Abstract
Background:
Poor sleep quality is prevalent among patients with rotator cuff tears (RCTs) and negatively influences the potential for healing and quality of life. However, there is a paucity of literature describing the magnitude and timing of changes in sleep quality after arthroscopic rotator cuff repair (RCR).
Purpose:
(1) To evaluate the prevalence of poor sleep quality in patients undergoing arthroscopic RCR and (2) to determine the timing and magnitude of changes in sleep quality after RCR.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
PubMed, OVID/Medline, and Cochrane databases were queried in January 2020 for literature investigating the prevalence of poor sleep quality in patients with RCTs or changes in sleep quality after arthroscopic RCR. Data pertaining to study characteristics, risk of bias, sleep quality assessments, and clinical outcomes were extracted. A qualitative analysis of the prevalence of poor sleep quality and changes in sleep quality was performed.
Results:
A total of 8 studies (1034 patients) were included. The mean Pittsburgh Sleep Quality Index (PSQI) ranged from 5.2 to 15.0 preoperatively among all studies, while the frequency of patients experiencing poor sleep quality ranged from 40.8% to 89.0% in 4 studies. Four studies reported the mean PSQI at a minimum of 6 months postoperatively, which ranged from 4.2 to 7.1. Four studies did not report the PSQI score or the proportion of patients who experienced poor postoperative sleep quality. One study evaluated the PSQI at 12 months postoperatively, which decreased to 4.2 from 5.8 at 6 months. One study evaluated the PSQI at 24 months postoperatively, which decreased to 5.5 from 6.2 at 6 months.
Conclusion:
Patients with RCTs have a high prevalence of poor sleep quality. Consistent improvements in sleep quality are observed in the 6 months after arthroscopic RCR, but there is limited evidence based on the available data to characterize changes in sleep quality beyond this time. More evidence is needed to characterize changes in sleep quality beyond 6 months and how these changes are perceived by this patient population.
Keywords: sleep, rotator cuff, Pittsburgh Sleep Quality Index, repair, arthroscopic
Sleep disturbance is commonly associated with rotator cuff pathology and has been linked to the increased production of inflammatory cytokines at night.2,15,17 Indeed, it has been estimated that only 11% of patients with symptomatic rotator cuff tears have normal sleep.2,14,17 As such, sleep quality has gained attention as a component of health that requires attention in patients undergoing rotator cuff repair (RCR).2
Sleep is a dynamic form of fluctuations in cognitive activity and allows for energy conservation and reorganization of neuronal activity.21 Periods of four consecutive nights with <6 hours of sleep have been associated with impaired cognitive performance, altered glucose metabolism, and appetite dysregulation.6,11,16,27 Poor sleep quality has also been shown to negatively influence quality of life and contribute to depression and anxiety.3,5 As sleep quality constitutes an important role in postoperative healing and overall patient satisfaction, it is imperative to continue to investigate these disturbances in patients undergoing RCR to mitigate potential negative health effects.26 To this end, a number of recent studies have aimed to examine and quantify the influence of RCR on changes in sleep quality.
Austin et al2 studied the influence that arthroscopic RCR had on changes in sleep quality and reported that sleep was significantly improved after surgical intervention but was negatively affected by pre- and postoperative narcotic pain medication use.14 However, other studies have disputed the association of narcotic use with sleep change quality8 and reported varying degrees in the timing and magnitude of changes in sleep quality after arthroscopic RCR.7,10,22 Furthermore, investigative efforts that have evaluated additional factors that interact with and influence sleep quality in patients with rotator cuff disease remain limited.15,23
For the aforementioned reasons, the purpose of the current study was (1) to evaluate the prevalence of poor sleep quality in patients undergoing arthroscopic RCR and (2) to determine the timing and magnitude of changes in sleep quality after RCR. We hypothesized that the prevalence of poor sleep quality was high before arthroscopic intervention and that sleep quality would improve early in the postoperative period.
Methods
Article Identification and Selection Process
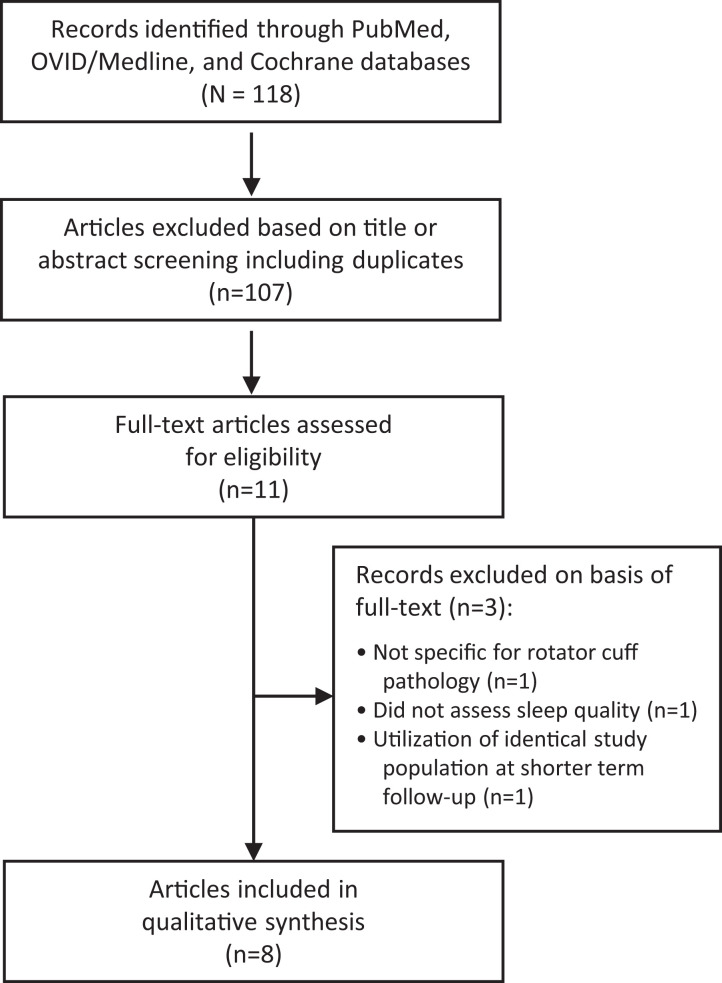
Articles were extracted in accordance with the 2009 PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.20 Utilizing the Boolean search terms rotator cuff and sleep, the query for studies was performed in January 2020 for published literature pertaining to arthroscopic RCR and sleep quality assessments. The query was performed using the Cochrane Database of Systematic Reviews, the Cochrane Central Register of Controlled Trials, PubMed (2008-2019), and OVID/Medline (2008-2019).
Inclusion criteria for the search consisted of all studies published in the English language reporting information regarding the assessment of sleep quality in patients who underwent arthroscopic RCR. Exclusion criteria consisted of cadaveric studies, animal studies, basic science articles, editorial articles, surveys or case reports, open RCR, and articles evaluating sleep quality for other musculoskeletal pathology. No study follow-up restriction was utilized because the purpose of this study was to determine changes in sleep quality regardless of the time, and this would increase the overall study yield.
Two investigators (K.N.K., D.M.R.) independently reviewed the abstracts from all identified articles. Articles were excluded on the basis of the title and abstract if they failed to mention the rotator cuff and sleep quality. Full-text articles were obtained for review to allow further assessment of inclusion and exclusion criteria when necessary. A thorough review of references from the included studies was also performed to ensure that no studies were missed through the systematic search.
Quality Assessment
The Methodological Index for Non-randomized Studies (MINORS) checklist13 was used to evaluate the quality of all included studies. The checklist involves 12 items to assess quality, 4 of which are applicable to comparative studies. The 4 additional criteria specific to comparative groups were used to assess the bias present in articles when selecting cohorts. The maximum MINORS score is 16 for noncomparative studies and 24 for comparative studies. Each study was scored by 1 author (D.M.R.).
Data Extraction and Statistical Analysis
All data were recorded in a custom spreadsheet using a modified information extraction table.12 The level of evidence of the studies was assigned according to the classification as specified by Wright et al.29 Categories for data collection for each full article included publication characteristics, patient demographics, inclusion and exclusion criteria, outcome tool to assess sleep quality, and patient-reported outcome scores. Means and standard deviations were extracted to calculate pooled values for patient demographics, while ranges were reported for the primary outcome of sleep quality to avoid potential bias incurred through improper pooling given the study heterogeneity and variable reporting. Forest plots were constructed to depict pre- and postoperative Pittsburgh Sleep Quality Index (PSQI) scores among the studies. All descriptive analyses were performed in Stata Version 16.1 (StataCorp). Forest plots were generated using the computing software R (Version 1.2.1335; R Foundation for Statistical Computing).
Results
Study Characteristics and Heterogeneity
A total of 8 studies with a total of 1034 patients undergoing primary arthroscopic RCR were included in the final analysis (Figure 1).
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart for study selection.
Of these patients, 486 were male and 548 were female. The pooled age and body mass index (mean ± SD) among all patients were 61.2 ± 2.8 years and 29.2 ± 0.9 kg/m2. Of the included studies, 4 were case series, 2 were cohort studies, and 2 were cross-sectional studies. Additional study methodology is presented in Table 1.
Table 1.
Study Characteristics, Methodology, and Sleep Quality Assessmentsa
| Criteria | Mean PSQI / Sleep Disturbance, % | |||||
|---|---|---|---|---|---|---|
| Lead Author (Year) | LOE | No. | Inclusion | Exclusion | Pre | Post |
| Cho (2015)7 | 4 | 47 | Primary arthroscopic RCR without concomitant procedures, ASA score <3 | Presence of massive RCT (>5 cm), ASA score ≥3, history of drug addiction, severe neurological lesion, allergy to any medication or local anesthetics used in study | 6.6/— | 5.8/—, 4.2/—b |
| Gumina (2016)10 | 3 | 508 | Primary arthroscopic RCR with RCT diagnosed through physical examination, radiograph, and MRI | Previous operation on ipsilateral shoulder, inflammatory joint disease, GHOA of the operative or contralateral shoulder | 5.2/40.8 | — |
| Horneff (2017)14 | 4 | 56 | Primary arthroscopic RCR without concomitant procedures | Workers’ compensation benefits, irreparable tears, revision surgery, and concomitant severe GHOA or adhesive capsulitis | 11.7/89 | 6.2/38, 5.5/41c |
| Reyes (2017)22 | 4 | 209 | Primary arthroscopic RCR with a unilateral symptomatic full-thickness RCT confirmed by MRI | Age <18 y, bilateral shoulder symptoms, RCT arthropathy, isolated subscapularis tears, bilateral full-thickness RCT, partial-thickness RCT, prior shoulder surgery, shoulder injections within the subacromial space or glenohumeral joint in the previous 6 mo, acute shoulder fractures or dislocations within previous 6 mo, history of psychotic or mood disorders, dementia, current substance abuse, current diagnosis of a sleep disorder | 9.8/— | — |
| Serbest (2017)23 | 4 | 31 | Primary arthroscopic RCR with full-thickness RCT that failed treatment with NSAIDs or physiotherapy after at least 3 mo | Irreparable tears, revision surgery, open RCR, severe GHOA, adhesive capsulitis, sleep apnea disorder, neuropsychiatric disease, taking medication for sleep disorder, follow-up <6 mo | 15/— | 6/58 |
| Khazzam (2018)15 | 4 | 117 | Patients with a clinical diagnosis of impingement or full-thickness RCT | Inability to complete the questionnaire, lack of a diagnosis of rotator cuff disease, prior shoulder surgery, acute fractures involving the proximal humerus or shoulder girdle, glenohumeral joint instability, other shoulder pathology not involving the rotator cuff, glenohumeral joint arthritis, adhesive capsulitis, RCT arthropathy with pseudoparalysis, documented history of psychotic or mood disorder, current substance abuse, diagnosed sleep disorder | 9.5/— | — |
| Glogovac (2019)8 | 4 | 48 | Primary arthroscopic RCR without concomitant procedures | — | 9.5/79 | 7.1/53 |
| Ansok (2020)1 | 2 | 18 | Full-thickness rotator cuff tear as determined by ultrasound or MRI | Prior RCR, previously diagnosed primary sleep disorder, severe GHOA, adhesive capsulitis | 8.4/— | — |
aDashes (—) indicate not reported. ASA, American Society of Anesthesiologists score; GHOA, glenohumeral osteoarthritis; LOE, level of evidence; MRI, magnetic resonance imaging; NSAID, nonsteroidal anti-inflammatory drug; Post, postoperative; Pre, preoperative; PSQI, Pittsburgh Sleep Quality Index; RCR, rotator cuff repair; RCT, rotator cuff tear.
bIndicates sleep quality beyond 6-month postoperative time point.
cIndicates sleep quality beyond 12-month postoperative time point.
Sleep Quality Assessment
All 8 studies evaluated sleep quality using the PSQI. The PSQI is a validated sleep quality assessment tool that has been used in many orthopaedic subspecialties to investigate and quantify the presence or absence of sleep abnormalities, with a score ≥5 indicative of poor sleep quality.4 The total PSQI score ranges from 0 to 21, with higher PSQI scores indicating higher degrees of sleep abnormality.
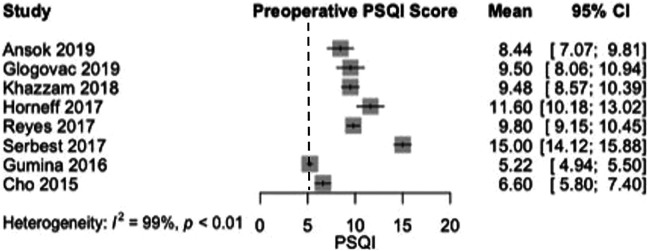
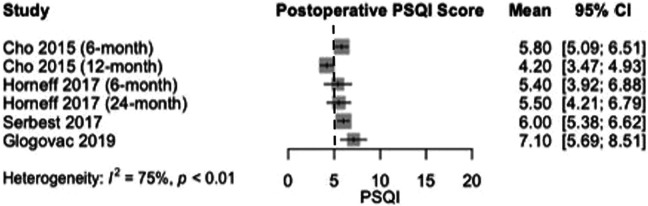
The mean PSQI ranged from 5.2 to 15.0 preoperatively among all studies (Figure 2), while the frequency of patients experiencing poor sleep quality based on the PSQI ranged from 40.8% to 89.0% in 4 studies. Heterogeneity for preoperative PSQI scores among the studies was very high (I 2 = 99%). Four studies reported the mean PSQI at a minimum of 6 months postoperatively, which ranged from 4.2 to 7.1 (Figure 3). Four studies did not report the PSQI score or the proportion of patients who experienced poor sleep quality postoperatively.
Figure 2.
Forest plot displaying the mean Pittsburgh Sleep Quality Index (PSQI) and 95% CI before rotator cuff repair. The pooled preoperative PSQI for all studies was 9.5. The dotted line indicates a PSQI equal to 5, which is the threshold for poor sleep quality.
Figure 3.
Forest plot displaying the mean Pittsburgh Sleep Quality Index (PSQI) and 95% CI at minimum 6-month follow-up after rotator cuff repair. The pooled postoperative PSQI for all studies was 5.7 (vs 9.5 preoperatively). The dotted line indicates a PSQI equal to 5, which is the threshold for poor sleep quality.
Two studies reported on sleep quality at >6 months postoperatively. Horneff et al14 performed a 2-year follow-up study from a cohort of 56 patients who underwent arthroscopic RCR in 2015. The follow-up in their study decreased by 33.9% to 37 patients at the time of their analysis. At 6 months postoperatively, the mean PSQI decreased from 11.7 to 6.2, and the prevalence of poor sleep quality decreased from 89% to 38% (P < .01). In their subsequent study, they reported that 41% of patients continued to experience poor sleep quality at a minimum of 2 years postoperatively and had a mean PSQI of 5.5 ± 4.0, which was not significantly different from the PSQI at postoperative month 6. Interestingly, they determined that the only independent demographic or surgical parameter that affected postoperative sleep was the continued use of narcotic pain medication, with patients using such medication having a mean PSQI of 12.5, as opposed to a mean score of 5.1 in nonusers. Likewise, Cho et al7 found that the mean PSQI score decreased from 6.6 ± 3.6 preoperatively to 5.8 ± 3.2 at 6 months postoperatively and 4.2 ± 3.3 at 12 months (P = .006).
Ansok et al1 was the only study that included an objective assessment of sleep quality as part of their investigation. In addition to administering the PSQI, all patients were provided with a Philips Respironics Actiwatch Spectrum Plus and wore this continuously for 2 weeks. One button on the watch allowed patients to indicate their time of intent to sleep as well as their time of awakening. They also had patients subjectively record these same measures. No objective sleep measures were found to correlate with the PSQI. Interestingly, the authors found that patients significantly overreported their duration of sleep by a mean 89.7 minutes (P < .001) and sleep efficiency by a mean 17.72% (P < .001). The authors reported that, when compared with a historical cohort of patients with normal sleep quality and no rotator cuff tears, patients with rotator cuff tears demonstrated significantly worse sleep duration, sleep efficiency, wake after sleep onset, and sleep onset latency (P < .001 for all).
Association of Shoulder-Specific Patient-Reported Outcomes With Sleep Quality
Two studies investigated the association between shoulder-specific patient-reported outcomes and sleep quality. Cho et al7 found that the mean visual analog scale (VAS) pain score decreased from 6.7 ± 1.6 to 1.3 ± 1.4, the mean University of California, Los Angeles score increased from 12.8 ± 4.9 to 31.0 ± 3.3, and the mean American Shoulder and Elbow Surgeons (ASES) score increased from 42.5 ± 16.5 to 87.2 ± 10.9 (P < .001) at 12 months postoperatively. There were no significant correlations between clinical outcome scores and the PSQI score. Horneff et al14 reported that statistically significant improvements were observed in the Simple Shoulder Test and the VAS pain score at 24 months postoperatively (P < .001 for both). Furthermore, these outcomes moderately correlated with the PSQI score (VAS, Spearman rho = 0.479 [P < .001]; Simple Shoulder Test, Spearman rho = −0.505 [P < .001]). Khazzam et al15 found that the mean VAS pain score was significantly correlated with the PSQI in patients with full-thickness rotator cuff tears (0.27; P = .004); however, no significant correlations existed between the PSQI and the ASES or Single Assessment Numeric Evaluation (SANE) score.
The remaining 5 studies did not assess shoulder-specific outcomes or their association with the PSQI, nor did they assess non–shoulder-specific outcomes. Serbest et al23 evaluated changes in the Constant and Western Ontario Rotator Cuff Index at 6-month follow-up and found significant improvements, but they did not analyze the association between these outcomes and the PSQI. Likewise, Gumina et al10 and Reyes et al22 did not evaluate the relationship between the PSQI and clinical outcomes.
Ansok et al1 reported that the VAS pain score was significantly correlated with the PSQI (r = 0.5260; P = .0249), but they did not assess associations between shoulder-specific clinical or functional outcomes and the PSQI. Glogovac et al8 found that the Connor-Davidson Resilience Scale score, a measure of the ability to cope with stress, was correlated with the PSQI (R 2 = 0.09; P = .028); however, they did not assess associations between shoulder-specific clinical or functional outcomes and the PSQI.
Bias Assessment
The mean MINORS score was 12.3 ± 2.2, indicating moderate methodological bias of the studies in the review. The level of methodological quality may partially explain the heterogeneity of results and outcome reporting found among the studies in this review. For example, excessive lost-to-follow-up percentages and inappropriate follow-up periods may lead to selection biases, and patients who continue to follow up may be those who experience better sleep quality. Table 2 details the missing criteria accounting for the methodological bias in the included studies.
Table 2.
Bias Assessment Using MINORS Criteriaa
| Itemb | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lead Author (Year) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | Totalc |
| Cho (2015)7 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 15 | ||||
| Gumina (2016)10 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 1 | 2 | 2 | 2 | 0 | 15 |
| Horneff (2017)14 | 2 | 1 | 2 | 2 | 0 | 2 | 1 | 0 | 10 | ||||
| Reyes (2017)22 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 14 | ||||
| Serbest (2017)23 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 1 | 9 | ||||
| Khazzam (2018)15 | 2 | 0 | 2 | 2 | 0 | 0 | 0 | 1 | 7 | ||||
| Glogovac (2019)8 | 2 | 2 | 2 | 2 | 0 | 2 | 1 | 1 | 12 | ||||
| Ansok (2020)1 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 21 |
aBlank cells indicate not applicable. MINORS, Methodological Index for Non-randomized Studies.
bItems: 1, a clearly stated aim; 2, inclusion of consecutive patients; 3, prospective collection of data; 4, endpoint appropriate to the aim of the study; 5, unbiased assessment of the study endpoint; 6, follow-up period appropriate to the aim of the study; 7, loss of follow-up <5%; 8, prospective calculation of study size; 9, an adequate control group; 10, contemporary group used; 11, baseline equivalence of groups; 12, adequate statistical analysis.
cMaximum score: 16 for items 1-8 (noncomparative studies) and 24 for items 1-12 (comparative studies).
Discussion
The principal findings of the current study were as follows. First, the prevalence of poor sleep quality among patients undergoing arthroscopic RCR was high, ranging between 40.8% and 89%, while the PSQI ranged from 6.6 to 15. Second, among the 4 studies that reported postoperative changes in sleep quality, the prevalence of poor sleep quality ranged from 38% to 58%, while the PSQI ranged from 4.2 to 7.1. Finally, 2 studies investigated sleep quality at a follow-up period >6 months after arthroscopic RCR, which demonstrated that improvements in sleep quality were maintained at 12 and 24 months as opposed to the preoperative period but still indicated a high burden of poor sleep quality.
The current study found that poor sleep quality was prevalent among patients undergoing arthroscopic RCR, as the PSQI ranged from 6.6 to 15.0. This finding is in accordance with the reported prevalence of poor sleep quality in other orthopaedic subspecialties.9,18,19,24,25,28 Despite the recent shift toward modifying preoperative factors that may portend a suboptimal outcome, efforts toward actively addressing poor sleep quality have yet to be adopted. Although the cause of disruptions in sleep quality is likely multifactorial, there is evidence that patients’ perception of their injury and the pain they experience are both contributors to this phenomenon.16 Furthermore, Khazzam et al15 found 9 variables with statistically significant associations with poor sleep quality in patients with rotator cuff tears: hypertension (0.29; P = .002), depression (0.27; P = .002), pain per VAS (0.27; P = .004), low back pain (0.25; P = .007), female sex (0.24; P = .001), diabetes mellitus (0.24; P = .01), and body mass index (0.22; P = .02). Serbest et al23 found that nonmodifiable factors such as acromioclavicular osteoarthritis, the operated side, size of the rotator cuff tear, the number of stabilizing sutures, biceps tenotomy, subacromial decompression, and the application of distal clavicular excision did not have any association with the PSQI. Future studies are warranted to test and delineate protocols consisting of behavioral or pharmaceutical intervention to address modifiable factors associated with poor sleep to improve the sleep quality among these patients.
Interestingly, sleep quality appeared to consistently improve after arthroscopic RCR, decreasing in prevalence by up to 53%. However, of the 4 studies that reported postoperative sleep quality, only 1 demonstrated that the mean PSQI among all patients dropped to <5, indicating return to normal sleep quality.7 The lower bound of the 95% CI of the mean PSQI score at 24 months in the study by Horneff et al14 crossed the PSQI cutoff of 5 for poor sleep quality and may not be conclusive, while the lower bound of the 95% CI of the remaining 2 studies did not touch this cutoff.8,23 Furthermore, it is yet to be determined whether these changes in sleep are clinically meaningful, despite using this validated outcome tool. Although these studies demonstrate consistent sleep improvements, 2 studies assessed sleep at longer-term follow-up, with the longest follow-up showing a trend toward a reemergence of poor sleep quality among patients. This finding is certainly concerning given the numerous adverse effects on healing and mental health with which poor sleep quality is associated, especially in the RCR population. A possible explanation, given that only 2 studies sought to quantify postoperative clinical outcomes, is that poor function or RCR failure continued to contribute to poor sleep quality. Selection bias inherent to the studies identified in this review is also likely a contributor, as patients who choose not to respond to the postoperative surveys may represent those who experienced the greatest benefit after surgery. Regardless, although patients may experience rapid improvements in sleep quality, it is uncertain whether these improvements are clinically significant and whether they are sustained at longer-term follow-up. Notably, only 2 studies investigated changes in sleep quality >6 months after RCR; therefore, the improvements observed in the current review may not necessarily be applicable to all patients. Future studies must continue to assess changes in sleep quality throughout the postoperative period, and patients may benefit from these serial assessments, as better understanding the postoperative course of changes in sleep quality may offer opportunities for intervention to improve patient outcomes.
The current study results must be interpreted in the context of a few limitations. The number of studies in this systematic review was small, and a larger body of evidence may change the trends identified. The study designs also limit the findings of this systematic review, as only 50% of studies reported any follow-up and the studies are of a low level of evidence. Moreover, just 2 of the studies that reported follow-up did so at >6 months postoperatively. However, these findings emphasize the need for future research to address this relatively recent concern that is poor sleep quality, which may have significant health effects and portend worse outcomes.
Conclusion
Patients with rotator cuff tears have a high prevalence of poor sleep quality. Consistent improvements in sleep quality are observed within 6 months of arthroscopic RCR, but there is limited evidence based on the available data to characterize changes in sleep quality past this time. More evidence is needed to characterize changes in sleep quality beyond 6 months and how these changes are perceived by this patient population.
Footnotes
Final revision submitted June 24, 2020; accepted July 7, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: J.C. has received educational support from Arthrex and Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Ansok CB, Khalil LS, Muh S. Objective assessment of sleep quality in patients with rotator cuff tears. Orthop Traumatol Surg Res. 2020;106(1):61–66. [DOI] [PubMed] [Google Scholar]
- 2. Austin L, Pepe M, Tucker B, et al. Sleep disturbance associated with rotator cuff tear: correction with arthroscopic rotator cuff repair. Am J Sports Med. 2015;43(6):1455–1459. [DOI] [PubMed] [Google Scholar]
- 3. Badcock LJ, Lewis M, Hay EM, McCarney R, Croft PR. Chronic shoulder pain in the community: a syndrome of disability or distress? Ann Rheum Dis. 2002;61(2):128–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 5. Cho CH, Jung SW, Park JY, Song KS, Yu KI. Is shoulder pain for three months or longer correlated with depression, anxiety, and sleep disturbance? J Shoulder Elbow Surg. 2013;22(2):222–228. [DOI] [PubMed] [Google Scholar]
- 6. Cho CH, Seo HJ, Bae KC, Lee KJ, Hwang I, Warner JJ. The impact of depression and anxiety on self-assessed pain, disability, and quality of life in patients scheduled for rotator cuff repair. J Shoulder Elbow Surg. 2013;22(9):1160–1166. [DOI] [PubMed] [Google Scholar]
- 7. Cho CH, Song KS, Hwang I, Warner JJ. Does rotator cuff repair improve psychologic status and quality of life in patients with rotator cuff tear? Clin Orthop Relat Res. 2015;473(11):3494–3500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Glogovac G, Schumaier AP, Kennedy ME, et al. Narcotic use and resiliency scores do not predict changes in sleep quality 6 months after arthroscopic rotator cuff repair. Orthop J Sports Med. 2019;7(7):2325967119856282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gong L, Wang Z, Fan D. Sleep quality effects recovery after total knee arthroplasty (TKA)—a randomized, double-blind, controlled study. J Arthroplasty. 2015;30(11):1897–1901. [DOI] [PubMed] [Google Scholar]
- 10. Gumina S, Candela V, Passaretti D, Venditto T, Mariani L, Giannicola G. Sleep quality and disturbances in patients with different-sized rotator cuff tear. Musculoskelet Surg. 2016;100(suppl 1):33–38. [DOI] [PubMed] [Google Scholar]
- 11. Ha E, Lho YM, Seo HJ, Cho CH. Melatonin plays a role as a mediator of nocturnal pain in patients with shoulder disorders. J Bone Joint Surg Am. 2014;96(13):e108. [DOI] [PubMed] [Google Scholar]
- 12. Harris JD, Quatman CE, Manring MM, Siston RA, Flanigan DC. How to write a systematic review. Am J Sports Med. 2014;42(11):2761–2768. [DOI] [PubMed] [Google Scholar]
- 13. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Horneff JG, 3rd, Tjoumakaris F, Wowkanech C, Pepe M, Tucker B, Austin L. Long-term correction in sleep disturbance is sustained after arthroscopic rotator cuff repair. Am J Sports Med. 2017;45(7):1670–1675. [DOI] [PubMed] [Google Scholar]
- 15. Khazzam MS, Mulligan EP, Brunette-Christiansen M, Shirley Z. Sleep quality in patients with rotator cuff disease. J Am Acad Orthop Surg. 2018;26(6):215–222. [DOI] [PubMed] [Google Scholar]
- 16. Kunze KN, Leong NL, Beck EC, Bush-Joseph CA, Nho SJ. Hip arthroscopy for femoroacetabular impingement improves sleep quality postoperatively. Arthroscopy. 2019;35(2):461–469. [DOI] [PubMed] [Google Scholar]
- 17. Longo UG, Facchinetti G, Marchetti A, et al. Sleep disturbance and rotator cuff tears: a systematic review. Medicina (Kaunas). 2019;55(8):453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Manning BT, Kearns SM, Bohl DD, Edmiston T, Sporer SM, Levine BR. Prospective assessment of sleep quality before and after primary total joint replacement. Orthopedics. 2017;40(4):e636–e640. [DOI] [PubMed] [Google Scholar]
- 19. Martinez R, Reddy N, Mulligan EP, Hynan LS, Wells J. Sleep quality and nocturnal pain in patients with hip osteoarthritis. Medicine (Baltimore). 2019;98(41):e17464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. BMJ. 2009;339:B2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Onen SH, Onen F, Courpron P, Dubray C. How pain and analgesics disturb sleep. Clin J Pain. 2005;21(5):422–431. [DOI] [PubMed] [Google Scholar]
- 22. Reyes BA, Hull BR, Kurth AB, Kukowski NR, Mulligan EP, Khazzam MS. Do magnetic resonance imaging characteristics of full-thickness rotator cuff tears correlate with sleep disturbance? Orthop J Sports Med. 2017;5(11):2325967117735319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Serbest S, Tiftikci U, Askin A, Yaman F, Alpua M. Preoperative and post-operative sleep quality evaluation in rotator cuff tear patients. Knee Surg Sports Traumatol Arthrosc. 2017;25(7):2109–2113. [DOI] [PubMed] [Google Scholar]
- 24. Shakya H, Wang D, Zhou K, Luo ZY, Dahal S, Zhou ZK. Prospective randomized controlled study on improving sleep quality and impact of zolpidem after total hip arthroplasty. J Orthop Surg Res. 2019;14(1):289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Trouw AG, Patel A, Yang A, Jauregui J, Caligiuri D, Choueka J. Improvement in sleep quality after carpal tunnel release. J Long Term Eff Med Implants. 2018;28(1):55–61. [DOI] [PubMed] [Google Scholar]
- 26. Veldhuis JD, Iranmanesh A. Physiological regulation of the human growth hormone (GH)–insulin-like growth factor type I (IGF-I) axis: predominant impact of age, obesity, gonadal function, and sleep. Sleep. 1996;19(10):S221–S224. [DOI] [PubMed] [Google Scholar]
- 27. Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Weinberg M, Mollon B, Kaplan D, Zuckerman J, Strauss E. Improvement in sleep quality after total shoulder arthroplasty. Phys Sportsmed. 2020;48(2):194–198. [DOI] [PubMed] [Google Scholar]
- 29. Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85(1):1–3. [PubMed] [Google Scholar]