Summary
Ocular complications of coronavirus disease 2019 (COVID-19) do not essentially cause serious visual loss. However, due to the characteristics of this disease, delays in diagnosis and treatment in hospitalized patients may leave them with serious visual impairment. If conjunctivitis is suspected, ophthalmological follow-up is needless because it is expected spontaneous healing. Diplopia is often complicated for extra-ocular neurological findings and need neurological consults. Ophthalmologists should be consulted for ocular surface disease, high intraocular pressure, and ocular inflammation that may cause visual loss if patients complain of blurred vision, visual loss, and ocular pain. The problem is unconscious patients with risk of developing high intraocular pressure or keratitis. An ophthalmologist should be consulted as soon as possible if eye redness or pupil abnormalities appear in these patients. We developed a flowchart for ophthalmic consultations in hospitalized patients with COVID-19, for facilities where an ophthalmologist is not always present, and for third or fourth waves or, a pandemic of another infectious disease.
Keywords: COVID-19, flowchart, ocular complication, ophthalmology, eye
Almost one year has passed since the emergence of the new coronavirus. In addition to conjunctivitis, there have been reports of serious sight-threatening ocular diseases, particularly in hospitalized patients who have been left with impaired vision after recovery from coronavirus disease 2019 (COVID-19). Ideally, an ophthalmologist should be present for all cases of suspected ocular disease. However, not all facilities that accept COVD-19 patients have an ophthalmologist on staff. At the National Center for Global Health and Medicine, the Department of Ophthalmology, Disease Control and Prevention Center, and Department of Intensive Care Medicine staffs have been working together to reduce the risk of infection among ophthalmologists, and minimize the wasteful use of medical materials including PPE, with the primary goal of eliminating visual impairment in COVID-19 patients. Based on previous reports, we developed a flowchart of ophthalmic consultations in hospitalized patients with COVID-19, for use in facilities where an ophthalmologist is not always present, and useful in the event of a third or fourth wave, or a pandemic of another infectious disease.
Conjunctivitis was the first reported ocular manifestation of COVID-19 (1). If patients have no consciousness disorder and present mostly bilateral conjunctival hyperemia, chemosis, epiphora, watery discharge, mild eyelid edema without blurred vision or sight-threatening events, Route A in Figure 1 is thought for conjunctivitis, and only follow up would be needed because these findings are heal spontaneously.
Figure 1.
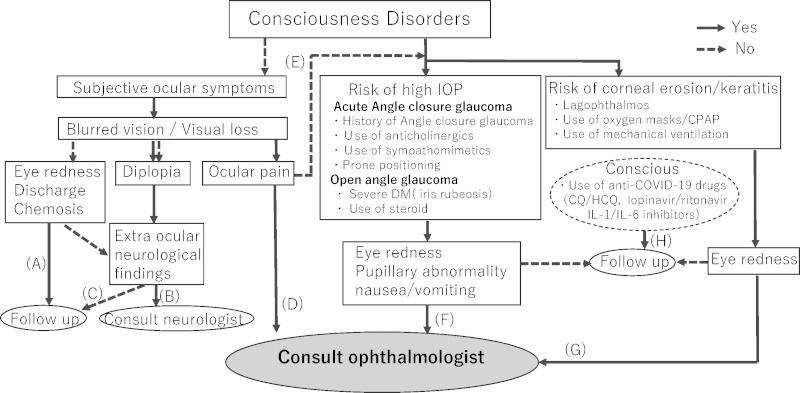
Flowchart for ophthalmic consultations and suspected diseases in hospitalized patients with COVID-19. Route (A) conjunctivitis, (B) intracranial diseases, (C) peripheral abducens or oculomotor nerve palsy, (D) ocular surface disorders or high IOP, (E) retinal diseases or optic neuritis, (F) high IOP, (G) infectious keratitis secondary to corneal erosion, (H) side effect of medicine for COVID-19. CPAP, continuous positive airway pressure; CQ, Chloroquine; DM, diabetes mellitus; HCQ, hydroxychloroquine; IOP, intraocular pressure.
Route B and C is thought to be Neuro-Ophthalmological Complications. If patients complain about diplopia with extraocular neurological findings like polyneuritis, Guillain-Barré syndrome, meningitis, encephalomyelitis, and encephalopathy, intracranial disease should be suspected and a neurologist should be consulted first (Route-B) (2). Patient complaints about diplopia without other neurological findings are rare cases. When peripheral abducens or oculomotor nerve palsy is suspected in COVID-19 inpatients, ophthalmological examinations should end (Route-C) and careful neurological follow up should be initiated.
The most common ocular complications are ocular surface disorders. When patients complain of blurred vision and irritation or ocular pain, existence of ocular surface disorders, especially infectious keratitis, should be ruled out. In cases of high intraocular pressure (IOP) that leads to blurred vision and deep ocular pain with nausea or vomiting, immediate ocular treatment is necessary to avoid permanent visual loss (Route-D).
If patients complain of blurred vision or visual loss only, retinal diseases or optic neuritis should be considered. COVID-19-associated coagulopathy may predispose patients to a spectrum of thromboembolic events. As for retinal findings, not only subtle cotton-wool spots and microhemorrhages along the retinal arcade (3), but isolated central retinal artery occlusion and impending central retinal vein occlusion secondary to COVID-19 has been published (4,5). The latter leads to visual loss without ocular pain and extra ocular neurological complications. However, even though macular edema occurs after occlusion, only follow up is required because of the difficulty of ophthalmological treatments like anti-vascular endothelial growth factor (VEGF) vitreous injection. Ischemic or inflammatory optic neuritis, progression of pre-existing diseases, such as diabetic retinopathy or age-related maculopathy, will also contribute to visual loss. However, a full ophthalmological examination is difficult and ocular treatment is limited to hospitalized patients with COVID-19. Therefore, if the risk of high IOP or infectious keratitis due to corneal erosion can be ruled out, these diseases can be followed until a full ophthalmological examination and treatment is available after discharge (Route-E).
For severe COVID-19 patients in Intensive Care Units who could not convey eye problems by consciousness disorder, high IOP is the most notable sight-threatening complication. In general, a history of angle-closure glaucoma, use of anticholinergics (atropine, ipratropium bromide, tricyclic antidepressants, and antihistamine), sympathomimetics (adrenaline, noradrenaline, dopamine, ephedrine, salbutamol, and terbutaline), and other drugs (sulfonamides derivatives and topiramate), are risk factors for acute angle-closure glaucoma. Moreover, prone positioning for improving respiratory outcomes can critically reduce ocular perfusion causing an increase in venous pressure and subsequent increase IOP (6). Diabetes mellitus (DM) is one of the factors that can make COVID-19 more severe, and systemic steroids are used for severe patients. Iris rubeosis due to proliferative diabetic retinopathy, and longitudinal use of steroids for steroid responders, these are not angle-closure, sometimes increases IOP. When patients have the fore-mentioned risks, and emerging eye redness, larger pupil size in affected eye, nausea or vomiting; IOP check-up should be done as soon as possible (Route-F).
Infectious keratitis due to corneal erosion should be avoided in patients with consciousness disorder (7). Lagophthalmos due to use of muscle relaxants or sedating agents, dry eyes from oxygen masks, continuous positive airway pressure (CPAP), or mechanical ventilation leads to ocular surface disorder. This can develop primarily into infectious keratitis and eventually corneal erosion resulting in irreversible visual loss by corneal opacity (Route-G).
The side effects of COVID-19 medication should be taken into account. Chloroquine (CQ) and its derivative hydroxychloroquine (HCQ) are mainly used to treat malaria, amebiasis, and rheumatologic diseases, while lopinavir and ritonavir are widely used for the treatment of HIV. The reported toxicity of these drugs include irreversible sight-threatening maculopathy called Bulls eye. Despite the fact that most of the patients treated with CQ and HCQ for COVID-19 receive potentially retinotoxic doses, no reports of retinal toxicity have been described under 2 weeks of CQ or HCQ administration. Moreover ritonavir-associated retinal toxicity has been reported with limited chronic use. Significantly short-term use for these drugs for COVID-19 treatment might be a small concern for retinal toxicity (8,9). Interleukin-1 inhibitors (e.g., anakinra) and interleukin-6 inhibitors (e.g., sarilumab, siltuximab, and tocilizumab) under evaluation for the treatment of COVID-19 should be monitored for nystagmus or bilateral retinopathy side effects (Route-H).
At present, telecommunication using smartphones in ophthalmology is rapidly evolving. Anterior segment imaging especially, does not require an ophthalmologist and can be performed by paramedical staff. Some superior quality devices make it possible to provide posterior pole retina and optic disc images without any attachments (10). To prevent visual impairment for inpatients with COVID-19, it is important to follow this flowchart, sometimes with use of mentioned devices, for consultation with ophthalmologist at the appropriate time.
Funding: None
Conflict of Interest
The authors have no conflict of interest to disclose.
References
- 1. Lu CW, Liu XF, Jia ZF. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020; 395:e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wei H, Yin H, Huang M, Guo Z. The 2019 novel cornoavirus pneumonia with onset of oculomotor nerve palsy: a case study. J Neurol. 2020; 267:1550-1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Marinho PM, Marcos AAA, Romano AC, Nascimento H, Belfort R Jr. Retinal findings in patients with COVID-19. Lancet. 2020; 395:1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Acharya S, Diamond M, Anwar S, Glaser A, Tyagi P. Unique case of central retinal artery occlusion secondary to COVID-19 disease. IDCases. 2020; 21:e00867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Invernizzi A, Pellegrini M, Messenio D, Cereda M, Olivieri P, Brambilla AM, Staurenghi G. Impending central retinal vein occlusion in a patient with coronavirus disease 2019 (COVID-19). Ocul Immunol Inflamm. 2020; 28:1290-1292. [DOI] [PubMed] [Google Scholar]
- 6. Sanghi P, Malik M, Hossain IT, Manzouri B. Ocular Complications in the prone position in the critical care setting: the COVID-19 pandemic. J Intensive Care Med. 2020 Sep 28:885066620959031 doi: 10.1177/0885066620959031. [DOI] [PubMed] [Google Scholar]
- 7. Sansome SG, Lin PF. Eye care in the intensive care unit during the COVID-19 pandemic. Br J Hosp Med (Lond). 2020; 81:1-10. [DOI] [PubMed] [Google Scholar]
- 8. Marmor MF. COVID-19 a n d c h l o r o q u i n e / hydroxychloroquine: is there ophthalmological concern? Am J Ophthalmol. 2020; 213:A3-A4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Roe RH, Jumper JM, Gualino V, Wender J, McDonald HR, Johnson RN, Fu AD, Cunningham ET. Retinal pigment epitheliopathy, macular telangiectasis, and intraretinal crystal deposits in HIV-positive patients receiving ritonavir. Retina. 2011; 31:559-565. [DOI] [PubMed] [Google Scholar]
- 10. Pujari A, Saluja G, Agarwal D, Selvan H, Sharma N. Clinically useful smartphone ophthalmic imaging techniques. Graefes Arch Clin Exp Ophthalmol. 2020 Sep 11. doi: 10.1007/s00417-020-04917-z. [DOI] [PubMed] [Google Scholar]


