Abstract
Background:
Long head of biceps tendon pathology is a well-described source of pain in the anterior adult shoulder. Shoulder arthroscopic surgeons face this condition on a frequent basis because of the increasing aging population. Trends in treatment for this condition have varied over recent decades. An understanding of these trends may help orthopaedic surgeons counsel these patients.
Purpose:
To evaluate trends in treatment selection, patient population, and complications in recent part II examinees of the American Board of Orthopaedic Surgery (ABOS) board examination.
Study Design:
Cross-sectional study.
Methods:
Using a database maintained by the ABOS, we accessed and analyzed examinee data from 2008 to 2019 to evaluate trends in the following categories: examination year/subspecialty, region, patient age/sex, International Classification of Diseases code, Current Procedural Terminology code, and complications. These data points were analyzed for all board-eligible candidates from 2008 to 2019.
Results:
The annual number of proximal biceps tendon (PBT) procedures performed increased significantly from 597 cases in 2008 to 2203 cases in 2019 (P < .001). Incidence of biceps tendon tenotomy significantly decreased between the years 2007 and 2018 (P < .001). Both open and arthroscopic biceps tenodesis significantly increased between 2007 and 2018 (P < .001). Most PBT cases were performed simultaneously with other procedures (17,283/17,861; 96.8%). The most common PBT procedure performed overall was open tenodesis of long tendon of biceps (∼60.8%). Complication rates for PBT procedures reported each year did not significantly change between 2007 and 2018 (7.5% vs 9.7%; P = .103).
Conclusion:
PBT procedures are being increasingly performed among recently trained orthopaedic surgeons. Proximal biceps tenotomy has significantly declined, whereas proximal biceps tenodesis, open or arthroscopic, has significantly increased, demonstrating a possible shift in the standard of care among new surgeons.
Keywords: biceps tendon, arthroscopy, biceps tenodesis, biceps tenotomy
The long head of biceps tendon (LHBT) is a well-described source of pain in the anterior adult shoulder. Chronic LHBT pathology is seen in up to 75% of patients with rotator cuff tears.15 Shoulder arthroscopic surgeons and surgeons who perform open procedures, such as shoulder arthroplasty and open rotator cuff repair, commonly face this condition, and trends in treatment have varied over the past 2 decades.
The most frequently used interventions are tenotomy and tenodesis. Multiple systematic reviews and meta-analyses have been performed to evaluate outcomes after these procedures.6,12,21 The most commonly accepted benefits of tenotomy include decreased operative times, decreased cost, and easier rehabilitation.2,16 This, however, comes at the cost of increased risk of muscular deformity (ie, Popeye sign), recurrent biceps cramping and, despite a lack of concrete evidence, a fear of strength and endurance deficits with biceps use. Tenodesis offers a theoretical cosmetic advantage but otherwise has not been shown to be functionally beneficial.5,11,21 Biomechanical data have suggested that tenodesis offers stronger biomechanical properties over tenotomy.1,13,20 One cadaveric study demonstrated a 2.8 times higher load to failure for tenodesis compared with tenotomy (311 vs 111 N).22 Although tenodesis has a theoretical biomechanical advantage, some authors suggest that tenotomy offers significantly better results in shoulder function compared with tenodesis.3 Understanding other surgeons’ treatment selection trends may benefit the provider when discussing these options with patients.
The American Board of Orthopaedic Surgery (ABOS) recently created a case submission database for all sitting candidates between the years 2008 and 2019, representing an operative period between the years 2007 and 2018. Candidates performing surgery in 2007, underwent board examination in 2008. Likewise, candidates performing surgery in 2018, underwent board examination in 2019. Thus, the surgical cases occurred from 2007 to 2018, while the board examinations occurred from 2008-2019. The data are organized according to examination year/subspecialty, region, patient age and sex, International Classification of Diseases code, Current Procedural Terminology (CPT) code, and complications. This data set can be useful in analyzing the trends in practice of board-eligible orthopaedic surgeons, as it accurately reflects what is being taught in current residency and fellowship programs. Recent fellowship- and residency-trained graduates often use the techniques they learned in training and, therefore, may reflect the current academic orthopaedic community as a whole.
The purpose of this study was to evaluate trends in treatment selection, patient population, and complications in recent ABOS part II examinees of the ABOS board examination. We hypothesized that overall treatment for LHBT pathology would significantly increase over time with a specific increase in tenodesis over tenotomy. To our knowledge, a similar analysis has not been performed to date.
Methods
Once identified in the ABOS database, patients were stratified based on whether they underwent a proximal biceps tendon (PBT) procedure according to the CPT codes submitted with each case. The CPT codes 23405–Tenotomy biceps tendon, 23430–Open tenodesis of long tendon of biceps (LTB), and 29828–Arthroscopic biceps tenodesis were used to represent the patient population. Patients were then organized according to case year in order to evaluate chronological trends in treatment. Statistical analysis was performed using R software Version 3.6.1 (R Foundation for Statistical Computing). We used t tests for unequal variances to compare age and sex in our sample population. To evaluate trends in treatment selection over time, multiple regression analyses were performed. Complications were assessed using chi-square tests with odds ratios calculated for ages ≥50, ≥60, and ≥70 years. In patients who underwent rotator cuff repair (RCR), the repair method (ie, open vs arthroscopic) was also assessed to determine whether there were associated trends in LHBT treatment selection. Regression analysis was used to compare these variables.
Results
Between the years 2008 and 2019, a total of 8611 board-eligible orthopaedic surgeons performed 1,030,853 total cases submitted for the ABOS part II examination. Of those 1,030,853 cases, 17,861 cases consisted of PBT procedures, making up 1.73% of all cases. Further, 78 cases (0.4% of all PBT cases) contained more than one PBT code.
Overall Trends
The annual number of PBT procedures performed significantly increased from 597 cases in 2008 to 2203 cases in 2019 (P < .001). The ratio of PBT cases submitted per number of applicants increased significantly over that same period from 0.89% to 2.78% (P = .009) (Table 1). Additionally, the ratio of PBT procedures per total annual cases submitted increased significantly over the study period (P < .001).
Table 1.
Trends in Total Proximal Biceps Tendon (PBT) Cases by Yeara
| Examination Year | Total No. of Candidates | Total No. of PBT Cases | Ratio of PBT Cases Submitted/No. of Applicants | Ratio of PBT Cases Submitted/Total Annual Cases |
|---|---|---|---|---|
| 2008 | 664 | 597 | 0.89 | 0.68 |
| 2009 | 663 | 783 | 1.18 | 0.91 |
| 2010 | 680 | 1009 | 1.48 | 1.23 |
| 2011 | 662 | 1357 | 2.04 | 1.72 |
| 2012 | 722 | 1202 | 1.66 | 1.35 |
| 2013 | 689 | 1597 | 2.31 | 1.91 |
| 2014 | 770 | 1883 | 2.44 | 2.08 |
| 2015 | 746 | 1780 | 2.38 | 1.97 |
| 2016 | 729 | 1879 | 2.57 | 2.27 |
| 2017 | 743 | 1699 | 2.28 | 1.96 |
| 2018 | 753 | 1902 | 2.52 | 2.19 |
| 2019 | 790 | 2203 | 2.78 | 2.48 |
| Total | 8611 | 17891 | 2.07 | 1.73 |
aOverall, the number of PBT cases submitted increased, as did the ratios of PBT cases submitted per applicant and per number of total cases submitted.
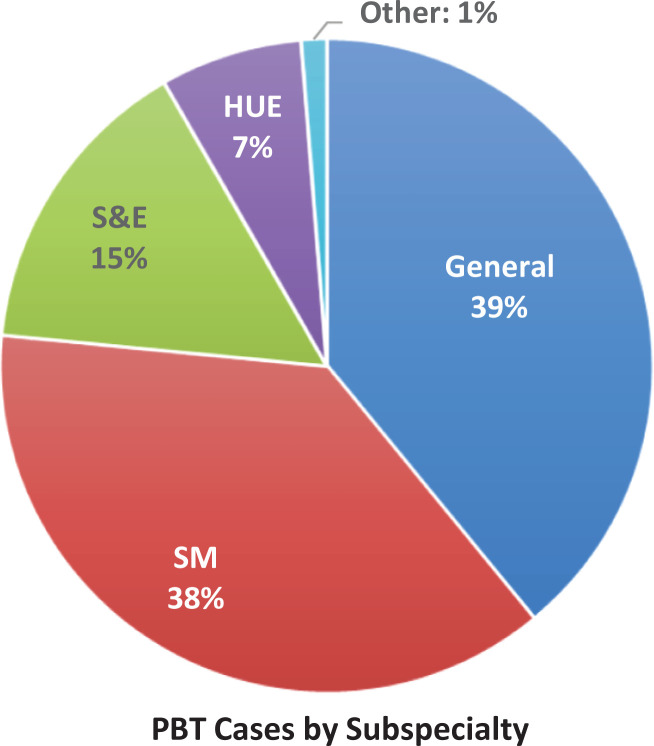
General orthopaedic surgeons performed 6968 (39.01%) PBT cases, sports medicine surgeons performed 6700 (37.51%), shoulder and elbow surgeons performed 2714 (15.19%), and hand and upper extremity surgeons performed 1255 (7.03%). The remaining 224 (1.25%) procedures were performed by surgeons trained in other subspecialties, which are classified as “other” (Figure 1).
Figure 1.
Percentage of proximal biceps tendon (PBT) cases by subspecialty. HUE, hand/upper extremity; Other, all other subspecialties reported; S&E, shoulder/elbow; SM, sports medicine.
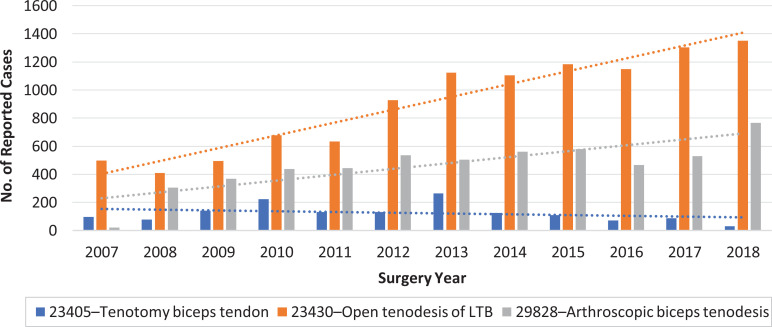
Most PBT cases were performed with another procedure (17,283/17,861; 96.76%). Of the 17,861 total PBT cases submitted, the majority were code 23430–Open tenodesis of LTB (10,894/17861; 61%), followed by code 29828–Arthroscopic biceps tenodesis (5,547/17,861; 31%), and code 23405–Tenotomy biceps tendon (1,498/17,861; 8%). The incidence of code 23405 did not significantly change between the years 2007 and 2018 (P < .001) (Figure 2). The incidence of code 23430 significantly increased between 2007 and 2018 (P < .001). The incidence of code 29828 significantly increased between 2007 and 2018 (P < .001).
Figure 2.
Number of proximal biceps tendon cases performed per year. LTB, long tendon of biceps.
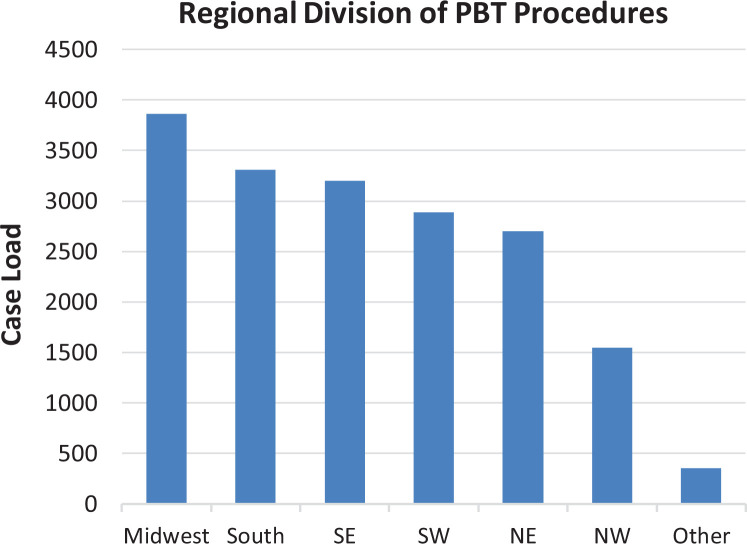
Figure 3 shows the geographic distribution for PBT procedures. The majority of procedures were performed in the Midwest region of the United States (21.63%), followed by the South (18.52%), the Southeast (17.92%), and the Southwest (16.17%). The remaining procedures were performed in all other regions (25.77%).
Figure 3.
Frequency of proximal biceps tendon (PBT) cases broken down by geographical region. NE, Northeast; NW, Northwest; SE, Southeast; SW, Southwest.
Rotator Cuff Repairs
There were 34,796 RCR cases submitted, consisting of codes 23410–Repair of ruptured rotator cuff open: acute; 23410–Repair of ruptured rotator cuff open: chronic; 23420–Reconstruction of complete rotator cuff avulsion: chronic; and 29827–Arthroscopic RCR. Of those 34,796 submitted, 9712 (27.9%) cases were associated with a PBT code. We found that 960 (9.9%) RCR cases were performed with code 23405–Tenotomy biceps tendon, 4865 (50.1%) cases were performed with code 23430–Open tenodesis of LTB, and 3887 (40.0%) cases were performed with code 29828–Arthroscopic biceps tenodesis. Between 2007 and 2018 there was a significant decrease in the total number of RCR codes submitted, from 3530 (10.1%) in 2007 to 2784 (8.0%) in 2018 (P < .001). Across the study period, the percentage of code 23405 cases submitted in conjunction with RCR codes significantly decreased between 2007 and 2018 (P < .001). The number of cases submitted for codes 23430 and 29828 in conjunction with RCR codes significantly increased between 2007 and 2018 (P < .001 for both). The percentage of RCR codes submitted with PBT also significantly increased over the study period between the years 2008 and 2019 (P < .001). When RCR was performed with a PBT code, 23430 was the code most commonly used (∼50%), followed by code 29828 (∼40%) and code 23405 (∼10%).
Overall, the incidence of RCR being performed in conjunction with PBT followed the same trends as PBT alone. Use of code 23430–Open tenodesis of LTB and code 29828–Arthroscopic biceps tenodesis significantly increased over the study period (P < .001), whereas RCR codes submitted with PBT code 23405–Tenotomy biceps tendon significantly decreased over the study period (P < .001).
Demographic Analysis
The majority of patients who underwent a PBT procedure were male (63.85%; n = 11,403), and their mean age was 51.65 ± 12.67 years. Female patients made up 36.15% of all patients (n = 6457) with a mean age of 57.13 ± 12.91 years. A significant difference in age was noted between male and female patients (P < .001). Only 38 (0.21%) cases were performed on pediatric patients (age <18 years).
Subanalysis of each individual code was performed. Code 23405–Tenotomy biceps tendon showed significantly more female than male patients (P = .043) with no difference in age (P = .09). Code 23430–Open tenodesis of LTB, showed significantly more male patients (P < .001) with female patients significantly older than males (P < .001). Code 29828–Arthroscopic biceps tenodesis, showed significantly more male patients (P < .001) with female patients significantly older than their male counterparts (P < .001).
Complications
A total of 3046 complications (3046/17,861; 17.1%) were reported across all procedures, of which 2258 were listed as surgical (2258/3046; 74.1%), 585 were listed as medical (585/3046; 19.2%), and 203 were listed as related to anesthesia (203/3046; 6.7%). There were 173 reoperations (173/17,861; 0.97%) and 227 readmissions (227/17,861; 1.27%).
Of the surgeon-reported surgical complications, the most frequently reported ones were stiffness/arthrofibrosis (n = 416/2258; 18.4%), surgical unspecified (n = 351/2258; 15.5%), pain–recurrent/persistent/uncontrolled (n = 257/2258; 11.4%), failure of tendon/ligament repair (n = 181/2258; 8.0%), nerve palsy/injury (n = 172/2258; 7.6%), and infection (n = 166/2258; 7.4%) (Table 2). The frequency of surgical complication rates for PBT procedures reported each year did not significantly change between the years 2007 and 2018 (7.5% vs 9.7%; P = .103).
Table 2.
Surgeon-Reported Surgical Complications Sorted by Incidence
| Surgical Complications | Incidence |
|---|---|
| Stiffness/arthrofibrosis | 416 |
| Surgical unspecified | 351 |
| Pain--recurrent/persistent/uncontrolled | 257 |
| Failure of tendon/ligament repair | 181 |
| Nerve palsy/injury | 172 |
| Infection | 166 |
| Implant failure | 125 |
| Wound healing delay | 91 |
| Implant failure/fracture/malfunction | 88 |
| Fall | 64 |
| Bone fracture | 58 |
| Tendon/ligament | 54 |
| Skin ulcer | 42 |
| Hematoma | 38 |
| Loss of reduction | 27 |
| Dislocation | 26 |
| Reflex sympathetic dystrophy | 20 |
| Wound dehiscence | 19 |
| Surgical procedure intervention | 18 |
| Nonunion | 13 |
| Implant fracture | 8 |
| Vascular | 7 |
| Hemorrhage | 6 |
| Malunion | 6 |
| Graft problem | 2 |
| Wrong side/site | 2 |
| Spinal cord injury | 1 |
| Total | 2258 |
Increasing patient age significantly increased the risk of complications across the study period. Each decade increase in age past the age of 50 demonstrated an increased risk of complications. When stratified by age, patients ≥50 years had an odds ratio of 1.11 of sustaining a complication (P = .014), patients ≥60 years had an odds ratio of 1.24 of sustaining a complication (P < .001), and patients ≥70 years had an odds ratio of 1.47 of sustaining a complication (P < .001) (Table 3).
Table 3.
Risk of Complication by Age
| Age Group | Odds Ratio for Sustaining Complication | P Value |
|---|---|---|
| ≥50 y | 1.11 | .014 |
| ≥60 y | 1.24 | <.001 |
| ≥70 y | 1.47 | <.001 |
When comparing complication rates between subspecialties, we found that sports medicine surgeons, general orthopaedic surgeons, shoulder/elbow surgeons, and hand/upper extremity surgeons all had lower complication rates than surgeons in other subspecialities (P < .05 for all). Sports medicine surgeons had lower surgical complication rates than hand/upper extremity surgeons and those in other subspecialties (P = .032 and P < .001, respectively). We noted no difference in surgical complication rates between sports medicine surgeons compared with shoulder/elbow surgeons and general orthopaedic surgeons (P = .169 and P = .7586, respectively). General orthopaedic surgeons had lower complication rates than hand/upper extremity surgeons and other subspecialties (P = .048 and P < .001, respectively) but had no difference in complication rates when compared with shoulder/elbow surgeons. Shoulder/elbow surgeons had significantly lower surgical complication rates than surgeons in other subspecialties (P = .002) but demonstrated no difference in complication rates compared with hand/upper extremity surgeons. Hand/upper extremity surgeons had significantly lower complication rates when compared with surgeons in other subspecialties. Complication rates trended inversely with number of procedures performed, with an R 2 correlation of 0.59. This trend was not statistically significant (P = .12) (Table 4).
Table 4.
Total Complications and Complication Rates by Subspecialtya
| Subspecialty | Total No. of Surgical Complications | Total No. of PBT Cases | Complication Rate, % |
|---|---|---|---|
| Sports medicine | 686 | 6700 | 10.20 |
| General orthopaedics | 725 | 6968 | 10.40 |
| Shoulder and elbow | 304 | 2714 | 11.20 |
| Hand/upper extremity | 154 | 1255 | 12.30 |
| All other subspecialties | 41 | 224 | 18.3 |
| Total | 1910 | 17,861 | 10.69 |
aTotals are listed for the entire duration of the study period between 2008 and 2019. PBT, proximal biceps tendon.
When analyzing complication rates for each procedure code, we found significantly higher complication rates listed for code 23430–Open tenodesis of LTB than for codes 23405–Tenotomy biceps tendon and 29828–Arthroscopic biceps tenodesis (P < .001 for both). No difference in complication rates was seen between codes 23405–Tenotomy biceps tendon and 29828–Arthroscopic biceps tenodesis (P = .447).
Discussion
The main findings of this study indicate that (1) PBT tendon procedures are being increasingly performed among recently trained orthopaedic surgeons; (2) the use of biceps tenotomy has significantly declined; (3) both open biceps tenodesis and arthroscopic tenodesis use have significantly increased; (4) most PBT codes are performed in conjunction with another procedure; and (5) although the incidence of PBT codes is significantly increasing, complication rates have remained relatively constant.
Overall, the most common PBT procedure performed was open tenodesis of the LTB followed by arthroscopic biceps tenodesis and tenotomy of the biceps tendon. Furthermore, the overall number of PBT procedures performed significantly increased over the study period, with the average number of PBT cases submitted per applicant more than tripling from 2008 to 2019. The increasing incidence of overall PBT procedures suggests that surgeons are recognizing it more frequently as a source of pathology. Despite the increased use of PBT procedures, complication rates have not significantly increased during that same time.
During the study period, surgeons trended toward the more complex reparative procedures of tenodesis (either open or arthroscopic) over that of tenotomy alone. Even with the increased use of more complex PBT procedures, complication rates did not significantly increase during that same time period. Newly trained surgeons are moving away from isolated tenotomy while favoring biceps tenodesis. Open tenodesis is still the most common procedure performed among all PBT codes; however, the use of arthroscopic techniques has gained considerable popularity.
Recent evidence and reviews have not shown a significant difference in strength and outcomes when comparing tenodesis versus tenotomy; however, there have been reports of higher rates of Popeye deformity after tenotomy.5,9,10,18,19 According to Galdi et al,7 patients have strong preferences for which procedure they undergo. Significant patient concerns are the fear of cosmetic (Popeye) deformities, continued pain, dysfunction in strength or endurance, and recovery time. In that study, the majority of patients chose to undergo biceps tenodesis over tenotomy due to those factors. The main concerns in choosing tenodesis over tenotomy were cosmesis and residual postoperative pain and dysfunction. This suggests that patient preference may have contributed to the higher use of tenodesis in the present study. Interestingly, significantly more female patients underwent tenotomy of the biceps tendon than male patients, which may in part be explained by a lower concern for “muscular appearance” in women compared with men. Regardless, other than an increased complication rate with open tenodesis identified in this review, neither arthroscopic nor open biceps tenodesis has been proven to be superior to the other.8 Surgeon preference or comfort may play a large role in procedure selection.18 Another possible explanation that cannot be proven from this data set is the contribution of reimbursement rates for the surgeons themselves. Both arthroscopic and open biceps tenodesis procedure codes reimburse at a higher level than biceps tenotomy, which may factor into the decision-making process for the surgeon. Furthermore, relationships that surgeons may have with companies that manufacture tenodesis screws and suture anchors may affect the trends seen in this review.
RCR codes continue to have a high association with PBT codes. Of all the RCR codes submitted, approximately 28% were submitted with a PBT code. Isolated treatment for PBT pathology followed the same pattern when performed with RCR codes. Rates of tenodesis, open or arthroscopic, increased over the study period while tenotomy alone decreased. Similar results have been shown when tenodesis and tenotomy were compared in conjunction with RCR.14
The overall complication rate for PBT procedures approached 17.1%; however, these complications appear to be minor in that only 0.97% required reoperation and 1.27% required readmission. Overall, complication rates were closely related to the number of procedures performed by the subspecialty. General orthopaedic and sports medicine surgeons had the lowest complication rates (10.4% and 10.2%, respectively) while performing the most procedures (6968 and 6700 cases, respectively), whereas surgeons in the “Other” category performed the fewest PBT procedures throughout the study period (224 cases) and had the highest complication rate (18.3%). This trend suggests that experience and number of PBT procedures performed may correlate with decreased complication rates. However, it should be noted that the high number of associated procedures performed makes it difficult to identify which complications were truly biceps related and which may have resulted from other procedures.
The limitations of this study should be noted.4,17 This data set comprises only new graduates of orthopaedic surgery residencies and may not reflect the overall orthopaedic community. Data derived from the surgeries performed, clinical outcomes, and complications may reflect the relative inexperience of the surgeons. Second, because this is a retrospective review, data are dependent on accurate recording from the study participants. Data may also be subject to bias because of the nature of the data collection. The surgeons contributing to this data set know they are in, what is referred to as, their “collection period.” This may have significant effects on their surgical choices, which patients they treat, and which patients undergo which operative procedure. Likewise, complications are listed only for the 6-month “collection period” and may not capture overall complication rates outside of that time period.
Conclusion
PBT procedures are being increasingly performed among recently trained orthopaedic surgeons. Proximal biceps tenotomy has significantly declined, whereas proximal biceps tenodesis, open or arthroscopic, has significantly increased, demonstrating a possible shift in the standard of care among new surgeons.
Footnotes
Final revision submitted June 23, 2020; accepted July 6, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: S.D.J. has received educational support from Gemini Mountain Medical. S.G.T. has received educational support from Quest Medical. R.M.F. has received grant support from Arthrex, educational support from Arthrex/Medwest and Smith & Nephew, speaking fees from Arthrex, and royalties from Elsevier. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Ahmad CS, DiSipio C, Lester J, Gardner TR, Levine WN, Bigliani LU. Factors affecting dropped biceps deformity after tenotomy of the long head of the biceps tendon. Arthroscopy. 2007;23(5):537–541. [DOI] [PubMed] [Google Scholar]
- 2. Boileau P, Baque F, Valerio L, Ahrens PM, Chuinard C, Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89(4):747–757. [DOI] [PubMed] [Google Scholar]
- 3. Franceschi F, Longo UG, Ruzzini L, Papalia R, Rizzello G, Denaro V. To detach the long head of the biceps tendon after tenodesis or not: outcome analysis at the 4-year follow-up of two different techniques. Int Orthop. 2007;31(4):537–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Frank RM, Cotter EJ, Hannon CP, Harrast JJ, Cole BJ. Cartilage restoration surgery: incidence rates, complications, and trends as reported by the American Board of Orthopaedic Surgery part II candidates. Arthroscopy. 2019;35(1):171–178. [DOI] [PubMed] [Google Scholar]
- 5. Friedman JL, FitzPatrick JL, Rylander LS, Bennett C, Vidal AF, McCarty EC. Biceps tenotomy versus tenodesis in active patients younger than 55 years: is there a difference in strength and outcomes? Orthop J Sports Med. 2015;3(2):2325967115570848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Frost A, Zafar MS, Maffulli N. Tenotomy versus tenodesis in the management of pathologic lesions of the tendon of the long head of the biceps brachii. Am J Sports Med. 2009;37(4):828–833. [DOI] [PubMed] [Google Scholar]
- 7. Galdi B, Southren DL, Brabston EW, et al. Patients have strong preferences and perceptions for biceps tenotomy versus tenodesis. Arthroscopy. 2016;32(12):2444–2450. [DOI] [PubMed] [Google Scholar]
- 8. Gombera MM, Kahlenberg CA, Nair R, Saltzman MD, Terry MA. All-arthroscopic suprapectoral versus open subpectoral tenodesis of the long head of the biceps brachii. Am J Sports Med. 2015;43(5):1077–1083. [DOI] [PubMed] [Google Scholar]
- 9. Hassan S, Patel V. Biceps tenodesis versus biceps tenotomy for biceps tendinitis without rotator cuff tears. J Clin Orthop Trauma. 2019;10(2):248–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hufeland M, Wicke S, Verde PE, Krauspe R, Patzer T. Biceps tenodesis versus tenotomy in isolated LHB lesions: a prospective randomized clinical trial. Arch Orthop Trauma Surg. 2019;139(7):961–970. [DOI] [PubMed] [Google Scholar]
- 11. Koh KH, Ahn JH, Kim SM, Yoo JC. Treatment of biceps tendon lesions in the setting of rotator cuff tears. Am J Sports Med. 2010;38(8):1584–1590. [DOI] [PubMed] [Google Scholar]
- 12. Lam F, Mok D. Treatment of the painful biceps tendon—tenotomy or tenodesis? Curr Orthop. 2006;20(10):370–375. [Google Scholar]
- 13. Mazzocca AD, Rios CG, Romeo AA, Arciero RA. Subpectoral biceps tenodesis with interference screw fixation. Arthroscopy. 2005;21(7):896. [DOI] [PubMed] [Google Scholar]
- 14. Meraner D, Sternberg C, Vega J, Hahne J, Kleine M, Leuzinger J. Arthroscopic tenodesis versus tenotomy of the long head of biceps tendon in simultaneous rotator cuff repair. Arch Orthop Trauma Surg. 2016;136(1):101–106. [DOI] [PubMed] [Google Scholar]
- 15. Murthi AM, Vosburgh CL, Neviaser TJ. The incidence of pathologic changes of the long head of the biceps tendon. J Shoulder Elbow Surg. 2000;9(5):382–385. [DOI] [PubMed] [Google Scholar]
- 16. Osbahr DC, Diamond AB, Speer KP. The cosmetic appearance of the biceps muscle after long-head tenotomy versus tenodesis. Arthroscopy. 2002;18(5):483–487. [DOI] [PubMed] [Google Scholar]
- 17. Parker BR, Hurwitz S, Spang J, Creighton R, Kamath G. Surgical trends in the treatment of meniscal tears: analysis of data from the American Board of Orthopaedic Surgery certification examination database. Am J Sports Med. 2016;44(7):1717–1723. [DOI] [PubMed] [Google Scholar]
- 18. Patel KV, Bravman J, Vidal A, Chrisman A, McCarty E. Biceps tenotomy versus tenodesis. Clin Sports Med. 2016;35(1):93–111. [DOI] [PubMed] [Google Scholar]
- 19. Ribeiro FR, Ursolino APS, Ramos VFL, Takesian FH, Tenor AC, Jr, Costa MPD. Disorders of the long head of the biceps: tenotomy tenodesis. Rev Bras Ortop. 2017;52(3):291–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Richards DP, Burkhart SS. A biomechanical analysis of two biceps tenodesis fixation techniques. Arthroscopy. 2005;21:861–866. [DOI] [PubMed] [Google Scholar]
- 21. Shang X, Chen J, Chen S. A meta-analysis comparing tenotomy and tenodesis for treating rotator cuff tears combined with long head of the biceps tendon lesions. PloS One. 2017;12(10): e0185788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wolf RS, Zheng N, Weichel D. Long head biceps tenotomy versus tenodesis: a cadaveric biomechanical analysis. Arthroscopy. 2005;21:182–185. [DOI] [PubMed] [Google Scholar]