Abstract
The treatment landscape for metastatic urothelial cancer (mUC) beyond first-line platinum-based chemotherapy has changed significantly over the last 5 years with the recent approvals of the immune checkpoint inhibitors (ICIs), fibroblast growth factor receptor (FGFR) inhibitors and most recently Enfortumab Vedotin (EV). EV is a novel antibody–drug conjugate (ADC), that delivers monomethyl auristatin E (MMAE), a microtubule-disrupting agent, inside cells harboring the cell surface nectin-4 receptor. In mUC, EV has shown encouraging response rates and received accelerated approval from the Food and Drug Administration (FDA) in December 2019 in the post-platinum and ICI setting. EV is generally well tolerated, with the main toxicities being neuropathy, skin rash, alopecia and fatigue. Notably EV can also be administered to patients with renal dysfunction, which is commonly a concern in this patient population. EV is now being tested in combination strategies and in earlier disease settings in urothelial cancers. In this review, we will discuss its mechanism of action, clinical trials leading to FDA approval as well as ongoing trials and future directions.
Keywords: Antibody-drug conjugates, Metastatic Urothelial Carcinoma, Enfortumab Vedotin
Introduction
Urothelial cancer (UC) is the ninth most common cancer worldwide, accounting for 549,393 new cases and 199,922 deaths annually.1 UC affects men more often than women, and the median age at diagnosis is 70. The most common risk factor for UC is smoking. This, compounded with advanced age at diagnosis, results in a patient population that is generally older, frailer, and frequently has multiple comorbidities, making it challenging to administer standard treatments or enroll patients onto clinical trials. Although UC most commonly arises from the bladder, it can also arise from the urethra, ureters, and the renal calyces (upper tract). At presentation, about 70% of patients have non-muscle-invasive (NMIBC) disease, 25% muscle-invasive disease (MIBC), and 5% will already be metastatic.
Metastatic UC (mUC) has a dismal prognosis with a median overall survival (OS) of just over 1 year and even less in patients with visceral disease. In the first-line mUC setting, cisplatin-based chemotherapy remains the standard of care with objective response rates (ORRs) of approximately 50%.2 Patients who are either cisplatin-unfit or platinum-refractory pose a significant therapeutic challenge. In the platinum-refractory setting, the immune checkpoint inhibitor (ICI) Pembrolizumab, which targets the programmed cell death protein 1 (PD1) is considered the standard of care. This is based on the Keynote 045 randomized phase III study that showed Pembrolizumab significantly prolonged OS by approximately 3 months over second-line chemotherapy (10.1 versus 7.3 months, HR 0.73, p < 0.00015).3 Benefit was seen regardless of the PD-L1 expression status, and led to the broad approval of Pembrolizumab in the platinum-refractory mUC setting. However, as seen in this and other studies with the ICIs, the ORR with second-line ICIs remains relatively low, between 13% and 20%, especially in patients with visceral metastases. In Keynote 045, progression-free survival (PFS) actually favored chemotherapy, suggesting that there is likely a subset of patients with rapidly progressive disease despite treatment with ICIs. Unfortunately, treatment options remain very limited beyond platinum and ICIs. The taxanes (and in Europe, Vinflunine) have shown activity in the post-platinum setting, but are also associated with standard chemotherapy-related toxicities and have not been formally tested in the post-platinum and ICI settings.4,5
In patients with platinum-refractory mUC who have susceptible genetic alterations in FGFR2 or FGFR3, the targeted therapy Erdafitinib recently received accelerated Food and Drug Administration (FDA) approval. This was based on an open-label phase II study, which enrolled 99 patients with mUC, and showed a confirmed ORR of 40%.6 However, only 15–20% of mUC patients will have susceptible FGFR alterations and would be candidates for Erdafitinib, and FGFR screening is not yet widely available, underscoring a significant unmet need for the majority of patients in the platinum- and ICI-refractory setting.
Enfortumab Vedotin (EV) is a novel antibody–drug conjugate (ADC) which recently received FDA accelerated approval in the platinum- and ICI-refractory setting. This was based on a single-arm, phase II study in a heavily pretreated patient population showing an ORR of 44%, PFS of 5.8 months and an OS of 11.7 months.7 EV is generally well tolerated, does not require biomarker selection, and represents an important novel therapeutic strategy in mUC and will be the focus of this review.
Antibody–drug conjugate: definition and context
ADCs are an emerging class of drugs designed to increase the therapeutic index of a drug by linking cytotoxic agents to highly specific monoclonal antibodies (mAbs). As such, ADCs have higher selectivity for tumor cells compared with standard cytotoxic agents, and potentially less toxicity and fewer off-target side effects. ADCs bind to tumor-associated antigens, triggering endocytosis, internalization, and release of the cytotoxic payload in target tumor cells after lysosomal degradation.8
Ten ADCs are currently approved by the FDA in patients with solid or hematological malignancies as shown in Table 1. Overall, 283 studies are currently recruiting which assess the efficacy and safety of ADCs in patients with cancer.
Table 1.
FDA-approved ADC’s in cancer patients.
| Agents | Antibody Target | Cytotoxic agent | Indication |
| Trastuzumab Emtasine (T-DM1) * | HER2 | Emtasine | Metastatic HER2+ Breast cancer |
| Trastuzumab Deruxtecan | HER2 | Topoisomerase inhibitor | Metastatic HER2+ Breast Cancer |
| Sacituzumab Govitecan** | TROP2 | Topoisomerase inhibitor | Metastatic TN Breast Cancer |
| Enfortumab Vedotin** | Nectin-4 | Monomethyl auristatin (MMAE) | Metastatic Urothelial Cancer |
| Brentuximab Vedotin | CD 30 | Monomethyl auristatin (MMAE) | Hodgkin’s lymphoma, systemic anaplastic large cell lymphoma, other CD30-expressing peripheral T-cell lymphomas |
| Inotuzumab Ozogamicin | CD 22 | Calicheamicin | B-cell precursor acute lymphoblastic leukemia |
| Gemtuzumab Ozogamicin | CD33 | N-acetyl-gamma-calicheamicin | Acute myeloid leukemia |
| Polatuzumab Vedotin | CD79b | MMAE | Diffuse large B-cell lymphoma |
| Moxetumomab pasudotox | CD22 | Pseudomonas exotoxin A | Hairy cell leukemia |
| Belantamab Mafodotin - blmf | BCMA | Monomethyl auristatin F | Multiple Myeloma |
Abbreviations: ADC (Antibody Drug Conjugates) HER2 (Human Epidermal Growth Factor Receptor 2), TN (Triple Negative breast cancer), BCMA (B-cell maturation antigen)
First ADC approved in solid tumors **Accelerated approval
Components of an antibody–drug conjugate
An ADC has three major components.9–11 By linking the three components described below, there are fewer cytotoxic side effects to normal tissues and at the same time, increased drug concentration in target tissues.
Antibody: The antibody (Ab) is a large, Y-shaped protein which recognizes a unique epitope (antigen) on the surface of the tumor cell. Ideally the antigen should be expressed at higher levels in tumor tissue compared with normal tissue. This preferentially increases the uptake into tumor cells compared with normal cells, and may reduce toxicity. Humanized and fully human antibodies are preferred as they have less immunogenicity. Furthermore, a homogenous expression of the antigen by the tumor may increase uptake of the ADC. The accessibility of the antigen from the bloodstream is also important to maximize the availability of ADC to the target. Most antibodies used in ADCs are the IgG1 subtype. While their primarily function as carriers of the cytotoxic drug to tumor cells, some IgG1 Ab, such as the one used in EV, may also elicit antibody-dependent cellular cytotoxicity and complement-dependent cytotoxicity, which may further improve activity of ADC.12
Linker: The linker attaches the antibody to the cytotoxic agent. The linker is stable in the bloodstream and releases the drug only after binding to the target, thereby avoiding systemic toxicities. Depending on their intracellular stability and mechanism of degradation, linkers are classified as cleavable and non-cleavable. Cleavable linkers become unstable under the low pH, protease-enriched environment of lysosomes or high intracellular levels of glutathione. Non-cleavable linkers are stable and solely depend on lysosomal degradation to release their payload.
Cytotoxic Agent: The target of cytotoxic agents is either the deoxyribonucleic acid (DNA) or the microtubule network within the cell. Some payloads are small and lipophilic and can exhibit the “bystander effect,” where by the payload cytotoxic agent can diffuse into nearby cells and cause cell kill irrespective of the expression of the target antigen on their surface.12 One example of a cytotoxic payload that exerts a notable bystander effect is MMAE used in EV.
Enfortumab Vedotin
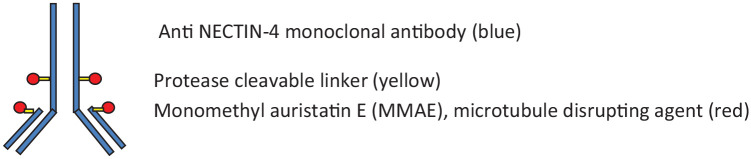
EV (ASG-22CE) is an ADC consisting of a fully human monoclonal antibody to nectin-4 which is also known as poliovirus receptor-related protein 4 (PVRL4). It is a member of the nectin family of Ca+2-independent immunoglobulin-like adhesion molecules which are involved in a number of critical cellular processes. Nectins 1–3 are expressed in adult tissue while Nectin 4 is primarily expressed in the embryo, placenta and in the skin.13 Nectin 4 is overexpressed by a number of cancers, but is particularly prevalent in UC and breast cancer, making it an ideal therapeutic target.14 The EV antibody binds with high affinity and specificity to nectin-4 expressing cells avoiding cross-reactivity with other nectin-expressing cells.15 Once bound EV is internalized, leading to the intracellular release of the microtubule-disrupting agent MMAE which leads to apoptosis of the tumor cell (Figure 1). Preclinical testing of EV in mouse and patient xenograft models demonstrated encouraging anti-tumor activity and led to further clinical evaluation.
Figure 1.
Enfortumab Vedotin Structure.
EV clinical studies
A summary of the current EV trials is shown in Table 2, with specific highlights below.
Table 2:
Key trials with Enfortumab Vedotin.
| Name/ Number | Drug | Population | Phase | EV Dose/Schedule | N | Objectives | Status/Results |
|---|---|---|---|---|---|---|---|
|
NCT02091999 EV-101 |
EV | mUC and Other Nectin-4 Expressing Solid Tumors | Phase 1 Dose Escalation |
Escalating doses up to 1.25 mg/kg on D1, D8, D15 of every 28 day cycle | 155 | Safety Tolerability, PK |
Completed ORR 43% mOS 12.3 mo |
|
NCT03219333 EV-201 |
EV | Locally Advanced or mUC Cohort 1 : Prior Platinum and ICI Cohort 2: Prior ICI, Platinum naive/ineligible |
Phase 2 | 1.25 mg/kg on D1, D8, D15 of every 28 days cycle | 219 | Objective Response Rate | Completed Cohort 1, N=125 ORR 44% Cohort 2, N=91 ORR 52% |
|
NCT03474107 EV-301 |
EV vs. Docetaxel/ Vinflunine/ Paclitaxel |
Locally Advanced or mUC, Prior Platinum and ICI | Phase 3 Randomized |
1.25 mg/kg on D1, D8, D15 of every 28 day cycle | 608 | Overall Survival | Completed EV OS HR 0.70 EV PFS HR 0.61 |
|
NCT04223856 EV-302 |
EV + Pembrolizumab vs. Gemcitabine + Platinum |
Locally Advanced or mUC, Treatment Naive | Phase 3 Randomized |
EV 1.25 mg/m2 D1, D8 of each 21 days cycle | 760 | Progression Free Survival and Overall Survival | Recruiting |
|
NCT03288545 EV-103 |
EV alone or with Pembrolizumab/ Cisplatin/ Carboplatin/ Gemcitabine |
mUC/Muscle Invasive Bladder Cancer | Phase 1 /2 Multiple Cohorts |
EV 1.25 mg/m2 D1, D8 of each 21 days cycle | 407 | Safety, Tolerability, Efficacy |
Recruiting Cohort A: Cis-unfit mUC EV+Pembro N=45 ORR 71% |
|
NCT03869190 MORPHEUS mUC |
Atezolizumab + EV (Other arms with Atezolizumab and anticancer therapies) |
Locally Advanced or mUC, Prior Platinum | Randomized Phase 1b/2 | EV 1.25 mg/m2 D1, D8 of each 21 days | 385 (total) | Objective Response Rate | Recruiting |
Abbreviations: EV (Enfortumab Vedotin), mUC (metastatic urothelial cancer), PK (Pharmacokinetics), ORR (Objective Response Rate), mOS (median overall survival), HR (Hazard Ratio), PFS (Progression Free Survival)
Phase I
The phase I EV-101 dose-escalation/dose-expansion study was conducted in patients who were resistant or refractory to treatment and had nectin-4-positive tumors (including mUC).16 The aim of Part A was to establish the recommended phase II dose (RP2D). Part B evaluated EV in three dose-expansion cohorts: patients with mUC and severe renal insufficiency, patients with lung cancer, and patients with ovarian cancer. Part C was a dose-expansion cohort in patients with mUC previously treated with an ICI.
Between June 2014 and October 2018, 201 patients with Nectin-4-positive tumors were enrolled, with 25 patients in the dose escalation phase of which 21 had mUC. In total 155 mUC patients were treated with EV. Initially, the expression of Nectin-4 on tumor biopsy was required for trial entry, but this criterion was removed after it was found that almost all mUC tumors highly expressed Nectin-4.
EV was dose escalated to 1.25 mg/kg given on Days 1, 8, and 15 of each 28-day cycle. Although this dose was deemed the RP2D, responses were also seen at lower dose levels. Impressively, the ORR was 43% in heavily pretreated patients—29% of them having received ⩾3 lines of prior treatments and 39% having liver metastasis. Among 112 patients treated at the RP2D, ORR was 43% (48/112), and the complete response (CR) rate was 5% (5/112). In patients treated with ICIs and taxanes, respectively, the ORR was 42.7% and 33.3%. Similar response rates were seen in patients who were ⩾75 years old and in patients with upper tract disease. The estimated median PFS was 5.4 months (95% CI, 5.1–6.3 mos); and median OS was 12.3 months (95% CI 9.3–15.3 mos).
The most common treatment-related adverse events (AEs) related to EV were fatigue, alopecia, rash and peripheral neuropathy. The rash was due to nectin-4 expression on human skin keratinocytes, and peripheral neuropathy was mediated by the microtubule inhibitor (MMAE). Serious cases of hyperglycemia related to EV were reported in 3.2% of patients and ultimately led to the exclusion of patients with elevated blood glucose levels. In phase I testing, EV showed encouraging activity and tolerability. The RP2D was established as 1.25 mg/m2 given weekly, 3 weeks out of 4.
Phase II EV 201
EV-201 was a global, single-arm two-cohort phase II trial for patients with locally advanced or mUC (NCT03219333).7 In cohort 1, 125 patients previously treated with platinum and an ICI were enrolled and treated at the RP2D. Cohort 2 enrolled patients who were platinum-naïve or platinum-ineligible and were previously treated with an ICI only.
Cohort 1
Efficacy results from cohort 1 are now published and were consistent with the results from EV-101, with an ORR of 44% and a CR rate of 12%, with a short time to response and duration of response of 7.6 months. Interestingly, patients responded regardless of prior response to ICIs, or presence of poor prognostic factors such as liver metastases. Median OS was 11.7 months in a poor-risk patient population, half of which received three or more lines of prior therapy. Cross-trial comparisons notwithstanding, EV showed higher response rates than the taxanes which also target the microtubules and are frequently used in this setting.
The most common treatment-related adverse events (TRAEs) in the EV 201 (cohort 1) trial are shown in Table 3.
Table 3.
Most common treatment-related adverse events (TRAE) occurring in ⩾20% in the EV201 study (Cohort 1).
| TRAE (n = 125) | Any grade | Grade 3+ |
|---|---|---|
| Fatigue | 62 (50) | 7 (6) |
| Alopecia | 61 (49) | 0 |
| Decreased appetite | 55 (44) | 1 (1) |
| Dysgeusia | 50 (40) | 0 |
| Peripheral sensory neuropathy | 50 (40) | 2 (2) |
| Nausea | 49 (39) | 3 (2) |
| Diarrhea | 40 (32) | 3 (2) |
| Maculopapular rash | 27 (22) | 5 (4) |
| Decreased weight | 28 (22) | 1 (1) |
| Dry skin | 28 (22) | 0 |
Any grade fatigue (6% Grade 3+) and alopecia were reported in about half of the patients, suggesting even though ADCs are targeted to nectin-expressing cells, systemic effects cannot be entirely eliminated. Decreased appetite (44% all grade, 1% grade 3+) dysgeusia (40% all grade, no grade 3+) and nausea (39% all grade, 2% grade 3+) were also reported but were manageable with supportive care.
Treatment-related peripheral sensory neuropathy, any grade, occurred in 40% with 2% grade 3+, and was more common than motor neuropathy (14%). Of the patients with peripheral neuropathy at baseline, 48% did not experience worsening. Most patients had resolution or ongoing grade 1 peripheral neuropathy at last follow-up. Peripheral sensory neuropathy was, however, the most common TRAE that led to dose reduction (9%) and discontinuation (6%). As neuropathy is a cumulative AE, this could be explained by the fact that patients were treated with an MMAE (microtubule inhibitor)-based therapy for several months (median duration of response was 7.6 months); and that all patients in cohort 1, had received prior platinum-based chemotherapy.
Maculopapular skin rash was an anticipated, on-target toxicity based on Nectin-4 expression in the skin, and occurred in 22%, with 4% grade 3+. Most were low grade with onset during the first treatment cycle. Two patients discontinued treatment due to rash, one had Stevens–Johnson syndrome, which resolved after drug discontinuation and systemic steroids. Of all patients with a rash, 73% had complete resolution, and 20% had improvement to grade 1. Rash was generally manageable with topical or systemic steroids, oral; antihistamines, and dose delays or reductions.
Treatment-related hyperglycemia, also seen in the phase I study, and of unclear etiology, occurred in 11% of patients, regardless of pre-existing hyperglycemia at baseline. It is therefore recommended that blood glucose levels be monitored closely in patients with or at risk for diabetes mellitus or hyperglycemia receiving EV.
Overall, in the EV201 study quality of life was either maintained, or improved with treatment. The EV201 study (Cohort 1) confirmed the activity and tolerability of EV in the platinum- and ICI-refractory setting, and led ultimately to the accelerated FDA approval in this setting and formed the basis for the phase III EV-301 trial.17
Cohort 2
In a recent press release, October 2020, positive results were also reported from EV201, Cohort 2—which evaluated EV in patients who had previously received an ICI, but no prior platinum-based chemotherapy. Results showed an ORR of 52% (95% CI 40.8–62.4) per blinded independent central review and a median duration of response of 10.9 months (Seagen, Astellas press release October 2020).
Phase III
The phase III EV-301 clinical trial (NCT03474107) randomized 550 platinum- and ICI-refractory patients with mUC to EV or investigator’s choice chemotherapy (Paclitaxel, Docetaxel or Vinflunine). A press release from this phase III study reported that this study has met its primary endpoint of OS compared with investigator choice treatment (HR, 0.70; p = 0.001). The secondary endpoint was also met with an impressive 39% risk reduction of progressive disease or death (HR, 0.61; p < 0.00001). This multicenter randomized trial is the first to report a significant improvement in both endpoints of OS and PFS in heavily pre-pretreated patients with mUC, compared with chemotherapy alone (press release).
Taken together, EV represents an important novel therapeutic strategy in patients with platinum- and ICI-refractory disease. Given its efficacy and tolerability in heavily pretreated patients, there is significant interest in testing EV in combination strategies and in the non-metastatic disease settings.
Future directions
EV in first-line cisplatin-unfit metastatic UC
Up to 50% of patients with locally advanced or mUC are ineligible for standard first-line cisplatin-based regimens due to poor performance status, compromised renal function or other comorbidities. In this setting, standard treatment options include carboplatin-based regimens, which have inferior outcomes compared with cisplatin-based regimens, and ICIs. ICIs are not widely available and are restricted to patients who are ineligible for carboplatin regardless of PD-L1 expression level in the tumor; or cisplatin-ineligible patients with tumors expressing PD-L1. Overall ORRs with either carboplatin or ICIs are relatively low, and outcomes remain poor, highlighting a significant unmet need. As EV is not cleared renally and can be used in patients with renal dysfunction, it may be an ideal choice in this setting.
In preclinical models, MMAE-based antibody–drug conjugates have also been shown to be able to induce immunogenic cell death, resulting in an anti-tumor immune response.18,19 Given the potential synergy and non-overlapping toxicities between EV and the ICIs, combining EV and an ICI in first-line cisplatin-ineligible mUC patients was a logical next step in the development of EV in mUC.
EV 103 trial
The EV-103 trial is a multi-cohort trial evaluating EV alone and in combination with other therapies, in both platinum-eligible and ineligible patients, and in both advanced and MIBC settings. Several cohorts will be assessed in this study: EV + Pembrolizumab in first-line cisplatin-unfit (cohort A), EV + Pembrolizumab in second line (cohort B), EV + Cisplatin (cohort D), EV + Carboplatin (cohort E), EV + Gemcitabine (Cohort F) and EV + platinum and Pembrolizumab (Cohort G). EV was administered at a dose of 1.25 mg/kg but the schedule of administration was changed from D1, D8, D15 every 28 days cycle to D1, D8 of each 21 days cycle.
EV 103, Cohort A
Initial results from Cohort A, EV and Pembrolizumab in cisplatin-ineligible 1L mUC, were recently reported.20 A total of 45 patients received EV (1.25 mg/kg days 1 and 8 of every 3-week cycle) in combination with pembrolizumab (200 mg every 3 weeks). The prespecified primary endpoints were safety and tolerability, and key secondary endpoints were ORR, duration of response, and median OS.
In terms of the primary endpoint of safety, 51% (23/45) of patients experienced a grade 3 or 4 AE. Fatigue, alopecia, neuropathy, and diarrhea were the most common toxicities (40–49%), and 13% (6/45) experienced grade ⩾3 lipase elevation. A single patient (2%) died of multiorgan dysfunction in the context of acute kidney injury and atrial fibrillation with rapid ventricular response.
In terms of efficacy, the ORR was 71% (32/45) (95% CI 55.7%–83.6%), and the CR rate was 13% (6/45). Another 22% (10/45) had stable disease, leading to a disease control rate of 93%. Patients with liver metastases had an ORR of 53.3%, and patients responded regardless of their PD-L1 expression level. Patients with a high PD-L1 status (CPS ⩾10%) had an ORR of 78.6%, whereas patients with low PD-L1 status (CPS <10%) had an ORR of 63.2%, which is still comparable to first-line cisplatin-based chemotherapy. Median time to response was 2 months and response duration ranged from 1.0 to 10.5 months.
Although we need to interpret the results of this small single-arm, non-randomized trial cautiously, the preliminary results of Cohort A suggest that the combination of EV and an ICI may be synergistic and potentially represents a major advance in the field. Interestingly, ICIs have not shown clear synergy when administered concurrently with chemotherapy. Both the phase III IMvigor 130 study which combined chemotherapy and the ICI Atezolizumab and the Keynote 361 (press release) study that combined chemotherapy and the ICI Pembrolizumab had somewhat disappointing results.21 However, the Javelin study evaluating maintenance Avelumab after first-line chemo showed a significant improvement in OS and is now FDA approved, suggesting a maintenance strategy should be considered for patients achieving stable disease or response to first-line chemotherapy.22
Given the preliminary promising data of the combination EV and pembrolizumab, a larger randomized trial is underway to formally evaluate this combination strategy. The phase III EV-302 clinical trial will randomize patients with previously untreated locally advanced or mUC to EV (given D1 and D8 of a 21-day cycle) + Pembrolizumab (Arm A) or standard of care platinum-based chemotherapy. PFS and OS will be the primary endpoints (NCT04223856). This pivotal trial will further define the role of EV in first-line mUC. In light of the recent Javelin data, one outstanding question is whether a maintenance-type strategy would need to be incorporated into both arms of this trial to further improve outcomes of this combination approach.
Muscle-invasive bladder cancer
Based on the efficacy and tolerability of EV in mUC there is significant interest in moving EV into the MIBC setting. MIBC is a highly aggressive, yet potentially curable disease. It is currently managed with a combination of cisplatin-based neoadjuvant chemotherapy (NAC) and local definitive therapy; however, many patients are not candidates for cisplatin-based NAC. Two single-arm phase II studies, PURE and ABACUS, have recently shown efficacy of the neoadjuvant ICIs in this setting.23,24 In the EV-103 study, two separate cohorts will explore EV alone and EV in combination with Pembrolizumab in the neoadjuvant setting. Whether EV may have a place in the adjuvant setting also remains to be seen. In Her2+ breast cancer, when pathological CR is not achieved after NAC, adjuvant ADC T-DM1 significantly improves disease-free survival.25 It may be interesting to assess whether EV similarly may have a role in patients who have residual disease after receiving standard NAC.
Sacituzumab Govitecan
Another ADC currently under investigation in advanced UC is Sacituzumab Govitecan (SG). This is a humanized ADC which links the anti-Trop 2 monoclonal antibody to SN-38, which is the active metabolite of irinotecan. As a camptothecin, SN38 inhibits the nuclear topoisomerase 1 enzyme, inducing double-stranded DNA breaks during S-phase of mitosis. SG at a recommended phase II dose of 10 mg/kg, given on day 1, 8 of a 21-day cycle, has accelerated FDA approval in patients with previously treated triple-negative metastatic breast cancer. At the European Society for Medical Oncology virtual congress 2020, results from cohort 1 of the phase II TROPHY U-O1 study, of SG in patients with mUC that was platinum and ICI refractory was presented. The ORR was 27% (n = 31, 95% CI 19–37%), median PFS was 5.4 months (95% CI 3.5–6.9 months), and median OS 10.5 months (8.2–12.3 months). The most common grade 3+ AEs were different from EV and included neutropenia, leukopenia, anemia, diarrhea, nausea and fatigue—with seven (6%) patients discontinuing due to TRAEs, GCSF usage was 30% and there was one treatment-related death due to sepsis.26 Given these encouraging results, a phase III confirmatory trial TROPiCS, comparing SG with investigator’s choice of chemotherapy (Paclitaxel, Docetaxel or Vinflunine) is underway. However, given the recent announcement of positive results from the EV301 study, a key question going forwards will be the choice of comparator arm on this trial, and where this drug will fit into the treatment paradigm.
Treatment sequencing
As several novel therapies enter the treatment paradigm an important consideration will be how best to sequence these treatments in a given patient. Currently in the first-line setting, based on the Javelin 100 study, front-line chemotherapy followed by maintenance Avelumab (ICI inhibitor) is the new standard of care.22 At the time of disease progression, based on the EV 301 trial, EV would be the next recommended approach. However, in patients with severe hyperglycemia or peripheral neuropathy SG may be an alternate approach, pending further confirmation from the phase III TROPICs trial. As EV and SG have different mechanisms of action and toxicity profiles, they could potentially be used sequentially, but data to support this approach are not yet available. In first-line patients who are not platinum-eligible, ICI has accelerated approval in some jurisdictions. At the time of progression, based on the recent press release from EV201, cohort 2 study, EV is likely a reasonable option in this setting. For patients who have FGFR2/3 mutations/alterations, and may be less responsive to immunotherapy, Erdafitinib may be the preferred option in the platinum-refractory setting. Following progression, EV may be an option but limited data on sequencing in this setting are available. In jurisdictions without access to these new options, the taxanes, which are relatively well tolerated and inexpensive, have response rates of approximately 25%, remain a viable option.4
Conclusion
EV is a novel ADC which is showing both tolerability and efficacy in a heavily pretreated and often frail, unselected patient population with mUC. EV already has accelerated FDA approval in the cisplatin-refractory and ICI-refractory setting, where a press release has recently reported positive phase III data, with final results expected in 2021. Combination strategies, in particular with the ICI Pembrolizumab in first-line cisplatin-unfit mUC, have also shown very encouraging early results and a phase III trial is currently underway. There is also significant interest in moving EV earlier in the treatment paradigm where potentially there may be better efficacy, and perhaps less toxicity, especially neuropathy if patients are platinum-naïve. There remain several unanswered questions—for example, how best to sequence all the novel therapies and standard therapies now available in this disease, and whether there are biomarkers or subgroups according to The Cancer Genome Atlas that may show preferential response to these agents when given in a particular sequence. Clinical trials will be needed to answer these important questions and several are already ongoing. It has indeed been an exciting time in the field of UC, where we are finally beginning to see unprecedented improvements in both tolerability of novel treatments and overall outcomes across the spectrum of this disease.
Footnotes
Author Contributions: Conception or design of the work, M.A. and S.S.;
Data collection, M.A. and S.S.;
Data analysis and interpretation, M.A., C.S., S.T., D.J. and S.S.;
Drafting the article, M.A., S.T. and S.S.;
Critical revision of the article, M.A., C.S., D.J. and S.S.;
Final approval of the version to be published, S.S.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement: Dr. Sridhar has received research funding from Bayer, Janssen, and honoraria from Roche, Merck, Pfizer, Astra Zeneca, BMS, Janssen, Bayer, Astellas, Sanofi Aventis, Immunomedex.
ORCID iDs: Di Maria Jiang  https://orcid.org/0000-0002-1950-2292
https://orcid.org/0000-0002-1950-2292
Srikala S. Sridhar  https://orcid.org/0000-0002-6994-1285
https://orcid.org/0000-0002-6994-1285
Contributor Information
Marie Alt, Princess Margaret Cancer Center, University Health Network, Toronto, ON, Canada.
Carlos Stecca, Princess Margaret Cancer Center, University Health Network, Toronto, ON, Canada.
Swanee Tobin, Princess Margaret Cancer Center, University Health Network, Toronto, ON, Canada.
Di Maria Jiang, Princess Margaret Cancer Center, University Health Network, Toronto, ON, Canada.
Srikala S. Sridhar, Associate Professor, Department of Medicine, Medical Oncologist, Princess Margaret Cancer Center, Chair, GU Medical Oncologists of Canada, 7-625 OPG, 610 University Avenue, Toronto, ON M5G 2M9, Canada.
References
- 1. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018; 68: 394–424. [DOI] [PubMed] [Google Scholar]
- 2. von der Maase H, Hansen SW, Roberts JT, et al. Gemcitabine and cisplatin versus methotrexate, vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: results of a large, randomized, multinational, multicenter, phase III study. J Clin Oncol 2000; 18: 3068–3077. [DOI] [PubMed] [Google Scholar]
- 3. Bellmunt J, de Wit R, Vaughn DJ, et al. Pembrolizumab as second-line therapy for advanced urothelial carcinoma. N Engl J Med 2017; 376: 1015–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sridhar SS, Blais N, Tran B, et al. Cctg BL12: randomized phase II trial comparing nab-paclitaxel (Nab-P) to paclitaxel (P) in patients (pts) with advanced urothelial cancer progressing on or after a platinum containing regimen (NCT02033993). J Clin Oncol 2018; 36: 4505. [Google Scholar]
- 5. Bellmunt J, Theodore C, Demkov T, et al. Phase III trial of vinflunine plus best supportive care compared with best supportive care alone after a platinum-containing regimen in patients with advanced transitional cell carcinoma of the urothelial tract. J Clin Oncol 2009; 27: 4454–4461. [DOI] [PubMed] [Google Scholar]
- 6. Loriot Y, Necchi A, Park SH, et al. Erdafitinib in locally advanced or metastatic urothelial carcinoma. N Engl J Med 2019; 381: 338–348. [DOI] [PubMed] [Google Scholar]
- 7. Rosenberg JE, O’Donnell PH, Balar AV, et al. Pivotal trial of enfortumab vedotin in urothelial carcinoma after platinum and anti-programmed death 1/programmed death ligand 1 therapy. J Clin Oncol 2019; 37: 2592–2600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Borcoman E, Le Tourneau C. Antibody drug conjugates: the future of chemotherapy? Curr Opin Oncol 2016; 28: 429–436. [DOI] [PubMed] [Google Scholar]
- 9. Carter PJ, Senter PD. Antibody-drug conjugates for cancer therapy. Cancer J 2008; 14: 154–169. [DOI] [PubMed] [Google Scholar]
- 10. Senter PD. Potent antibody drug conjugates for cancer therapy. Curr Opin Chem Biol 2009; 13: 235–244. [DOI] [PubMed] [Google Scholar]
- 11. Polson AG, Calemine-Fenaux J, Chan P, et al. Antibody-drug conjugates for the treatment of non-Hodgkin’s lymphoma: target and linker-drug selection. Cancer Res 2009; 69: 2358–2364. [DOI] [PubMed] [Google Scholar]
- 12. Beck A, Goetsch L, Dumontet C, et al. Strategies and challenges for the next generation of antibody-drug conjugates. Nat Rev Drug Discov 2017; 16: 315–337. [DOI] [PubMed] [Google Scholar]
- 13. Zhang Y, Zhang J, Shen Q, et al. High expression of Nectin-4 is associated with unfavorable prognosis in gastric cancer. Oncol Lett 2018; 15: 8789–8795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Challita-Eid PM, Satpayev D, Yang P, et al. Enfortumab vedotin antibody-drug conjugate targeting Nectin-4 is a highly potent therapeutic agent in multiple preclinical cancer models. Cancer Res 2016; 76: 3003–3013. [DOI] [PubMed] [Google Scholar]
- 15. Samanta D, Almo SC. Nectin family of cell-adhesion molecules: structural and molecular aspects of function and specificity. Cell Mol Life Sci 2015; 72: 645–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rosenberg J, Sridhar SS, Zhang J, et al. EV-101: a phase I study of single-agent enfortumab vedotin in patients with Nectin-4-positive solid tumors, including metastatic urothelial carcinoma. J Clin Oncol 2020; 38: 1041–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McGregor BA, O’Donnell PH, Balar A, et al. Quality of life of metastatic urothelial cancer (mUC) patients treated with enfortumab vedotin (EV) following platinum-containing chemotherapy and a checkpoint inhibitor (CPI): data from EV-201cohort 1. Ann Oncol 2019; 30(Suppl. 5): V367–V368. [Google Scholar]
- 18. Muller P, Martin K, Theurich S, et al. Microtubule-depolymerizing agents used in antibody-drug conjugates induce antitumor immunity by stimulation of dendritic cells. Cancer Immunol Res 2014; 2: 741–755. [DOI] [PubMed] [Google Scholar]
- 19. Müller P, Rios-Doria J, Harper J, et al. Combining ADCs with immuno-oncology agents. In: Damelin M. (ed.) Innovations for next-generation antibody-drug conjugates, cancer drug discovery and development. Cham: Humana Press, 2018. [Google Scholar]
- 20. Rosenberg JE, Flaig TW, Friedlander TW, et al. Study EV-103: preliminary durability results of enfortumab vedotin plus pembrolizumab for locally advanced or metastatic urothelial carcinoma. J Clin Oncol 2020; 38(Suppl. 6): 441. [Google Scholar]
- 21. Grande E, Galsky MD, Arranz Arija JA, et al. LBA14_PR - IMvigor130: efficacy and safety from a phase III study of atezolizumab (atezo) as monotherapy or in combination with platinum-based chemotherapy (PBC) vs placebo + PBC in previously untreated locally advanced or metastatic urothelial carcinoma (mUC). Ann Oncol 2019; 30(Suppl. 5): v888–v889. [Google Scholar]
- 22. Powles T, Park SH, Voog E, et al. Maintenance avelumab + best supportive care (BSC) versus BSC alone after platinum-based first-line (1L) chemotherapy in advanced urothelial carcinoma (UC): JAVELIN bladder 100 phase III interim analysis. J Clin Oncol 2020; 38.33052757 [Google Scholar]
- 23. Necchi A, Raggi D, Gallina A, et al. Updated results of PURE-01 with preliminary activity of neoadjuvant pembrolizumab in patients with muscle-invasive bladder carcinoma with variant histologies. Eur Urol 2020; 77: 439–446. [DOI] [PubMed] [Google Scholar]
- 24. Powles T, Kockx M, Rodriguez-Vida A, et al. Clinical efficacy and biomarker analysis of neoadjuvant atezolizumab in operable urothelial carcinoma in the ABACUS trial. Nat Med 2019; 25: 1706–1714. [DOI] [PubMed] [Google Scholar]
- 25. von Minckwitz G, Huang CS, Mano MS, et al. Trastuzumab emtansine for residual invasive HER2-positive breast cancer. N Engl J Med 2019; 380: 617–628. [DOI] [PubMed] [Google Scholar]
- 26. Loriot Y, Balar AV, Petrylak DP, et al. , (eds). LBA24 - Final results from TROPHY-U-01 cohort 1: a phase 2 open label study of sacituzumab govitecan (SG) in patients with metastatic urothelial cancer (mUC) and disease progression after platinum (PLT)-based regimens and checkpoint inhibitors (CPI). Presented at the European Society of Medical Oncology Annual Virtual Meeting, 19 September-18 October 2020, Switzerland. [Google Scholar]