INTRODUCTION
Pediatric overweight and obesity have reached epidemic proportions in the United States. In fact, more than one-third of US children and adolescents are overweight or obese, defined as having a Body Mass Index (BMI) at or above the 85th percentile.1 In 2007, the American Academy of Pediatrics (AAP) published clinical practice guidelines for the treatment of overweight and obesity in children and adolescents. These guidelines recommend using a stepwise approach to the treatment of pediatric overweight and obesity, including prevention, such as healthy lifestyle choices; controlled weight management; all-inclusive management using providers from multiple disciplines; and tertiary management. The appropriate level of intervention, that is, step, is determined based on a child’s age and BMI percentile.2
Researchers have found the use of the AAP guidelines to be effective in the treatment of pediatric overweight and obesity. In a meta-analysis of 24 randomized trials, combined dietary and physical activity modifications, similar to those recommended in the AAP guideline steps, led to small to moderate improvements in BMI in obese children.3 Furthermore, residential weight loss programs, recommended in the Tertiary Care Intervention step of the AAP guidelines, have resulted in decreases in BMI and fat mass.4 In addition, researchers have found that children following the AAP screen time limitations and physical activity recommendations were less likely to be overweight than their peers not following these recommendations.5
Many health care providers are aware of the existence of the AAP guidelines. Despite this awareness and evidence to support their use, there are gaps between these guidelines and what providers are actually doing in practice. As early as 2006, a study revealed that approximately 73% of nurse practitioners (NPs) working in family or pediatric general practice settings were aware of recommendations to screen for overweight and obesity using BMI.6 However, these practitioners were not regularly using pediatric BMI percentiles to screen for pediatric overweight and obesity. In fact, only 9 of 82 NPs surveyed always calculated a BMI for children at least once a year and only 5 NPs surveyed used changes in BMI percentiles to monitor for disproportionate weight gain.6 In addition, more than 40% of NPs surveyed were not using any guidelines whatsoever to direct their screening for overweight or obesity.6
Other researchers have also studied this phenomenon. During a chart review of well-child visits of 255 children, providers correctly identified only 34% of overweight and obese patients and provided only 11% of overweight and 26% of obese patients with appropriate counseling.7 These findings were echoed in a 2011 study, which surveyed 96 hospital-affiliated pediatric primary care providers. These researchers found that although 83% of providers did use BMI percentiles, less than 25% and 35% of providers used the correct BMI percentile cut offs for overweight and obesity, respectively.8 Furthermore, another study determined that pediatric providers correctly identified only 5% and 28% of overweight and obese patients, respectively, in patient charts.9 Not surprisingly, the use of electronic medical records versus paper charts seems to improve provider documentation of BMI for overweight and obese patients10,11 and will likely be a valuable resource in the screening for and management of pediatric overweight and obesity.
Not only are providers underutilizing the AAP’s guidelines, but it also seems that providers may be overestimating their utilization of these guidelines. Surveys of pediatric providers and chart reviews found that although 93% of providers reported calculating BMI, only 73% of charts had a documented BMI.12 In addition, only 22% of overweight and 51% of obese children were correctly identified as such in the charts. Furthermore, in these surveys, physicians overestimated their discussion of physical activity, sugary beverage intake, and appropriate history taking.12 The aforementioned studies highlight the need for much improvement with regard to pediatric overweight and obesity guideline utilization in the primary care setting. Research has long shown that clinical practice guidelines improve quality of care, patient outcomes, and the consistency of care provided.13 Thus, the proper implementation of these guidelines may improve the care provided to, and the outcomes for, overweight and obese pediatric patients.
Several barriers to the implementation of the AAP guidelines have already been identified in the literature, such as lack of time, lack of training, lack of resources, and patient and provider sensitivity toward the subject of overweight and obesity,14,15 which may prevent or discourage providers from screening for BMI and using these guidelines in primary care. This is echoed by a survey of school nurses, which found not only that BMI was infrequently being used to assess for obesity, but also that school nurses did not feel competent in providing students with appropriate counseling.16 There may be several unidentified barriers unique to school-based health centers (SBHCs) that are hindering implementation of these pediatric overweight and obesity guidelines. Identifying barriers to the implementation of pediatric overweight and obesity clinical practice guidelines may lead to the development of strategies to better enable implementation, thus improving the quality of care provided to overweight and obese patients in SBHCs.
METHODS
This project applied a quality improvement design, using the Plan Do, Study, Act (PDSA) cycle as a methodological framework to improve the use of the AAP overweight and obesity guidelines for children and adolescents in SBHCs. Participants in this quality improvement project were school-based NPs and licensed practical nurses (LPNs) working for a community health network in Manhattan, New York. There were 6 SBHCs within the community health network at the time of this project; each clinic was staffed with one full-time NP and one full-time LPN. The first author (LY) was one of the SBHC NPs and was not a participant in the project. Consequently there were 5 NPs and 6 LPNs who participated in the project. Inclusion criteria were working as an NP or an LPN at an SBHC in Manhattan that was part of a particular community health network. NPs were required to have a master’s degree or higher, and LPNs were required to have a high school diploma and certificate from an LPN school. In addition, all participants were required to speak English. Exclusion criteria included working at an SBHC that was not part of the particular community health network, working at the community health network separate from the school-based health team, and being a different type of health care provider or staff member besides an NP or an LPN. There were no restrictions on participant age, gender, racial or ethnic group, marital status, or socioeconomic status. Of note, however, is that all participants in the sample were women.
This project used a staff survey to assess the barriers to implementation of the AAP’s 2007 recommendations for the treatment of overweight and obesity in SBHCs, knowledge of these guidelines, current practices and adherence to these guidelines, and attitudes toward these guidelines. Surveys from previous studies in the literature review served as a guiding framework for the barrier and attitude questions. In addition, possible barriers unique to school-based health clinics, such as parents not wanting their children to miss classes or parents not being present in the clinic, were also included in the survey. There were 2 separate surveys, 1 for NPs (71 items) and 1 for LPNs (56 items), which were appropriate for each profession’s scope of practice. Participants received a full explanation of the project and its purpose. No compensation for completing the survey was provided. Participant confidentiality was maintained by using Survey Monkey, an online survey tool, to construct a survey that protected the identities of the participants by deidentifying the data. The first author (LY) distributed these surveys from Survey Monkey through the community health network’s secure e-mail system. The Survey Monkey software program stored the data generated.
RESULTS
Barriers
Several barriers were identified through the surveys of NPs and LPNs. Barriers were separated into those found mainly in primary care and those unique to school-based health. The most commonly cited primary care–based barriers by both NPs and LPNs were lack of patient compliance (100%), family lifestyle such as sedentary behaviors and poor eating habits (100%), and the poor dietary practices (100%) and sedentary behaviors (100%) common in American culture. NPs also most frequently cited lack of patient motivation (100%), limited parent motivation and involvement in the treatment process (100%), and parent refusal to recognize their child’s overweight or obese status (100%) as barriers. In addition, LPNs most frequently cited insufficient community resources to refer to (100%) as a barrier.
Of those barriers specifically related to school-based health, the most commonly cited barrier by both NPs and LPNs was the fact that children have little control over the groceries purchased and food cooked at home (100%). NPs also most commonly cited the lack of parent or guardian physical presence during an appointment (100%) as a barrier (Fig. 1). LPNs also frequently cited that children have difficulty paying attention to counseling provided in the SBHCs (83.34%) (Fig. 2).
Fig. 1.
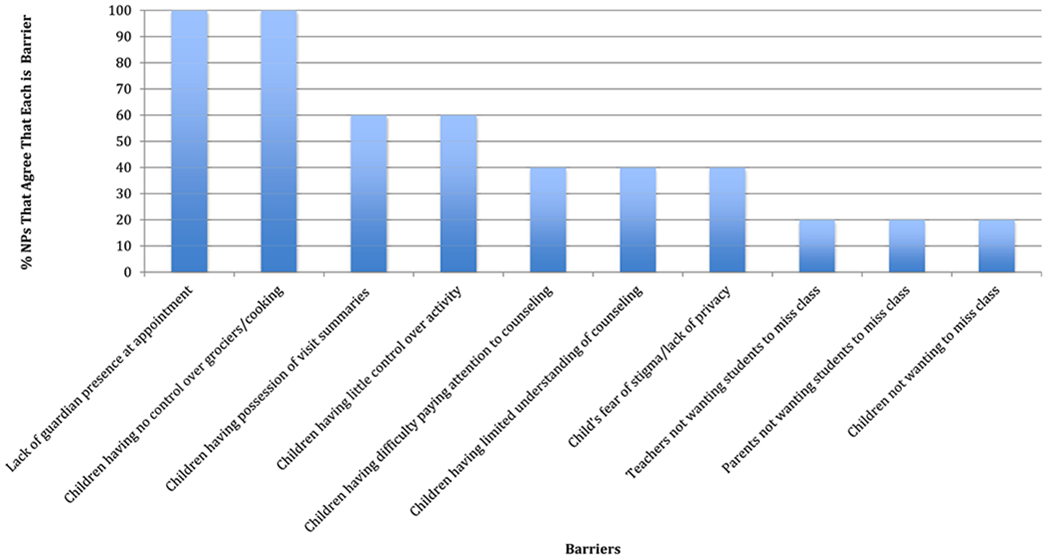
Barriers unique to school-based health—NP.
Fig. 2.
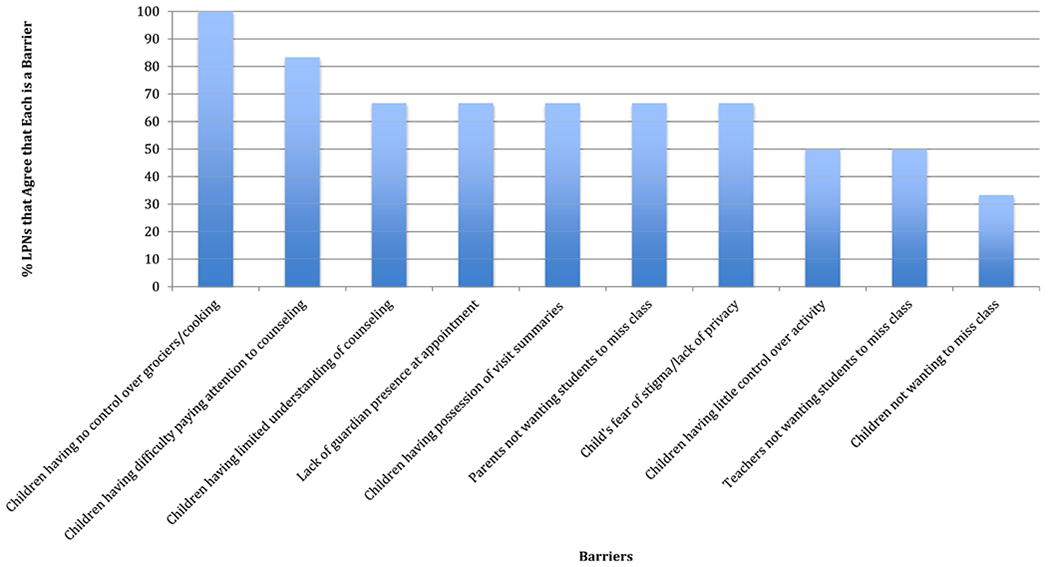
Barriers unique to school-based health—LPN.
When asked about other possible barriers to guideline implementation in the school-based clinic setting, 2 NPs noted poor communication with primary care providers (PCPs) and having to direct patients to their PCP to obtain needed referrals. In addition, 2 NPs noted competing mental health issues and stress as barriers to addressing overweight and obesity. Another NP mentioned patient and family motivation and one LPN cited a lack of parent involvement.
When asked what would be helpful in the SBHCs to address these barriers, 2 NPs mentioned having clear, step-by-step protocols readily available in the clinics. Three NPs recommended additional services and resources in the school, such as mental health services, a nutritionist, and more staff. One NP mentioned finding ways to increase continuity between patients, parents, and the clinic. Two LPNs suggested more student and parent workshops to address this discontinuity issue and increase involvement of patients and families in physical activities and healthy lifestyles.
Attitudes
All LPNs and 4 of 5 NPs agreed that pediatric overweight and obesity is a significant problem in the United States, whereas 5 of 6 LPNs and all 5 NPs believed they could make an impact on the epidemic. All NPs and half of the LPNs were familiar with the AAP guidelines and believed that these recommendations could be effective in the management of pediatric overweight and obesity. Additional NP and LPN attitudes are included in Tables 1 and 2. Of particular note is that 4 of 5 NPs and only half of the LPNs believed they had adequate training to provide patients with proper dietary and physical activity recommendations and all NPs agreed that having practice recommendations and protocols readily available in the school-based health clinic would be helpful in their treatment of overweight and obese patients.
Table 1.
Nurse practitioner attitudes
| Attitude | Strongly Disagree (N) | Disagree (N) | Agree (N) | Strongly Agree (N) |
|---|---|---|---|---|
| Measuring and documenting BMI is an important part of the assessment of pediatric overweight and obesity | 0 | 0 | 3 | 2 |
| I have adequate training to provide patients with proper dietary and physical activity counseling and treatment for overweight and obesity | 0 | 1 | 2 | 2 |
| I feel comfortable discussing pediatric overweight and obesity with my patients and their families | 0 | 0 | 3 | 2 |
| Having practice recommendations and protocols readily available in the school-based health clinic would be helpful in my treatment of pediatric overweight and obesity | 0 | 0 | 3 | 2 |
| I feel more comfortable treating other medical conditions, such as asthma and atopic dermatitis, than I do treating overweight and obesity | 0 | 2 | 2 | 1 |
Table 2.
Licensed practical nurse attitudes
| Attitude | Strongly Disagree (N) | Disagree (N) | Agree (N) | Strongly Agree (N) |
|---|---|---|---|---|
| Measuring and documenting BMI is an important part of the assessment of pediatric overweight and obesity | 0 | 0 | 4 | 2 |
| I have adequate training to provide patients with proper dietary and physical activity counseling and treatment for overweight and obesity | 0 | 3 | 3 | 0 |
| I feel comfortable discussing pediatric overweight and obesity with my patients and their families | 0 | 1 | 5 | 0 |
| Having practice recommendations and protocols readily available in the school based health clinic would be helpful in my treatment of pediatric overweight and obesity | 0 | 0 | 5 | 1 |
| I feel comfortable weighing and measuring children | 0 | 0 | 3 | 3 |
Current Practices
All NPs and 5 of 6 LPNs reported assessing and documenting BMI at least annually starting at age 2 years. With regard to health behaviors, all NPs reported assessing most of the recommended dietary and activity factors. Three of five NPs (60%) reported assessing frequency of eating outside of the home. Only 2 of 5 NPs (40%) reported assessing excessive portion sizes. All NPs reported counseling on most of the dietary and physical activity recommendations. However, only 2 of 5 NPs (40%) noted routinely counseling to remove televisions and other electronic screens from children’s primary sleeping areas. Only one NP reported counseling on eating meals together as a family, allowing the child to self-regulate food intake, and avoiding overly restrictive feeding behaviors.
None of the NPs and half of the LPNs reported scheduling monthly follow-up visits as recommended when a child is identified as overweight or obese. In addition, only 3 of 5 NPs reported routinely ordering the recommended screening blood work for overweight children and only 2 of 5 NPs order the recommended blood work for obese children. There were also inconsistencies among NPs regarding when they chose to counsel parents to increase monitoring via logs of diet, physical activity, and sedentary behaviors; to refer patients to a comprehensive multidisciplinary team; to refer patients to a tertiary weight management center; and to counsel patients and parents regarding weight maintenance and/or weight loss.
Knowledge
All NPs and LPNs knew the correct age for beginning assessment of BMI. All NPs and 5 of 6 LPNs knew the correct BMI percentile for obese children. However, only 4 of 5 NPs (80%) knew the correct criteria for a normal BMI percentile, and only 3 of 5 NPs (60%) knew the correct criteria for an overweight BMI percentile. Only 2 LPNs (33%) knew the correct BMI percentile for normal weight and overweight children. In addition, only 3 of 5 NPs (60%) correctly identified the recommended screening blood work for an obese child.
All NPs knew when an overweight or obese child should progress from general dietary and exercise recommendations to increased monitoring. However, none knew that increased monitoring involves further reduction in screen time and referral to a dietician. Furthermore, none of the NPs knew that obese children typically have weekly visits when referred to a multidisciplinary team, and one NP did not know that tertiary care interventions should occur in pediatric weight management settings.
DISCUSSION
Evaluating the barriers to implementation of pediatric overweight and obesity guidelines will enable NPs and LPNs in SBHCs to overcome barriers unique to the school-based health setting. The surveys identified several issues within the SBHCs. The current practices of the school-based health staff do not align with the AAP guidelines. In addition, barriers identified in this project were similar to those identified in the literature. These barriers included those that school-based providers can control, such as provider and practice barriers, and those that school-based health nurses have little control over, such as patient and community or societal barriers.
Issues that can be immediately addressed are those that the school-based health providers can control, which are the provider and practice barriers. As the studies found in the literature,14,17–20 some of the NPs and LPNs felt that they needed more training to provide patients with proper dietary and physical activity recommendations. These findings are also reflected in earlier surveys of school nurses, which found that school health staff did not feel competent in providing students with appropriate diet and activity counseling.16 In addition, like the existing literature,21 a major problem identified in the surveys was that the school-based NPs and LPNs do not fully understand the proper BMI percentile cut offs for normal, overweight, and obese children. Consequently, children may not be receiving treatment per the AAP guidelines simply because the providers do not recognize their overweight or obese status. Proper identification of overweight and obese students is vital to prevention and treatment. Furthermore, some of the NPs surveyed in this project reported that they do not know and are not ordering the recommended blood work for overweight and obese children. Consequently, continuing education focused on the management of overweight and obese children should be provided to the school-based staff. This training should include dietary and activity counseling and proper identification of overweight and obese BMI percentiles.
All NPs agreed that having a written practice protocol for the treatment of pediatric overweight and obesity would be helpful in the SBHCs. In addition, 2 NPs mentioned having clear practice protocols again when asked what would be helpful to overcome barriers to guideline implementation. Clear, straightforward protocols, including recommended blood work, should be embedded as treatment templates into the electronic health record system used by the SBHCs. This project found that, like previous studies,14 lack of follow-up appointments was a significant barrier. Overweight and obese students were not being seen in the SBHCs regularly for follow-up appointments. Thus, regular follow-up appointments should be included as part of these treatment protocols. There were also large discrepancies amongst the NPs regarding when they chose to counsel patients and parents to increase monitoring via logs, to refer patients to comprehensive multidisciplinary teams, or to refer patients to tertiary weight management centers. These inconsistencies were also reflected in the assessment of guideline knowledge. Thus, the suggested stepwise treatments should also be assimilated into the treatment protocols.
This project identified barriers unique to school-based health that were not found in the literature, such as the lack of parent or guardian physical presence during an appointment and lack of communication with PCPs, resulting in poor continuity of care. Specific protocols encouraging increased communication with parents and PCPs during and after appointments and encouraging parents to accompany their children to the clinic if possible are ways in which these barriers can be overcome. These findings were presented to the school-based health team and obesity education sessions have been developed for the subsequent school year as a first step to overcome some of these barriers.
Interestingly, a lack of time identified by other researchers6,14,17–21 was not one of the most frequently cited barriers. This makes sense; SBHCs have more flexible schedules because providers may call down students from class at times that are convenient for the clinic. Also unlike the literature, lack of health insurance6,14 was not one of the most frequently cited barriers. This also makes sense, because SBHCs do not collect fees directly from patients or families, regardless of a patient’s insurance status. These 2 factors emphasize the unique opportunities school-based health providers have to affect the struggle against the overweight and obesity epidemic in the United States.
Strengths and Limitations
Many of the reported barriers were similar to what is known in the literature. However, one of the strengths of this project is that it highlighted barriers that are possibly unique to school-based health. Another strength of this project was the length and detail of the surveys distributed, which resulted in a lot of information gleaned from respondents’ answers. Furthermore, there were open-ended questions at the end of the survey, which allowed respondents to include additional information. However, a major limitation of this scholarly project was the small sample size and that project was performed exclusively at 6 SBHC branches of one community health network in Manhattan, NY, which limits the generalizability of these findings. Future quality improvement and research should seek to gather further knowledge of the barriers to implementation of the AAP’s obesity guidelines in larger, more diversified samples.
Future Implications for Practice
The most commonly reported barriers were those largely out of the provider’s control. In addition, this project uniquely highlighted the fact that children have little control over the groceries purchased and food cooked at home. Barriers embedded in cultural and home life contexts are more difficult to act on than barriers found within the clinics. However, possible ways to address these barriers, and future intervention phases for PDSA cycles, include sending home printed educational information regarding healthy eating, physical activity, and screen time with students after their appointments. In addition, as suggested by the LPNs, organizing student and parent workshops to increase involvement of patients and families in physical activities and to promote healthy lifestyles is a possible way to overcome these barriers.
Like a previous study, NPs also cited competing health care needs, such as stress and mental health issues,21 taking priority over overweight and obesity counseling as a barrier. At the time of the survey, only 4 of the 6 SBHCs surveyed had part time access to social workers that address mental health needs. Some of the staff suggested increasing services, such as mental health services, as a potential means of overcoming this barrier. Although this is a costly and time-consuming solution, this may be explored in the future as a means of alleviating competing health care needs.
Another barrier uniquely cited in this project was the fact that children have difficulty paying attention to counseling provided in the school-based health clinics. The lack of parent or guardian presence in the clinic exacerbates this barrier, because adults are not physically present in the clinics with their children to hear and reinforce this counseling. This is further reflected by only 1 NP reporting counseling on eating meals together as a family, allowing the child to self-regulate food intake, and avoiding overly restrictive feeding behaviors. School-based health providers must be creative in addressing this barrier. Using motivational interviewing in the future may be an effective way to increase student engagement during appointments.
SUMMARY
Pediatric overweight and obesity is a grave public health issue in the United States. With overweight and obesity come significant physical health problems, psychological problems, social problems, and school problems. In 2007, the American Academy of Pediatrics published clinical practice guidelines for the treatment of overweight and obesity in children and adolescents. However, health care providers are not using these guidelines due to a variety of barriers already identified in the literature. Treatment of overweight and obese students in SBHCs presents unique problems; however, this has not been assessed in the existing literature. This project identified unique barriers to treatment in SBHCs, including lack of parent or guardian presence and difficulties in promoting continuity of care between the SBHCs and PCPs. From this work, we can begin to develop interventions to help address these issues within the school-based clinical setting. Identifying barriers to guideline implementation will empower school-based health providers to address these barriers, perhaps leading to the implementation of changes that transform these barriers into facilitators. These actions may improve the quality of care provided to overweight and obese pediatric patients, which could also lead to positive impacts on BMI and may improve health outcomes for overweight and obese children.
KEY POINTS.
This article aims to identify the barriers to the implementation of the 2007 American Academy of Pediatrics’ Recommendations for Treatment of Child and Adolescent Overweight and Obesity in a school-based primary care setting.
This project applied a quality improvement design using the Plan, Do, Study, Act cycle. An electronic survey was administered to nurse practitioners and licensed practical nurses working in school-based health clinics in New York. The survey assessed perceived barriers to guideline implementation and knowledge of, attitudes toward, and adherence to these guidelines.
There were gaps in guideline knowledge and discrepancies in assessment, counseling, and treatment practices.
The most commonly cited primary care–based barriers were lack of patient compliance, family lifestyle, and the poor dietary practices and sedentary behaviors common in America. The most commonly cited school-based barriers were that children have little control over the groceries purchased and foods cooked at home and the lack of parent presence during appointments.
Footnotes
Disclosure Statement: The authors have no relevant financial relationships with any commercial companies that have a direct financial interest in subject matter or materials discussed in this article or with any companies making any competing products.
REFERENCES
- 1.Centers for Disease Control and Prevention. Childhood obesity facts 2015. Available at: http://www.cdc.gov/healthyschools/obesity/facts.htm. Accessed July 15, 2018.
- 2.Spear BA, Barlow SE, Ervin C, et al. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics 2007;120(s4):s254–88. [DOI] [PubMed] [Google Scholar]
- 3.McGovern L, Johnson JN, Paulo R, et al. Treatment of pediatric obesity: a systematic review and meta-analysis of randomized trials. J Clin Endocrinol Metab 2008; 93(12):4600–5. [DOI] [PubMed] [Google Scholar]
- 4.Gately PJ, Cooke CB, Barth JH, et al. Children’s residential weight-loss programs can work: a prospective cohort study of short-term outcomes for overweight and obese children. Pediatrics 2005;116(1):73–7. [DOI] [PubMed] [Google Scholar]
- 5.Laurson KR, Eisenmann JC, Welk GJ, et al. Combined influence of physical activity and screen time recommendations on childhood overweight. J Pediatr 2008;153(2):209–14. [DOI] [PubMed] [Google Scholar]
- 6.Larsen L, Mandleco B, Williams M, et al. Childhood obesity: prevention practices of nurse practitioners. J Am Acad Nurse Pract 2006;18(2):70–9. [DOI] [PubMed] [Google Scholar]
- 7.Reyes I An evaluation of the identification and management of overweight and obesity in a pediatric clinic. J Pediatr Health Care 2015;29(5):e9–14. [DOI] [PubMed] [Google Scholar]
- 8.Rausch JC, Perito ER, Hametz P. Obesity prevention, screening, and treatment practices of pediatric providers since the 2007 expert committee recommendations. Clin Pediatr 2011;50(5):434–41. [DOI] [PubMed] [Google Scholar]
- 9.Dilley KJ, Martin LA, Sullivan C, et al. Identification of overweight status is associated with higher rates of screening for comorbidities of overweight in pediatric primary care practice. Pediatrics 2007;119(1):e148–55. [DOI] [PubMed] [Google Scholar]
- 10.Bode DV, Roberts TA, Johnson C. Increased adolescent overweight and obesity documentation through a simple electronic medical record intervention. Mil Med 2013;178(1):115–8. [DOI] [PubMed] [Google Scholar]
- 11.Keehbauch J, San Miguel G, Drapiza L, et al. Increased documentation and management of pediatric obesity following implementation of an EMR upgrade and education. Clin Pediatr 2012;51(1):31–8. [DOI] [PubMed] [Google Scholar]
- 12.Chelvakumar G, Levin L, Polfuss M, et al. Perception and documentation of weight management practices in pediatric primary care. WMJ 2014;113(4):149–53. [PubMed] [Google Scholar]
- 13.Woolf AH, Grol R, Hutchinson A, et al. Potential benefits, limitations, and harms of clinical guidelines. BMJ 1999;318(7182):527–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Findholt NE, Davis MM, Michael YL. Perceived barriers, resources, and training needs of rural primary care providers relevant to the management of childhood obesity. J Rural Health 2013;29(s1):s17–24. [DOI] [PubMed] [Google Scholar]
- 15.Walker O, Strong M, Atchinson R, et al. A qualitative study of primary care clinicians’ views of treating childhood obesity. BMC Fam Pract 2007;8(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nauta C, Byrne C, Wesley Y. School nurses and childhood obesity: an investigation of knowledge and practices among school nurses as they relate to childhood obesity. Issues Compr Pediatr Nurs 2009;32(1):16–30. [DOI] [PubMed] [Google Scholar]
- 17.Jelalian E, Boergers J, Alday CS, et al. Survey of physician attitudes and practices related to pediatric obesity. Clin Pediatr 2003;42(3):235–45. [DOI] [PubMed] [Google Scholar]
- 18.Klein JD, Sesselberg TS, Johnson MS, et al. Adoption of body mass index guidelines for screening and counseling in pediatric practice. Pediatrics 2010;125(2):265–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Small L, Anderson D, Sidora-Arcoleo K, et al. Pediatric nurse practitioners’ assessment and management of pediatric overweight/obesity: result from 1999 and 2005 cohort surveys. J Pediatr Health Care 2009;23(4):231–41. [DOI] [PubMed] [Google Scholar]
- 20.Story MT, Neumark-Stzainer DR, Sherwood NE, et al. Management of child and adolescent obesity: attitudes, barriers, skills, and training needs among health care professionals. Pediatrics 2002;110(s1):210–4. [PubMed] [Google Scholar]
- 21.Flower KB, Perrin EM, Viadro CL, et al. Using body mass index to identify overweight children: barriers and facilitators in primary care. Ambul Pediatr 2007; 7(1):38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]


