Abstract
Introduction:
The most common cause of myocardial ischemia is atherosclerotic epicardial coronary artery disease, present in 90% of patients. Risk factors positively correlate with the onset, development and subsequent complications of atherosclerotic disease.
Aim:
Determine the percentage frequency of classic risk factors for coronary disease in patients with non-ST segment elevation myocardial infarction (NSTEMI), with regard to gender.
Methods:
A retrospective study was conducted on 600 respondents, treated for NSTEMI at the Clinic for Internal Medicine of the University Clinical Center (UKC) Tuzla, in the period from June 2016 to December 2019.
Results:
Overall, smoking was the leading risk factor (65%), followed by hypertension (58%), hyperlipoproteinemia (39%), overweight (33%), positive family burden (30%) and diabetes mellitus (19%). In male patients, the leading risk factor was smoking, rating at 74%, while in female patients – it was hypertension at 67%. In younger groups of patients leading risk factors were smoking and a positive family burden.
Conclusion:
With adequate prevention and treatment measures, a significant reduction in the prevalence of the cardiovascular disease can be achieved, since the risk factors for its development have long been known. Quitting smoking is one of the most effective secondary prevention measure since it reduces the reinfarction risk rate by 50%. Knowledge of coronary risks, as well as success in reducing them, can greatly contribute to patients’ overall sense of contentment and significantly raise their self-confidence.
Keywords: risk factors, coronary disease, smoking
1. INTRODUCTION
Cardiovascular disease (CVD) is one of the most important health and economic problems of the modern world. Ischemic heart disease (IHD) is the leading cause of death in men over 45 and women over 65 years of age (1). The disease affects men earlier, while women are mostly protected until menopause, due to estrogen. With the onset of menopause, this difference is equalized, so the incidence and mortality of IHD become approximately the same (2).
The most common cause of myocardial ischemia is atherosclerotic epicardial coronary artery disease, present in 90% of patients (3). Atherosclerosis is a multifactorial, inflammatory disease, not the result of mere lipid accumulation (4). Epidemiological studies have shown that the risk of atherosclerosis is associated with certain risk factors. The “classic” risk factors are elevated blood pressure, diabetes, hypercholesterolemia, overweight, physical inactivity, smoking, gender, genetics and age (1).
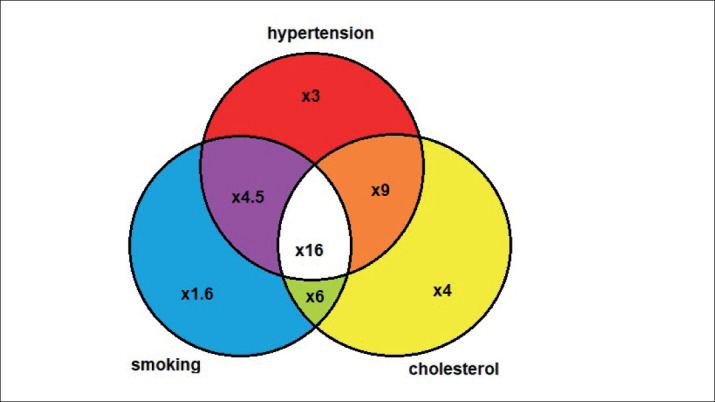
Individual (as an independent variable), and to an even greater extent combined risk factors (in different combinations, when their combined effect is mutually potentiated and multiplied), have a significant role in the development and occurrence of IHD (Figure 1) (5). Elevated arterial pressure is the first of the observed risk factors favoring the onset of atherosclerotic CVD (6).
Figure 1. The level of risk associated with hypertension, smoking and high cholesterol. (adapted from Poulter, 1993).
2. AIM
The aim of this study was to determine the percentage frequency of classic risk factors for IHD in patients with non-ST segment elevation myocardial infarction (NSTEMI), with regard to gender.
3. PATIENTS AND METHODS
A retrospective study was conducted on 600 respondents, treated for NSTEMI at the Clinic for Internal Medicine of the University Clinical Center Tuzla, in the period from June 2016 to December 2019. There were 370 male and 230 female respondents, ages 30-79, with an average age of 52.4±10.2 years. The diagnosis of NSTEMI was made based on typical changes: troponin levels, electrocardiographic and echocardiographic findings. The percentages of leading risk factors (hypertension, smoking, hyperlipoproteinemia, overweight, diabetes mellitus, and positive family burden) in the total sample and with regard to gender were determined. Nutritional status was assessed based on the Body Mass Index (BMI), the ratio between body mass expressed in kilograms to squared body height expressed in meters. The reference value of BMI for overweight was over 25. The results obtained were statistically analyzed by the standard descriptive statistics method (measures of central tendency, dispersion and association).
4. RESULTS
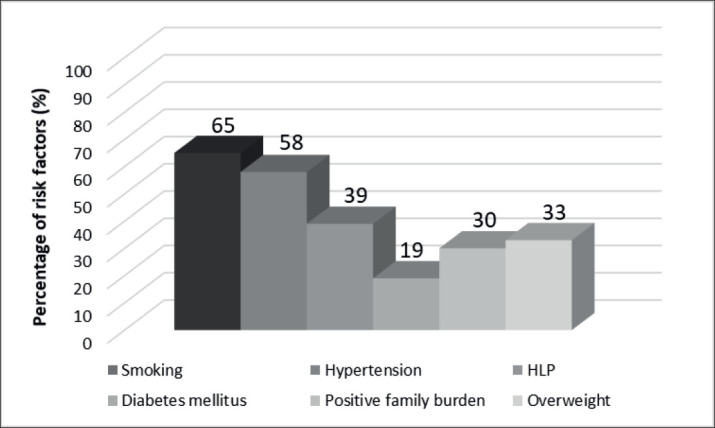
In a total sample of 600 respondents, smoking was the leading risk factor in 65% (392/600), followed by hypertension in 58% (345/600), hyperlipoproteinemia (HLP) in 39% (235/600), overweight in 33% (200/600), a positive family burden in 30% (180/600) and diabetes mellitus in 19% (115/600) (Figure 2).
Figure 2. Risk factors in a total sample of respondents.
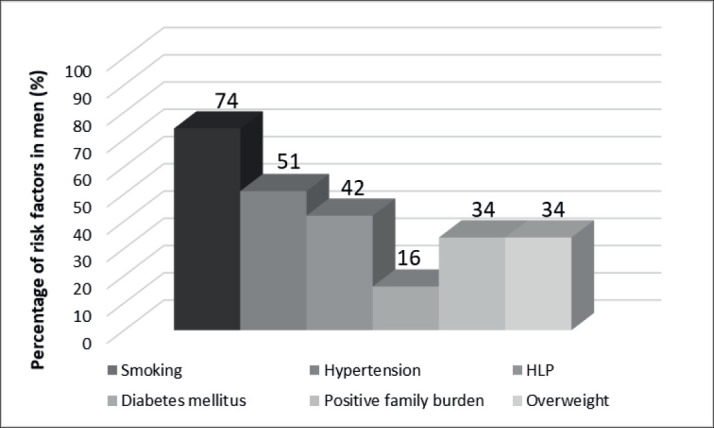
The leading risk factor in men was smoking, in 74% (272/370), of which the majority, 54% (200/370), had a smoking history of more than five years. Hypertension was present in 51% (190/370), followed by: HLP 42% (155/370), overweight 34% (125/370), positive family burden 34% (125/370), and diabetes mellitus in 16% (60/370) (Figure 3).
Figure 3. Risk factors in men with NSTEMI.
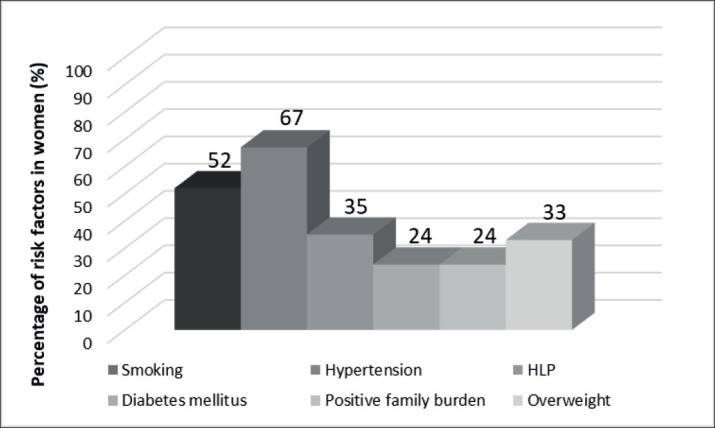
The leading risk factor in women was hypertension in 67% (155/230) of respondents, followed by smoking 52% (120/230), HLP 35% (80/230), overweight 33% (75/230), diabetes mellitus 24% (55/230) and positive family burden in 24% (55/230), as shown in Figure 4.
Figure 4. Risk factors in women with NSTEMI.
5. DISCUSSION
Hypertension is considered to be the most important risk factor for IHD. According to some studies, people with high blood pressure have a three times higher risk of developing CVD compared to normotensive individuals (7). In our study, hypertension was present in 58% of respondents, which is slightly lower compared to some previous studies from the region (8). These results can be explained by a higher percentage of respondents belonging to younger age groups, in our total sample. With regard to gender, hypertension was more common in women than in men (67% and 51%, respectively).
The leading risk factor in terms of frequency was smoking (65% of all respondents). With regard to gender, smoking was identified as a risk factor in 74% of male and 52% of women. The high ranking of smoking on the risk factors scale supports the notion of other authors that there is no safe level of cigarette smoking and that every cigarette is harmful (9).
Hyperlipoproteinemia was present in 39% of all respondents and ranked third on the risk factors scale. It was present in more than 30% of respondents in all age groups. With regard to gender, it was more common in men than in women (42% and 35%, respectively). Low high-density lipoprotein (HDL) has also been shown to be the most common indicator of dyslipidemia for IHD (10).
Overweight was present in 33% of respondents overall, and ranked fourth on the risk factors scale. It was also present in more than 30% of respondents in all age groups. With regard to gender, overweight was approximately equally frequent in both women and men (33% and 34%, respectively). Furthermore, positive family burden was present in 30% of all respondents, and it was more common in men than in women (34% and 24%, respectively).
Individuals with diabetes mellitus belong to a high-risk group for IHD, especially acute myocardial infarction, and they are three times more likely to develop the disease. The study by Rabbi et al. found that diabetes mellitus was present in 15 to 20% of all examined cases with acute myocardial infarction, which also had more frequent reinfarctions (11). IDH occurs in about half of the individuals with diabetes mellitus, with 20% of them developing a myocardial infarction. Intensive treatment of metabolic parameters may suppress the negative effects of hyperglycemia (12).
People with multiple risk factors (arterial hypertension, smoking, and hyperglycemia) are at a higher risk of many complications, including reinfarction and sudden death (13). Studies by other researchers have shown that the risk of ischemic stroke is three times more common in women who use oral contraceptives, in addition to being hypertensives and smokers (14).
In our study, men suffering from myocardial infarction were most often smokers (74%) and hypertensives (51%), while women were most often hypertensive (67%), followed by smokers (52%). A high percentage (67%) of positive family burden was present among respondents of both genders aged 30 to 39, and it decreased in older age groups. These results suggest that those with a positive family burden have a much higher risk of myocardial infarction at a younger age.
In the early 20th century, CVDs were responsible for 10% of mortality in the world (15). Today, they are responsible for half of the deaths in the developed world, due to the continuous implementation of public health improvement measures (vaccinations), which contributed to a significant increase in life expectancy, but also a sudden increase in CVD prevalence (16). Approximately one in five men and one in six women die from this disease (17).
In Bosnia and Herzegovina, there has always existed a tendency for IHD to increase. Coronary vascular diseases have been significant causes of mortality and morbidity since the 1960s, and the incidence has been higher in urban than in rural populations. From 1970 to 1990 mortality from CVDs in our country has tripled (18); accounting for 1/2 of the total mortality, while the second half included: malignant tumors, poisonings, injuries, respiratory diseases and others.
6. CONCLUSION
Over 50% of patients with acute myocardial infarction suffer from arterial hypertension, and 50% of those with untreated arterial hypertension die from acute myocardial infarction. Applying adequate preventive measures and treating patients, a significant reduction in the prevalence of CVDs can be achieved, as risk factors for their development have long been known. Smoking cessation is one of the most effective measures of secondary prevention, as it reduces the risk of reinfarction. The risk of CVD with combined risk factors (smoking, hypertension, and serum cholesterol above 8.5 mmol/L) is multiplied 16-fold (7).
Regular physical activity after myocardial infarction reduced mortality by 20%, as shown in a meta-analysis (19). Knowledge of coronary risks, as well as success in reducing them, can greatly contribute to patients’ sense of satisfaction and self-confidence. Patients and physicians should put more effort into emphasizing metabolic risk factors, which along with diabetes mellitus markedly increase the risk of reinfarction.
Author’s contribution:
All authors were included in all steps of preparation this article. Final proof reading was made by the first author.
Conflict of interest:
None to declare.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Cevc M. Jesu li trigliceridi samostalan i neovisan čimbenik rizika obolijevanja od koronarne bolesti? [Are triglycerides autonomous and independent risk factors for coronary heart disease?] Lipidi. 2000;9:3–9. [Google Scholar]
- 2.Kocijančić M. Cardiovascular medicine. [Cardiovascular medicine] Nauka, Belgrade. 1999:353–392. [Google Scholar]
- 3.Henry DP. Atherosclerosis and vascular protection: Symposium of atherogenesis. Am J Cardiol. 1990;66:31–61. [Google Scholar]
- 4.Miller M, Cannon CP, Myrphy SA, Qin J, Ray KK, Braunwald E PROVE IT-TIMI 22 Investigators. Impact of triglyceride levels beyond LDL cholesterol after acute coronary syndrome in the PROVE IT-TIMI 22 trial. J Am Coll Cardiol. 2008;51:724–730. doi: 10.1016/j.jacc.2007.10.038. [DOI] [PubMed] [Google Scholar]
- 5.Stožinić S. Infarkt miokarda. [Myocardial infarction] Naučna knjiga, Belgrade. 1991:198–284. [Google Scholar]
- 6.Rumboldt Z, Giunio L, Mirić D, Polić S, Božić A, Tonkić A. War-stress-induced medical emergencies in South Croatia. Lancet. 1993;341:965–966. doi: 10.1016/0140-6736(93)91260-s. [DOI] [PubMed] [Google Scholar]
- 7.Poulter N. Cardiovascular disease: Risk factors and intervention. In: Poulter N, Sever P, Thom S, editors. Oxford: Redcliffe Medical Press; 1993. pp. 330–336. [Google Scholar]
- 8.Sinanović O. Tuzla: Faculty of Medicine, University of Tuzla; 1983. Prognoza medikamentoznog i fizikalnog liječenja bolesnika sa akutnim cerebrovaskularnim inzultom. [Prognosis of medicament and physical treatment of patients with acute cerebrovascular stroke] Master’s thesis. [Google Scholar]
- 9.čop N. Smoking and Stroke. Medicus. 2001;10:55–62. [Google Scholar]
- 10.Shehab A, Al-Dabbagh, Almahmeed W, Bustani N, Nagelkerke N, Alnaeemi A, et al. Prevalence, characteristics and in-hospital outcomes of metabolic syndrome among patients with acute coronary syndrome in the United Arab Emirates. The Open Cardiovascular Medicine Journal. 2012;6:81–87. doi: 10.2174/1874192401206010081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Norris RM, Sammel NL. Predictor of late hospital death in acute myocardial infarction. Progress in Cardiovascular Diseases. 1980;23:257–260. doi: 10.1016/0033-0620(80)90008-0. [DOI] [PubMed] [Google Scholar]
- 12.Grembiale A, Cloro C, Iorio F, Cufone S, Succuro E, Arturi F. [Hyperglycaemia and acute coronary syndrome] Clin Ter. 2012;163:403–409. [PubMed] [Google Scholar]
- 13.May GS, Eberlein KA, Furberg CD, Passamani ER, DeMets DL. Secondary prevention after myocardial infarction: a review of long-term trials. Progress in Cardiovascular Diseases. 1982;24:331–352. doi: 10.1016/0033-0620(82)90010-x. [DOI] [PubMed] [Google Scholar]
- 14.Vidović M. Faculty of Medicine, University of Tuzla; 2002. Kvalitet života nakon moždanog udara. [Quality of life after stroke] Master’s thesis. [Google Scholar]
- 15.Gaziano TA. Economic burden and the cost-effectiveness of treatment of cardiovascular disease in Africa. Heart. 2008;94:140–144. doi: 10.1136/hrt.2007.128785. [DOI] [PubMed] [Google Scholar]
- 16.Zaman JM, Brunner E. Social inequalities and cardiovascular disease in South Asians. Heart. 2008;94:406–407. doi: 10.1136/hrt.2007.127480. [DOI] [PubMed] [Google Scholar]
- 17.Delaney EK, Murchie P, Lee AJ, Ritchie LD, Campbell NC. Secondary prevention clinics for coronary heart disease: a 10-year follow-up of randomised controlled trial in primary care. Heart. 2008;94:1419–1423. doi: 10.1136/hrt.2007.126144. [DOI] [PubMed] [Google Scholar]
- 18.Raljević E, Dilić M, čerkez F. Epidemiologija kardiovaskularnih bolesti. [Epidemiology of cardiovascular diseases] In: Raljević E, Dilić M, čerkez F, editors. Prevencija kardiovaskularnih bolesti. [Prevention of cardiovascular diseases]. Association of Cardiologist of Bosnia and Herzegovina. Sarajevo: 2003. pp. 11–31. [Google Scholar]
- 19.O’Conor GT, Buring JE, Yusuf S, Goldhaber SZ, Olmstead EM, Paffenbarger RS, Jr, et al. An overview of randomised trials of rehabilitation with exercise after myocardial infarction. Circulation. 1989;80:234–244. doi: 10.1161/01.cir.80.2.234. [DOI] [PubMed] [Google Scholar]


