A 62-year-old woman was evaluated for worsening dyspnoea. She had previously undergone coronary artery bypass surgery and had a history of a chronic loculated left pleural effusion (PE), which had previously been treated with repeated thoracentesis and talc pleurodesis. An echocardiogram was obtained, which was of suboptimal image quality, but it did demonstrate a small left ventricular (LV) chamber and normal LV ejection fraction. Pulsed wave Doppler of mitral valve inflow revealed significant respirophasic changes of the E-wave velocity (>25%), a short deceleration time (<160 ms), and an ‘L’ wave. There was also apparent ventricular interaction. Together these findings raised suspicion for constrictive pericarditis (CP), with the thought being that this condition resulted in dyspnoea due to impaired LV compliance, elevated filling pressures, and an inability to augment stroke volume with exertion.
Cardiac magnetic resonance (CMR) imaging was performed to evaluate the possibility of CP. Cine CMR was performed at a 1.5-Tesla MR scanner using an electrocardiogram gated steady-state free precession pulse sequence. As shown in a short-axis orientation of the heart, there is dyssynchronous contraction of the LV posterior wall but normal wall thickening (Videos 1–3). During systole, there is pronounced posterior motion of the LV posterior wall followed by flattening and compression of the same wall during diastole (Figures 1 and 2 and Supplementary material online, Figure S1). This phenomenon has been described in two-dimensional echocardiography as pseudodyskinesis and is commonly associated with liver or parenchymal lung disease.1
Figure 1.
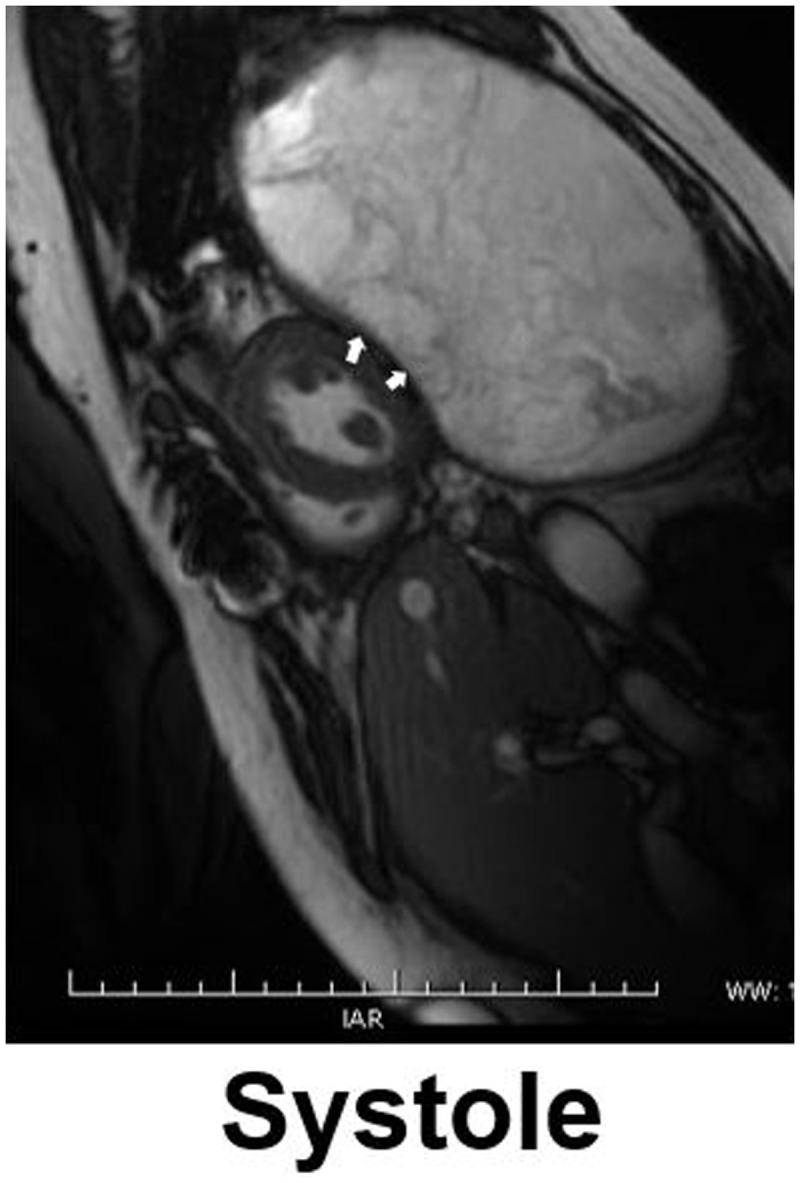
Cardiac magnetic resonance systolic frame showing normal wall thickening and protrusion of the posterior wall of the left ventricular towards a large left pleural effusion (see white arrows).
Figure 2.
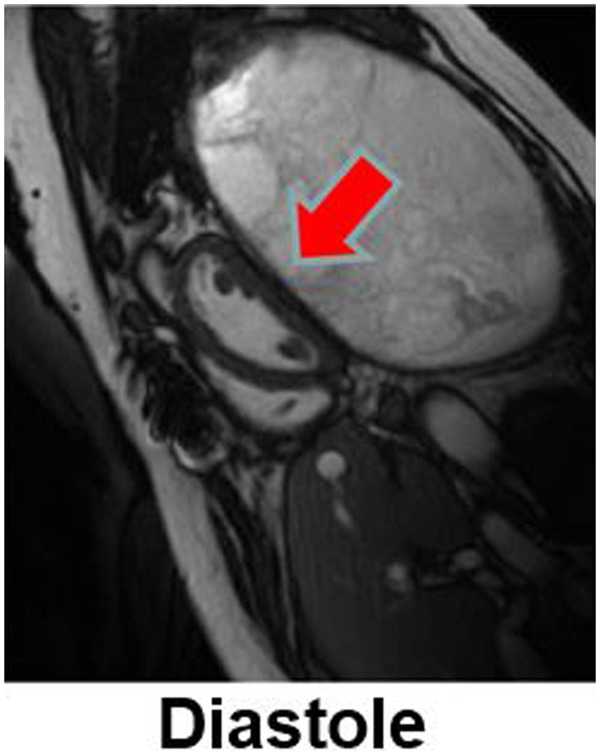
Cardiac magnetic resonance diastolic frame showing flattening and compression of the posterior wall of the left ventricular due to increased pleural pressures secondary to the loculated effusion (see red arrow).
The abnormal systolic motion of the posterior wall has previously been attributed to diaphragmatic elevation resulting from intrathoracic or intrabdominal pathology. Pleural effusions, likewise, can have a significant impact on cardiac haemodynamics. A study of 47 subjects with large PE by Wang et al.2 demonstrated that drainage of the PE resulted in significant increases in LV end-diastolic volume index, LV ejection fraction, and stroke volume. In rare instances, large left-sided PEs have even been shown to result in cardiac tamponade.3
In our case, we hypothesize that the patient’s left-sided PE is causing compression of the LV posterior wall in diastole impairing LV filling and reducing preload; in systole, the process is reversed by the higher intracardiac pressure (Supplementary material online, Figure S2). The patient was taken to the operating room and underwent a left thoracotomy and decortication for a large haemothorax and treatment of suspected‘trapped lung’ syndrome. The patient’s dyspnoea resolved status-post-thoracotomy and decortication.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Consent: The authors confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
Contributor Information
Matthew Gottbrecht, Division of Cardiovascular Medicine, Department of Medicine and Radiology, University of Massachusetts Medical School, ACC 4-240, 55 Lake Avenue North, Worcester, MA 01655, USA.
Waqas Qureshi, Division of Cardiovascular Medicine, Department of Medicine and Radiology, University of Massachusetts Medical School, ACC 4-240, 55 Lake Avenue North, Worcester, MA 01655, USA.
Theo E Meyer, Division of Cardiovascular Medicine, Department of Medicine and Radiology, University of Massachusetts Medical School, ACC 4-240, 55 Lake Avenue North, Worcester, MA 01655, USA.
Gerard P Aurigemma, Division of Cardiovascular Medicine, Department of Medicine and Radiology, University of Massachusetts Medical School, ACC 4-240, 55 Lake Avenue North, Worcester, MA 01655, USA.
References
- 1. Raisinghani A, Mahmud E, Sadeghi M, Peters B, Strachan GM, Huynh T. et al. Paradoxical inferior-posterior wall systolic expansion in patients with end-stage liver disease. Am J Cardiol 2002;89:626–629. [DOI] [PubMed] [Google Scholar]
- 2. Wang Z, Cai Q, Ban C, Chen D, Xu L, Wang X. et al. Improved heart hemodynamics after draining large-volume pleural effusion: a prospective cohort study. BMC Pulm Med 2018;18:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kopterides P, Lignos M, Papanikolaou S, Papadomichelakis E, Mentzelopoulos S, Armaganidis A. et al Pleural effusion causing cardiac tamponade: report of two cases and review of the literature. Heart Lung 2006;35:66–67. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


