Summary box.
Malaria remains a significant public health problem in India as it contributes >85% of estimated cases in South East Asia and almost half of all Plasmodium vivax cases globally.
There is a multiplicity of malaria stakeholders in India that include public sector agencies, private healthcare providers, defence forces, railways, industry, independent researchers and control programmes that at times operate in silos and this leads to fragmented data inputs and interpretation.
Lack of an established near real-time case-based surveillance system further challenges the ability to mount a cohesive and integrated malaria elimination agenda.
There is an urgent need to reformulate the boundaries of individual stakeholders and initiate a system that will allow them to coalesce data into a digital integrated platform.
Such a platform will provide near real-time epidemiological, entomological and commodity surveillance data that will be of immediate use to all stakeholders and will allow transparent and evidence-based formulation of malaria control policies.
Despite a substantial decline in global burden of malaria, it remains one of the most significant public health problems in Africa and South Asia. Malaria incidence has declined globally between 2010 and 2018 from 71 to 57 cases per 1000 population at risk but the pace of reduction has slowed between 2014 to 2018. An estimated ~228 million cases of malaria occurred worldwide in 2018 with WHO South East Asia region contributing 3.4% of the burden. Almost 85% of all malaria cases globally were borne by 18 African countries and by India, that additionally accounts for nearly half (47%) of all Plasmodium vivax cases globally.1
As malaria endemic countries shift their goal post from limiting morbidity and mortality (malaria control) to zero-incidence of indigenous case (malaria elimination) it becomes imperative that approaches and strategies also evolve in concert. There is thus clearly a need for the malaria health information system to switch from use of aggregated data to near real-time case-based surveillance.2 The malaria data collected via surveillance systems under national programmes is de facto the basis for country’s policies, strategies and operational activities. Incomplete data or data that are primarily used for reporting purposes, typically as in the routine national surveillance programmes, can only prolong malaria transmission owing to its inherent limitations for use in malaria control efforts, especially in underserved areas.3
In India, the National Vector Borne Disease Control Programme under the Ministry of Health and Family Welfare is a vertically implemented programme. India launched National Framework of Malaria Elimination in 2016 with the overall goal of zero indigenous cases in the country by 2030.
However, the robustness of the current Indian surveillance system is a matter of debate. There is a wide discrepancy between the reported cases and deaths by national programme of India and estimated cases by WHO and various research studies.4–6 In 2017, National Programme reported 0.84 million cases and 194 deaths whereas WHO estimated 9.6 million cases and 16.7K deaths during the same year.7 8 Another example of the discordance in numbers is the surveillance-based estimation of malaria burden that was completed by a nodal research body in India in 2015/2016 that estimated malaria incidence to be fourfold greater than the 1 million reported by the national programme, but threefold lesser than the 13 million estimated by the WHO. Similarly, the estimated deaths were 93-folds more than average 313 deaths reported by the national malaria programme in 2015/2016 but were comparable with that estimated by the WHO for India.6India State-Level Disease Burden Initiative 1990 to 2016 as part of Global Burden of Disease study estimated malaria to be responsible for 0.47% of total disability-adjusted life-years (0.19% to 1.08%) and 0.8% of deaths in all age groups caused by neglected tropical diseases and malaria.9
There could be multiple reasons for the above disagreement in numbers. The existing Indian surveillance system indeed has a time-lag in reporting due to paper-based data. It suffers from poor surveillance of the substantial mobile populations, forest workers, transitory urban slum populations, refugees and domestic or international tourists. In addition, it is inefficient at representing data from remote and inaccessible areas such as tribal and hilly regions.
The marginalised section of communities afflicted by malaria, suffer not only from neglect but also helplessness and dearth of healthcare opportunities. These communities need enabling environment and empowerment so as to enhance their reach out to the healthcare system and timely prevention and management. Persistent neglect and lack of focus on malaria in pregnancy has led it to become a hidden public health problem.10 Importantly, malaria cases treated by private healthcare providers, both qualified and unqualified, who otherwise impart approximately 70% of healthcare through hospitals, nursing homes, clinics or general practice are not accounted for in national figures.11 Moreover, armed forces, railways and organised industries like automobiles, coal, mines, steel, tea plantations and others with their own healthcare systems are missing from the numbers projected by national surveillance systems. In addition to the above missing links, the data which is routinely collected in the ambit of national programme lacks real-time data aggregation and is bereft of desirable level of resolution such as households. Finally, no extrapolation across geographical borders of Indian states is currently possible either within India or outside. Adjacent districts that belong to different states suffer from widely variable malaria incidence rates but lack of timely data sharing makes each side vulnerable to interstate import and export of malaria.
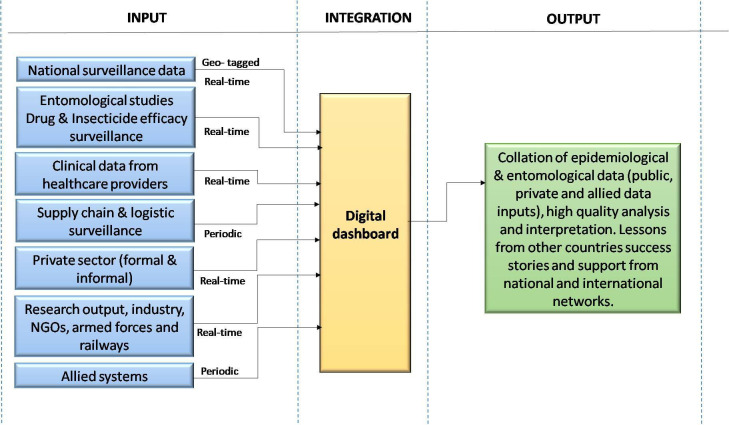
Further, the malaria incidence data from national programme are not available in the public domain in terms of granularity that is below the district level. The data are also not provided age, gender and month-wise thereby discouraging their analyses. These constraints also prevent both the identification of infection foci and timely adoption of corrective actions. Adding to the void, drug and insecticide efficacy surveillance, entomological surveillance, commodity and stock management are not part of the surveillance systems. Thus, though available in separate domains, the data are scattered and disintegrated. (figure 1)
Figure 1.
Malaria data integration. NGOs, non-governmental organisations.
Furthermore, India, the second most populous country, has a substantial proportion of researchers, scientists, doctors, non-government bodies, philanthropic organisations and many other independent bodies who work in the field of malaria. Besides reading the work in scientific literature, there is no centralised database in the country for the active researchers and malariologists to connect with each other, missing out on the opportunity of scientific deliberations, cross-fertilisation of research ideas and possible collaborations. Relying on meetings, workshops and lectures as a platform for efficient data exchange will continue to foster malaria control operations but in silos.
Lack of a one-window platform that can provide integrated malaria data presents real roadblocks towards enhancing our understanding of the dynamic situation of malaria in India. Several notable instances where integration can help are; (a) high quality data analysis and interpretation of the routine epidemiological and entomological information gathered at national and local levels can direct any midcourse corrections for implementation. This will need integration with data analysts and epidemiologists; and (b) collation and analysis of data generated by multiple agencies (like private sector, armed forces, industry, etc) and stakeholders (eg, non-governmental organisations working in states) at one platform. This would need to be preceded by data validation and standardisation of inputs from different sources.
Extensive training of and by the malaria programme managers and other players will be essential for the proposed platform to provide harmonised, robust, standardised, uniform and validated data. As much as possible, raw data can be made accessible at the platform so as to enable offline analyses of the same. Once malaria is made a notifiable disease, these partners would be mandated to share the real-time data. This will allow comprehensive and cohesive analyses on which subsequent evidence-based action can be based; (c) conglomeration of active researchers and malariologists and (d) lessons from other countries that have successfully eliminated malaria and from those struggling yet.
Internationally, there are examples of networks where researchers and clinical investigators are encouraged to share and access data through secure online systems. Examples are ‘The WorldWide Antimalarial Resistance Network’ (WWARN) that is part of the Infectious Diseases Data Observatory and is a collaborative platform to track the emergence and spread of malaria drug resistance.12 The Worldwide Insecticide Resistance Network (WIN) runs in a similar format.13
To meet the above exigencies of multiple, siloed and independent stakeholders we propose that consideration should be given to ‘convergence’ of data pertaining to malaria as a structural change to the way programmes are run currently. This convergence or data integration will absorb all data from independent agencies mentioned in figure 1 and aim to coalesce it on a digital platform. The integrated data will provide a single window digital platform that is lucid, inclusive, transparent, open access and multilayered. The digital platform can be a data hub for rendering valuable data as per the needs of the individual stakeholders. Some possible benefits are:
-
The digital platform can serve as a robust surveillance system wherein comprehensive, near real-time, patient-based data collected at all levels, by public and private sectors, on important epidemiological parameters such as demographic information including location, diagnosis and treatment, vector control interventions and monitoring of drug and insecticide resistance and supply chain logistics are reflected. Data capture at the level of villages or households will also translate into immediate data-driven control action and therefore mitigation of malaria.
The proposed digital platform will thus provide a window for ‘local data for local action’. ‘Minimum data sets’ could be defined denoting the least possible number of data points for standardisation and interoperability which could be useful to a range of stakeholders14 data analysis and timely interpretations will facilitate identification of potential hotspot of malaria and impending outbreaks. Feedback mechanisms with in-built alert systems and decision support systems from the central to peripheral levels of the health system and back would assist in efficiently containing new foci of disease. Effective and timely response from health system as result of the alerts would inform the digital information system that the activity has taken place operating as a tool for monitoring and evaluation.15 Cloud-based database or local databases can be selected depending on internet availability ensuring seamless reporting adhering to the pre-decided timelines.
Data on drug and insecticide resistance, parasite and vector behaviours, standard protocols in malaria elimination research, geospatial mapping, vector ecology, high-risk group mapping, novel tools like newer diagnostics or vector control tools, drug treatment trials would be valuable part of dashboard.
Data sources external to health systems, for example, census data providing population denominators, climate data, land use data and water bodies data can be also be made accessible. Migratory populations can be mapped for easy surveillance by using mobile phone technology or geo-tagged devices. These together directly or indirectly impact disease epidemiology and their merging could provide a panoramic view of vector borne diseases like malaria.
The digital platform will serve as a database of and for malariologists. It can include national and international consortia from different disciplines of malaria and allied fields. This would be an excellent opportunity for researchers and scholars to develop networks and share knowledge and resources. However, to assemble and accredit the data integration digital platform with all the above attributes and features, India needs to have seamless internet facility, provision for offline data entry, data server and safety firewalls for data security. It will need adequate governance and policy structures to ensure data privacy. Although a single window data platform can offer consolidation of vital data, resistance to it is a possible barrier.
Hindrances such as: (a) ‘policy obstacles’ on data sharing and data security3 especially in the context of cross-border (international) data sharing. To the neighbouring countries of Bhutan, Nepal, Bangladesh (bordering north-eastern region of India) and Sri Lanka import of malaria from India is a threat. However, transparent data sharing on malaria cases, drug/insecticide resistance and intervention tools though desirable may be stalled by bureaucratic inaction. Unfriendly political relationships between countries alongwith biosecurity concerns may also hamper smooth exchange of the data. A possible solution is to develop nationwide digital platforms with safeguard mechanisms like conditional ‘writing access’ limited authorised partners but with wide and free access and availability of data. This digital platform can be shared with neighbouring malarious countries for adoption so as to standardise data representation and also to facilitate exchange of vital information, if the countries so decide. Indian Council of Medical Research’s (ICMR) initiative of bringing all malariologists and researchers at one platform via Malaria Elimination Research Alliance-India (MERA-India) is a step towards integration of elimination research efforts. MERA-India, steered by National Institute of Malaria Research, is aptly placed to play this important role of international collaborations. MERA-India is being led by Secretary (Department of Health Research) and Director General, ICMR, the nodal research body of Indian government and supported by Ministry of Health and Family Welfare and WHO-SEARO. MERA-India is governed by independent experts and is a body with minimum bureaucracy involved. ICMR’s initiative ‘Regional Research Platform’, though focussed on emerging infectious diseases in its launch year (2019) can also be harnessed to link neighbouring South East Asian countries and support MERA-India in this proposed endeavour. (b) International donor agencies support malaria control and elimination programmes in developing countries like India. There may be a perceived risk that donor agencies may use the integrated data to assess and financially audit the performance of the national malaria control programme. This may worsen the hesitancy of the governments to fully adopt the digital platforms in lieu of fear of losing on the funding opportunities. However, such transparency will also provide new fillip to the national programme in terms of greater accountability. (c) In India’s federal system, health is a state subject and thus India’s states may be reluctant to share in near real-time the data on hotspots/outbreaks, supply chain inefficiencies and/or poor surveillance. However, the very purpose of this proposed digital dashboard is to bring to light national and state level data as this will provide an opportunity for greater accountability in the running of malaria programmes. (d) The possibility of stigmatisation and ostracisation of the areas identified as hotspots and/or outbreak prone due to the proposed digital solution. However, as COVID-19 pandemic has taught us already, the best policy for the government and public health officials in context of infectious diseases is utter transparency and sharing of data that the digital platform will enable.
Data integration is necessary but is just one of the component of the overall thrust for malaria elimination. There are several other notable gaps in the implementation of the current national programme which may be plugged concurrently. Given its size and complexity, India has adopted a subnational elimination plan (recommended by WHO) wherein a particular district or state is encouraged to achieve and maintain malaria-free status, even though transmission is likely to continue in other parts of the country for few more years. Financial and other awards have been announced by Indian government to give impetus to subnational malaria elimination and enthuse local health systems and public health administration.
As we become cognizant of the ascendancy, barriers, limitations and scope of the proposed digital data integration platform, we recognise the need for research in operationalisation of this concept. Methods and mechanisms need to be devised, tested and validated for each step before we embark on implementation and actual use of this digital dashboard. An example of existing dashboard is District Health Information Software-2 (DHIS 2) though it has its own constraints. Countries may develop their own tailor-made dashboards with their needs fitting in the context of their health ecosystems. In India, we feel that the ICMR can champion this cause of data integration platform. Via National Institute of Malaria Research (NIMR) and the national programme, this integration will aid in the malaria elimination ambition of the country. There is indeed a growing voice in national and international communities for integrating surveillance and control programmes that target communicable diseases. This is therefore vital and will allow optimisation of resources and enhancement of outputs.
COVID-19, despite its paralysing effect on the world, has mobilised one and all to share real-time data of daily cases and deaths. COVID-19 epidemiology is available on many dashboards even within India and its states (the state of Kerala has an exceptionally informative COVID-19 dashboard). The digital tracking of COVID-19 has empowered both public health specialists and the general population. This sets up a good precedent for malaria.16
As we move towards malaria elimination disruptive strategies are needed to challenge the conventional boundaries of health and allied systems. The time is opportune to dwell on remodelling our data collection methods, innovate on data collation and analysis and to freely share malaria data that is generated using public funds.4
Acknowledgments
We thank Department of Science and Technology (DST) for the JC Bose fellowship to AS.
Footnotes
Handling editor: Seye Abimbola
Contributors: AS and MR contributed equally.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Disclaimer: The views expressed in the submitted article are our own and not an official position of the institution or funder.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: There are no data in this work.
References
- 1.World malaria report 2019, Geneva. Available: https://www.who.int/publications-detail/world-malaria-report-2019 [Accessed 29 Sep 2020].
- 2.Malaria surveillance, monitoring & evaluation: a reference manual. World Health Organization. Available: https://www.who.int/docs/default-source/documents/publications/gmp/malaria-surveillance-monitoring-and-evaluation---a-reference-manual.pdf?sfvrsn=46489b3b_2 [Accessed 7 Nov 2020].
- 3.Feachem RGA, Chen I, Akbari O, et al. Malaria eradication within a generation: ambitious, achievable, and necessary. Lancet 2019;394:1056–112. 10.1016/S0140-6736(19)31139-0 [DOI] [PubMed] [Google Scholar]
- 4.Kumar A, Valecha N, Jain T, et al. Burden of malaria in India: retrospective and prospective view. Am J Trop Med Hyg 2007;77:69–78. 10.4269/ajtmh.2007.77.69 [DOI] [PubMed] [Google Scholar]
- 5.Das A, Anvikar AR, Cator LJ, et al. Malaria in India: the center for the study of complex malaria in India. Acta Trop 2012;121:267–73. 10.1016/j.actatropica.2011.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar A, Chaturvedi HK, Mohanty AK, et al. Surveillance based estimation of burden of malaria in India, 2015-2016. Malar J 2020;19:156. 10.1186/s12936-020-03223-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Malaria situation in India from 2016 National vector borne disease control programme. Available: https://nvbdcp.gov.in/WriteReadData/l892s/4763116151601880632.pdf [Accessed 7 Oct 2020].
- 8.Malaria country profile India, 2017. Available: https://www.who.int/malaria/publications/country-profiles/profile_ind_en.pdf?ua=1 [Accessed 7 Oct 2020].
- 9.India State-Level Disease Burden Initiative Collaborators Nations within a nation: variations in epidemiological transition across the states of India, 1990-2016 in the global burden of disease study. Lancet 2017;390:2437–60. 10.1016/S0140-6736(17)32804-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma VP. Hidden burden of malaria in Indian women. Malar J 2009;8:281. 10.1186/1475-2875-8-281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Balsari S, Fortenko A, Blaya JA, et al. Reimagining health data exchange: an application programming Interface-Enabled roadmap for India. J Med Internet Res 2018;20:e10725. 10.2196/10725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Worldwide Antimalarial Resistance Network’ (WWARN), 2020. Available: https://www.wwarn.org/ [Accessed 6 Oct 2020].
- 13.Worldwide insecticide resistance network (WIN), 2020. Available: https://win-network.ird.fr/ [Accessed 6 Oct 2020].
- 14.Ohrt C, Roberts KW, Sturrock HJW, et al. Information systems to support surveillance for malaria elimination. Am J Trop Med Hyg 2015;93:145–52. 10.4269/ajtmh.14-0257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lourenço C, Tatem AJ, Atkinson PM, et al. Strengthening surveillance systems for malaria elimination: a global landscaping of system performance, 2015-2017. Malar J 2019;18:315. 10.1186/s12936-019-2960-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rahi M, Das P, Sharma A. COVID-19 mitigation steps provide a blueprint for malaria control and elimination. Am J Trop Med Hyg 2020;103:28–30. 10.4269/ajtmh.20-0394 [DOI] [PMC free article] [PubMed] [Google Scholar]