Abstract
Meningioma of the spinal canal is very rare. Clear cell meningioma (CCM) with special histological features occurs more commonly in the spinal cord. A review of the published English-language literature identified 40 reported cases of children with intraspinal CCM and this current report presents an additional case of a 3-year-old child with confirmed lumbar CCM. The current case underwent gross total resection of the CCM. At 9 months after the operation, lumbar magnetic resonance imaging was undertaken and confirmed the absence of tumour recurrence. The child was able to walk normally again. During this period, the child did not receive adjuvant treatments such as radiotherapy and chemotherapy. An evaluation of the 41 cases demonstrated the following: (i) there was no significant difference between the recurrence rate of females and males; (ii) there was a significant difference in the recurrence rate based on the extent of resection (gross total resection versus partial resection); (iii) the recurrence rate in patients where the number of involved segments ≥3 levels was significantly higher than that in patients where the number of involved segments was 1–2 levels. For children with CCM, complete surgical resection might be an important characteristic for predicting the risk of the recurrence of CCM.
Keywords: Clear cell meningioma, spinal canal, recurrence, cerebrospinal fluid metastases
Introduction
Intraspinal meningioma is rare, and its subtype clear cell meningiomas (CCM), is even rarer.1 CCM has a unique histological feature and is described as a polygonal cell with clear cytoplasm, possibly associated with its higher glycine content.1 Although surgery is the main approach for CCM, it is associated with local recurrence and/or cerebrospinal fluid metastasis, which are major challenges during the treatment of CCM.2 Of particular concern are children with CCMs in the spinal canal. A review of the literature identified 40 cases of CCM reported to date.2–29 Worldwide, CCMs in the spinal canal are rare in children.3 This current case report describes a 3-year-old child treated for CCM of the spinal canal and reviews the currently available literature.
Case report
A 3-year-old girl had pain in her thighs for more than 2 months, but she remained active and her parents did not seek medical attention. Then, 1 month later, she began having difficulty walking. Her symptoms gradually worsened so she was admitted to the Department of Neurosurgery, First Affiliated Hospital of Nanchang University, Nanchang, Jiangxi Province, China on 8 March 2019. After admission, a physical examination did not reveal any neurological deficits. Magnetic resonance imaging (MRI) showed an oval-shaped mass of undetermined nature measuring approximately 3 cm in the horizontal position of L2 in the spinal canal (Figure 1). No other spinal lesions were observed. A schwannoma was suspected. The child was prepared for surgery and an L2 laminoplasty was performed. The tumour was completely removed during the operation. After the operation, the pain in both of her legs had subsided and she was able to walk again. Staining of tumour specimens was positive for parakeratin. At 9 months after the operation, the patient had a follow-up lumbar MRI (Figure 2) and no tumour recurrence was observed. The patient could walk normally. During this period, the child did not receive adjuvant treatments such as radiotherapy and chemotherapy.
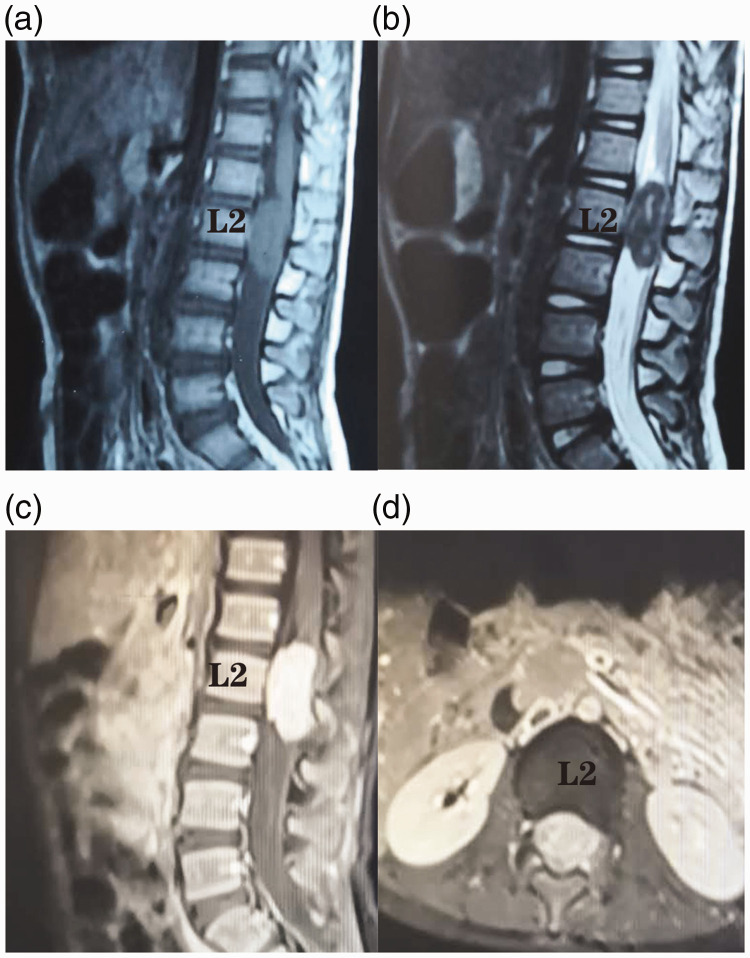
Figure 1.
Representative magnetic resonance imaging (MRI) scans showing an oval-shaped mass of undetermined nature, measuring approximately 3 cm in the spinal canal, in the horizontal position of L2 in a 3-year-old girl that had pain in her thighs for more than 3 months and had difficulty walking when she was admitted for assessment and diagnosis. No other spinal lesions were observed. (a) Sagittal T1 and (b) sagittal T2-weighted MRI images; (c) sagittal and axial (d) enhanced MRI images.
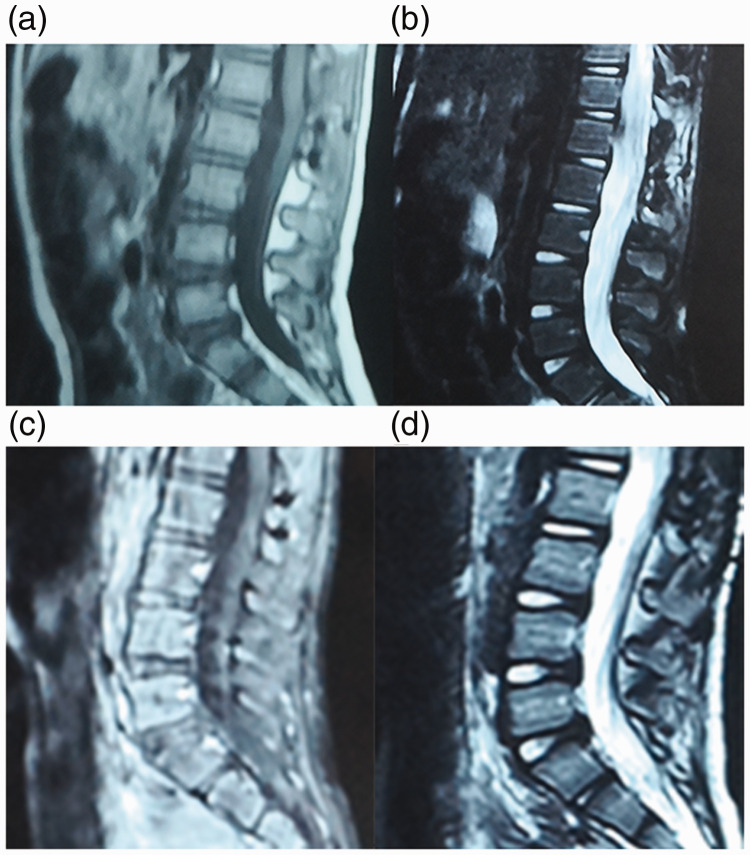
Figure 2.
Representative postoperative magnetic resonance imaging (MRI) scans in a 3-year-old girl that had pain in her thighs for more than 3 months and had difficulty walking when she was admitted for assessment and diagnosis. No tumour recurrence was observed. (a) Sagittal T1 and (b) sagittal T2-weighted MRI images on the third day after surgery; (c) sagittal T1 and (d) sagittal T2-weighted MRI images at 9 months after surgery.
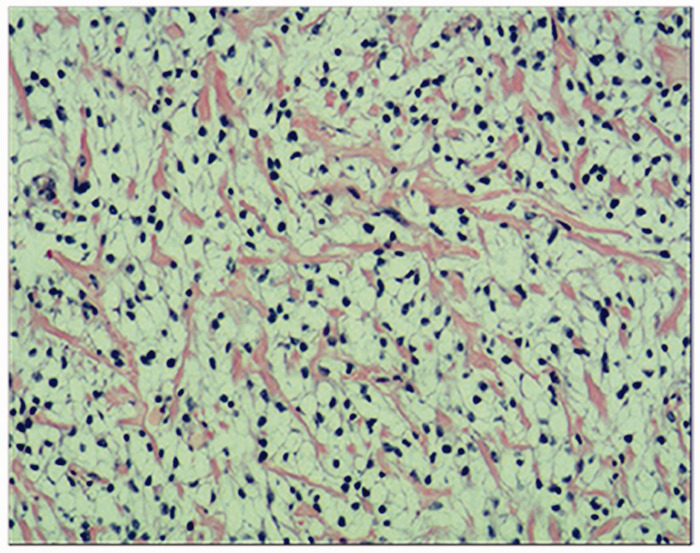
The histopathological results (Figure 3) were assessed by a pathologist at the First Affiliated Hospital of Nanchang University and by a histopathological diagnosis centre in Shanghai. The tumour was identified as a CCM. Tumour samples were stained for the relevant histopathological markers. Periodic acid-Schiff (PAS) staining was positive and immunostaining for Ki-67 showed a positive reaction with a labelling index of 20%. Immunohistochemical staining for parakeratin, vimentin, epithelial membrane antigen (EMA), progesterone receptor (PR), podoplanin (D2-40) and E-cadherin was also positive.
Figure 3.
Representative photomicrograph showing the histopathological findings from a sample of the tumour taken from a 3-year-old girl that had pain in her thighs for more than 3 months and had difficulty walking when she was admitted for assessment and diagnosis. The histology showed sheets of polygonal tumour cells with round or ovoid nuclei and clear cytoplasm. The tissue section was stained with haematoxylin and eosin stain. Scale bar 100 µm. The colour version of this figure is available at: http://imr.sagepub.com.
The parents of the patient provided written informed consent for the submission of this case report to the journal.
Discussion
Clear cell meningiomas are a rare subtype of meningioma that account for only 0.2–0.8% of meningiomas.1,2 In terms of their histopathological features, CCMs are described as polygonal cells with a clear cytoplasm.30 They are characterized by early local recurrence and cerebrospinal fluid metastasis. The World Health Organization defines CCM as grade II cancer. The incidence of CCM in children is higher than that in adults.3 The main symptoms are caused by compression of the parietal nerve.31 On imaging, CCM often has an apparent dural tail sign,26 which is most commonly seen in meningiomas.
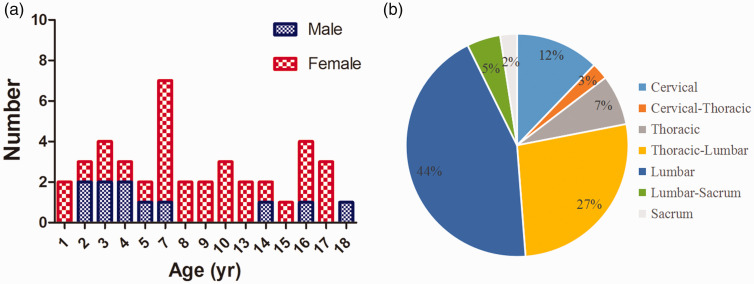
As part of this case report, the electronic databases PubMed® and Embase® were searched from inception to 1 May 2020 using the key words “meningioma” and “clear cell” in order to identify all other cases reported in the English-language literature. The inclusion criteria for cases of paediatric spinal CCM were as follows: (i) the cases were newly diagnosed spinal CCMs; (ii) the patient was <18 years; (iii) clinical characteristics, treatment process and clinical outcome of spinal CCM could be obtained. All statistical analyses of the baseline patient characteristics were performed using Prism 5.0 software (GraphPad Software, San Diego, CA, USA) with categorical data compared with χ2-test or Fisher’s exact test. A P-value < 0.05 was considered statistically significant. Based on the inclusion criteria, a total of 41 paediatric patients with spinal CCMs including this current case were identified.2–29 The characteristics of the 41 included cases are presented in Table 1 and Figure 4.2–29An evaluation of the 40 cases demonstrated the following: (i) there was no significant difference between the recurrence rate of females and males (nine of 29 [31.0%] versus four of 11 [36.4%], respectively); (ii) there was a significant difference in the recurrence rate based on extent of resection (gross total resection versus partial resection: nine of 36 [25.0%] versus four of four [100.0%], respectively; P = 0.002); (iii) the recurrence rate in patients with the number of involved segments ≥3 levels was significantly higher than that in patients with the number of involved segments was 1–2 levels (12 of 19 [63.2%] versus one of 20 [5.0%], respectively; P < 0.001) (Table 2). The data collected from this current literature review demonstrated that CCM can occur in children as young as 1-year-old, suggesting that CCM might develop even earlier, possibly during the growth of the spinal cord in embryonic development. CCM appears to be more common in girls and most cases of CCM reported to date occurred in the thoracic and lumbar spinal cords, rather than the cervical and temporal segments.
Table 1.
Clinical summary of 41 cases of paediatric intraspinal clear cell meningioma reported in the published literature including the present case.2–29
| First author | Age, years | Sex | Tumour location | Operation | RT | Recurrence/ months |
|---|---|---|---|---|---|---|
| Zorludemir 19952 | 9 | F | L3–L5 | GTR | No | Yes/6 |
| Zorludemir 19952 | 17 | F | L4–L5 | GTR | No | No |
| Balogun 20133 | 3 | M | L2–L5 | GTR | No | Yes/9 |
| Carra 20034 | 2 | M | T1–-L4 | GTR | No | Yes/60 |
| Cho 20035 | 17 | F | S1 | GTR | No | NA |
| Colen 20096 | 13 | F | L4–L5 | GTR | Yes | No |
| Douya 20017 | 5 | F | T11–L5 | GTR | No | No |
| Dubois 19988 | 10 | F | L1–L4 | GTR | No | Yes/6 |
| Evans 20159 | 3 | M | L1–L2 | GTR | No | No |
| Greene 200810 | 3 | F | Cervical spine | GTR | No | No |
| Heth 200011 | 7 | F | L4–L5 | GTR | No | No |
| Jallo 200112 | 2 | F | C3–C5 | PR | No | Yes/5 |
| Jallo 200112 | 8 | F | L3–L5 | GTR | No | Yes/6 |
| Kawasaki 202013 | 8 | F | L3 | GTR | No | No |
| Li 201614 | 4 | M | T11–T12 | GTR | No | No |
| Li 201614 | 7 | F | T11–L1 | GTR | No | No |
| Li 201614 | 7 | F | L2–L4 | GTR | No | No |
| Li 201915 | 15 | F | L3 | GTR | No | No |
| Li 201915 | 16 | M | L5–S1 | GTR | No | No |
| Li 201915 | 16 | F | T11–L1 | PR | Yes | Yes/120 |
| Li 201915 | 14 | F | L4 | PR | Yes | Yes/24 |
| Liu 200516 | 2 | M | T10–L1 | GTR | No | Yes/60 |
| Inoue 201817 | 5 | M | L5 | GRT | No | No |
| Matsui, 199818 | 9 | F | T11–T12, L2, L4–L5 |
PR | No | Yes/4 |
| Tunon-Pitalua 201119 | 17 | F | L5–S1 | GTR | No | No |
| Murakami 200120 | 10 | F | T12–L1, L2–L3 | GTR | No | No |
| Oviedo 200521 | 7 | M | L2–L3 | GTR | No | No |
| Park 200022 | 1 | F | T12–L2 | GTR | No | Yes/8 |
| Present case | 3 | F | L2 | GTR | No | No |
| Smith 201723 | 10 | F | L1–L2 | GTR | No | No |
| Tauziede-Espariat 201824 |
13 | F | C4–C5 | GTR | No | No |
| Vural 200725 | 4 | F | C1–C2 | GTR | No | No |
| Wang 201426 | 18 | M | C6–T2 | GTR | No | Yes/18 |
| Wu 201727 | 14 | M | C1–C2 | GTR | No | No |
| Wu 201727 | 7 | F | L2–L4 | GTR | No | No |
| Wu 201727 | 16 | F | T6–T7 | GTR | No | No |
| Wu 201928 | 7 | F | T11–L1 | GTR | No | No |
| Wu 201928 | 7 | F | L2–L4 | GTR | No | No |
| Wu 201928 | 4 | M | T11–12 | GTR | No | No |
| Wu 201928 | 16 | F | T12–L1 | GTR | No | No |
| Yu 200229 | 1 | F | T12–L2 | GTR | No | Yes/8 |
RT, radiotherapy; GTR, gross total resection; PR, partial resection.
Figure 4.
Age and sex distribution (a) and tumour location (b) of 41 cases of paediatric intraspinal clear cell meningioma reported in the published literature including the present case.2–29 The colour version of this figure is available at: http://imr.sagepub.com.
Table 2.
Baseline characteristics of paediatric patients including the present case (n = 40) with spinal clear cell meningioma identified in the published literature stratified according to recurrence.2–4,6–29
| Characteristic | Recurrence group n = 13 |
Non-recurrence group n = 27 |
Statistical analysisa |
|---|---|---|---|
| Sex | NS | ||
| Female | 9 (69.2) | 20 (74.1) | |
| Male | 4 (30.8) | 7 (25.9) | |
| Extent of resection | P = 0.002 | ||
| Gross total resection | 9 (69.2) | 27 (100.0) | |
| Partial resection | 4 (30.8) | 0 (0.0) | |
| Number of involved segmentsb | P < 0.001 | ||
| 1–2 levels | 1 (7.7) | 19 (73.1) | |
| ≥3 levels | 12 (92.3) | 7 (26.9) |
Data presented as n of patients (%).
aBetween-group comparison; Fisher's exact test; NS, no significant difference (P ≥ 0.05).
bData regarding involved segments were not available for one case in the non-recurrence group.
For tumours in the spinal canal, radical resection is the best treatment, but high recurrence rates affect quality of life, particularly in children.3 A previous study proposed that the extent of resection is an important factor when predicting the recurrence of CCM and complete resection is important.31 However, another study reported that despite gross total resection of the tumour, the recurrence rate was as high as 63%.16 In the cases reviewed in the current report (Table 1), four tumours were partially resected and each experienced recurrence within 120 months; two of them within 4–5 months. The remaining 37 patients underwent a gross total resection and nine of them experienced recurrence. The time to recurrence ranged from 6 months to 5 years. Patients that did not experience recurrence may have needed longer follow-up durations. A report of one patient that underwent postoperative radiotherapy after total tumour resection demonstrated no tumour recurrence at a 2-year follow-up.6 It is possible that radiotherapy reduces the recurrence rate of CCM. Controversially, one study did not recommend adjuvant radiotherapy for patients that underwent gross total resection because of the risk that radiotherapy might damage the spinal cord or other organs of paediatric patients.8 For this reason, the present case did not undergo radiotherapy or other kinds of adjuvant therapy. At 9 months after the operation, the present case had a follow-up lumbar MRI (Figure 2), which confirmed that there was no tumour recurrence. The patient was also able to walk normally. Therefore, is postoperative radiotherapy necessary for these patients? This current case will continue to be observed in order to determine their prognosis over a longer period of time.
The use of Ki-67 staining has been recommended to predict the recurrence rate of CCM.13 In this previous case, the Ki-67 labelling index was 26% and no recurrence of CCM was observed at the 2-year follow-up.13 However, some references describe the role of Ki-67 in the recurrence of CCM.2,13 In this current case, the Ki-67 labelling index was 20%. Similarly, tumour samples from the current case were stained for the relevant histopathological markers, including vimentin, EMA, PR, D2-40, E-Cadherin and PAS to predict the recurrence of CCM. Future studies should have longer follow-up times and a larger number of patients.
In conclusion, CCM should be considered a possibility when diagnosing meningiomas of the spinal canal, particularly in children. When pathological evidence is not clear, physicians should consider CCM. Knowing the high recurrence rate of CCM, more attention should be paid to ensure gross total resection is achieved. The establishment of relevant indicators for predicting recurrence risks and determining whether postoperative radiotherapy is necessary.
Footnotes
Author contributions: N.Y. provided this surgical case. Z.H. collected background information and drafted the manuscript. S.H. provided assistance with manuscript revision.
Declaration of conflicting interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Science and Technology Research Project of Jiangxi Provincial Department of Education (no. 170080).
ORCID iD: Nian-Zu Yu https://orcid.org/0000-0001-5195-0768
References
- 1.Ohba S, Sasaki H, Kimura T, et al. Clear cell meningiomas: three case reports with genetic characterization and review of the literature. Neurosurgery 2010; 67: E870–E871. [DOI] [PubMed] [Google Scholar]
- 2.Zorludemir S, Scheithauer BW, Hirose T, et al. Clear cell meningioma. A clinicopathologic study of a potentially aggressive variant of meningioma. Am J Surg Pathol 1995; 19: 493–505. [PubMed] [Google Scholar]
- 3.Balogun JA, Halliday W, Bouffet E, et al. Spinal clear cell meningioma in a 3-year-old: a case report. Pediatr Neurosurg 2013; 49: 311–315. [DOI] [PubMed] [Google Scholar]
- 4.Carra S, Drigo P, Gardiman M, et al. Clear cell meningioma in a 22-month-old male: update after five years. Pediatr Neurosurg 2003; 38: 162–163. [DOI] [PubMed] [Google Scholar]
- 5.Cho CB, Kim JK, Cho KS, et al. Clear cell meningioma of cauda equina without dural attachment. J Korean Neurosurg Soc 2003; 34: 584–585. [Google Scholar]
- 6.Colen CB, Rayes M, McClendon JJ, et al. Pediatric spinal clear cell meningioma. Case report. J Neurosurg Pediatr 2009; 3: 57–60. [DOI] [PubMed] [Google Scholar]
- 7.Douya H, Saegusa O, Saito M, et al. Cauda equina clear cell meningioma without dural attachment: report of two cases. Chiba Igaku 2001; 77: 249–253. [Google Scholar]
- 8.Dubois A, Sevely A, Boetto S, et al. Clear-cell meningioma of the cauda equina. Neuroradiology 1998; 40: 743–747. [DOI] [PubMed] [Google Scholar]
- 9.Evans LT, Van Hoff J, Hickey WF, et al. SMARCE1 mutations in pediatric clear cell meningioma: case report. J Neurosurg Pediatr 2015; 16: 296–300. [DOI] [PubMed] [Google Scholar]
- 10.Greene S, Nair N, Ojemann JG, et al. Meningiomas in children. Pediatr Neurosurg 2008; 44: 9–13. [DOI] [PubMed] [Google Scholar]
- 11.Heth JA, Kirby P, Menezes AH. Intraspinal familial clear cell meningioma in a mother and child. Case report. J Neurosurg 2000; 93: 317–321. [DOI] [PubMed] [Google Scholar]
- 12.Jallo GI, Kothbauer KF, Silvera VM, et al. Intraspinal clear cell meningioma: diagnosis and management: report of two cases. Neurosurgery 2001; 48: 218–221. [DOI] [PubMed] [Google Scholar]
- 13.Kawasaki Y, Uchida S, Onishi K, et al. Pediatric nondura-based clear cell meningioma of the cauda equina: case report and review of literature. Br J Neurosurg 2020; 34: 215–218. [DOI] [PubMed] [Google Scholar]
- 14.Li P, Yang Z, Wang Z, et al. Clinical features of clear cell meningioma: a retrospective study of 36 cases among 10,529 patients in a single institution. Acta Neurochir (Wien) 2016; 158: 67–76. [DOI] [PubMed] [Google Scholar]
- 15.Li J, Zhang S, Wang Q, et al. Spinal Clear Cell Meningioma: Clinical Study with Long-Term Follow-Up in 12 Patients. World Neurosurg 2019; 122: e415–e426. [DOI] [PubMed] [Google Scholar]
- 16.Liu PI, Liu GC, Tsai KB, et al. Intraspinal clear-cell meningioma: case report and review of literature. Surg Neurol 2005; 63: 285–289. [DOI] [PubMed] [Google Scholar]
- 17.Inoue T, Shitara S, Ozeki M, et al. Hereditary clear cell meningiomas in a single family: three-cases report. Acta Neurochir (Wien) 2018; 160: 2321–2325. [DOI] [PubMed] [Google Scholar]
- 18.Matsui H, Kanamori M, Abe Y, et al. Multifocal clear cell meningioma in the spine: a case report. Neurosurg Rev 1998; 21: 171–173. [DOI] [PubMed] [Google Scholar]
- 19.Tunon-Pitalua MC, Molina-Olier O, Alcala-Cerra G, et al. Intra-spinal clear cell meningioma. Case report and literature review. Neurocirugia (Astur) 2011; 22: 50–55 [Article in Spanish, English abstract]. [PubMed] [Google Scholar]
- 20.Murakami T, Imoto K, Takebayashi T, et al. Clear cell meningioma of cauda equina in a 10-year-old child. Tumor Res 2001; 36: 33–38. [Google Scholar]
- 21.Oviedo A, Pang D, Zovickian J, et al. Clear cell meningioma: case report and review of the literature. Pediatr Dev Pathol 2005; 8: 386–390. [DOI] [PubMed] [Google Scholar]
- 22.Park HC, Sohn MJ, Kim EY, et al. Spinal clear cell meningioma presented with progressive paraparesis in infancy. Childs Nerv Syst 2000; 16: 607–610. [DOI] [PubMed] [Google Scholar]
- 23.Smith MJ, Ahn S, Lee JI, et al. SMARCE1 mutation screening in classification of clear cell meningiomas. Histopathology 2017; 70: 814–820. [DOI] [PubMed] [Google Scholar]
- 24.Tauziede-Espariat A, Parfait B, Besnard A, et al. Loss of SMARCE1 expression is a specific diagnostic marker of clear cell meningioma: a comprehensive immunophenotypical and molecular analysis. Brain Pathol 2018; 28: 466–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vural M, Arslantas A, Ciftci E, et al. An unusual case of cervical clear-cell meningioma in pediatric age. Childs Nerv Syst 2007; 23: 225–229. [DOI] [PubMed] [Google Scholar]
- 26.Wang XQ, Huang MZ, Zhang H, et al. Clear cell meningioma: clinical features, CT, and MR imaging findings in 23 patients. J Comput Assist Tomogr 2014; 38: 200–208. [DOI] [PubMed] [Google Scholar]
- 27.Wu L, Yang C, Liu T, et al. Clinical features and long-term outcomes of pediatric spinal meningiomas. J Neurooncol 2017; 133: 347–355. [DOI] [PubMed] [Google Scholar]
- 28.Wu L, Fang J, Yang J, et al. Clinical features and surgical outcomes of spinal clear cell meningioma: An institutional experience. J Clin Neurosci 2019; 69: 55–60. [DOI] [PubMed] [Google Scholar]
- 29.Yu KB, Lim MK, Kim HJ, et al. Clear-cell meningioma: CT and MR imaging findings in two cases involving the spinal canal and cerebellopontine angle. Korean J Radiol 2002; 3: 125–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ahn ES, Chin LS, Gyure KA, et al. Long-term control after resection and gamma knife surgery of an intracranial clear cell meningioma: case report. J Neurosurg 2005; 102: 303–306. [DOI] [PubMed] [Google Scholar]
- 31.Zhang H, Ma L, Wang YB, et al. Intracranial Clear Cell Meningiomas: Study on Clinical Features and Predictors of Recurrence. World Neurosurg 2017; 97: 693–700. [DOI] [PubMed] [Google Scholar]