The COVID-19 (coronavirus disease 2019) pandemic has raised the visibility of serious health-related suffering and increased mortality worldwide, underscoring the critical need for improved access to quality palliative care in all health care delivery settings.1 The palliative nursing role—now, more than ever—is central to alleviating symptomatic and psychosocial distress, as well as achieving patient-identified goals throughout the continuum of serious illness and bereavement care.2,3 Currently, the primary goal of many health and palliative care organizations at national and international levels is palliative care integration throughout all of health care, including timely and safe access to controlled essential medicines and primary and specialist palliative care services in acute, long-term care, and community-based settings, and dignified care at the time surrounding death.4 Nurses, as the largest component of the health care workforce,5 have a professional, ethical mandate to ensure palliative care as a human right, to improve the quality of life for patients, their families, and caregivers.6,7
Nurses ideally deliver both primary and specialty palliative care, as dictated by their level of palliative care training, throughout the spectrum of their practice.8 Nurses deliver primary palliative care with general understanding of care for individuals with serious illness. This includes collaboration with the interdisciplinary team to deliver an integrated approach to care, using basic knowledge to manage pain and symptoms, communications skills to initiate advance care planning discussions and elicit patient and family values and preferences, awareness of community resources, and appropriate triggers for referral to specialist palliative care to establish an individualized care plan.3,9 Specialist palliative nurses with expert knowledge lead collaboration and care coordination to the psychosocial, cultural, and spiritual domains of the patient and family with the resources of the community. This includes management of complex pain and other symptoms, difficult discussions concerning goals of care and ethical dilemmas, and challenging interpersonal dynamics between patients and families.8 COVID-19 has heightened the urgent need for nurses to integrate palliative care into their practice. Critical care nurses are using palliative care skills daily for patients hospitalized with COVID-19.10 All nurses are collaborating to facilitate respectful and dignified care for patients at the end of life, be it at the hospital, hospice, home, or long-term-care setting.2
A foundational component of palliative nursing is the merging of both art and science to strategically relieve the “total pain” of patients.11 Not only do palliative nurses bring expert assessment and skills to the table, but they are also the primary interface between the patient, family, and the health care system.3 Nurses are responsible for using evidence-based clinical judgment and compassion in palliative care delivery. Compassion is an essential element of the patient experience in palliative care12 and is a predictor of patient satisfaction and associated health outcomes.13 In the face of suffering subsequent to COVID-19, the value of compassionate palliative nursing care cannot be overstated.
In response to the global need to support and honor palliative nurses during the pandemic, the End-of-Life Nursing Education Consortium (ELNEC) convened an expert group of palliative nurse specialists to provide evidence-based guidance across a host of palliative care domains. Synthesizing existing evidence with emerging literature regarding COVID-19, the team created an infographic to articulate and illustrate the role of the palliative nurse in the face of this public health crisis. Easy to use, convenient to share, and available to print as a poster, the infographic (Figure) provides information on primary and specialty palliative nursing, identifies explicit clinical and advocacy actions to support the patient and family in myriad care settings, and emphasizes the palliative nurse as essential to care in the COVID-19 era.
FIGURE.
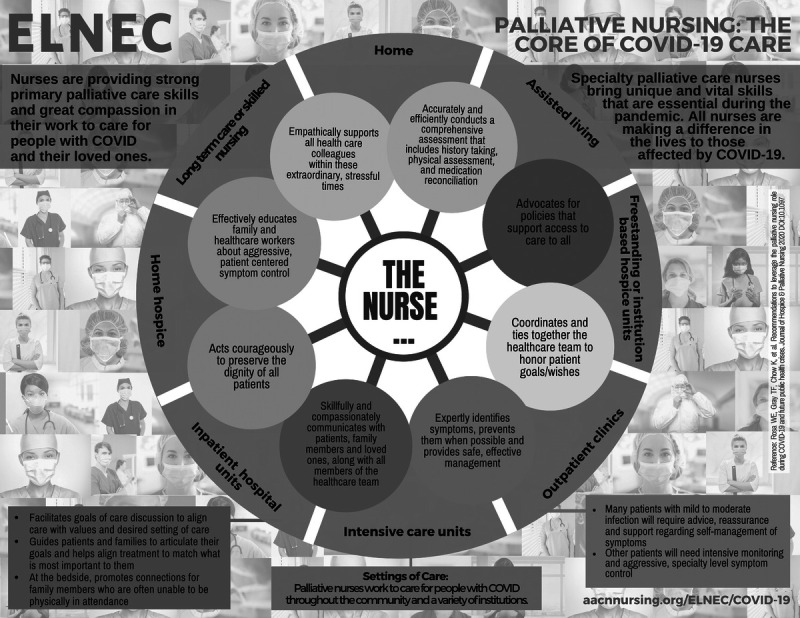
Palliative nursing: the core of COVID-19 care.
CONCLUSION
It is unclear how long the COVID-19 crisis will persist. As virus mitigation strategies and health systems evolve, so do the role and scope of palliative nursing. One thing that does not change is the core and fundamental principle of nursing to improve the living and dying experiences for the seriously ill and their families. Nurses and other professionals are encouraged to visit the ELNEC Support for Nurses During COVID-19 website to obtain additional clinical support tools related to pain and symptom management, grief and bereavement, communication, end-of-life care, primary palliative care, self-care, and cultural and health equity considerations, among other topics (https://www.aacnnursing.org/ELNEC/COVID-19). This infographic celebrates and honors the work of palliative nurses in all settings, in all countries, and throughout the care continuum to alleviate serious health-related suffering for the betterment of society and the patients and family members they serve.
Acknowledgment
The ELNEC COVID-19 team thanks Betty Ferrell, PhD, MA, RN, FAAN, FPCN, CHPN, for her guidance, encouragement, and support in the development of this infographic.
Footnotes
The authors have no conflicts of interest to disclose.
Contributor Information
Dorothy Wholihan, Email: dw57@nyu.edu.
Constance Dahlin, Email: cdahlin3@gmail.com.
William E. Rosa, Email: billyrosa@gmail.com.
Polly Mazanec, Email: pmm@case.edu.
Carol O. Long, Email: carollongphd@gmail.com.
Cheryl Thaxton, Email: thaxca@aol.com.
Kelly Greer, Email: kgreer@coh.org.
References
- 1.Radbruch L, Knaul FM, de Lima L, de Joncheere C, Bhadelia A. The key role of palliative care in response to the COVID-19 tsunami of suffering. Lancet. 2020;395(10235):1467–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosa WE Gray TF Chow K, et al. Recommendations to leverage the palliative nursing role during COVID-19 and future public health crises. J Hosp Palliat Nurs. 2020;22(4):260–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hospice & Palliative Nurses Association Palliative Nursing Scope and Standards. 6th ed Pittsburgh, PA: Hospice & Palliative Nurses Association; 2020. [Google Scholar]
- 4.Knaul FM Farmer PE Krakauer EL, et al. Alleviating the access abyss in palliative care and pain relief—an imperative of universal health coverage: the Lancet Commission Report. Lancet. 2018;391(10128):1391–1454. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization State of the world's nursing: investing in education, jobs and leadership. https://www.who.int/publications/i/item/9789240003279. Published 2020. Accessed September 7, 2020.
- 6.American Nurses Association Code of Ethics With Interpretive Statements. 2nd ed Silver Spring, MD: Nursebooks.org; 2015. [Google Scholar]
- 7.International Council of Nurses ICN position statement: nurses and human rights. International Council of Nurses. https://www.icn.ch/sites/default/files/inline-files/E10_Nurses_Human_Rights%281%29.pdf. Published 2011. Accessed September 7, 2020.
- 8.American Nurses Association and Hospice & Palliative Nurses Association Call for action: nurses lead and transform palliative care. https://www.nursingworld.org/~497158/globalassets/practiceandpolicy/health-policy/palliativecareprofessionalissuespanelcallforaction.pdf. Published 2017. Accessed September 7, 2020.
- 9.National Consensus Project for Quality Palliative Care Clinical Practice Guidelines for Quality Palliative Care. 4th ed Richmond, VA: National Coalition for Hospice and Palliative Care; 2018. [Google Scholar]
- 10.Rosa WE, Ferrell BR, Wiencek C. Increasing critical care nurse engagement of palliative care during the COVID-19 pandemic. Crit Care Nurse. 2020;e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferrell B, Paice JA. Oxford Textbook of Palliative Nursing. 5th ed New York: Oxford University Press; 2019. [Google Scholar]
- 12.Sinclair S McClement S Raffin-Bouchal S, et al. Compassion in health care: an empirical model. J Pain Symptom Manage. 2016;51(2):193–203. [DOI] [PubMed] [Google Scholar]
- 13.Dempsey C. The Antidote to Suffering: How Compassionate Connected Care Can Improve Safety, Quality, and Experience. New York: MGraw-Hill; 2018. [Google Scholar]


