Abstract
Introduction:
Counting of fetal movement (FM) during pregnancy is believed to be a method by which a woman estimates the fetal well-being. In 2015, it was estimated that 2.6 million babies had died in utero. A percentage of 30-55% of women who experience an episode of reduced fetal movement (RFM) within a week may face stillbirth.
Aim:
The aim of this review was to assess the impact of reduced fetal movements and of educational interventions on maternal counting of fetal movements on perinatal mortality, perinatal outcome and mode of delivery.
Methods:
A search of electronic databases was conducted for detecting studies that examine the coincidence of reduced fetal movements (RFM) in combination with stillbirth and perinatal morbidity.
Results:
The findings of this review suggest that there is an association between the incidence of stillbirth and the experience of alterations in fetal movements’ quantity and quality in the preceding weeks. Interventions on fetal movement counting, concerning both the number and the density of fetal movements, may reduce the adverse perinatal outcomes to an extent, after informing and making aware of the pregnant women for their meaning.
Conclusion:
Maternity care professionals should: a) inform pregnant women about the importance of FM counting, b) encourage pregnant women to be familiarized on the recognition of theirs’ baby normal pattern of fetal movements and c) alarm women when this pattern changes. Care professionals should emphasize that counting of fetal movements is not related only to movements’ quantity (number) but also to movements’ quality (density).
Keywords: fetal movement, reduced fetal movement, fetal movement counting, stillbirth, perinatal mortality
1. INTRODUCTION
Counting of fetal movement (FM) during pregnancy is a method by which a woman estimates the fetal well-being (1) without the need of a clinician or equipment. Women start feeling their baby’s movements between 16th and 20th weeks of pregnancy with primiparous women feeling their baby’s movements usually at 18 to 20 weeks and multiparous at 16 to 18 weeks (2). The number of movements has the tendency to increase up until the 32nd week of gestation (3, 4, 5), and since then, they plateau until term but do not decrease. As pregnancy advances, the nature of fetal movements may change due to the neurological development and maturation of the fetus (6). As fetal movement, is defined to be, any kick, flutter, swish or roll the mother senses (7). Fetal movements may be considered as a proof of the integrity of the musculoskeletal and central nervous systems. A normal fetus is capable of physical movement, and during the day has many periods of both rest and sleep.
Various methods have been described for counting and assessing the fetal movements by the pregnant woman. In the count-to-ten method (Cardiff method), ten fetal movements must be counted for a specific period of time every day. If there are less than 10 movements in 12 hours or if it is needed more time than the usual for the movements to happen, it may be a sign of fetal compromise (8). In the Sadovsky method, the woman is counting fetal movements three times a day after meals (9). In the fixed period method, there is counting of fetal movement for 1 hour every day or every six hours if the situation is anticipated to change (10).
In most cases, fetal movements are estimated by mothers’ perception and many physical and social factors may influence maternal perception of fetal movements. Many studies suggest that reduced sensation of fetal movements on behalf of the mother is associated with increased maternal BMI, anterior placenta placement, mother’s mobility, mother’s exercise pattern, fetal anterior position and higher birthweight infant (11,12,13). In addition, factors that affect maternal perception of reduced fetal movements (RFM) were advanced aged mothers and employed more than 8 hours per day mothers, due to low serotonin and high catecholamine levels (14, 15, 16). Another factor affecting mother’s perception of FM is the duration, regularity and sharpness of her exercise patterns, with mild to moderate exercises increasing her perception (14). Maternal exercise increases cortisol levels which is associated with increased fetal movements (17, 18). A supine position also reduces fetal movement sensation (14).
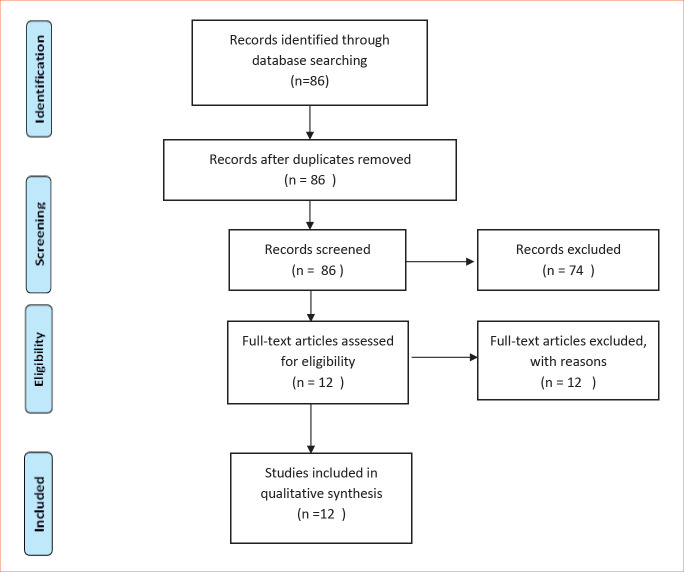
Figure 1. Flow Chart .
Reduced fetal movements are associated with low amniotic fluid volume, smoking, alcohol, drug consumption (benzodiazepins, opiods, bethadone), sedatives, corticosteroids, fetal sleep cycles, fetal compromise (12), fetal growth restriction and placental abnormalities (19, 20, 21). In addition, uterus artery Pulsatility Index (PI) at 19-23 weeks of gestation is strongly associated with the presence of RFM and subsequently with stillbirth (22). On the contrary, in a study of 21 women recorded FM under 30min of ultrasound surveillance showed that there was no significant relationship between the perception of FM and placental site, amniotic fluid index, BMI or parity (23). Furthermore, according to a recent study by Bradford et al. there are data showing that there is clear and significant association between fetal movements and time of day. These data indicate a clear diurnal pattern characterised by an increasing likelihood of strong fetal movement as the day advances and a corresponding decrease in the likelihood of quiet movements during the night (24).
Absence in fetal movements occurs during fetal sleep that usually last 20-40 min up until 90 min in normal full-term fetuses (25). Kantrowitz-Gordon et al. considered that mother’s perception is influenced not only by physical factors (e.g. advanced pregnancy) but also by social and psychological factors such as, educational level, maternal-fetal attachment, anxiety during pregnancy, and mindfulness (mindful awareness of fetal movement) (26). According to Winje et al. pregnancies with RFM should be taken under consideration since perinatal factors (such as maternal BMI, placental site and gestational age) can only explain a small part of the differentiation of fetal movement patterns (27). In 2015, it was estimated that 2,6 million babies had died in utero (28), and a percentage of 30-55% of women who experienced an episode of reduced fetal movement (RFM) within a week may face stillbirth (29, 30).
Therefore, there is a need for evidence based information in order to promote better health management during pregnancy as concerns the monitoring and meaning of FM during pregnancy and especially during the last trimester. It is important to establish whether, in practice, benefits outweigh risks or vice versa, both as a routine procedure and in selected high-risk pregnancies.
2. AIM
The aim of this review was to assess the impact of reduced fetal movements and of educational interventions on maternal counting of fetal movements on perinatal mortality, perinatal outcome and mode of delivery.
3. METHODS
A systematic search of electronic databases concerning medical care (PubMed, Medline, Cochrane, CINAHL and Scopus) was held, at the beginning of 2020 in order to detect studies, including randomized controlled trials (RCTs), cohort studies and case-control studies, that examined the association between reduced fetal movements and stillbirth and perinatal morbidity which were published in English language between 2010 and 2020. The population of interest was pregnant women with singleton pregnancies that either experienced reduced fetal movements or were trained about fetal movement counting. The terms that were used were fetal movements, reduced FM, perinatal outcome, low Apgar Score, stillbirth.
Additional methods of searching included the search of reference list of articles selected from the primary search, in order to identify studies that might not have been presented at the initial search.
Data collection and analysis was conducted by two authors simultaneously. The initial search generated 86 titles. Titles and abstracts were examined for relevance to the review objective. After the assessment of the titles and abstracts, 74 references were excluded because they were apparently not relevant to the objective of the study. From the remaining 12 studies, only relational data were included, which also investigated other issues such as maternal perception of fetal movements.
4. RESULTS
Reduced fetal movement and perinatal outcomes
Fetal movements have been a measure to estimate fetal well being. Studies presenting in (Table 1) assessed the relationship between reduced fetal movements and perinatal outcome.
Table 1. Studies examining the association between reduced fetal movements and perinatal and neonatal outcome.
| Study | Counrty | Study Design | Sample Size | Outcome Investigated | Results | ||
| Saastad et al.,2011 (39) | Norway | Randomized Controlled Trial (RCT) | Intervention group: 433, Control group: 532 >28w |
Estimation of the effect of FM counting on identification of Fetal pathology and pregnancy outcome | FM counting seemed to recognize clinically important changes in fetal status | Improved identification of FGR and low Apgar Scores No stillbirths was found |
|
| Dutton et al., 2012 (36) | UK, Norway | Cohort Study | 305 women with RFM | Association between RFM and perinatal and neonatal outcome | RFM associated with increased incidence of pregnancy complications including small for gestational age infants, fetal growth retardations and fetal hypoxia | Small for gestational age term and preterm fetus 19,1% NICU admission 0,7% No stillbirth was found |
|
| Nor Azlin et al., 2015 (37) | Malaysia | Retrospective study | 230 women with RFM | maternal and fetal outcomes of women who present primarily with reduced fetal movements | IOL 45,7% CS 15% Low birth weight <2,5 kg 6,9% NICU admission 3,5% |
No stillbirths | |
| Warland et al., 2015 (29) | Australia, New Zeland, UK, USA | Cohort Study- internet Survey | 1714 women with stillbirth >28 w |
Symptoms and experiences before stillbirth. Association between RFM and stillbirth |
RFM are associated with stillbirths | May appear a period of increased FM, a “gut” feeling sth is wrong | |
| McCarthy et al., 2016 (35) | Ireland | Case control study | Case group: 275 women with RFM Control group: 265 women with no RFM >28 w |
Association between RFM and stillbirth | RFM group: stillbirth rate 14,5 /1000 (1,5%) Control group: stillbirth 0/1000 |
RFM group: increased incidence of induction of labor in comparison to control group | |
| Delaram et al., 2016 (40) | Sahrekord, Iran | Randomized Controlled Trial (RCT) | Intervention group: 100, Control group: 108 208 28w |
Effect of FM counting on pregnancy outcome | No significant difference on pregnancy outcomes. | No cases of premature labour, intrauterine growth retardation and fetal death in the two groups. No difference in delivery mode. | |
| Heazell et al., 2017 (32) | Case control | Case group: 153 women with late stillbirth, Control group: 480 women with an ongoing pregnancy >28 w |
Women’s experiences of FM in relation to stillbirth | Alterations in FM were associated with increased risk of stillbirth | Increased risk of stillbirth: less likely to check FM during pregnancy, significant reduction of FM, a single episode of excessive FM, less likely to fell FM during bedtime on the last night | ||
| Decreased risk of stillbirth: increased frequency/strength, sometimes vigorous movements | |||||||
| Heazell et al., 2018 (33) | UK | Case control | Case group: 291 women with late stillbirth, Control group: 733 women with an ongoing pregnancy >28 |
Maternally perceived FM in association with late stillbirth | Increased strength and daily fetal hiccups in the last 2 weeks associate with a decreased incidence of stillbirth | Increased risk of stillbirth: decrease in strength or frequency of FM in last 2 weeks (specially if it was a recurrent phenomenon), single episode of fetal vigorous activity | |
| Decreased risk of stillbirth: increasing strength/frequency and/or in the last two weeks, fetal hiccups | |||||||
| Norman et al., 2018 (38) | UK Ireland |
Stepped wedge cluster-randomized trial | Intervention group: 227.860, Control group: 157.692 >24 w |
Association between increased women’s awareness of RFM and stillbirth incidence | No significant effect on incidence of stillbirth | Increased IOL, CS, admission in the NICU >48 h, | |
| Identified SGA fetuses | |||||||
| Akselssona et al., 2019 (41) | Sweden | Prospective study | 2592 >28w |
Awareness on FM and pregnancy outcome | Daily observation on FM- fewer admissions to NNU | Increased likelihood of CS before onset of labor | |
| Bradford et al., 2019 (49) | New Zealand | Case-control study | Case group: 164 women with stillbirth Control group: 569 women with normal pregnancy |
Fetal movement quality and association with stillbirth | Women with stillbirth were more likely to experience decrease in FM strength and frequency | Decreased risk of stillbirth among women referring more “vigorous” fetuses than usual, daily fetal hiccups, increased length of FM clusters | |
| Increased risk of stillbirth among women referring decreased frequency of FM, quiet/light movements in the evening | |||||||
| Sterpu et al., 2020 (34) | Stockholm, Sweden | Retrospective Cohort study | 3243 women referring RFM >22w |
Women’s experiences of FM in relation to stillbirth | Highest risk of poor neonatal outcome in small for gestational age fetuses with RFM 11,8% elective CS Recurrent episodes of RFM associated with higher rates of induction of labour | Fivefold higher risk in stillbirth among RFM women than normal population SGA fetuses have significantly higher stillbirth percentange, Low AS<7 at 5min |
|
In this review, studies that are included can be divided into two kinds. The first kind concern studies that examined the association between perinatal outcome of pregnancies that have already experienced reduced fetal movements and the second kind concern studies that examined the association between the perinatal outcome of pregnancies in which women were provided with information and education of the meaning and counting of fetal movements.
The primary outcome measure was the incidence of stillbirth (babies delivered without signs of life after less than 24 weeks’ gestation, or, if gestation was unknown, weighing 500 g or more). Other perinatal outcomes were fetal growth restriction, low Apgar Score, admission in the NICU, type of labour.
As concerns the stillbirth incidence, six studies assessed the relationship between women’s reporting reduced fetal movements and stillbirth and all of them found a positive correlation between reduced fetal movements and stillbirth (29, 31-35). Therefore, the findings of these studies suggest that there is an association between the incidence of stillbirth and the experience of alterations in fetal movements’ quantity and quality in the preceding weeks.
Tne study assessed the relationship between reduced fetal movements and variables of poor perinatal outcome (e.g. small for gestational age) (36). Prospective cohort study by Dutton et al. (36) conducted in 2012 included 303 pregnant women presenting with RFM after 28 gestational weeks. They found that 22.1% of these pregnancies ended in a poor perinatal outcome after RFM. The most common complication was small-for-gestational age term and preterm infants (19.1%). It was also found that 4.1% of neonates out of 303 pregnancies with a complain of reduced fetal movement weighed <10th centile, and 0,7% had to be admitted in the NICU.There were no stillbirths in this cohort, but 4 participants underwent emergency Caesarean section for pathological CTG and intrauterine asphyxia was confirmed at delivery by acidaemia in the umbilical arterial sample.
In a study by Nor Azlin et al., (37) was examined the pregnancy outcomes after a complaint of RFM in a population of 230 women. It was found that 6,9% of babies were born with a low birth weight <2,5 kg, 3,5% of babies admitted in NICU and there were no stillbirths in this study (37).
Warland et al. (29) conducted an international internet survey, including 1.714 women who experienced a late stillbirth and noted that a percentage of 30-55% of women who experienced an episode of reduced fetal movement (RFM) within a week may face stillbirth. Also it was founded that a 30,5% of the women who participated in the survey reported that they experienced significantly less fetal movements before stillbirth (29).
Mc Carthy et al. (35) in a case control study including 275 women presenting in the emergency department with a complain of reduced fetal movements, compared them with a control group consisting of 265 women with no complain of RFM. They found an incidence of 1,5% stillbirth and an incidence of 10.6% of NICU admission in the group of women with RFM compared to 7,2% in the control group of pregnancies.
The case control study by Heazell et al., conducted in 2017, women who experienced a stillbirth (n=153) were less likely to check on fetal movements during pregnancy, were less likely to be told to do so by a health professional and were more likely to experience a reduction in number of FM during the preceding two weeks or to have a singular episode of excessive fetal movements described as “wild” or “frantic” than women who had a live birth (n=480) (32). On another case-control study by Heazell et al. in 2018, investigating the association between maternally perceived fetal movements (frequency, intensity, strength of movements, hiccups) and fetal stillbirth by comparing the perception of fetal movements in women who experienced a late stillbirth (n=291) to a control group of women (n=733) at similar gestation, who had a live baby. They found that an increased strength or frequency of movements was correlated with a lower risk of stillbirth in contrast with an unchanged volume of them. They also found that a decrease in the strength or frequency of fetal movements was associated with an increased risk of late stillbirth particularly if this was a recurrent phenomenon. Additionally, it was noted that a single episode of vigorous fetal activity was also associated with an increased risk of stillbirth. The daily presence of fetal hiccups appeared to protect over stillbirth (33).
Bradford et al. (31) examined the association between fetal movements’ quality and pattern to late stillbirth in a case-control study. They concluded that changes in the fetal movement pattern such as a decrease in the strength and frequency of fetal movements and a fetal calmness during the night hours were more likely to be experienced from women with stillbirths (31).
Sterpu et al, (34) performed a retrospective cohort study and investigated the outcome of 3243 pregnancies presenting with reduced fetal movements. They concluded that the risk of stillbirth in pregnancies with reduced fetal movements is five times higher than in normal pregnancies (34). They also concluded that in this sample of women there was a higher frequency of low Apgar Score <7 at 5min: (3,3%), a higher frequency of low pH in umbilical cord blood (2,9%) and more babies had to be admitted in the NICU (3,9%). Additionally SGA fetuses had a significantly higher risk of stillbirth than normal fetuses (34).
Four studies examined the effect of training interventions for increased women’s awareness towards fetal movements on the incidence of stillbirths and other perinatal outcomes (38-41).
Study by Akselssona et al. (41), in 2019 including 2592 women, found that women who were using a counting method daily in order to focus on fetal movements were less likely to have their baby be admitted in the NICU in comparison to the control group.
A stepped wedge, cluster randomized trial conducted in 2018 by Norman et al, with a sample size of 409.175 women (157.692 deliveries during the control period, 23.623 deliveries in the washout period, and 227.860 deliveries in the intervention period) in 33 hospitals, examined whether the introduction of a care package for awareness of reduced fetal movements (RFM) would alter the incidence of stillbirth. It was found that the incidence of stillbirth was 4·40 per 1000 births during the control period and 4·06 per 1000 births in the intervention period and they concluded that there was not a considerable effect of the introduction of care package on the incidence of stillbirth nor on perinatal mortality (38). Furthermore it has been also found that fetuses during the intervention period had a prolonged stay in the NICU (for more than 48 hours) (38).
Saastad et al, conducted a randomized controlled trial in order to estimate the effect of fetal movement counting. Women in the intervention group used a modified count-to-ten method to estimate fetal movements, and found that they had a better recognition of FGR fetuses and a decrease in fetuses with very low Apgar Score in birth (39).
The randomized controlled trial by Delaram et al. (40) consisted of 208 women and assessed the effect of fetal movement counting on pregnancy outcomes. Pregnancy outcome was similar in the two groups of fetal movement counting and control. There were no cases of premature labour, intrauterine growth retardation and fetal death in the two groups.
Reduced fetal movements and Type of Labour.
Management of pregnancies with RFM is a controversial side of this incidence. Six studies on (Table 1) have found an association between reduced fetal movements and type of birth (34, 35, 37, 38, 40, 41).
Three studies assessed the relationship between women’s reporting reduced fetal movements and delivery mode and all of them found a positive correlation between reduced fetal movements and increased incidence of induction of labour and caesarean section (34, 35, 37).
In the study by Sterpu et al. (34) it was found that 64.8% of the women presenting with RFM had spontaneous labor, 23.5% underwent an induction of labor and 11.8% had elective CS before onset of labor. Sterpu et al found that women with repeated incidents of RFM had statistically significant higher incidence of induction of labor than women with a single episode of RFM (30.9% vs. 21.9%) (34).
In the McCarthy (35) study, women in the RFM group were less likely to have a spontaneous onset of labour, and more likely to undergo an induction of labour than the control group. An increase in the incidence of CS has been also found, which was not very significant (32.6% to 29.8%) (35).
In the study of Nor Azli et al. (37) women, who had a daily and structured approach to awareness of fetal movements, were more likely to have a caesarean section and an induction of labour as compared with women who used a non-structured method daily.
Three of these studies examined the effect of training interventions for increased women’s awareness towards fetal movements on the incidence of delivery mode (38, 40, 41).
Study by Akselssona et al. (41), in 2019, found that women who were using a counting method daily in order to focus on fetal movements were more likely to have a cesarean section in comparison to the control group.
The cluster randomized trial conducted by Norman et al (38) examined whether the introduction of a care package for awareness of reduced fetal movements (RFM) would alter the mode of delivery. It was found that the rates of elective and emergency caesarean sections were the same during the control period and the intervention period. In contrary, they found that the rate of induction of labour was higher during the intervention period (40.7%) than in the control period (35.8%).
The randomized controlled trial by Delaram et al. (40) assessed the effect of fetal movement counting on delivery mode. Delivery mode was similar in the two groups of fetal movement counting and control.
The findings of these studies suggest that there is an association between the incidence of induction of labour, caesarean sections and the experience of alterations in fetal movements’ quantity and quality in the preceding weeks.
5. DISCUSSION
The aim of this review was to assess the impact of reduced fetal movements and of educational interventions of maternal counting of fetal movements on perinatal mortality, perinatal outcome and mode of delivery.
During our review research it was found that most of the published studies examined the association between fetal movements and perinatal outcomes, through two different approaches. The first approach was to examine the perinatal outcome in women who already had experienced reduced fetal movements in comparison to women with normal fetal movements. The second approach was to estimate the difference of perinatal outcome between women who received education and information regarding the meaning and counting of fetal movements during pregnancy and women with no educational training.
As concerns the stillbirth incidence, six studies assessed the relationship between women’s reporting reduced fetal movements and stillbirth and all of them found a positive correlation between reduced fetal movements and stillbirth (29, 31-35). Three studies assessed the relationship between women’s reporting reduced fetal movements and delivery mode and all of them found a positive correlation between reduced fetal movements and increased incidence of induction of labour and caesarean section (34, 35, 37). Four studies examined the effect of training interventions for increased women’s awareness towards fetal movements on the incidence of stillbirths and on other perinatal outcomes (38-41) and two of them concluded that increased women’s awareness towards fetal movements associated with lower likelihood of baby’s NICU admission (41), bettter recognition of FGR fetuses and a decrease in fetuses with very low Apgar Score in birth (39). Three of these studies examined the effect of training interventions for increased women’s awareness towards fetal movements on the incidence of delivery mode (38, 40, 41) and one study of them found that women who were using a counting method daily in order to focus on fetal movements were more likely to have a cesarean section (41) and induction of labour (38) in comparison to the control group.
Therefore, the findings of this review suggest that there is an association between the incidence of stillbirth and the experience of alterations in fetal movements’ quantity and quality in the preceding weeks. These findings are in agreement with findings of previous studies. In a population based study which was conducted by Koshida et al. (44) identified major causes of preventable stillbirths, including delayed visits of pregnant women with decreased fetal movements to clinics or hospitals. Based on the results of their study, it was concluded that education for pregnant women is required as well as the necessity of improving obstetric care to prevent stillbirths (44). Our review findings are in agreement with findings of a previous review. In a previous systematic review by Winje et al., (45) it was depicted that women that used fetal movement counting once or more per week had less stillbirths by 21%, than control women, difference which was not statistically significant. However indirect evidence of this review recommends that fetal movement counting interference improved perinatal outcome, since the occurrence of stillbirth decreased in the RFM group of women during the intervention period (45). Additionally studies that included systematically counting of fetal movements (n: 11.069) found a statistically significant reduction in the range of stillbirth (45).
However, it should be noted that two studies examined the effect of training interventions for increased women’s awareness towards fetal movements on the incidence of stillbirths and other perinatal outcomes (38-41) and found that increased women’s awareness towards fetal movements was not associated with reduced stillbirth incidence of improved perinatal outcome (38, 40). The AFFIRM study which included 409.175 population found that, there was not considerable effect during the intervention period on the incidence of stillbirth and perinatal mortality (38). The intervention package included e-learning education for the clinical staff, an informative leaflet for pregnant women given around 20 weeks of gestation and a management plan for high risk pregnancies after 24 weeks of gestation, presented with RFM (38). Although in this trial awareness of pregnant women and the intervention of clinicians was not estimated. It should be pointed that these results should only be interpreted under the scope of investigating the efficacy of a training intervention on women’s awareness and ability to correctly report and count fetal movements. The findings of these studies should not be interpreted under the scope of drawing conclusions on the association between reduced fetal movements and stillbirth. It should become clear that the value of fetal movement counting by the women should not be underestimated because the findings of these studies did not demonstrate that increased awareness did not led to increased stillbirths. Flenady et al. supported that discouraging the promotion of awareness of fetal movements should be avoided and the detection of an approach which combines multiple methods to prevent stillbirth is essential (46).
However, it should be clear that a period of decreased fetal movements commonly precedes fetal death, but the absence of perceived fetal movements does not necessarily indicate fetal death or fetal compromise (42). It should be also noted that despite the evidence demonstrating a strong association between RFM and stillbirth, the majority of women reporting RFM will have a healthy baby (43). According to Holm Tveit et al. approximately 10% - 15% of women of late pregnancy will experience symptoms of RFM but the percentage of fetal death is much lower than 10%-15% (43).
Fetal movement counting is simple, economical, can be done by the woman without any equipment. However, it may cause unnecessary stress to the pregnant women and it may lead to increased antenatal admissions and medical interventions for excluding fetal compromise (42). Koshida et al. supported that educating women about the normal range and duration of fetal movements, would improve perinatal outcome in late pregnancy, saying that 10 fetal movements, typically should take place within 30 minutes (13). Nevertheless Warland et al., suggest that count to ten alarm limits should not be taken under consideration since every pregnancy has its own patterns and every woman should be familiarized with her own baby’s characteristics (47, 48).
Bradford et al, in a cross-sectional study in 2019, examining maternal perception of fetal movement in pregnancies with normal outcome, found that the strength of fetal movements in the last trimester is accretive, with frequent presence of fetal hiccup and the revealing of a diurnal pattern of fetal movements (24). A change in the quality of fetal movements should be taken more into consideration than any arithmetical issue might occur. Kicking and jolting may alter to pushing and rolling and according to Bradford and Maude, health providers should inform pregnant women about the increasing strength and evening movements throughout pregnancy (49). Therefore, WHO recommends the daily surveillance of fetal movements, using any kind of method, as an effort to make pregnant women and health care professionals aware of the importance of fetal movements, especially in late pregnancy (46).
6. CONCLUSION
RFM is a frequently occurring event during antenatal period, associated with different perinatal outcomes, such as stillbirth, inducing of labour, cesarean section and admission to NICU. It is important and necessary the research about RFM and perinatal outcome to be continued as also education of pregnant women in the identification of FM types and training of health care professionals on how to manage women which present with RFM. RFM is an important part of risk assessment in antenatal care, and it is clear that hospitals should examine the prevalence and management of RFM within their services. Maternity care professionals should inform pregnant women about the importance of maternal recognition of the baby’s normal pattern of number and density of fetal movements and alarm women when this pattern changes. Care professionals should inform pregnant women that counting the frequency of fetal movements is only one part of assessment of fetal well being. It is also important for women to appraise and report changes in strength, density and pattern of movements.
Author’s contribution:
KG contributing substantially to the conception and the design of the study. KG contributed substantially to the interpretation of the data, the preparation of the manuscript after revising it critically for important intellectual content. KB contributed in the acquisition, analysis and interpretation of data for the study and in drafting the manuscript. Both author gave final approval of the version to be published and final proof reading was made by the second author.
Conflict of interest:
None declared.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Heazell AE, Froen JF. Methods of fetal movement counting and the detection of fetal compromise. J Obstet Gynaecol. 2008;28:147–154. doi: 10.1080/01443610801912618. [DOI] [PubMed] [Google Scholar]
- 2.Cronje HS, Grobler CJF, Visser AA. Pretoria: J. A. van Schaik Publishers; 1996. Obstetrics in Southern Africa. [Google Scholar]
- 3.Natale R, Nasello-Paterson C, Turliuk R. Longitudinal measurements of fetal breathing, body movements, heart rate, and heart rate accelerations and decelerations at 24 to 32 weeks of gestation. Am J Obstet Gynecol. 1985;151:256–263. doi: 10.1016/0002-9378(85)90022-5. [DOI] [PubMed] [Google Scholar]
- 4.Eller DP, Stramm SL, Newman RB. The effect of maternal intravenous glucose administration on fetal activity. Am J Obstet Gynecol. 1992;167:1071–1074. doi: 10.1016/s0002-9378(12)80040-8. [DOI] [PubMed] [Google Scholar]
- 5.D’Elia A, Pighetti M, Moccia G, Santangelo N. Spontaneous motor activity in normal fetuses. Early Hum Dev. 2001;65:139–147. doi: 10.1016/s0378-3782(01)00224-9. [DOI] [PubMed] [Google Scholar]
- 6.Tveit JV, Saastad E, Bordahl PE, Stray-Pedersen B, FrØen JF. The epidemiology of decreased fetal movements. Proceedings of the Norwegian Perinatal Society Conference; Oslo, Norway. 2006. [Google Scholar]
- 7.Neldam S. Fetal movements as an indicator of fetal well-being. Dan Med Bull. 1983;30:274–278. [PubMed] [Google Scholar]
- 8.Bennet VR, Brown LK. Edinburgh: Churchill Livingstone; 1999. Myles Textbook for Midwives. [Google Scholar]
- 9.Boog G. Le comptage maternel des mouvements foetaux. Une méthode simple et sûre de surveillance de la grossesse (Maternal determination of fetal movements. A sure and simple method of monitoring the pregnancy) Rev Fr Gynecol Obstet. 1988;83(11):693–695. [PubMed] [Google Scholar]
- 10.Freda MC, Mikhail M, Mazloom E, Polizzoto R, Damus K, Merkatz I. Fetal movement counting: which method? MCN. The American Journal of Maternal Child Nursing. 1993;18:314–321. doi: 10.1097/00005721-199311000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Mohr Sasson A, Tsur A, Kalter A, Weissmann Brenner A, Gindes L, Weisz B. Reduced fetal movement: factors affecting maternal perception. J Matern Fetal Neonatal Med. 2016;29(8):1318–1321. doi: 10.3109/14767058.2015.1047335. [DOI] [PubMed] [Google Scholar]
- 12.Tveit JVH, Saastad E, Stray-Pedersen B, BØrdahl Per E, FrØen JF. Concerns for decreased foetal movements in uncomplicated pregnancies - Increased risk of foetal growth restriction and stillbirth among women being overweight, advanced age or smoking. Journal of Maternal-Fetal and Neonatal Medicine. 2010;23(10):1129–1135. doi: 10.3109/14767050903511578. [DOI] [PubMed] [Google Scholar]
- 13.Koshida S, Ono T, Tsuji S, Murakami T, Arima H, Takahashi K. Fetal movement frequency and the effect of associated perinatal factors: Multicenter study. Women Birth. 2019;32(2):127–130. doi: 10.1016/j.wombi.2018.06.010. [DOI] [PubMed] [Google Scholar]
- 14.Sheikh M, Hantoushzadeh S, Shariat M. Maternal perception of decreased fetal movements from maternal and fetal perspectives, a cohort study. BMC Pregnancy and Childbirth. 2014;14:286. doi: 10.1186/1471-2393-14-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haque Z, Haleem DJ. Role of peripheral serotonin in stress induced obesity. Medical Channel. 2011;17:5–10. [Google Scholar]
- 16.Katz VL, Jenkins T, Haley L, Bowes WA. Jr: Catecholamine levels in pregnant physicians and nurses: a pilot study of stress and pregnancy. Obstet Gynecol. 1991;77:338–342. [PubMed] [Google Scholar]
- 17.DiPietro JA, Costigan KA, Gurewitsch ED. Fetal response to induced maternal stress. Early Hum Dev. 2003;74:125–138. doi: 10.1016/j.earlhumdev.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 18.DiPietro JA, Kivlighan KT, Costigan KA, Laudenslager ML. Fetal motor activity and maternal cortisol. Dev Psychobiol. 2009;51:505–512. doi: 10.1002/dev.20389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Warrander LK, Heazell AE. Identifying placental dysfunction in women with reduced fetal movements can be used to predict patients at increased risk of pregnancy complications. Med Hypotheses. 2011;76(1):17–20. doi: 10.1016/j.mehy.2010.08.020. [DOI] [PubMed] [Google Scholar]
- 20.Warrander LK, Batra G, Bernatavicius G, et al. Maternal perception of reduced fetal movements is associated with altered placental structure and function. PLoS One. 2012;7:e34851. doi: 10.1371/journal.pone.0034851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Winje BA, Roald B, Kristensen NP, Froen JF. Placental pathology in pregnancies with maternally perceived decreased fetal movement - a population-based nested case-cohort study. PLoS One. 2012;7:e39259. doi: 10.1371/journal.pone.0039259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pagani G, D’antonio F, Khalil A, Akolekar R, Papageorghiou A, Bhide A, Thilaganathan B. Association Between Reduced Fetal Movements At Term And Abnormal Uterine Artery Doppler Indices. Ultrasound Obstet Gynecol. 2014;43:548–552. doi: 10.1002/uog.13220. [DOI] [PubMed] [Google Scholar]
- 23.Brown R, Higgins LE, Johnstone ED, Wijekoon JH, Heazell AEP. Maternal perception of fetal movements in late pregnancy is affected by type and duration of fetal movement. The Journal of Maternal-Fetal & Neonatal Medicine. 2015;29(13):2145–2150. doi: 10.3109/14767058.2015.1077509. [DOI] [PubMed] [Google Scholar]
- 24.Bradford BF, Cronin RS, McKinlay CJD, Thompson JMD, Mitchell EA, Stone PR, et al. A diurnal fetal movement pattern: Findings from a cross-sectional study of maternally perceived fetal movements in the third trimester of pregnancy. PLoS One. 2019;14(6):e0217583. doi: 10.1371/journal.pone.0217583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Velazquez MD, Rayburn WF. Antenatal evaluation of the fetus using fetal movement monitoring. Clin Obstet Gynecol. 2002;45:993–1004. doi: 10.1097/00003081-200212000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Kantrowitz-Gordon I, Cunningham E, Reynolds N. Measurement of Maternal Mindful Awareness of Fetal Movement. J Midwifery Womens Health. 2019;64:604–612. doi: 10.1111/jmwh.12981. [DOI] [PubMed] [Google Scholar]
- 27.Winje BA, RØislien J, FrØen JF. Temporal patterns in count-to-ten fetal movement charts and their associations with pregnancy characteristics: a prospective cohort study. BMC Pregnancy and Childbirth. 2012;12:124. doi: 10.1186/1471-2393-12-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.De Bernis L, Kinney MV, Stones W, Hoope-Bender P, Vivio D, Hopkins Leisher S, et al. Stillbirths: ending preventable deaths by 2030. Lancet. 2016;387:703–716. doi: 10.1016/S0140-6736(15)00954-X. [DOI] [PubMed] [Google Scholar]
- 29.Warland J, O’Brien LM, Heazell AE, Mitchell EA. For the Stillbirth Consortium. An international internet survey of the experiences of 1,714 mothers with a late stillbirth: the STARS cohort study. BMC Pregnancy Childbirth. 2015;15:172. doi: 10.1186/s12884-015-0602-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Efkarpidis S, Alexopoulos E, Kean L, et al. Case-control study of factors associated with intrauterine fetal deaths. MedGenMed. 2004;6:53. [PMC free article] [PubMed] [Google Scholar]
- 31.Bradford BF, Cronin RS, McCowan LME, McKinlay CJD, Mitchell EA, Thompson JMD. Association between maternally perceived quality and pattern of fetal movements and late stillbirth. Scientific Reports. 2019;9:9815. doi: 10.1038/s41598-019-46323-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heazell AEP, Warland J, Tomasina S, Coomarasamy C, Budd J, Mitchell EA, O’Brien LM. Stillbirth is associated with perceived alterations in fetal activity – findings from an international case control study. BMC Pregnancy and Childbirth. 2017;17:369. doi: 10.1186/s12884-017-1555-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heazell AEP, Budd J, Li M, Cronin R, Bradford B, McCowan LME. Alterations in maternally perceived fetal movement and their association with late stillbirth: findings from the Midland and North of England stillbirth: case–control study. BMJ Open. 2018;8(7):e020031. doi: 10.1136/bmjopen-2017-020031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sterpu I, Pilo C, Koistinen IS, Lindqvist PG, Gemzell-Danielsson K, Itzel EW. Risk factors for poor neonatal outcome in pregnancies with decreased fetal movements. Acta Obstet Gynecol Scand. 2020;00:1–8. doi: 10.1111/aogs.13827. [DOI] [PubMed] [Google Scholar]
- 35.McCarthy CM, Meaney S, O’Donoghue K. Perinatal outcomes of reduced fetal movements: a cohort study. BMC Pregnancy and Childbirth. 2016;16:169. doi: 10.1186/s12884-016-0964-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dutton P, Warrander LK, Roberts SA, Bernatavicius G, Byrd LM, Gaze D, et al. Predictors of poor perinatal outcome following maternal perception of reduced fetal movement - a prospective cohort study. PLoS One. 2012;7(7):e39784. doi: 10.1371/journal.pone.0039784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nor Azlin MI, Maisarah AS, Rahana AR, Nasir Shafiee M, Aqmar Suraya S, Abdul Karim AK, et al. Pregnancy outcomes with a primary complaint of perception of reduced fetal movements. Journal of Obstetrics and Gynaecology. 2015;35:13–15. doi: 10.3109/01443615.2014.930108. [DOI] [PubMed] [Google Scholar]
- 38.Norman JE, Heazell AEP, Rodriguez A, Weir C, Stock SJE, Calderwood CJ, et al. Awareness of fetal movements and care package to reduce fetal mortality (AFFIRM): a stepped wedge,cluster-randomised trial. Lancet. 2018;392:1629–1638. doi: 10.1016/S0140-6736(18)31543-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saastad E, Winje BA, Stray Pedersen B, FrØen JF. Fetal Movement Counting Improved Identification of Fetal Growth Restriction and Perinatal Outcomes - a Multi-Centre, Randomized, Controlled Trial. PLoS One. 2011;6(12):e28482. doi: 10.1371/journal.pone.0028482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Delaram M, Jafarzadeh L. The Effects of Fetal Movement Counting on Pregnancy Outcomes. Journal of Clinical and Diagnostic Research. 2016;10(2):SC22–SC24. doi: 10.7860/JCDR/2016/16808.7296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Akselsson A, Lindgrenb H, Georgssonc S, Warlandd J, Petterssone K, Radestadf I. Daily structured approach to awareness of fetal movements and pregnancy outcome – a prospective study. Sexual & Reproductive Healthcare. 2019;20:32–37. doi: 10.1016/j.srhc.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 42.Mangesi L, Hofmeyr GJ, Smith V, Smyth RMD. Fetal movement counting for assessment of fetal wellbeing (Review) Cochrane Database of Systematic Reviews. 2015;10 doi: 10.1002/14651858.CD004909.pub3. Art. No.: CD004909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Holm Tveit JV, Saastad E, Stray-Pedersen B, BØrdahl EP, Flenady V, Fretts R, et al. Reduction of late stillbirth with the introduction of fetal movement information and guidelines - a clinical quality improvement. BMC Pregnancy and Childbirth. 2009;9:32. doi: 10.1186/1471-2393-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Koshida S, Ono T, Tsuji S, Murakami T, Arima H, Takahashi K. Excessively delayed maternal reaction after their perception of decreased fetal movements in stillbirths: Population-based study in Japan. Women Birth. 2017;30(6):468–471. doi: 10.1016/j.wombi.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 45.Winje BA, Wojcieszek AM, Gonzalez-Angulo LY, Teoh Z, Norman J, FrØen JF, Flenady V. Interventions to enhance maternal awareness of decreased fetal movement: a systematic review. BJOG. 2016 May;123(6):886–898. doi: 10.1111/1471-0528.13802. [DOI] [PubMed] [Google Scholar]
- 46.Flenady V, Ellwood D, Bradford B, Coory M, Middleton P, Gardener G, et al. Beyond the headlines: Fetal movement awareness is an important stillbirth prevention strategy. Women and Birth. 2019;32(1):1–2. doi: 10.1016/j.wombi.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 47.Warland J, Heazell A, Bradford B, Cronin R, McCowan L. The problem with counting fetal movements. Women Birth. 2020;33(3):e309. doi: 10.1016/j.wombi.2019.06.007. [DOI] [PubMed] [Google Scholar]
- 48.Pollock D, Ziaian T, Pearson E, Cooper M, Warland J. Breaking through the silence in antenatal care: Fetal movement and stillbirth education. Women Birth. 2020;33(1):77–85. doi: 10.1016/j.wombi.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 49.Bradford B, Maude R. Maternal perception of fetal movements in the third trimester: A qualitative description. Women Birth. 2018;31(5):e287–e293. doi: 10.1016/j.wombi.2017.12.007. [DOI] [PubMed] [Google Scholar]
- 50.World Health Organization. WHO recommendation on daily fetal movement counting. 2016. https://extranet.who.int/rhl/topics/preconception-pregnancy-childbirth-and-postpartum-care/antenatal-care/who-recommendation-daily-fetal-movement-counting. published: December.