 | 65.6% | 20+ | Underweight; Overweight; Obesity; Morbid obesity |
Influenza severity (admission to ICU) |
Underweight: 1.13 (0.86, 1.49) Overweight: 0.80 (0.70, 0.94) Obesity: 0.90 (0.76, 1.08) Morbid obesity: 0.91 (0.77, 1.09) |
5 |
| Coleman et al. (40) | US | 2012 | 2623 | 65.42% | 45 ± 17 | Obesity; Morbid obesity |
Influenza | Obesity: 0.95 (0.75, 1.20) Morbid obesity: 1.10 (0.8, 1.52) |
6 |
| Morgan et al. (41) | US | 2010 | 594 | N/A | N/A | Obesity; Morbid obesity |
Hospitalization; Death |
Obesity: hospitalization: 1.5 (0.8, 2.8); death: 4.9 (2.4, 9.9) Morbid obesity: hospitalization: 3.1 (1.5, 6.6); death: 7.6 (2.1, 27.9) |
6 |
| Halvorson et al. (42) | US | 2018 | 2811 | 61% | 22+ | Overweight; Obesity; Morbid obesity |
Hospitalization | Overweight: 0.8 (0.6, 1.0) Obesity: 0.7 (0.5, 1.0) Morbid obesity: 0.9 (0.6, 1.2) |
6 |
| Van Kerkhove et al. (62) | US | 2015 | 11086 | 10.5% | 28-40 | obesity | Hospitalization severe outcomes | Obesity: 1.6 (1.2, 2.1) | 7 |
| Louie et al. (43) | US | 2010 | 534 | 52% | 46 (20, 92) | Morbid obesity | Death | Morbid obesity: 2.8 (1.4, 5.9) | 6 |
| Jime´nez-Garcı´a et al. (44) | Spain | 2012 | 11499 | 54.2% | 18+ | Obesity | Death | Obesity: 1.88 (1.07, 3.92) | 5 |
| Díaz et al. (45) | Spain | 2011 | 416 | 41.93% | 43.1 ± 12.2 | Obesity | Death | Obesity: 1.56 (0.95, 2.54) | 6 |
| Tempia et al. (46) | South Africa | 2016 | 465 | 64.95% | 5+ | Obesity | Hospitalization | Obesity: 12.1 (1.6, 88.8) | 6 |
| Martin et al. (47) | US | 2013 | 161 | 35.4% | 40-46 | Obesity | Hospitalization; death | Hospitalization: 2.93(1.50, 5.71) death: 5.33 (0.61, 46.71) |
5 |
| Bijani et al. (48) | Iran | 2016 | 55 | 43.6% | 25.7 ± 16.9 | Obesity | Severe manifestation | Obesity: 0.89 (0.08, 10.43) | 5 |
| Cui et al. (49) | China | 2010 | 68 | N/A | 41 (18, 66) | Obesity | Death | Obesity: 23.06 (0.95, 2.54) | 7 |
| Santa-Olalla Peralta et al. (63) | Spain | 2010 | 3025 | N/A | 38 (0,94) | Obesity | Severe outcomes | Obesity: 2.01 (1.38, 2.94) | 6 |
| Gilca et al. (50) | Canada | 2011 | 716 | 54.05% | 5+ | Obesity; Morbid obesity | Hospitalization; ICU or death | Obesity: hospitalization: 1.3 (0.8, 2.0); death: 1.0 (0.5, 2.3) Morbid obesity: hospitalization: 2.0 (0.6, 6.2); death: 0.4 (0.09, 2.0) |
6 |
| Lenzi et al. (51) | Brazil | 2011 | 4740 | 53.31% | 0-90 | Obesity | Hospitalization | Obesity: 2.994 (1.638, 5.472) | 5 |
| Yu et al. (52) | China | 2011 | 9966 | 44% | 22 (11, 39) | Obesity | Severe outcomes | Obesity: 1.54 (1.35, 1.76) | 6 |
| Viasus et al. (53) | Spain | 2010 | 585 | 48.7% | 39 (16, 87) | Morbid obesity | Severe outcomes | Morbid obesity: 6.7 (2.25, 20.19) | 6 |
| Tang et al. (53) | China | 2010 | 457 | 42.23% | 25 (6, 42) | Overweight; Obesity |
Severe outcomes | Overweight: 3.13 (1.83, 5.36) Obesity: 4.05 (1.72, 9.52) |
6 |
| Karki et al. (55) | Australia | 2018 | 246494 | 46.99% | 50+ | Obesity; Morbid obesity |
Influenza incidence; Hospitalization | Incidence: Obesity: 1.27 (1.10, 1.46) Morbid obesity: 1.69 (1.24, 2.29) Hospitalization: Obesity: 1.57 (1.22, 2.01); Morbid obesity: 4.81 (3.23, 7.17) |
9 |
| Zhou et al. (56) | China | 2015 | 65841 | 66.14% | 65+ | Obesity | Influenza mortality | Obesity: 1.19 (1.01, 1.42) | 8 |
| Campitelli et al. (57) | Canada | 2014 | 396581 | 48.92% | 18-64 | Overweight; Obesity; Morbid obesity |
Acute respiratory infection for influenza | Overweight: 1.10 (1.07, 1.13) Obesity: 1.17 (1.13, 1.22) Morbid obesity: 1.19 (1.12, 1.25) |
8 |
| Kwong et al. (58) | Canada | 2011 | 82545 | 50.49% | 18+ | Obesity; Morbid obesity |
Hospitalization | Obesity: 1.45 (1.03, 2.05) Morbid obesity: 2.12 (1.45, 3.10) |
9 |
| Pițigoi et al. (59) | Romania | 2019 | 345 | 55.9% | 74 (68, 80) | Obesity | Hospitalization | Obesity: 2.1 (1.3, 3.4) | 7 |
| Guerrisi et al. (60) | France | 2019 | 6992 | 61% | 0-75 | Underweight Overweight; Obesity |
Influenza-like illness | Underweight:0.92(0.77,1.11) Overweight:1.18(1.08,1.29) Obesity:1.28(1.14,1.44) |
8 |
| Myles et al. (61) | UK | 2012 | 1520 | 52.6% | 26(9,44) | Obesity | Severe outcomes | Obesity:2.22(1.18,4.18) | 7 |
Table 2.
Characteristics of included studies on the severity and mortality of COVID-19.
| Author | Country | Year | Number | Women (%) | Age | Group | Outcome | OR (95%CI) | NOS score |
|---|---|---|---|---|---|---|---|---|---|
| Simonnet et al (11). | France | 2020 | 124 | 27% | 60 (51, 70) | Obesity; Morbid obesity |
Severe manifestation; ICU | Obesity:3.45(0.83,14.31) Morbid obesity: 7.36 (1.63, 33.14) |
6 |
| Cai et al (19). | China | 2020 | 383 | 52.21% | 48 (39, 54) | Overweight; Obesity |
Severe manifestation; ICU | Overweight: 1.84 (0.99, 3.43) Obesity: 3.4 (1.4, 8.26) |
7 |
| Wu et al (20). | China | 2020 | 280 | 46% | 43.12 ± 19 | Obesity | Severe influenza outcomes | Obesity: 1.3 (1.09, 1.54); | 5 |
| Lighter et al (21). | US | 2020 | 3615 | N/A | N/A | Obesity; morbid obesity | Severe manifestation; ICU | Obesity: 1.8 (1.2, 2.7) Morbid obesity: 3.6 (2.5, 5.3) |
5 |
| Ong et al (22). | Singapore | 2020 | 182 | 60% | 43 (27, 52) | Obesity | Severe manifestation; ICU | Severe manifestation: 6.32 (1.23, 32.34) ICU: 3.13 (0.57, 17.13) |
5 |
| Gao et al (23). | China | 2020 | 150 | 37.3% | 35-63 | Obesity | Severe manifestation and ICU | Obesity: 3 (1.22, 7.38) | 6 |
| Pettie et al (24). | US | 2020 | 238 | 52.5% | 58.5 ± 17 | Obesity | mortality | Obesity: 1.7 (1.1, 2.8) | 6 |
| Hajifathalian et al (24). | US | 2020 | 770 | 39.2% | 64 ± 16.7 | Obesity | ICU and mortality | ICU: 1.76 (1.24, 2.48) mortality: 1.15 (0.62, 2.14) |
7 |
| Busetto et al (26). | Italy | 2020 | 92 | 38.1% | 70.5 ± 13.3 | Obesity | Admission to ICU; death | ICU: 11.65 (3.88, 34.96) mortality: 0.27 (0.03, 2.05) |
6 |
| Palaiodimos et al (27). | US | 2020 | 200 | 51% | 64 (54, 73.5) | Morbid obesity | mortality | Morbid obesity: 3.78 (1.45, 9.83) | 7 |
| Denova-Gutiérrez et al (28). | Mexico | 2020 | 3844 | 42% | 45.4 ± 15.8 | Obesity | Severe outcome; ICU | Obesity: 1.43 (1.11, 1.83) | 6 |
Obesity Increases the Risk of Influenza Infection and Hospitalization
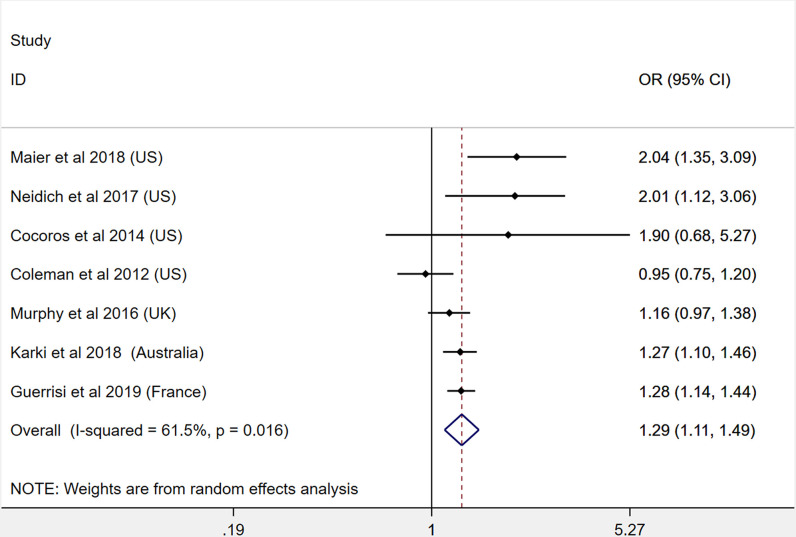
A total of 7 studies were included for the meta-analysis of obesity and influenza infection risk (30, 33, 34, 36, 40, 55, 60). Our pooled analysis shows that patients with obesity had a significantly higher risk for influenza infection (OR: 1.29, 95% CI: 1.11-1.49, I2: 61.5%, n=7). This result is presented in Figure 2. Due to the heterogeneity between the included studies, we performed subgroup analysis according to different regions. The results show that the heterogeneity was decreased in non–North American countries (Supplement Figure 1).
Figure 2.
Odds ratios for influenza infection in patients with obesity versus patients without obesity.
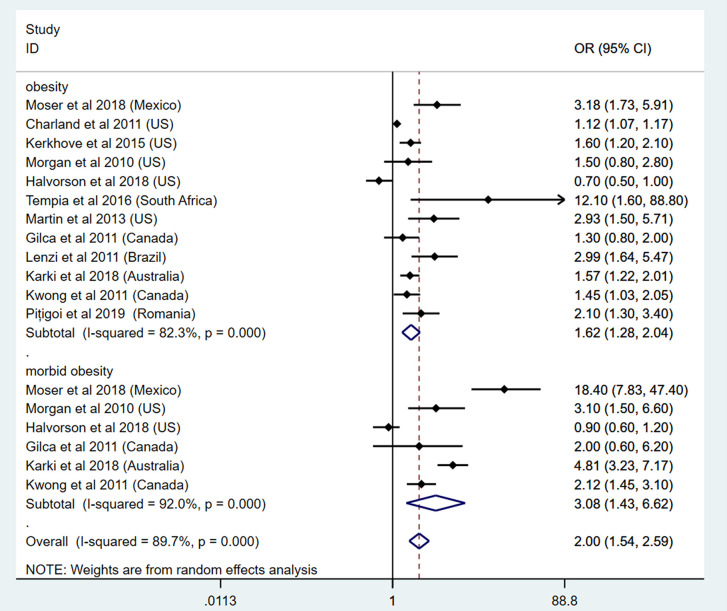
As for the risk of hospitalization, 18 studies were included in this part. To specify the effect of obesity classes on influenza hospitalization, 12 studies focused on the link between obesity and influenza hospitalization (32, 38, 41, 42, 46, 47, 50, 51, 55, 58, 59, 62). Among these, 6 studies focused on the link between morbid obesity and influenza hospitalization (32, 41, 42, 50, 55, 58). Our results show that patients with obesity had an increased risk for hospitalization because of influenza (OR: 1.62, 95% CI: 1.28-2.04, I2: 82.3%, n=12). In addition, patients with morbid obesity had extremely higher risk for hospitalization (OR: 3.08, 95% CI: 1.43-6.62, I2: 92%, n=6). The overall analysis showed consistent results (OR: 2.00, 95% CI: 1.54-2.59, I2: 89.7%, n=18). This result is presented in Figure 3. As for the subgroup analysis, the heterogeneity between the included studies did not show any decrease after subgroup analysis by different regions (Supplement Figure 1).
Figure 3.
Odds ratios for influenza-induced hospitalization in patients with obesity and morbid obesity.
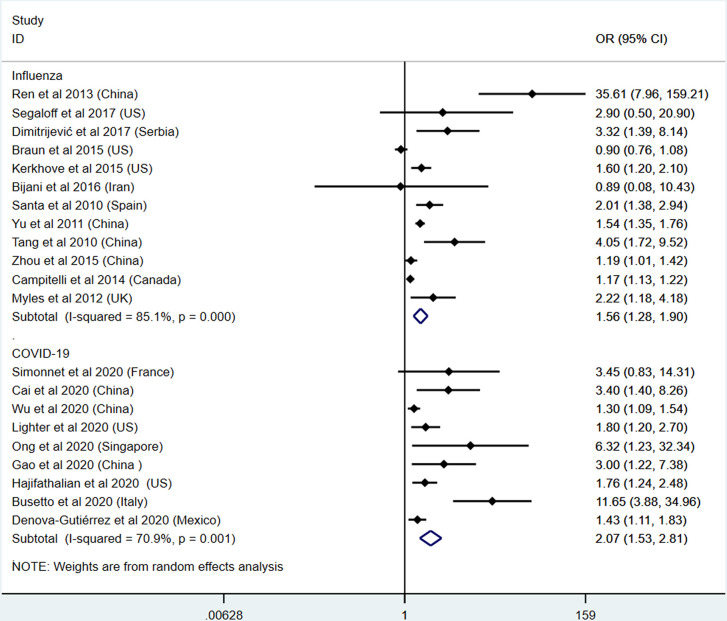
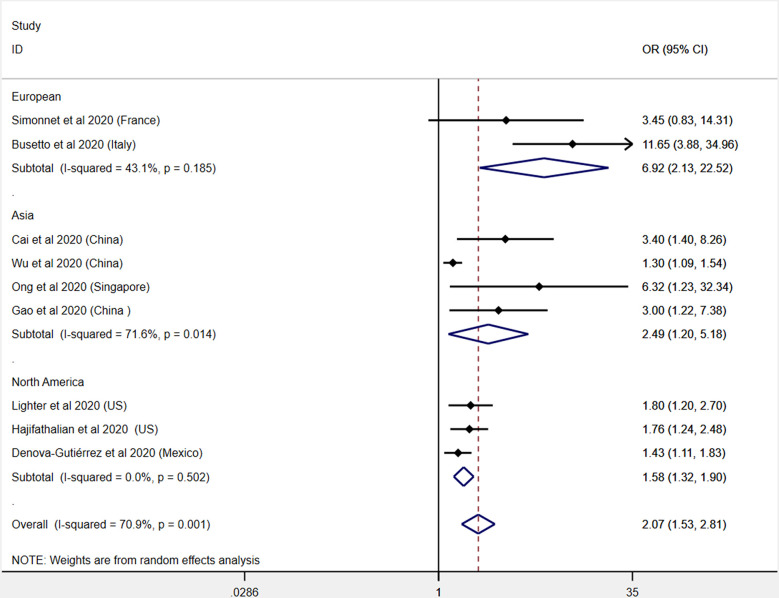
Obesity Aggravates Disease Severity and Increases the Risk of ICU Admission in Both Influenza and COVID-19
The severe outcomes consist of severe manifestations, admission to ICU, and requirement for mechanical supports. In this section, 12 influenza studies and 9 COVID-19 studies were included (11, 19–23, 25, 26, 28–31, 37, 39, 48, 52, 54, 56, 57, 61, 62). The pooled analysis results show that patients with obesity had an increased risk for severe outcome of both influenza (OR: 1.56, 95% CI: 1.28-1.90, I2: 85.1%, n=12) and COVID-19 (OR: 2.07, 95% CI: 1.53-2.81, I2: 70.9%, n=9). Compared with influenza, obesity patients with COVID-19 might present a higher risk for ICU admission and worse outcomes. This result is presented in Figure 4. To further explore the heterogeneity between the included studies, subgroup analysis was applied by different regions (Supplement Figure 1). The heterogeneity was significantly decreased in each subgroup of COVID-19 studies, indicating the region characteristic for the COVID-19 studies (Figure 5).
Figure 4.
Odds ratios for severe outcome or admission to ICU in patients with obesity and influenza or COVID-19.
Figure 5.
Subgroup analysis (by region) on the effects of obesity on the severity and mortality of COVID-19.
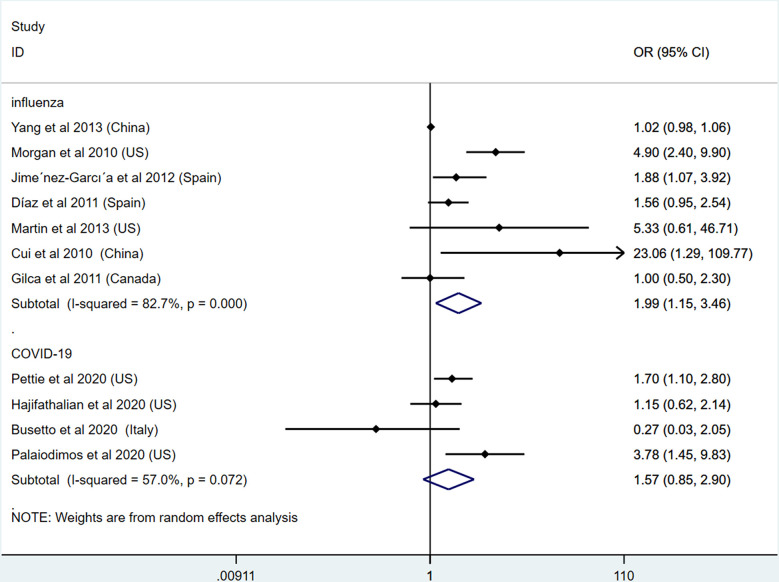
Obesity Increases the Mortality of Influenza but Has No Adverse Effect on the Mortality of COVID-19
In addition to the severe outcome of both diseases, we then detected the effects of obesity on the mortality of influenza and COVID-19. In this section, 7 studies on influenza and 4 studies on COVID-19 were included (24–27, 35, 41, 44, 45, 47, 49, 50). Our results show that patients with obesity presented higher mortality of influenza (OR: 1.99, 95% CI: 1.15-3.46, I2: 82.7%, n=7). However, inconsistent with influenza studies, our results show no link between obesity and mortality of COVID-19 (OR: 1.57, 95% CI: 0.85-2.90, I2: 57%, n=12). This result demonstrates that, although obesity could aggravate the severe outcome of COVID-19, obesity does not increase the death rate based on available studies. This result is presented in Figure 6. To further explore the heterogeneity of the included studies, subgroup analysis was applied by different regions (Supplement Figure 1).
Figure 6.
Odds ratios for the mortality of patients with obesity and influenza or COVID-19.
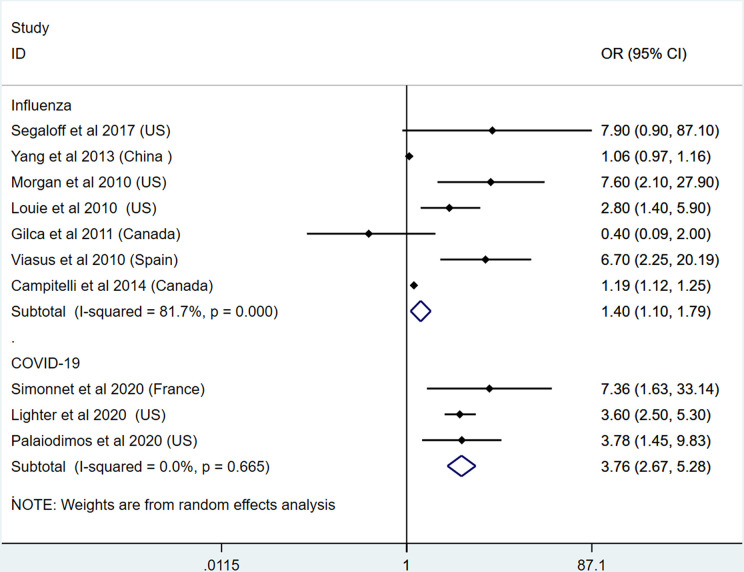
Morbid Obesity Is Linked to Severity and Mortality of Both Influenza and COVID-19
To detect the effects of different obesity classes on the severity and mortality of influenza and COVID-19, we applied the meta-analysis on morbid obesity studies. In this section, 7 studies on influenza and 3 studies on COVID-19 were included (11, 21, 27, 31, 35, 41, 43, 50, 53, 57). The results show that morbid obesity is a significant predictor or risk factor for the severe outcomes and death of influenza (OR: 1.40, 95% CI: 1.10-1.79, I2: 81.7%, n=7) and COVID-19 (OR: 3.76, 95% CI: 2.67-5.28, I2: 0%, n=3). Compared with influenza, COVID-19 infection in patients with morbid obesity induced higher mortality. This result is presented in Figure 7. Due to the limited number of studies, subgroup analysis was not performed.
Figure 7.
Odds ratios for severe outcome and mortality in patients with morbid obesity and influenza or COVID-19.
Publication Bias Assessment and Sensitivity Assessment
Begg’s tests were applied to evaluate publication bias. Because of the limited number of studies included in each section, no conclusive information was found after Begg’s tests and sensitivity assessment. The results are shown in Supplement Figure 1.
Discussion
The Influence of Obesity on the Severity and Mortality of Influenza and COVID-19
In the present meta-analysis, we systematically reviewed studies focusing on the influence of obesity on the severity and mortality of influenza and COVID-19. The results show obesity could increase the risk and severe outcomes of both influenza and COVID-19. Higher mortality of influenza was found in patients with obesity. Compared with influenza, COVID-19 patients with obesity present higher risk of severe outcomes and admission to ICU but not mortality. These results indicate the characteristic of COVID-19, which is higher infection rate and lower mortality. Thus, more strategies on weight control and physical regulation should be encouraged to decrease the risk of COVID-19 infection and its development.
The impact of different obesity classes on the severity and mortality of COVID-19 was unclear so far. In the present meta-analysis, we analyzed the relationship between morbid obesity and severity or mortality of COVID-19. The results show patients with morbid obesity have higher risk for the severe outcome of COVID-19. Different from patients with obesity, morbid obesity is linked with higher mortality. Thus, patients with morbid obesity should be given more attention, especially when they are infected with COVID-19. However, available evidence in this field is extremely limited. More studies should be conducted to explore the different impacts of obesity classes on the outcome of COVID-19.
Because the severe outcomes of COVID-19 are influenced by multiple factors (64), obesity might be one of the important influencing factors. Obesity could induce and aggravate the severe clinical manifestations of COVID-19 through influencing metabolism, inflammation, immune responses, and other pathways (65). At the same time, other factors, such as age, diabetes, hypertension, and cardiovascular diseases, can also cooperate with obesity to play a part in the development of COVID-19 (66). Thus, to discuss more influencing factors of severe COVID-19 is of great value.
In the present meta-analysis, we performed a subgroup analysis to discuss the heterogeneity of the included studies. Different regions were chosen as parameters to evaluate the heterogeneity. The results show significant decreased heterogeneity in the regions of Europe and North America in COVID-19 studies, indicating the existence of specific regional characteristics of COVID-19 (67). For the included studies on influenza, we did not find a valuable factor that could be used as a parameter to decrease the heterogeneity. Common parameters used for subgroup analysis, such as age and sex, are not suitable in the present studies. Because some studies did not provide enough information on these influencing factors, it is difficult to conduct subgroup analysis. Future studies should pay more attention to detecting more influencing factors on the severity and mortality of COVID-19.
Numerous studies have indicated the influenza vaccination could help to protect patients with obesity from the risk of influenza (68). However, its effect on COVID-19 is not clear so far, and available information is controversial. Because of the coming winter, it will be a great challenge for the global healthcare systems because the epidemic of influenza season is on the way. Due to the lack of a COVID-19 vaccine, the immunization for influenza might be helpful to prevent the epidemic wave of seasonal influenza and the co-circulation of both influenza and COVID-19 (69). A study from Zanettini et al. shows the influenza vaccination is helpful to reduce the mortality of COVID-19 in the elderly population (70). However, the effect of the influenza vaccination on other populations in preventing COVID-19 risk is quite limited and needs more evidence in this field (71). High influenza vaccine uptake rates in a well-matched season between the circulating influenza strains and the vaccine influenza strains could reduce the epidemiological noise of influenza during the COVID-19 epidemic. Thus, for patients with obesity, children, elders, pregnant women, and patients with chronic diseases, the influenza vaccination is highly advised.
Strengths
To our knowledge, this is the first meta-analysis to compare the effects of obesity on the severity and mortality of influenza and COVID-19. In addition to a rigorous methodology to conduct the meta-analysis, we also applied subgroup analysis, evaluation of publication bias, and sensitivity analysis. To further explore the risk-increasing effect of obesity specifically, we also performed analysis comparing BMI classes with each other.
Limitations
One significant limitation of the present study is that the majority of the included studies are retrospective studies. Because the pandemic of influenza and COVID-19 are not designed or planned, it is difficult to conduct the cohort study further. Besides this, the high heterogeneity of included studies does limit the ability to accurately estimate the size of the effects. Moreover, the BMI definition and the criteria for the admission to ICU might be different across different countries, which might influence the final results to some degree. For the assessment of publication bias, we tried to apply the Begg’s test. Sensitivity analysis was also performed. However, due to the limited number of included studies and high heterogeneity, no conclusive information was provided.
Implications for Future Research
Based on available evidence, obesity or BMI should be considered as an important parameter for a COVID-19 risk assessment model. More studies in this field are encouraged to further examine whether obesity is an independent risk factor or predictor. Besides this, future studies should include detailed anthropometric parameters of patients with COVID-19. Moreover, basic research exploring the underlying mechanism of COVID-19 and obesity are urgently needed in the near future.
Conclusion
Consistent with influenza, COVID-19 patients with obesity and morbid obesity present with a higher risk for severe outcome and admission to ICU. No correlation was found between obesity and mortality of COVID-19. Thus, obesity or BMI should be recommended as important parameters for COVID-19 risk assessment. Special monitoring and earlier treatment should be implemented in COVID-19 patients with elevated BMI. Furthermore, prevention of obesity and regular physical activity are important methods to fight against the COVID-19 pandemic.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.
Author Contributions
XZ and GW designed the study. XZ and QH wrote the paper. XG and GH selected the paper. ZL and YL did the data extraction and analysis. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by grants (GW) from the National Natural Science Fund of China (81670732, 81970687) and Department of Science and Technology of Jilin Province(201909010006JC, 20170623005TC). This work was also supported by grants (XZ) from the National Natural Science Fund of China (81900726) and the 10th Youth Project of the First Hospital of Jilin University (JDYY102019025).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2020.595109/full#supplementary-material
References
- 1. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet (2020) 395:1054–62. 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yu N, Li W, Kang Q, Xiong Z, Wang S, Lin X, et al. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-centre, descriptive study. Lancet Infect Dis (2020) 20:559–64. 10.1016/S1473-3099(20)30176-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Short KR, Kedzierska K, van de Sandt CE. Back to the Future: Lessons Learned From the 1918 Influenza Pandemic. Front Cell Infect Microbiol (2018) 8:343. 10.3389/fcimb.2018.00343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mertz D, Kim TH, Johnstone J, Lam PP, Science M, Kuster SP, et al. Populations at risk for severe or complicated influenza illness: systematic review and meta-analysis. BMJ (2013) 347:f5061. 10.1136/bmj.f5061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kitahara CM, Flint AJ, Berrington de Gonzalez A, Bernstein L, Brotzman M, MacInnis RJ, et al. Association between class III obesity (BMI of 40-59 kg/m2) and mortality: a pooled analysis of 20 prospective studies. PloS Med (2014) 11:e1001673. 10.1371/journal.pmed.1001673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg (2020) 78:185–93. 10.1016/j.ijsu.2020.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zhao X, Han Q, Liu Y, Sun C, Gang X, Wang G. The Relationship between Branched-Chain Amino Acid Related Metabolomic Signature and Insulin Resistance: A Systematic Review. J Diabetes Res (2016) 2016:2794591–2794591. 10.1155/2016/2794591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhao X, Han Q, Gang X, Wang G. Altered brain metabolites in patients with diabetes mellitus and related complications - evidence from (1)H MRS study. Biosci Rep (2018) 38:1–13. 10.1042/BSR20180660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Karlsson EA, Beck MA. The burden of obesity on infectious disease. Exp Biol Med (Maywood) (2010) 235:1412–24. 10.1258/ebm.2010.010227 [DOI] [PubMed] [Google Scholar]
- 10. Jain S, Chaves SS. Obesity and influenza. Clin Infect Dis (2011) 53:422–4. 10.1093/cid/cir448 [DOI] [PubMed] [Google Scholar]
- 11. Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, et al. Obesity study, High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation. Obesity (Silver Spring) (2020) 28:1195–9. 10.1002/oby.22831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Luzi L, Radaelli MG. Influenza and obesity: its odd relationship and the lessons for COVID-19 pandemic. Acta Diabetol (2020) 57:759–64. 10.1007/s00592-020-01522-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Xiang YT, Li W, Zhang Q, Jin Y, Rao WW, Zeng LN, et al. Timely research papers about COVID-19 in China. Lancet (2020). 10.1016/S0140-6736(20)30375-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clin Res ed.) (2009) 339:b2700–0. 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bray GA, Heisel WE, Afshin A, Jensen MD, Dietz WH, Long M, et al. The Science of Obesity Management: An Endocrine Society Scientific Statement. Endocr Rev (2018) 39:79–132. 10.1210/er.2017-00253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhai P, Ding Y, Wu X, Long J, Zhong Y, Li Y. The epidemiology, diagnosis and treatment of COVID-19. Int J Antimicrob Agents (2020) 55:105955. 10.1016/j.ijantimicag.2020.105955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vemula SV, Zhao J, Liu J, Wang X, Biswas S, Hewlett I. Current Approaches for Diagnosis of Influenza Virus Infections in Humans. Viruses (2016) 8:96. 10.3390/v8040096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lo CK-L, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol (2014) 14:45–5. 10.1186/1471-2288-14-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cai Q, Chen F, Wang T, Luo F, Liu X, Wu Q, et al. Obesity and COVID-19 Severity in a Designated Hospital in Shenzhen. China Diabetes Care (2020) 43:1392–8. 10.2337/dc20-0576 [DOI] [PubMed] [Google Scholar]
- 20. Wu J, Li W, Shi X, Chen Z, Jiang B, Liu J, et al. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19). J Intern Med (2020) 288:128–38. 10.1111/joim.13063 [DOI] [PubMed] [Google Scholar]
- 21. Jennifer L, Michael P, Sarah H, Stephanie S, Diane J, Fritz F, et al. Obesity in patients younger than 60 years is a risk factor for Covid-19 hospital admission. Clin Infect Dis (2020) 71:896–97. 10.1093/cid/ciaa415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ong SWX, Young BE, Leo Y-S, Lye DC. Association of higher body mass index (BMI) with severe coronavirus disease 2019 (COVID-19) in younger patients. Clin Infect Dis Off Publ Infect Dis Soc America (2020). ciaa548. 10.1093/cid/ciaa548 [DOI] [PMC free article] [PubMed]
- 23. Gao F, Zheng KI, Wang XB, Sun QF, Pan KH, Wang TY, et al. Obesity Is a Risk Factor for Greater COVID-19 Severity. Diabetes Care (2020) 43:e72–4. 10.2337/dc20-0682 [DOI] [PubMed] [Google Scholar]
- 24. Pettit NN, MacKenzie EL, Ridgway J, Pursell K, Ash D, Patel B, et al. Obesity is Associated with Increased Risk for Mortality Among Hospitalized Patients with COVID-19. Obesity (Silver Spring) (2020) 28:1806–10. 10.1002/oby.22941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hajifathalian K, Kumar S, Newberry C, Shah S, Fortune B, Krisko T, et al. Obesity is associated with worse outcomes in COVID-19: Analysis of Early Data From New York City. Obesity (Silver Spring) (2020) 28:1606–12. 10.1002/oby.22923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Busetto L, Bettini S, Fabris R, Serra R, Dal Pra C, Maffei P, et al. Obesity and COVID-19: an Italian snapshot. Obesity (Silver Spring) (2020) 28:1600–05. 10.1002/oby.22918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Palaiodimos L, Kokkinidis DG, Li W, Karamanis D, Ognibene J, Arora S, et al. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism (2020) 108:154262. 10.1016/j.metabol.2020.154262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Denova-Gutierrez E, Lopez-Gatell H, Alomia-Zegarra JL, Lopez-Ridaura R, Zaragoza-Jimenez CA, Dyer-Leal DD, et al. The association between obesity, type 2 diabetes, and hypertension with severe COVID-19 on admission among Mexicans. Obesity (Silver Spring) (2020) 28:1826–32. 10.1002/oby.22946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ren Y-y, Yin Y-y, Li W-q, Lin Y, Liu T, Wang S, et al. Risk factors associated with severe manifestations of 2009 pandemic influenza A (H1N1) infection in China: a case-control study. Virol J (2013) 10:149–9. 10.1186/1743-422X-10-149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Maier HE, Lopez R, Sanchez N, Ng S, Gresh L, Ojeda S, et al. Obesity Increases the Duration of Influenza A Virus Shedding in Adults. J Infect Dis (2018) 218:1378–82. 10.1093/infdis/jiy370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Segaloff HE, Evans R, Arshad S, Zervos MJ, Archer C, Kaye KS, et al. The impact of obesity and timely antiviral administration on severe influenza outcomes among hospitalized adults. J Med Virol (2018) 90:212–8. 10.1002/jmv.24946 [DOI] [PubMed] [Google Scholar]
- 32. Moser JS, Galindo-Fraga A, Ortiz-Hernandez AA, Gu W, Hunsberger S, Galan-Herrera JF, et al. Underweight, overweight, and obesity as independent risk factors for hospitalization in adults and children from influenza and other respiratory viruses. Influenza Other Respir Viruses (2019) 13:3–9. 10.1111/irv.12618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Neidich SD, Green WD, Rebeles J, Karlsson EA, Schultz-Cherry S, Noah TL, et al. Increased risk of influenza among vaccinated adults who are obese. Int J Obes (Lond) (2017) 41:1324–30. 10.1038/ijo.2017.131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Murphy R, Fragaszy EB, Hayward AC, Warren-Gash C. Investigating obesity as a risk factor for influenza-like illness during the 2009 H1N1 influenza pandemic using the Health Survey for England. Influenza Other Respir Viruses (2017) 11:66–73. 10.1111/irv.12420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Yang L, Chan KP, Lee RS, Chan WM, Lai HK, Thach TQ, et al. Obesity and influenza associated mortality: evidence from an elderly cohort in Hong Kong. Prev Med (2013) 56:118–23. 10.1016/j.ypmed.2012.11.017 [DOI] [PubMed] [Google Scholar]
- 36. Cocoros NM, Lash TL, DeMaria, Jr. A, Klompas M. Obesity as a risk factor for severe influenza-like illness. Influenza Other Respir Viruses (2014) 8:25–32. 10.1111/irv.12156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Dragana D, Dragan I, Slavica RA, Vesna S, Mijomir P, Goran S, et al. Diseases, Predictors of Hospitalization and Admission to Intensive Care Units of Influenza Patients in Serbia through Four Influenza Seasons from 2010/2011 to 2013/2014. Jpn J Infect Dis (2017) 70:275–83. 10.7883/yoken.JJID.2016.210 [DOI] [PubMed] [Google Scholar]
- 38. Charland KM, Buckeridge DL, Hoen AG, Berry JG, Elixhauser A, Melton F, et al. Relationship between community prevalence of obesity and associated behavioral factors and community rates of influenza-related hospitalizations in the United States. Influenza Other Respiratory Viruses (2013) 7:718–28. 10.1111/irv.12019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Braun ES, Crawford FW, Desai MM, Meek J, Kirley PD, Miller L, et al. Obesity not associated with severity among hospitalized adults with seasonal influenza virus infection. Infection (2015) 43:569–75. 10.1007/s15010-015-0802-x [DOI] [PubMed] [Google Scholar]
- 40. Coleman LA, Waring SC, Irving SA, Vandermause M, Shay DK, Belongia EA. Evaluation of obesity as an independent risk factor for medically attended laboratory-confirmed influenza. Influenza Other Respir Viruses (2013) 7:160–7. 10.1111/j.1750-2659.2012.00377.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Morgan OW, Bramley A, Fowlkes A, Freedman DS, Taylor TH, Gargiullo P, et al. Morbid obesity as a risk factor for hospitalization and death due to 2009 pandemic influenza A(H1N1) disease. PloS One (2010) 5:e9694. 10.1371/journal.pone.0009694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Halvorson EE, Peters TR, Skelton JA, Suerken C, Snively BM, Poehling KA. Is weight associated with severity of acute respiratory illness? Int J Obes (Lond) (2018) 42:1582–9. 10.1038/s41366-018-0044-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Louie JK, Acosta M, Samuel MC, Schechter R, Vugia DJ, Harriman K, et al. A novel risk factor for a novel virus: obesity and 2009 pandemic influenza A (H1N1). Clin Infect Dis (2011) 52:301–12. 10.1093/cid/ciq152 [DOI] [PubMed] [Google Scholar]
- 44. Jimenez-Garcia R, Hernandez-Barrera V, Rodriguez-Rieiro C, Lopez de Andres A, de Miguel-Diez J, Jimenez-Trujillo I, et al. Hospitalizations from pandemic Influenza [A(H1N1)pdm09. infections among type 1 and 2 diabetes patients in Spain. Influenza Other Respir Viruses (2013) 7:439–47. 10.1111/j.1750-2659.2012.00419.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Diaz E, Rodriguez A, Martin-Loeches I, Lorente L, Del Mar Martin M, Pozo JC, et al. Impact of obesity in patients infected with 2009 influenza A(H1N1). Chest (2011) 139:382–6. 10.1378/chest.10-1160 [DOI] [PubMed] [Google Scholar]
- 46. Tempia S, Walaza S, Moyes J, Cohen AL, von Mollendorf C, Treurnicht FK, et al. Risk Factors for Influenza-Associated Severe Acute Respiratory Illness Hospitalization in South Africa, 2012-2015. Open Forum Infect Dis (2017) 4:ofw262. 10.1093/ofid/ofw262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Martin ET, Archer C, McRoberts J, Kulik J, Thurston T, Lephart P, et al. Epidemiology of severe influenza outcomes among adult patients with obesity in Detroit, Michigan, 2011. Influenza Other Respir Viruses (2013) 7:1004–7. 10.1111/irv.12115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bijani B, Pahlevan AA, Qasemi-Barqi R, H.J.I.M. Jahanihashemi Metabolic syndrome as an independent risk factor of hypoxaemia in influenza A (H1N1) 2009 pandemic. Le infezioni in Medicine (2016) 24:123–30. [PubMed] [Google Scholar]
- 49. Cui W, Zhao H, Lu X, Wen Y, Zhou Y, Deng B, et al. Factors associated with death in hospitalized pneumonia patients with 2009 H1N1 influenza in Shenyang. China BMC Infect Dis (2010) 10:145. 10.1186/1471-2334-10-145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gilca R, De Serres G, Boulianne N, Ouhoummane N, Papenburg J, Douville-Fradet M, et al. Risk factors for hospitalization and severe outcomes of 2009 pandemic H1N1 influenza in Quebec, Canada. Influenza Other Respir Viruses (2011) 5:247–55. 10.1111/j.1750-2659.2011.00204.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lenzi L M.Â., Silva LR, Grochocki MH, Pontarolo R. Pandemic influenza A (H1N1) 2009: risk factors for hospitalization. J Bras Pneumol (2012) 38:57–65. 10.1590/S1806-37132012000100009 [DOI] [PubMed] [Google Scholar]
- 52. Yu H, Feng Z, Uyeki TM, Liao Q, Zhou L, Feng L, et al. Risk Factors for Severe Illness with 2009 Pandemic Influenza A (H1N1) Virus Infection in China. Clin Infect Dis (2011) 52:457–65. 10.1093/cid/ciq144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Viasus D, Pano-Pardo JR, Pachon J, Campins A, Lopez-Medrano F, Villoslada A, et al. Novel Influenza, Factors associated with severe disease in hospitalized adults with pandemic (H1N1) 2009 in Spain. Clin Microbiol Infect (2011) 17:738–46. 10.1111/j.1469-0691.2010.03362.x [DOI] [PubMed] [Google Scholar]
- 54. Tang F, Huo X, Li L, Zu RQ, Xu K, Qi X, et al. T., Risk factors for severe cases of influenza A H1N1. Acta Universitatis Med Nanjing Natural Sci (2010) 30:1262–5. 10.1360/972010-923 [DOI] [Google Scholar]
- 55. Karki S, Muscatello DJ, Banks E, MacIntyre CR, McIntyre P, Liu B. Association between body mass index and laboratory-confirmed influenza in middle aged and older adults: a prospective cohort study. Int J Obes (Lond) (2018) 42:1480–8. 10.1038/s41366-018-0029-x [DOI] [PubMed] [Google Scholar]
- 56. Zhou Y, Cowling BJ, Wu P, Chan WM, Lee SY, Lau EH, et al. Adiposity and influenza-associated respiratory mortality: a cohort study. Clin Infect Dis (2015) 60:e49–57. 10.1093/cid/civ060 [DOI] [PubMed] [Google Scholar]
- 57. Campitelli MA, Rosella LC, Kwong JC. The association between obesity and outpatient visits for acute respiratory infections in Ontario, Canada. Int J Obes (Lond) (2014) 38:113–9. 10.1038/ijo.2013.57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Kwong JC, Campitelli MA, Rosella LC. Obesity and respiratory hospitalizations during influenza seasons in Ontario, Canada: a cohort study. Clin Infect Dis (2011) 53:413–21. 10.1093/cid/cir442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Pițigoi D, Nițescu M, Streinu-Cercel A, Bacruban R, Ivanciuc AE, Lazăr M, et al. Characteristics of influenza in elderly patients with and without diabetes, hospitalized for severe acute respiratory infection in a tertiary care hospital from Bucharest Romania - a three-year prospective epidemiological surveillance study. Germs (2019) 9:142–7. 10.18683/germs.2019.1169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Guerrisi C, Ecollan M, Souty C, Rossignol L, Turbelin C, Debin M, et al. Factors associated with influenza-like-illness: a crowdsourced cohort study from 2012/13 to 2017/18. BMC Public Health (2019) 19:879. 10.1186/s12889-019-7174-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Myles PR, Semple MG, Lim WS, Openshaw PJ, Gadd EM, Read RC, et al. Predictors of clinical outcome in a national hospitalised cohort across both waves of the influenza A/H1N1 pandemic 2009-2010 in the UK. Thorax (2012) 67:709–17. 10.1136/thoraxjnl-2011-200266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Van Kerkhove MD, Cooper MJ, Cost AA, Sanchez JL, Riley S. Risk factors for severe outcomes among members of the United States military hospitalized with pneumonia and influenza, 2000-2012. Vaccine (2015) 33:6970–6. 10.1016/j.vaccine.2015.09.115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Santa-Olalla Peralta P, Cortes-García M, Vicente-Herrero M, Castrillo-Villamandos C, Arias-Bohigas P, Pachon-del Amo I, et al. Risk factors for disease severity among hospitalised patients with 2009 pandemic influenza A (H1N1) in Spain, April - December 2009. Eurosurvllance (2010) 15(38):19667. 10.2807/ese.15.38.19667-en [DOI] [PubMed] [Google Scholar]
- 64. Foldi M, Farkas N, Kiss S, Zadori N, Vancsa S, Szako L, et al. Obesity is a risk factor for developing critical condition in COVID-19 patients: A systematic review and meta-analysis. Obes Rev (2020) 21:e13095. 10.1111/obr.13095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Smith SM, Boppana A, Traupman JA, Unson E, Maddock DA, Chao K, et al. Impaired glucose metabolism in patients with diabetes, prediabetes, and obesity is associated with severe COVID-19. J Med Virol (2020). 10.1002/jmv.26227 [DOI] [PMC free article] [PubMed]
- 66. Kalligeros M, Shehadeh F, Mylona EK, Benitez G, Beckwith CG, Chan PA, et al. Association of Obesity with Disease Severity Among Patients with Coronavirus Disease 2019. Obesity (Silver Spring Md.) (2020) 28:1200–4. 10.1002/oby.22859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Jin Y, Yang H, Ji W, Wu W, Chen S, Zhang W, et al. Virology, Epidemiology, Pathogenesis, and Control of COVID-19. Viruses (2020) 12:372. 10.3390/v12040372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wolff GG. Influenza vaccination and respiratory virus interference among Department of Defense personnel during the 2017-2018 influenza season. Vaccine (2020) 38(2020):350–4. 10.1016/j.vaccine.2019.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Maltezou HC, Theodoridou K, Poland G. Influenza immunization and COVID-19. Vaccine 38(2020):6078–9. 10.1016/j.vaccine.2020.07.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Zanettini C, Omar M, Dinalankara W, Imada EL, Colantuoni E, Parmigiani G, et al. Influenza Vaccination and COVID19 Mortality in the USA. Preprint medRxiv (2020). 10.1101/2020.06.24.20129817 [DOI] [PMC free article] [PubMed]
- 71. Thindwa D, Garcia Quesada M, Liu Y, Bennett J, Cohen C, Knoll MD, et al. Use of seasonal influenza and Pneumococcal polysaccharide vaccines in older adults to reduce COVID-19 mortality. Vaccine (2020) 38:5398–401. 10.1016/j.vaccine.2020.06.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding authors.