Description
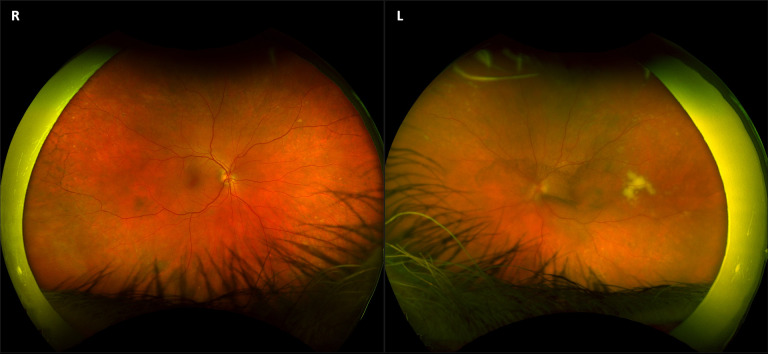
A 66-year-old man presented with a 1-month history of hazy vision in his left eye, worsening over the past 2 days. His medical history included hypothyroidism and hypertension. Best-corrected Snellen visual acuity was 6/9 and hand movements in the right and left eyes, respectively, with no evidence of relative afferent pupillary defect. Dilated slit-lamp examination showed normal anterior segments with intraocular pressures of 14 mm Hg bilaterally. Dilated funduscopy revealed a left central vitritis (binocular indirect ophthalmoscopy score of 1). There was a left epiretinal membrane without macular oedema, optic nerve abnormality or stigmata of retinal vasculitis. There was a creamy white subretinal pigment epithelial (sub-RPE) lesion temporal to the left macula measuring 4 disc diameters in area (figure 1). Of note, the patient had been diagnosed with cerebellar primary central nervous system (CNS) lymphoma (PCNSL) 2 years previously, with completion of primary chemotherapy (cytarabine, rituximab, methotrexate, procarbazine and vincristine) 4 months previously. In light of this history, posterior uveitis secondary to PCNSL, termed primary vitreoretinal lymphoma (PVRL), was considered the main differential diagnosis. Widefield colour photography (Optos California, Optos plc, Scotland, figure 1) and spectral domain optical coherence tomography (OCT, Cirrus 5000, Carl Zeiss Meditec, Dublin, California, USA, figure 2) were performed to clarify the clinical picture.
Figure 1.
Widefield colour photographs of the right and left eyes showing a normal fundus for age on right (R), and central vitritis with white subretinal lesion temporal to the macula on the left (L).
Figure 2.
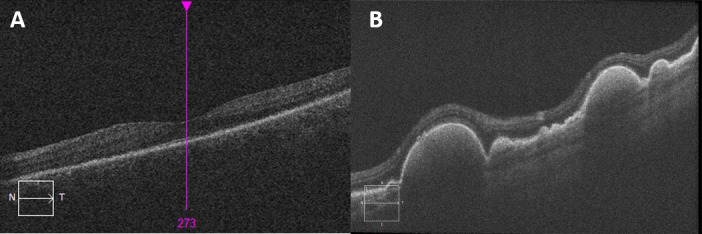
(A) Left macular OCT image showing normal foveal morphology. (B) High-resolution OCT image through the lesions temporal to the left macula confirming their subretinal pigment epithelial location. OCT, optical coherence tomography.
In order to precisely ascertain the plane and location of the lesions, a high-resolution OCT of the left eye was performed, reaffirming a sub-RPE plane (figure 2). In light of the previous diagnosis of PCNSL and lack of other historical red flags for posterior uveitis, a tissue biopsy was not performed as the risk to vision, such as retinal detachment and tumour seeding, was deemed higher than the diagnostic benefit.
While PVRL is an exceedingly rare malignancy, its exact incidence remains elusive.1 Ocular involvement in cases of established PCNSL is even rarer, hovering around merely 1% of all intraocular tumours.2 When PVRL does present, it masquerades as posterior uveitis, often obscuring the prompt and early diagnosis and thus presenting an onerous challenge for the clinicians.3 Since it usually presents as vitritis, treatment with steroids serves to mask the symptoms, rendering the diagnosis of PVRL even more difficult.3 In elderly patients with insidious-onset posterior uveitis with or without a pre-existing diagnosis of PCNSL, PVRL should be considered among the differential diagnoses, and multimodal imaging may help to locate an occult subretinal or sub-RPE deposit, further expediting the diagnosis in such instances.4 Treatment options for monocular disease without CNS lesions include intravitreal methotrexate/rituximab and orbital radiotherapy.5 Similarly, low-beam stereotactic radiotherapy has been recommended for localised remission of ocular symptoms.6 In contrast, CNS involvement necessitates systemic chemotherapy, including high-dose methotrexate.5 Combination systemic therapy with rituximab and methotrexate has been shown to yield a 94%–100% remission rate.7 In our case, the patient was referred to the primary oncology team for consideration of orbital radiotherapy. Nevertheless, the decision of whether to commence intravitreal chemotherapy or localised radiotherapy as the first-line treatment remains at the epicentre of a management dilemma.
Learning points.
In elderly patients with or without a history of primary central nervous system lymphoma and gradual-onset visual loss with signs of posterior uveitis, primary vitreoretinal lymphoma (PVRL) should be considered in the differential diagnosis with subretinal infiltrates (seen in 20%) as a pathognomonic finding.
Steroid therapy may mask the symptoms of PVRL, and a high index of suspicion for PVRL must be maintained in older patients.
Approximately 65%–90% of PVRL cases are associated with asymptomatic CNS lesions;, neuroimaging is therefore recommended for all PVRL cases.
Acknowledgments
The authors would like to thank the Photographic Department, Royal Victoria Eye and Ear Hospital, Dublin, Ireland.
Footnotes
Contributors: KAJS and CCM diagnosed the patient. TA and KAJS wrote the manuscript. All authors revised and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Sagoo MS, Mehta H, Swampillai AJ, et al. . Primary intraocular lymphoma. Surv Ophthalmol 2014;59:503–16. 10.1016/j.survophthal.2013.12.001 [DOI] [PubMed] [Google Scholar]
- 2.Bardenstein DS. Intraocular lymphoma. Cancer Control 1998;5:317–25. 10.1177/107327489800500403 [DOI] [PubMed] [Google Scholar]
- 3.Chan C-C, Rubenstein JL, Coupland SE, et al. . Primary vitreoretinal lymphoma: a report from an international primary central nervous system lymphoma Collaborative group symposium. Oncologist 2011;16:1589–99. 10.1634/theoncologist.2011-0210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davis JL. Intraocular lymphoma: a clinical perspective. Eye 2013;27:153–62. 10.1038/eye.2012.250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou M, Xu G. Recent progress in the diagnosis and treatment of primary vitreoretinal lymphoma. Taiwan J Ophthalmol 2016;6:170–6. 10.1016/j.tjo.2016.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berenbom A, Davila RM, Lin H-S, et al. . Treatment outcomes for primary intraocular lymphoma: implications for external beam radiotherapy. Eye 2007;21:1198–201. 10.1038/sj.eye.6702437 [DOI] [PubMed] [Google Scholar]
- 7.Chan C-C, Sen HN. Current concepts in diagnosing and managing primary vitreoretinal (intraocular) lymphoma. Discov Med 2013;15:93–100. [PMC free article] [PubMed] [Google Scholar]