Abstract
Objectives
Concussions and mild traumatic brain injuries are important medical issues, particularly among youth as the long-term health consequences of these injuries can become increasingly problematic. The purpose of this study was to examine recent trends in diagnosed concussions among pediatric patients in a large health care system.
Methods
This was a retrospective, population-based epidemiology study design that queried all patient files (pediatrics included) using electronic medical health records and further stratified patients based on type of concussion, age, sex, and year from 2013 to 2018.
Results
Electronic health records from a cohort of 8 832 419 (nmales = 4 246 492; nfemales = 4 585 931) patient visits were assessed for concussion diagnosis and filtered for those whose concussive event led to a loss of consciousness (LOC) or not (nLOC). Of these patients, 12 068 were diagnosed with a concussion (LOC = 3 699; nLOC = 8 369) with an overall incidence rate of 1.37 concussions per 1000 patients. Overall, the number of patients diagnosed with a concussion increased by 5063 (LOC = 1351; nLOC = 3712) from 2013 to 2018. Males and females presented with similar rates of concussions 5919 (49.05%) and 6149 concussions (50.95%), respectively. Of total diagnosed concussions, 4972 (LOC = 815; nLOC = 4157) were under the age of 18 and represented 41.2% of all diagnosed concussions with an incidence rate of 6.79 per 1000 patients.
Conclusion
The number of concussions diagnosed appear to be on the rise with the largest number of concussions being diagnosed in those under the age of 18. Future studies should seek to determine primary causality and the long-term health implications of concussions with or without LOC.
Keywords: traumatic brain injury, adolescents, sports injury
Introduction
A concussion is defined as a transient disturbance of brain function induced by physical trauma that often involves a complex pathophysiological process.1 Concussions commonly occur as a result of a blow to the body, neck, or head that creates impulsive forces acting on the head. As a result, these forces can disrupt neuronal cell membranes and axons leading to a multifaceted dysregulation of cellular metabolism, ultimately resulting in short-term neurologic impairment.1 Diagnosis of a concussion typically depends on detection of functional impairment and symptoms.
Recent media attention has markedly increased public concern about the long-term effect of concussions, particularly for adolescent athletes. Further, the available data suggest that the rate of concussion diagnoses may be increasing.2,3 From 2006 to 2014, emergency department (ED) visits for TBI have increased by approximately 64% for patients of all ages.4 In contrast, TBI-related ED visits from 2001 through 2010 increased by approximately 91% for children younger than 14 years.3 In a sample of 8.8 million patients younger than 65 years, approximately 40% of all concussion diagnoses were in patients younger than 19 years.2 This trend in adolescent concussions may be particularly problematic because early exposure to repetitive head impacts can lead to summative effects later in life and predispose patients to complications such as anxiety, cognitive decline, decision-making difficulties, and other concerns.5
Given the risks associated with pediatric concussion, up-to-date knowledge on recent concussion rates is important for guiding best practices and policy decisions regarding safety. Therefore, the primary aim of this brief report was to examine trends in concussions by assessing a robust cross-sectional population seen at a large health care system from 2013 through 2018.
Methods
Setting
The reporting of this study is in compliance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement.6 We retrospectively searched electronic health records of patients seen across a large US healthcare enterprise from January 1, 2013, through December 31, 2018 to identify patients with a concussion diagnosis using all diagnostic codes applicable to concussions. The study size was determined by the number of patient visits that occurred during the study period.
Procedures
We extracted demographic characteristics (age and sex) and determined whether the concussive event resulted in a loss of consciousness (LOC) or no loss of consciousness (nLOC) to classify severity of concussion. Patients were stratified by age to identify specific trends in concussion rates among certain age groups as follows: <18, 18-37, 38-59, and >60 years of age. Pediatric and adolescent patients were further stratified into the following age categories: 5-10, 11-15, and 16-20 years of age. Descriptive analysis was used to assess incidence rates. This study was considered exempt from review from our Institutional Review Board for Human Research Guidelines as it did not involve human subjects and only de-identified patient data was used. As a result, informed consent was waived as only de-identified electronic health records were used.
Results
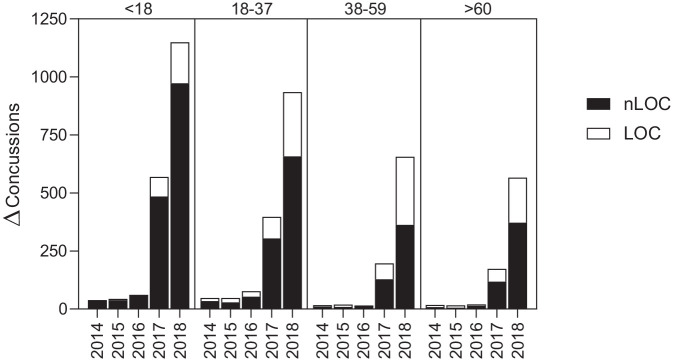
Electronic health records from a cohort of 8 832 419 (nmales = 4 246 492; nfemales = 4 585 931) patient visits were assessed for concussion diagnosis and filtered for those whose concussive event led to a loss of consciousness (LOC) or not (nLOC). Of these patients, 12 068 were diagnosed with a concussion (LOC = 3699; nLOC = 8369) with an overall incidence rate of 1.37 concussions per 1000 patients. Sex differences in total concussions were equivocal with males and females presenting with 5919 (49.05%) and 6149 concussions (50.95%), respectively. Overall, the number of patients diagnosed with a concussion increased by 5063 (LOC = 1351; nLOC = 3712) from 2013 to 2018 as seen in Figure 1.
Figure 1.
Year-to-year change in number of concussion diagnoses by year, type, and age.
Abbreviations: LOC, loss of consciousness; nLOC, non-loss of consciousness.
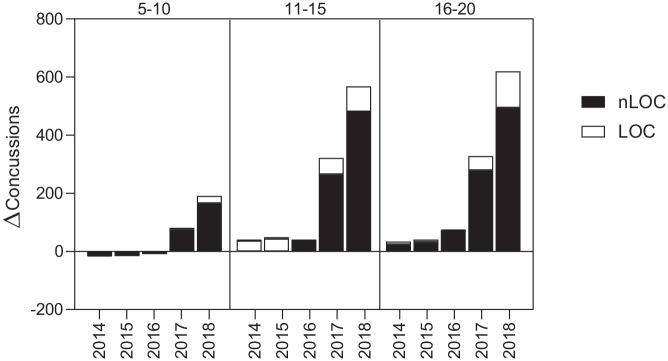
Of total diagnosed concussions, 4972 (LOC = 815; nLOC = 4157) were under the age of 18 and represented 41.2% of all diagnosed concussions with an incidence rate of 6.79 per 1000 patients as seen in Figure 2.
Figure 2.
Total number of patients diagnosed with a concussion from 2013 to 2018 by type and age.
Abbreviations: LOC, loss of consciousness; nLOC, non-loss of consciousness.
Those between the ages of 18-37 presented with the next highest incidence rate (2.06 concussions per 1000 patient visits) and 3454 total concussions (LOC = 1143; nLOC = 2311). Patients 38-59 and >60 years of age presented with 2102 (LOC = 1059; nLOC = 1043; incidence ratio = 0.74 concussions per 1000 patient visits) and 1540 (LOC = 682; nLOC = 858; incidence ratio = 0.30 concussions per 1000 patient visits) concussions, respectively. Table 1 provides a summary of the number of diagnosed concussions in adult per year based on loss of consciousness or not.
Table 1.
Number of Diagnosed Concussions in Adults by Year.
| nLOC concussions | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 2013 |
2014 |
2015 |
2016 |
2017 |
2018 |
||||||||||||
| M | F | T | M | F | T | M | F | T | M | F | T | M | F | T | M | F | T | |
| <18 | 158 | 125 | 283 | 185 | 136 | 321 | 204 | 155 | 359 | 236 | 181 | 417 | 515 | 387 | 902 | 1001 | 874 | 1875 |
| 18 to 37 | 38 | 62 | 100 | 50 | 84 | 134 | 68 | 95 | 163 | 85 | 131 | 216 | 225 | 295 | 520 | 509 | 669 | 1178 |
| 38 to 59 | 13 | 36 | 49 | 16 | 44 | 60 | 21 | 48 | 69 | 22 | 60 | 82 | 61 | 149 | 210 | 215 | 358 | 573 |
| >60 | 12 | 12 | 24 | 16 | 16 | 32 | 19 | 19 | 38 | 26 | 26 | 52 | 85 | 85 | 170 | 271 | 271 | 542 |
| Total | 221 | 235 | 456 | 267 | 280 | 547 | 312 | 317 | 629 | 369 | 398 | 767 | 886 | 916 | 1802 | 1996 | 2172 | 4168 |
| LOC concussions | ||||||||||||||||||
| Age | 2013 |
2014 |
2015 |
2016 |
2017 |
2018 |
||||||||||||
| M | F | T | M | F | T | M | F | T | M | F | T | M | F | T | M | F | T | |
| <18 | 35 | 38 | 73 | 33 | 40 | 73 | 38 | 41 | 79 | 43 | 39 | 82 | 102 | 64 | 166 | 211 | 131 | 342 |
| 18 to 37 | 35 | 42 | 77 | 40 | 51 | 91 | 43 | 67 | 110 | 54 | 80 | 134 | 102 | 125 | 227 | 267 | 237 | 504 |
| 38 to 59 | 43 | 49 | 92 | 47 | 51 | 98 | 51 | 57 | 108 | 50 | 60 | 110 | 88 | 91 | 179 | 237 | 235 | 472 |
| >60 | 24 | 21 | 45 | 27 | 28 | 55 | 33 | 32 | 65 | 35 | 36 | 71 | 65 | 61 | 126 | 165 | 155 | 320 |
| Total | 137 | 150 | 287 | 147 | 170 | 317 | 165 | 197 | 362 | 182 | 215 | 397 | 357 | 341 | 698 | 880 | 758 | 1638 |
| Total concussions | ||||||||||||||||||
| Age | 2013 |
2014 |
2015 |
2016 |
2017 |
2018 |
||||||||||||
| M | F | T | M | F | T | M | F | T | M | F | T | M | F | T | M | F | T | |
| <18 | 193 | 163 | 356 | 218 | 176 | 394 | 242 | 196 | 438 | 279 | 220 | 499 | 617 | 451 | 1068 | 1,212 | 1005 | 2217 |
| 18 to 37 | 73 | 104 | 177 | 90 | 135 | 225 | 111 | 162 | 273 | 139 | 211 | 350 | 327 | 420 | 747 | 776 | 906 | 1682 |
| 38 to 59 | 56 | 85 | 141 | 63 | 95 | 158 | 72 | 105 | 177 | 72 | 120 | 192 | 149 | 240 | 389 | 452 | 593 | 1045 |
| >60 | 36 | 33 | 69 | 43 | 44 | 87 | 52 | 51 | 103 | 61 | 62 | 123 | 150 | 146 | 296 | 436 | 426 | 862 |
| Total | 358 | 385 | 743 | 414 | 450 | 864 | 477 | 514 | 991 | 551 | 613 | 1164 | 1243 | 1257 | 2500 | 2876 | 2930 | 5806 |
While those under the age of 18 presented with the greatest number of concussions in this cohort, only 16.39% of all diagnoses within this age group were accompanied by LOC as a reported symptom, the lowest of any age group. Over half (50.4%) the patients diagnosed with a concussion between the ages of 38-59 report LOC while those >60 and 18-37 years of age report LOC for ~44% and ~33% of concussive events, respectively.
Those under the age of 18 experienced the largest increase in concussion diagnoses (Figure 2) with 1861 (LOC = 1592; nLOC = 269) more diagnoses in 2018 compared to 2013. The second largest increase was observed in the 18-37 year old age (1505) group where the increase in LOC events exceed that of the <18 age group (LOC = 427; nLOC = 1078). While the number of concussion diagnoses steadily increased by ~16% each year from 2013 to 2016, a marked increase in incidence can be seen for 2017 to 2018 where total number of concussion increased by ~115% and ~132%, respectively.
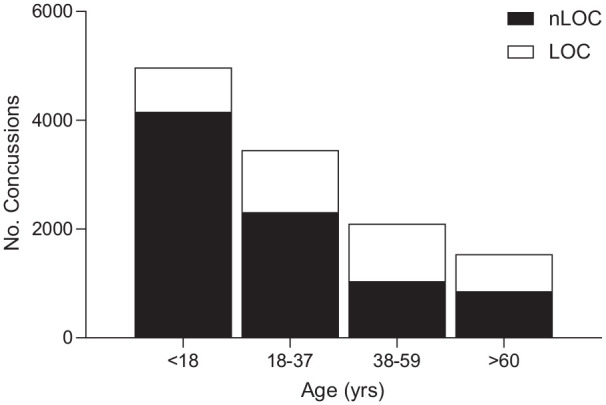
When those under the age of 20 were examined as a sub-cohort, 6362 patients had been diagnosed with a concussion (LOC = 1134; nLOC = 5228). Young male patients presented with more concussions than young female patients (males = 3446; females = 2916) with equivocal differences in LOC events between sexes (17.59% and 18.11% of concussions for young males and females, respectively). Overall, patients in the 11-15 and 16-20 age group presented with a similar number of concussions (2785 and 2615, respectively), however; those in 16-20 reported a higher prevalence of LOC as a symptom (50.88% vs 35.01%). Similar to the data reported above, a marked increase in both number of concussions and rate of growth was observed in this sub-cohort as seen in Figure 3.
Figure 3.
Year-to-year change in number of concussion diagnoses by year, type, and age for youth patients.
Abbreviations: LOC, loss of consciousness; nLOC, non-loss of consciousness.
Youth patients were diagnosed with 2338 more concussions (LOC = 364; nLOC = 1974) in 2018 compared to 2013 and the total number of concussions increased ~103.7% for both 2017 and 2018. Patients between the ages of 11-20 experienced the highest increase in the occurrence of concussions between 2013 and 2018 as summarized in Table 2.
Table 2.
Number of Diagnosed Concussions in Youth by Year.
| nLOC concussions | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 2013 |
2014 |
2015 |
2016 |
2017 |
2018 |
||||||||||||
| M | F | T | M | F | T | M | F | T | M | F | T | M | F | T | M | F | T | |
| 5 to 10 | 60 | 48 | 108 | 56 | 38 | 94 | 47 | 31 | 78 | 40 | 29 | 69 | 99 | 45 | 144 | 189 | 120 | 309 |
| 11 to 15 | 90 | 55 | 145 | 113 | 72 | 185 | 143 | 91 | 234 | 155 | 116 | 271 | 300 | 236 | 536 | 551 | 466 | 1017 |
| 16 to 20 | 38 | 49 | 87 | 50 | 61 | 111 | 70 | 73 | 143 | 109 | 106 | 215 | 259 | 235 | 494 | 471 | 517 | 988 |
| Total | 188 | 152 | 340 | 219 | 171 | 390 | 260 | 195 | 455 | 304 | 251 | 555 | 658 | 516 | 1174 | 1211 | 1103 | 2314 |
| LOC concussions | ||||||||||||||||||
| Age | 2013 |
2014 |
2015 |
2016 |
2017 |
2018 |
||||||||||||
| M | F | T | M | F | T | M | F | T | M | F | T | M | F | T | M | F | T | |
| 5 to 10 | 12 | 10 | 22 | 10 | 10 | 20 | 10 | 10 | 20 | 10 | 10 | 20 | 16 | 10 | 26 | 31 | 21 | 52 |
| 11 to 15 | 16 | 21 | 37 | 17 | 17 | 34 | 18 | 11 | 29 | 20 | 12 | 32 | 58 | 31 | 89 | 111 | 65 | 176 |
| 16 to 20 | 18 | 26 | 44 | 20 | 34 | 54 | 22 | 41 | 63 | 25 | 39 | 64 | 59 | 54 | 113 | 133 | 106 | 239 |
| Total | 46 | 57 | 103 | 47 | 61 | 108 | 50 | 62 | 112 | 55 | 61 | 116 | 133 | 95 | 228 | 275 | 192 | 467 |
| Total concussions | ||||||||||||||||||
| Age | 2013 |
2014 |
2015 |
2016 |
2017 |
2018 |
||||||||||||
| M | F | T | M | F | T | M | F | T | M | F | T | M | F | T | M | F | T | |
| 5 to 10 | 72 | 58 | 130 | 66 | 48 | 114 | 57 | 41 | 98 | 50 | 39 | 89 | 115 | 55 | 170 | 220 | 141 | 361 |
| 11 to 15 | 106 | 76 | 182 | 130 | 89 | 219 | 161 | 102 | 263 | 175 | 128 | 303 | 358 | 267 | 625 | 662 | 531 | 1193 |
| 16 to 20 | 56 | 75 | 131 | 70 | 95 | 165 | 92 | 114 | 206 | 134 | 145 | 279 | 318 | 289 | 607 | 604 | 623 | 1227 |
| Total | 234 | 209 | 443 | 266 | 232 | 498 | 310 | 257 | 567 | 359 | 312 | 671 | 791 | 611 | 1402 | 1486 | 1295 | 2781 |
Discussion
The current brief report aimed to identify recent trends in the rate of concussion diagnoses by reviewing electronic health records of approximately 8.8 million patient visits to a US healthcare system. The main finding of this retrospective analysis was that concussion diagnoses are continuing to increase, particularly among individuals younger than 20 years. Further, concussion diagnoses substantially increased from 2013 (n = 743) to 2018 (n = 5806). These results are consistent with those of Zhang et al2 who conducted a similar cross-sectional analysis of more than 8.8 million patients and also reported an increase in concussion diagnoses over time, with the highest incidence in patients aged 10 to 19 years. Further, the trends in the current investigation were similar to previous estimates from the National Electronic Injury Surveillance System for the number of ED visits for all nonfatal TBI’s among persons aged <19 years between 2001 to 2009.7 Specifically, this report indicated that the number of TBI-related ED visits related to sports and recreation activities increased approximately 62% from 2001 to 2009 with the highest rate observed among males aged 10 to 19 years.
The results from the current study are in alignment with previously published international epidemiology studies.8 However, it is difficult to directly compare and contrast specific trend data as widespread differences in the definition, diagnosis, access to care and sport participation exist globally.8,9 A population study conducted by Health Canada in 2006 reported that young males were most likely to report a concussion with more than 54% of all concussions being reported being attributable to a sports-related injury.10 More recently, a retrospective, population-based study out of Canada, indicated a 4-fold increase in concussion-related ambulatory visits per 100 000 children from 2003 to 2013, with the greatest increase observed in patients between the ages of 13 to 19 years old, which is similar to the age trend reported in the current study.11
Although the increase in concussion diagnoses reported here may indicate an increased frequency of injury, heightened awareness in the past decade regarding the risk of long-term health outcomes from TBI is likely a strong contributor to the rapid increase in concussion diagnoses. This heightened awareness has also led to increasingly stringent policies and procedures for concussion detection, management, and return-to-play protocols among athletic organizations,12 which likely decreases the number of sport-related concussions that previously might have remained undiagnosed. It is also possible that increased participation in sport-related activities may have a role in the rise in concussions; most concussions and TBI-related injuries appear to be associated with sports, with an estimated 1.1 to 1.9 million sport-related concussions occurring annually.7,13 A recent meta-analysis reported rugby, hockey and American football to have the highest incidence rates per 1000 athlete exposures with rates of 4.18, 1.2, and 0.53, respectively.13 Young male athletes, in particular, appear to be at a higher risk of TBI with 71% of all sports and recreation-related TBI’s during 2001 to 2009 to be among males. Sports and recreation-related activities involving a high degree of contact or risks of falls such as hockey/ice skating, football, soccer, horseback riding, tobogganing/sledding, and all-terrain vehicle riding appear to have the highest percentage of ED visits that were attributable to TBI’s.7 Therefore, the higher incidence of concussions in those <18 years observed in the current study, could be a result of increased sport activity and recreation-related activities that inherently increase the risk for high contact events compared to older adult populations. However, because data regarding the mechanisms of injury for this cohort are unavailable, these contributions are speculative.
Limitations
Limitations of the current study include the inherent shortcomings of a retrospective analysis of patient records. As such, we lacked information about the mechanisms of injury, detailed demographic characteristics, and post-concussion outcomes. Thus, we are unable to identify causal relationships that explain the increase in concussions or any relationship between injury mechanism and symptom severity. Finally, the study was not able to account for undiagnosed or unreported concussions. There is also a bias of underreporting actual concussion occurrences as not all patients may seek medical care and receive a documented concussion diagnosis.
Conclusion
The data presented herein support previous studies reporting increased rates of concussion diagnoses across the United States. This increase is particularly marked in pediatric patients (≤19 years). In the future, more research should focus on preventative measures to help reduce the incidence of concussion. Thankfully, several sport organizations have adopted a standardized step wise “Return to Play” protocol to ensure an athlete is fully recovered from a concussion before returning to their sport.
Footnotes
Abbreviations: ED, emergency department.
LOC, loss of consciousness.
nLOC, no loss of consciousness.
STROBE, Strengthening the Reporting of Observational Studies in Epidemiology.
TBI, traumatic brain injury.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Andrew T. Askow  https://orcid.org/0000-0002-0757-8943
https://orcid.org/0000-0002-0757-8943
Jacob L. Erickson  https://orcid.org/0000-0002-9975-8836
https://orcid.org/0000-0002-9975-8836
Andrew R. Jagim  https://orcid.org/0000-0002-6651-5096
https://orcid.org/0000-0002-6651-5096
References
- 1. Harmon KG, Clugston JR, Dec K, et al. American Medical Society for Sports Medicine position statement on concussion in sport. Br J Sports Med. 2019;53:213-225. [DOI] [PubMed] [Google Scholar]
- 2. Zhang AL, Sing DC, Rugg CM, Feeley BT, Senter C. The rise of concussions in the adolescent population. Orthop J Sports Med. 2016;4:2325967116662458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Winkler EA, Yue JK, Burke JF, et al. Adult sports-related traumatic brain injury in United States trauma centers. Neurosurg Focus. 2016;40:E4. [DOI] [PubMed] [Google Scholar]
- 4. Taylor CA, Bell JM, Breiding MJ, Xu L. Traumatic brain injury-related emergency department visits, hospitalizations, and deaths—United States, 2007 and 2013. MMWR Surveill Summ. 2017;66:1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Montenigro PH, Alosco ML, Martin BM, et al. Cumulative head impact exposure predicts later-life depression, apathy, executive dysfunction, and cognitive impairment in former high school and college football players. J Neurotrauma. 2017;34:328-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344-349. [DOI] [PubMed] [Google Scholar]
- 7. Centers for Disease Control and Prevention. Nonfatal traumatic brain injuries related to sports and recreation activities among persons aged ≤19 years—United States, 2001-2009. MMWR Morb Mortal Wkly Rep. 2011;60:1337-1342. [PubMed] [Google Scholar]
- 8. Hon KL, Leung AKC, Torres AR. Concussion: a global perspective. Semin Pediatr Neurol. 2019;30:117-127. [DOI] [PubMed] [Google Scholar]
- 9. Kazl C, Torres A. Definition, classification, and epidemiology of concussion. Semin Pediatr Neurol. 2019;30:9-13. [DOI] [PubMed] [Google Scholar]
- 10. Gordon KE, Dooley JM, Wood EP. Descriptive epidemiology of concussion. Pediatr Neurol. 2006;34:376-378. [DOI] [PubMed] [Google Scholar]
- 11. Zemek RL, Grool AM, Rodriguez Duque D, et al. Annual and seasonal trends in ambulatory visits for pediatric concussion in Ontario between 2003 and 2013. J Pediatr. 2017;181:222-228.e2. [DOI] [PubMed] [Google Scholar]
- 12. Yang J, Comstock RD, Yi H, Harvey HH, Xun P. New and recurrent concussions in high-school athletes before and after traumatic brain injury laws, 2005 to 2016. Am J Public Health. 2017;107:1916-1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pfister T, Pfister K, Hagel B, Ghali WA, Ronksley PE. The incidence of concussion in youth sports: a systematic review and meta-analysis. Br J Sports Med. 2016;50:292-297. [DOI] [PubMed] [Google Scholar]