Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic has affected every country on earth, and family physicians (FPs) have helped patients at every stage. The first objective of our study was to study the FPs' knowledge about COVID-19 and second objective was to assess their attitudes, stress and death anxiety surrounding the current pandemic.
Materials and Methods
An online questionnaire was prepared to collect responses from FPs between March-April 2020. A descriptive and correlational design was utilized.
Results
240 FPs from eight countries were evaluated. The majority reported that they received most information from medical journals (77%). Most of the respondents also noted that the most common symptoms were acute respiratory syndrome and fever - with the most effective treatment in most cases consisting of symptomatic treatment (41%). Although FPs generally had a positive attitude, most of them (68%) were concerned about contacting COVID-19 from patients and as a result, they experienced increased stress (64%).
Conclusion
The research was conducted during the COVID-19 outbreak while the FPs were working on the frontline of the pandemic. This research revealed that most of the FPs had good knowledge of, and a positive attitude towards COVID-19 treatment. It was observed that participants who tended towards conscientiousness, emotional stability, and openness to experience, and who had higher life satisfaction, and lower levels of death anxiety also reported more positive attitudes towards COVID-19. While the main target population of COVID-19 disease were the older age groups, FPs' attitudes and fear levels were not associated with age, gender, or years of experience.
Keywords: Anxiety, Fear of death, COVID-19, Family physician, Knowledge, Attitude
Introduction
During the last two decades, the world has faced a number of potentially deadly coronavirus (CoV) outbreaks that have caused severe diseases such as severe acute respiratory syndrome (SARS) and middle east respiratory syndrome (MERS) [1,2]. At the end of 2019, a novel CoV, designated later as SARS-CoV-2, appeared in Wuhan, China and caused many deaths worldwide [3]. As of July 8, 2020 there have been more than 11,669,000 confirmed cases of coronavirus disease 2019 (COVID-19) globally, including about 539,000 confirmed deaths, in 215 countries, areas or territories with cases, as reported by World Health Organization (WHO) [4].
Coronaviruses are a large family of viruses that cause illness ranging from a common cold to life threatening diseases. The novel COVID-19 has been shown to be the cause of human respiratory failure. To prevent and/ or treat the diseases caused by COVID-19, vaccine and pharmaceutical studies are currently underway. Therefore, applying preventive measures to reduce the spread of the virus is of most importance. The WHO and the Centers for Disease Control and Prevention (CDC) have published recommendations for the prevention and control of COVID-19 infections in health care settings. This includes hand hygiene and the wearing of personal protective equipment [5,6].
Health care providers (HCPs) play an important role in managing and treating patients but at the same time, they themselves face great risks [7]. During this outbreak, declared as a global public health emergency, thousands of HCPs have been infected and have died from COVID-19 while caring for patients fighting this highly contagious and fatal disease [8]. Most physicians are trained to put patients first, and are often considered heroes; however, as human beings they can experience the same emotions as others. HCPs can feel anger, sadness, fear, and anxiety, on occasions leading to suicide. Due to stigma, however, many suicides will never be reported [9,10]. Only a small number have so far come to light during the COVID-19 pandemic [11].
HCPs face great pressure due to various factors such as insufficient personal protective equipment, heavy workloads, isolation, burnout, high infection risk, family separation, and fear of transmitting the disease [12]. Family physicians (FPs) cannot avoid such situations, since they are the entry point of the healthcare system [13]. Acute respiratory tract infections are among the most common reasons for visiting a FP [14].
In the early stages of pandemics, healthcare workers in Wuhan and the surrounding areas took on an enhanced sense of responsibility and spirit of teamwork in treating patients [12]. FPs were on the frontline at every stage, yet took no part in the decision-making process. In our ever-changing world, the nature of contagious diseases changes, too. How can we evaluate the attitudes of FPs in conditions in which their families, patients, and they themselves are threatened? Studies have shown that fear of the unknown and insecurity can lead to the development of mental health disorders, stress, anxiety and depression [15]. Mass tragedies - such as infectious disease pandemics - can cause waves of increased fear, leading to disturbances in the daily functioning and well-being of large portions of the population including physicians [16]. The main factors to influence the attitudes and behaviours of the physicians are likely to be their COVID-19 knowledge levels, but fear of death, satisfaction of life, perceived stress, and personality traits also play an important role [17]. It is also important to focus on those factors for the better understanding of planned behavior towards COVID-19.
To our knowledge, there are few studies conducted among FPs to gauge their knowledge and attitude towards COVID-19 till date. It is a well-known fact that healthcare workers, especially Family Medicine physicians, work in the frontline and deal with the emotional side of medicine every day. Their role in tackling the pandemic is crucial. Despite this, the known information about their knowledge, attitudes and practices towards SARS-Cov-2 is extremely limited. Our study has created additional insight into the knowledge and attitude of FPs towards COVID-19 and further policy action (improved training, counseling to prevent burnout) can be taken, if it is required.
Our hypothesis for this study was that FPs have good knowledge and positive attitudes towards COVID-19. Furthermore, we suggested, that the higher the physical well-being in terms of quality of life of the physicians and the lower the levels of fear, anxiety, and stress, the more positive their attitudes towards patients with COVID-19 will be.
Thus, we aimed to evaluate, in addition to the knowledge and the attitude, the relationship between FPs' knowledge and attitudes of COVID-19, with their behaviours, psychosocial factors, and personality traits, utilized during the treatment of these patients.
Materials and Methods
This cross-sectional study was based on an internet E-survey of a convenience sample of family physicians in eight countries from March-April 2020. Our total sample size was approximately 240 FPs from eight countries; however, to compensate for possible dropouts, we decided on a sample size of 250. We used a purposive sampling method. The participants were told the time that the survey would take, which data would be stored, where and for how long, who the investigators were, and the purpose of the study. We used a pretested questionnaire, developed in Google Forms, consisting of 4 sections: 1) Introduction page, 2) General information section with demographic and socio-economic characteristics of the participants, 3) Section with questions regarding knowledge, attitudes and practices during the COVID-19 epidemic, 4) Section with four scales to measure personality traits and physical and mental wellbeing. The study protocol was reviewed and approved by the Izmir University of Economics Ethical Committee (approval no:B.30.2.IEÜSB.0.05.05-20-062). Consent for participation was given by each participant digitally. Data was collected and protected by the principal investigator in an encrypted hard drive. The electronic questionnaire (in English) was pilot tested before being sent out. It was an open survey with participant recruitment via the Internet. The survey and its objectives were promoted across multiple communication channels, such as social media and email groups. The responses were entered directly into a database. Our survey was voluntary, and no incentives were offered. The questions were set in a Google form in such a way to allow easy checking for completeness by the investigators. We noted unique variables such as view rate, participation rate, and completion rate. We also maintained a log file for analysis. No methods such as weighting of items or propensity scores had been used to adjust for the non-representative sample. The scales used for this research were:
1. For assessment of knowledge component, responses are categorized as “Definitely not”, “Probably not”, “Possibly”, “Probably”, “Very probably” and “Definitely”. We considered that participants who responded “Possibly”, “Probably”, “Very probably” and “Definitely”, had good knowledge, as conceptualization of this novel disease was changing regularly. For assessment of attitude, we categorized our positive statements into three orders: “Disagree”, “Neither agree nor disagree”, and “Agree”. We considered FPs who responded, “Agree” to the statements to have a positive attitude (>50% average score).
2. The Ten-Item Personality Inventory (TIPI), to assess the personality predisposition of the participant (Extraversion, Agreeableness, Conscientiousness, Emotional Stability, Openness to Experience). TIPI is a brief assessment, consisting of 2 items for each of the 5 domains represented in the Five Factor Model (FFM) of personality [18]. One item contains two desirable and two undesirable descriptors (e.g. for Extraversion: extraverted, enthusiastic, and reserved, quiet). Each of the ten items are rated on a 7-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree). This scale was chosen because of its brevity and simplicity. The proper psychometric properties of the TIPI were demonstrated in several studies and countries [19,20,21].
3. Satisfaction with life scale (SWLS): This is a short 5-item instrument to measure global cognitive judgments of satisfaction with one's life, ranging from 5 (extremely dissatisfied with life) to 35 (extremely satisfied), with a score of 20 representing a neutral point on the scale [22]. The SWLS was shown to be a valid and reliable measure of life satisfaction in several studies, suited for use in various population groups, which makes possible the savings of interview time and resources compared to other life satisfaction tools [23,24,25].
4. Perceived stress scale: The Perceived Stress Scale (PSS) is a Ten Item Scale and it is the most widely used psychological instrument for measuring the perception of stress, ranging from 0 (never stressed) to 4 (very often stressed). Scores ranging from 0 - 13 are considered low stress; 14 - 26, moderate stress; and 27 - 40, high perceived stress. The psychometric properties of the PSS have been assessed in different cultures worldwide and has been found to have adequate validity and reliability in various populations [26,27].
5. Death anxiety scale: Templer Death Anxiety Scale (DAS) developed by Donald I. Templer [28] measures the extent of death anxiety a person experiences. This is a scale based on ten factors i.e., 1) Externally caused deaths, 2) The thought of death, 3) Excruciating pain, 4) Fear of surgery, 5) The image of death, 6) Death proximity, 7) Presence of death, 8) Death anxiety denial, 9) Dreams of death, and 10) Death thoughts, with true/false rating options. Score ranges 15 - 35 are perceived as low death anxiety, 36 - 55, as moderate, and 56 - 75, as high death anxiety. The DAS has good psychometric properties and had been used in hundreds of studies [29,30,31].
Data was accordingly analyzed using SPSS version 21 (IBM, Chicago, IL, USA). Descriptive statistics, correlational and group comparison analyses were utilized. Non-parametric tests of Spearman rho, Mann Whitney U and Kruskal Wallis H tests were used due to the normality violation.
Results
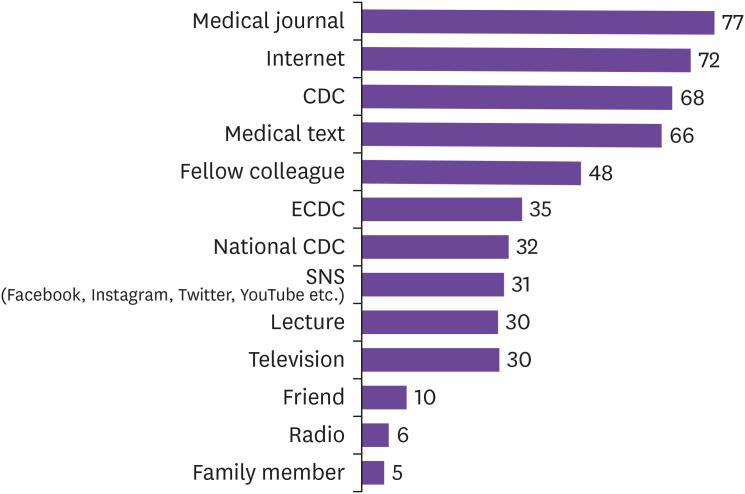
Respondents were 250 FPs with a knowledge of English from different countries. Of the sample, 146 (58%) were female, and 3 (1%) preferred not to report gender. Age and years of work experience, respectively, ranged from 24 to 68 (M = 40.58, SD = 8.88), and 1 to 43 (M = 12.35, SD = 8.96). Additionally, 103 (41%) FPs reported contacting at least one infectious disease from a patient. The participant breakdown across the various countries were 58 (23%) from Turkey, 56 (22%) from Greece, 42 (17%) from the United States, 11 (4%) from Portugal, 6 (2%) from Spain, 5 (2%) from Italy, 4 (2%) from Canada and 61 (24%) for all other countries. We asked the respondents to report their sources of information about the COVID-19 virus. The greatest number (77%) reported medical journals as a source. Other major primary sources were the internet (72%), the CDC (68%) and medical texts (66%). In addition to the sources of information listed in Figure 1, other reported sources were WHO, workplaces, governmental institutions, medical organizations, and newspapers.
Figure 1. Sources of information about COVID-19 (%).
Table 1 shows FPs' knowledge about the transmission of COVID-19. The majority (93%) of respondents reported that the virus would most likely be transmitted by spending more than 15 minutes within 2 meters of a confirmed case through direct physical contact in the same place and/or closed environment such as classroom, hospital, airplane, or any kind of transportation without protection. Total 96% of FPs reported that healthcare professionals and laboratory workers having direct physical contact with a confirmed case without recommended personal protective equipment could also be at risk.
Table 1. Knowledge about the transmission of COVID-19, n (%).
| Items | Definitely not | Probably not | Possibly | Probably | Very probably | Definitely |
|---|---|---|---|---|---|---|
| A person living in the same house with a symptomatic, laboratory confirmed COVID-19 case | 5 (2) | 6 (2) | 17 (7) | 32 (13) | 117 (47) | 73 (29) |
| A person who has been in direct physical contact (e.g. shaking hands) with a confirmed COVID-19 case | 4 (2) | 8 (3) | 43 (17) | 51 (20) | 108 (43) | 36 (14) |
| A person having direct contact with infectious secretions of a confirmed COVID-19 case without protection (e.g. being coughed on or touched used paper tissues without gloves) | 3 (1) | 1 (<1) | 19 (8) | 25 (10) | 95 (38) | 107 (43) |
| A person having had face contact or spent more than 15 minutes within 2 meters of an infected COVID-19 person | 6 (2) | 13 (5) | 41 (16) | 43 (17) | 97 (39) | 50 (20) |
| A person who spent 15 minutes or more and at a distance of less than 2 meters with a COVID-19 case, in a closed environment (e.g. classroom, meeting room, hospital waiting room, etc.) | 3 (1) | 8 (3) | 30 (12) | 49 (20) | 99 (40) | 61 (24) |
| A healthcare professional or other person providing direct care for a COVID-19 case, or laboratory workers handling and processing specimens from a COVID-19 case without recommended PPE | 1 (<1) | 6 (2) | 27 (11) | 43 (17) | 94 (38) | 79 (32) |
| Airplane passengers seated within two seats in any direction of the COVID-19 case, travel companions or persons providing care or crew members who had close contact with the COVID-19 case | 4 (2) | 11 (4) | 41 (16) | 62 (25) | 91 (34) | 41 (16) |
| A person who spent less than 15 min or at a distance of more than 2 meters, in a closed environment with a COVID-19 case | 7 (3) | 64 (26) | 73 (29) | 68 (27) | 27 (11) | 11 (4) |
| A person having had face-to-face contact for less than 15 min and at a distance of less than 2 meters, with a COVID-19 case | 5 (2) | 35 (14) | 64 (26) | 58 (23) | 65 (26) | 23 (9) |
| Traveling together with a COVID-19 case in any kind of transportation | 6 (2) | 27 (11) | 72 (29) | 68 (27) | 54 (22) | 23 (9) |
COVID-19, coronavirus disease 2019; PPE, personal protective equipment.
According to the majority of respondents, as illustrated in Table 2, acute respiratory syndrome and fever are considered among most common symptoms of COVID-19, while other possible symptoms mentioned are fatigue, joint and muscle pain, headache, sore throat, nausea and vomiting. They reported it was not possible for redness of the eyes, rashes, polyuria, and internal and external bleeding to be considered symptoms of the virus.
Table 2. Knowledge about the symptoms of COVID-19, n (%).
| Items | Definitely not | Probably not | Possibly | Probably | Very probably | Definitely |
|---|---|---|---|---|---|---|
| Fever | - | 2 (1) | 50 (20) | 42 (17) | 102 (41) | 54 (22) |
| Fatigue | - | 11 (4) | 79 (32) | 61 (24) | 80 (32) | 19 (8) |
| Joint and muscle pain | 1 (<1) | 17 (7) | 86 (34) | 68 (27) | 64 (26) | 14 (6) |
| Headache | 1 (<1) | 11 (4) | 114 (47) | 70 (28) | 44 (18) | 10 (4) |
| Sore throat | 1 (<1) | 26 (10) | 82 (33) | 55 (22) | 66 (26) | 20 (8) |
| Nausea and vomiting | 5 (2) | 47 (19) | 108 (43) | 66 (26) | 22 (9) | 2 (1) |
| Redness of the eyes | 10 (4) | 89 (36) | 88 (35) | 36 (14) | 25 (10) | 2 (1) |
| Rashes | 23 (9) | 141 (56) | 56 (22) | 21 (8) | 9 (4) | - |
| Polyuria | 53 (21) | 146 (58) | 32 (26) | 13 (5) | 6 (2) | - |
| Internal and external bleeding | 54 (22) | 125 (50) | 49 (20) | 18 (7) | 4 (2) | - |
| Acute respiratory distress syndrome | 3 (1) | 4 (2) | 38 (15) | 40 (16) | 102 (41) | 63 (25) |
COVID-19, coronavirus disease 2019.
As shown in Table 3, 41% of respondents reported that the most effective treatment for COVID-19 could be symptomatic treatment, but 61% reported that antibiotics were probably not a proper treatment method. Antivirals and immunoglobulins were other possible treatments mentioned.
Table 3. Knowledge about the treatment of COVID-19, n (%).
| Items | Definitely not | Probably not | Possibly | Probably | Very probably | Definitely |
|---|---|---|---|---|---|---|
| Symptomatic | 6 (2) | 4 (2) | 52 (21) | 43 (17) | 43 (17) | 102 (41) |
| Antivirals | 18 (7) | 23 (9) | 75 (30) | 48 (19) | 53 (21) | 33 (13) |
| Antibiotics | 103 (41) | 51 (20) | 45 (18) | 31 (12) | 14 (6) | 6 (2) |
| Immunoglobulins | 28 (11) | 43 (17) | 85 (34) | 44 (18) | 41 (16) | 9 (4) |
COVID-19, coronavirus disease 2019.
The participants generally reported a positive attitude towards COVID-19 (>60%). As seen in Table 4, they mostly agreed with the personal issues relating to the need to provide care to a COVID-19 patient, be a volunteer, work at a treatment center and attend workshops about the prevention of COVID-19. However, of those, 50% reported that they would discourage family members/friends volunteering for a COVID-19 vaccine trial.
Table 4. Attitude towards COVID-19, n (%).
| Items | Disagree | Neither disagree nor agree | Agree |
|---|---|---|---|
| I would be willing to be a volunteer in COVID-19 vaccine trial | 93 (37) | 52 (21) | 105 (42) |
| I would encourage family members/friends to be volunteers in COVID-19 vaccine trial | 124 (50) | 58 (23) | 68 (27) |
| I would be willing to work in the COVID-19 treatment/isolation center | 66 (26) | 34 (14) | 150 (60) |
| I would like to attend any workshop/training in COVID-19 prevention | 18 (7) | 14 (6) | 218 (87) |
| I would provide care for a patient with COVID-19 | 27 (11) | 21 (8) | 202 (81) |
| Not to provide care to a patient with COVID-19 is not ethical | 31 (12) | 20 (8) | 199 (80) |
COVID-19, coronavirus disease 2019.
We further asked the respondents about the incubation period of COVID-19 in the final section of knowledge about the virus in the questionnaire. 83% of the participants reported an incubation period of 2 to 14 days; 15%, of 14 to 21 days; and 2%, of 21 to 28 days. No one reported an incubation period of more than 28 days.
Table 5 shows the numbers and percentages relating to the fear of COVID-19 among FPs. 68% were worried about contacting COVID-19 from a patient, and 64% reported stress related to this. Three out of four also reported a fear of infecting family or friends as a result of providing care to confirmed cases.
Table 5. Fear of COVID-19, n (%).
| Items | Disagree | Neither disagree nor agree | Agree |
|---|---|---|---|
| I am worried about contacting COVID-19 from a patient | 53 (21) | 27 (11) | 170 (68) |
| I feel stressed when I think of acquiring COVID-19 as a result of patient care | 61 (24) | 29 (12) | 160 (64) |
| I am afraid to put my family/friends at risk of COVID-19, when I provide care to a patient with COVID-19 | 40 (16) | 23 (9) | 187 (75) |
COVID-19, coronavirus disease 2019.
The means, standard deviations and Spearman rho correlations are given in Table 6. Attitude towards COVID-19 was significantly and positively associated with the personality traits of conscientiousness, r (250) = 0.22, P <0.01, emotional stability, r (250) = 0.20, P <0.01, openness to experience, r (250) = 0.17, P <0.01, and satisfaction with life, r (250) = 0.26, P <0.01, but there was a significant inverse correlation between attitude and death anxiety, r (250) = -0.22, P <0.01. Those with a tendency towards conscientiousness, emotional stability, and openness to experience, and who were more satisfied with life, and had less death anxiety also reported a more positive attitude towards COVID-19. Fear of COVID-19 had a significant positive correlation only with death anxiety, r (250) = 0.27, P <0.01. Those with higher death anxiety reported higher fear of COVID-19.
Table 6. Means, standard deviations, and Spearman rho correlations.
| Variables | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Extraversion | 4.15 | 1.41 | |||||||||
| 2. Agreeableness | 4.87 | 1.06 | −0.19a | ||||||||
| 3. Conscientiousness | 5.35 | 1.10 | 0.05 | 0.25a | |||||||
| 4. Emotional stability | 4.78 | 1.24 | 0.13b | 0.23a | 0.27a | ||||||
| 5. Openness to experience | 5.21 | 1.08 | 0.31a | 0.11 | 0.37a | 0.21a | |||||
| 6. Satisfaction with life | 24.58 | 5.77 | 0.10 | 0.07 | 0.13b | 0.27a | 0.03 | ||||
| 7. Perceived stress | 17.47 | 6.09 | −0.14b | −0.08 | −0.17a | −0.40a | −0.08 | −0.43a | |||
| 8. Death anxiety | 6.56 | 3.01 | −0.18a | 0.02 | −0.16b | −0.24a | −0.13b | −0.24a | 0.43a | ||
| 9. Attitude towards COVID-19 | 4.92 | 1.10 | 0.04 | 0.08 | 0.22a | 0.20a | 0.17a | 0.26a | −0.11 | −0.22a | |
| 10. Fear of COVID-19 | 5.13 | 1.34 | −0.07 | 0.12 | 0.09 | −0.09 | 0.01 | −0.02 | 0.06 | 0.27a | −0.07 |
aP <0.01, (2-tailed).
bP <0.05.
Lastly, attitude towards and fear of COVID-19 were analyzed and compared across groups regarding demographic and occupational information. This included gender, age, and working experience in countries having more than thirty participants. Age was associated with neither attitude, r (250) = 0.08, P = 0.22, nor fear, r (250) = -0.04, P < 0.54. Years of working experience was also unrelated to attitude, r (250) = 0.10, P = 0.11, or fear, r (250) = -0.07, P = 0.29. No significant results were further found between the genders for attitude, U = 6,655, P = 0.19, or fear, U = 7,225, P = 0.79.
Despite the insignificant difference in attitude, U = 7,331, P = 0.67, between groups, a Mann-Whitney U test showed that those who had never caught an infectious disease from a patient reported higher fear of COVID-19 (Mdn = 5.33) than those who had at least once (Mdn = 5), U = 6,249, P = 0.02. A Kruskal-Wallis H test indicated that there were statistically significant differences in the attitudes toward COVID-19 scores, χ 2 (2) = 24.30, P <0.001, between Greece, Turkey and United States, but no significant result was found for the fear of COVID-19 across the countries, χ 2 (2) = 3.87, P = 0.14. The mean ranks were 69 for Greece, 66 for Turkey and 108 for the United States. Bonferroni corrections and mean ranks provided evidence of more positive attitudes towards COVID-19 in the United States compared to Greece and Turkey.
Discussion
This research was conducted during the COVID-19 outbreak when the FPs were on the frontline of the pandemic. It is important for front-liners like FPs to have the most up-to-date medical information about prevention, symptoms, treatment and guidelines [27]; therefore, it is necessary to gauge their knowledge, attitude and mental wellbeing related to COVID-19.
Our study showed good knowledge about the SARS-2 coronavirus in terms of infection, prevention, symptoms and therapeutic approach and mostly positive attitudes towards the patients with COVID-19. Similar findings were observed in the study of Zhou M. et al [17], where the majority of the participants demonstrated sufficient knowledge of COVID-19, and this is important as knowledge directly affects attitudes. Our findings revealed that medical journals were the main source of their knowledge. This may be due to day by day the knowledge evolving knowledge about COVID-19 and due to current trend of info-demics, the FPs kept them updated through authentic knowledge resources like medical journals and it is a good sign.
Given the mode of transmission, FPs in contact with COVID-19 patients were expected to have a high risk of infections. Previous clinical studies have shown that the prevalence of MERS among FPs in contact with infected patients ranged from 0.3% to 20.9%. In our study, most of the FPs opined that use of personal protective equipment is crucial to reducing the transmission. They also recommended the use of gowns, gloves and surgical masks for droplet precaution, which reflects their good knowledge of COVID-19 prevention.
Regarding sign and symptoms, the majority of respondents correctly knew the most common symptoms of COVID-19. Similar findings were observed in the study of Zhou M. et al [17]. However, the majority of them wrongly believed that redness of the eyes, rashes, polyuria, and internal and external bleeding may not happen in COVID-19. It may be because we conducted this study in early phases (evolving phase) of COVID-19 and those above-mentioned symptoms may not be described in the medical literature at that time.
We found that participants tending conscientiousness, emotional stability, and openness to experience, and who were more satisfied with life, and had less death anxiety reported more positive attitudes towards COVID-19. This could be explained by the “realistic threat” of COVID-19 pandemics; Kachanoff et al reported that such a realistic threat predicted greater self-reported compliance. Described as “An almost perfect killing machine”, COVID-19 is a realistic threat [32]. FPs who were open to experience and more satisfied with life were able to cope with the threat more easily.
Stress is defined as an adaptive psychophysical reaction in response to a physical, social, or psychological stimulus. Our study revealed that FPs were under moderate stress (mean score-17.3). Thus, the ability to cope with stress is the key to managing the COVID-19 crisis. Flesia et al. performed a study among 2,053 participants, and revealed that the importance of three key personal qualities: calmness, emotional balance and a sense of acceptance [33]. These qualities are also helpful for managing patients and their families in emergency situations, as well as for chronic disease management.
The target population of COVID-19 has different features according to age, but FPs' attitudes, and fear condition is unaffected by age, gender, or years of experience. The reason, it could be speculated, was that COVID-19 was a new experience to all the FPs.
Bonferroni corrections and mean ranks provided evidence that attitudes towards COVID-19 in the United States were more positive than in Greece and Turkey. Flores argues that culture influences clinical care, and may have clinical results in the relationship between patients and physicians. Normative cultural values and culture competency could contribute to this result, although another possible reason is that Greece and Turkey have hosted a much larger refugee population than other countries recently, and this is a realistic challenge not only for the family physicians, but also for the community structure of these two countries [34]. There are also cultural factors; according to Hofstede et al, uncertainty avoidance and power distance in Greece and Turkey is higher than in the United States [35]. Hofstede et al. also revealed that the USA scores higher on individualism, which is associated with the most positive reactions, while Turkey and Greece are more collectivist in nature [35,36]. In contrast, death anxiety is universal [37], explaining the lack of significant difference across the countries.
Our study concluded that our study participants had good knowledge and positive attitude towards COVID-19. The attitude component was especially positive among those who tended towards conscientiousness, emotional stability, and openness to experience, and who were more satisfied with life. The fear of COVID-19 was generally high, and particularly among those with higher death anxiety, and those who had never contacted an infectious disease from a patient.
It has been observed that “Preparedness among healthcare workers” for COVID-19 has been the focus of many researchers [35,36,37] till date. To our knowledge, no study has been conducted evaluating the knowledge and attitude among the family physicians towards COVID-19, and this is the strength of our study. Additionally, very few studies have been conducted on family physicians' behaviors, psychosocial factors, and personality traits and “fear of death” during COVID-19 which directly influences the knowledge and attitude among FPs towards COVID-19 treatment.
The target of 30 participants from each selected country (Turkey, Greece, USA, India and Portugal) [38] was reached for only three of the countries. The response rate for online surveys could be predicted as being from 52% to 81% [39]. To avoid data loss, “Forced Answering” was the method used, but this may have been one of the main reasons for the low response rate [40]. The findings shed light on family physicians' attitudes towards infectious diseases, and will increase awareness, leading to new studies in similar situations.
Recommendations: This pandemic has not ended yet. If healthcare workers are physically or mentally unwell, then their community will also suffer. The mental health of frontline workers must be well evaluated in order to create sustainable solutions. The “Warwick-Edinburgh Mental Well-being Scale” or the “Scales of Psychological Well-being Scales” could be one of the tools for this aim for further studies.
Footnotes
Conflict of Interest: No conflicts of interest.
- Conceptualization: OG, HP, SB, KH.
- Data curation: OG, HP, MB, KH.
- Formal analysis: OG, HP.
- Investigation: OG, SB, KH.
- Methodology: OG, HP, SB, EJ.
- Project administration: OG.
- Resources: OG, MB.
- Supervision: HP, SB.
- Validation: HP.
- Visualization: MB, EJ.
- Writing - original draft: OG, HP, MB, SB, KH, EJ.
- Writing - review & editing: OG, MB, SB, KH, EJ.
References
- 1.Cooke FJ, Shapiro DS. Global outbreak of severe acute respiratory syndrome (SARS) Int J Infect Dis. 2003;7:80–85. doi: 10.1016/S1201-9712(03)90001-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Omari A, Rabaan AA, Salih S, Al-Tawfiq JA, Memish ZA. MERS coronavirus outbreak: Implications for emerging viral infections. Diagn Microbiol Infect Dis. 2019;93:265–285. doi: 10.1016/j.diagmicrobio.2018.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Munster VJ, Koopmans M, van Doremalen N, van Riel D, de Wit E. A novel coronavirus emerging in China - Key questions for impact assessment. N Engl J Med. 2020;382:692–694. doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO) WHO coronavirus disease (COVID-19) dashboard 2020. [Accessed 22 September 2020]. Available at: https://covid19.who.int/
- 5.Centers for Disease Control and Prevention (CDC) Infection control guidance for healthcare rrofessionals about coronavirus (COVID-19) [Accessed 3 June 2020]. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control.html.
- 6.World Health Organization (WHO) Country & Technical Guidance - Coronavirus disease (COVID-19) [Accessed 10, July, 2020]. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/health-workers.
- 7.World Health Organization (WHO) Coronavirus disease (COVID-19) outbreak: rights, roles and responsibilities of health workers, including key considerations for occupational safety and health. [Accessed 18 March 2020]. Available at: https://www.who.int/publications/i/item/coronavirus-disease-(covid-19)-outbreak-rights-roles-and-responsibilities-of-health-workers-including-key-considerations-for-occupational-safety-and-health.
- 8.Cook T, Kursumovic E, Lennane S. Exclusive: deaths of NHS staff from covid-19 analysed. Health Serv J. 2020;2020:22. Available at: https://www.hsj.co.uk/exclusive-deaths-of-nhs-staff-from-covid-19-analysed/7027471.article. [Google Scholar]
- 9.Aasland OG. Physician suicide-why? Gen Hosp Psychiatry. 2013;35:1–2. doi: 10.1016/j.genhosppsych.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 10.Weichenthal L. Stigma surrounding physician suicides means many go unreported. [13 January 2017]. Available at: https://www.acepnow.com/article/stigma-surrounding-physician-suicides-means-many-go-unreported/?singlepage=1&theme=print-friendly.
- 11.American College of Emergency Physicians (ACEP) ACEP mourns loss of NY physician, Dr. Lorna Breen. [Accessed 27 April 2020]. Available at: https://www.acep.org/corona/COVID-19/covid-19-articles/acep-mourns-loss-of-ny-physician/
- 12.Xiong Y, Peng L. Focusing on health-care providers' experiences in the COVID-19 crisis. Lancet Glob Health. 2020;8:e740–1. doi: 10.1016/S2214-109X(20)30214-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dunlop C, Howe A, Li D, Allen LN. The coronavirus outbreak: the central role of primary care in emergency preparedness and response. BJGP Open. 2020;4:bjgpopen20X101041. doi: 10.3399/bjgpopen20X101041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hardy V, Thompson M, Keppel GA, Alto W, Dirac MA, Neher J, Sanford C, Hornecker J, Cole A. Qualitative study of primary care clinicians' views on point-of-care testing for C-reactive protein for acute respiratory tract infections in family medicine. BMJ Open. 2017;7:e012503. doi: 10.1136/bmjopen-2016-012503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin Neurosci. 2020;74:281–282. doi: 10.1111/pcn.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Balaratnasingam S, Janca A. Mass hysteria revisited. Curr Opin Psychiatry. 2006;19:171–174. doi: 10.1097/01.yco.0000214343.59872.7a. [DOI] [PubMed] [Google Scholar]
- 17.Zhang M, Zhou M, Tang F, Wang Y, Nie H, Zhang L, You G. Knowledge, attitude, and practice regarding COVID-19 among healthcare workers in Henan, China. J Hosp Infect. 2020;105:183–187. doi: 10.1016/j.jhin.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gosling SD, Rentfrow PJ, Swann WB., Jr A very brief measure of the Big-Five personality domains. J Res Pers. 2003;37:504–528. [Google Scholar]
- 19.Ehrhart MG, Ehrhart KH, Roesch SC, Chung-Herrera BG, Nadler K, Bradshaw K. Testing the latent factor structure and construct validity of the ten-item personality inventory. Pers Individ Dif. 2009;47:900–905. [Google Scholar]
- 20.Romero E, Villar P, Gómez-Fraguela XA, López-Romero L. Measuring personality traits with ultra-short scales: A study of the Ten Item Personality Inventory (TIPI) in a Spanish sample. Pers Individ Dif. 2012;53:289–293. [Google Scholar]
- 21.Nunes A, Limpo T, Lima CF, Castro SL. Short scales for the assessment of personality traits: development and validation of the portuguese Ten-Item Personality Inventory (TIPI) Front Psychol. 2018;9:461. doi: 10.3389/fpsyg.2018.00461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 23.Singelis TM, Yamada AM, Barrio C, Laney JH, Her P, Ruiz-Anaya A, Lennertz ST. Metric equivalence of the bidimensional acculturation scale, the satisfaction with life scale, and the self-construal scale across Spanish and English language versions. Hisp J Behav Sci. 2006;28:231–244. [Google Scholar]
- 24.Vassar M. A note on the score reliability for the satisfaction with life scale: an RG study. Soc Indic Res. 2008;86:47–57. [Google Scholar]
- 25.Pavot W, Diener E, Colvin CR, Sandvik E. Further validation of the satisfaction with life scale: evidence for the cross-method convergence of well-being measures. J Pers Assess. 1991;57:149–161. doi: 10.1207/s15327752jpa5701_17. [DOI] [PubMed] [Google Scholar]
- 26.Lee EH. Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res (Korean Soc Nurs Sci) 2012;6:121–127. doi: 10.1016/j.anr.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 27.Örücü MÇ, Demir A. Psychometric evaluation of perceived stress scale for Turkish university students. Stress Health. 2009;25:103–109. [Google Scholar]
- 28.Templer DI. The construction and validation of a death anxiety scale. J Gen Psychol. 1970;82:165–177. doi: 10.1080/00221309.1970.9920634. [DOI] [PubMed] [Google Scholar]
- 29.Templer DI, Awadalla A, Al-Fayez G, Frazee J, Bassman L, Connelly HJ, Arikawa H, Abdel-Khalek AM. Construction of a death anxiety scale-extended. Omega (Westport) 2006;53:209–226. [Google Scholar]
- 30.Abdel-Khalek AM. Death, anxiety, and depression: A comparison between Egyptian, Kuwaiti, and Lebanese undergraduates. Omega (Westport) 2002;45:277–287. [Google Scholar]
- 31.Thorson JA, Powell FC. A revised death anxiety scale. Death Stud. 1992;16:507–521. [Google Scholar]
- 32.Kachanoff FJ, Bigman YE, Kapsaskis K, Gray K. Measuring two distinct psychological threats of COVID-19 and their unique impacts on wellbeing and adherence to public health behaviors. 2020. [Accessed 5 May 5 2020]. Avialable at: https://www.ethicalpsychology.com/2020/05/measuring-two-distinct-psychological.html.
- 33.Flesia L, Fietta V, Colicino E, Segatto B, Monaro M. Stable psychological traits predict perceived stress related to the COVID-19 outbreak. [Accessed 24 April 2020]. Avialable at: https://psyarxiv.com/yb2h8. [DOI] [PMC free article] [PubMed]
- 34.Flores G. Culture and the patient-physician relationship: achieving cultural competency in health care. J Pediatr. 2000;136:14–23. doi: 10.1016/s0022-3476(00)90043-x. [DOI] [PubMed] [Google Scholar]
- 35.Hofstede G, Hofstede GJ, Minkov M. Cultures and Organizations: Software of the Mind. Revised and expanded 3rd ed. Maidenhead: MaGraw-Hill; 2010. [Google Scholar]
- 36.Hofstede G. Dimensionalizing cultures: The Hofstede model in context. Online readings in psychology and culture. [Accessed 1 December 2011]. Avialable at: https://scholarworks.gvsu.edu/orpc/vol2/iss1/8/
- 37.Kastenbaum R, Costa PT., Jr Psychological perspectives on death. Annu Rev Psychol. 1977;28:225–249. doi: 10.1146/annurev.ps.28.020177.001301. [DOI] [PubMed] [Google Scholar]
- 38.Bujang MA, Sa'at N, Bakar TM. Determination of minimum sample size requirement for multiple linear regression and analysis of covariance based on experimental and non-experimental studies. EpidemiolBiostatist Public Health. 2017;14:e12117 [Google Scholar]
- 39.Cull WL, O'Connor KG, Sharp S, Tang SF. Response rates and response bias for 50 surveys of pediatricians. Health Serv Res. 2005;40:213–226. doi: 10.1111/j.1475-6773.2005.00350.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Décieux PJ, Mergener A, Neufang MK, Sischka P. Implementation of the forced answering option within online surveys: Do higher item response rates come at the expense of participation and answer quality? Psihologija. 2015;48:311–326. [Google Scholar]