Abstract
Rationale: Physical activity while being exposed to high concentrations of air pollution may lead to greater inhalation of pollutant particles and gases. Thus, owing to features of the built city environment, specific locations where physical activity take place may put individuals at increased risk for harmful inhaled exposures leading to decrements in lung function.
Objectives: The objectives were to determine locations throughout an urban landscape where children engage in moderate to vigorous activity (MVA). We hypothesized that outdoor activity would be associated with increased exposure to air pollution and reduced lung function.
Methods: Children aged 9–14 years living in New York City (NYC) (n = 151) wore global positioning system devices and wrist accelerometers for two 24-hour periods. Time-stamped global positioning system points and accelerometer data were aggregated and mapped using ArcGIS to determine locations where children engaged in MVA. Location-specific particulate matter <2.5 microns and nitrogen dioxide (NO2) was determined based on land use regression models of street-level pollution. Temporal air pollution exposure was determined based on daily concentrations collected at one central site in NYC. Forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and forced expiratory flow, midexpiratory phase (FEF25–75) were collected following each 24-hour period. Data were analyzed using multivariable linear regression models to examine associations between MVA time and both lung function and air pollution in separate models. Additionally, a multiplicative interaction term (MVA time × season) was included to test whether the association between MVA time and lung function outcomes varied by warmer versus colder months.
Results: On average, children spent less MVA time outdoors (38.2 ± 39.6 min/d) compared with indoors (71.9 ± 74.7 min/d, P < 0.01), regardless of season. The majority of outdoor MVA occurred along sidewalks and roadbeds (30.2 ± 33.3 min/d, 76.9% of outdoor) where annual average concentrations of NO2 were relatively high. Interquartile range (IQR) increase in outdoor MVA time (44 min) was associated with higher levels of annual average NO2 (P < 0.01) but not particulate matter <2.5 microns. In warmer months, for IQR increase in outdoor MVA time, children had 1.41% lower FEV1/FVC (95% confidence interval [95% CI], −2.46 to −0.36) and 4.40% lower percent predicted FEF25–75 (95% CI, −8.02 to −0.78). These results persisted even after adjustment for location-specific annual average concentrations of NO2. No association was observed between MVA time and lung function in colder months (P > 0.05), and a formal test for interaction (MVA time × season) was significant (P value for interaction = 0.01 and 0.03 for FEV1/FVC and FEF25–75, respectively).
Conclusions: Children in NYC spent less time active outdoors compared with indoors. Outdoor activity was greatest near traffic sources and associated with higher annual average concentrations of NO2. In warmer months, outdoor activity was associated with lower lung function, but this association did not appear to be mediated by higher exposure to outdoor pollution during exercise.
Keywords: exercise, nitrogen dioxide, asthma, built environment
Exposure to ambient pollution is a well-documented trigger of impaired lung function in children (1–3). Although regular physical activity has been associated with improved spirometry outcomes (4–6), increased minute ventilation during activity could result in increased lung deposition of pollutant gases and particles (7). Children may be particularly susceptible to the effects of physical activity in polluted environments and related airway injury because of ongoing development of the respiratory tract throughout early childhood and adolescence (8). For example, children living in high-ozone communities of Southern California who participated in at least three sports had greater than threefold increased risk of developing asthma over a 5-year period compared with children who did not participate in sports but lived in the same high-ozone communities (9). These findings suggest there is a mediation effect of pollution whereby high activity leads to increased inhalation of ambient pollution and subsequent airway hyperreactivity. The significant role of physical activity in the relationship between air pollution and lung function is corroborated by several short-term exposure studies. In adults, reduced lung function has been observed following physical activity in locations of high traffic-related air pollution exposure (10, 11) including particulate matter <2.5 microns (PM2.5) and nitrogen dioxide (NO2) (12). However, there is little known about how physical activity level is related to air pollution exposure and lung function in children. This is particularly important given the current World Health Organization recommendations that children participate in at least 60 minutes of moderate to vigorous activity daily (13, 14).
Features of the built city environment can influence both the amount of time one engages in physical activity (15–17) and the concentration of ambient pollution one is exposed to. In dense metropolitan areas, streets and adjacent roadbeds that are flanked on both sides by tall buildings have some of the highest concentrations of ambient pollution (18–20). Also, in many urban communities, playgrounds and athletic fields are located adjacent to high-traffic roadways, potentially increasing the amount of time children are engaged in highly active behaviors in highly polluted environments (21). To mitigate risk, we need to better understand where children spend time being physically active across an urban landscape and what the ambient pollutant exposures are during those periods of time. Accelerometers and global positioning system (GPS) devices can be combined to identify patterns and locations of physical activity across a geographic area (22, 23).
In a sample of 9- to 14-year-old children who live in New York City (NYC), our objective was to 1) characterize locations where children spent time engaged in physical activity and 2) examine the associations between locations of physical activity and both air pollution exposure (PM2.5 and NO2) and lung function. We hypothesized that owing to features of the built city environment, outdoor physical activity would be associated with increased exposure to air pollution and reduced lung function and that air pollution would modify the association between outdoor activity and lung function. Also, we investigated associations stratified by season owing to seasonal fluctuations in patterns of physical activity (24).
Methods
Study Participants
Study participants (n = 163) were enrolled from the Columbia Center for Children’s Environmental Health longitudinal birth cohort study. African American and Dominican mothers were recruited during pregnancy from Northern Manhattan and the South Bronx of NYC as previously described (25). For this nested case–control observational study to evaluate environmental factors associated with respiratory outcomes (26), children were recruited based on age (target 9–14 yr) and current asthma status. Because of the high prevalence of disease and morbidity in the community, the sample was enriched for children with asthma (target 50% asthma) to assess for potential effect modification. Asthma was diagnosed by a pulmonologist or allergist, and to meet enrollment criteria for the nested study, children had to report symptoms of asthma medication use in the 1 year before recruitment (27, 28). Children completed questionnaires at the end of each 24-hour GPS monitoring period to confirm their whereabouts while wearing the monitor. Complete data on GPS locations, physical activity, and lung function were available for n = 151 participants who were included in this analysis (see Figure E1 in the online supplement).
Physical Activity
Physical activity level was assessed using a wrist-mounted accelerometer (Actical, Philips Respironics) on the nondominant wrist for 6 consecutive days that overlapped with the 2 days of GPS measurement (i.e., visit 1 and 2; see Figure E2). As published previously, reported physical activity level did not vary significantly between days during which the GPS device was versus was not worn (29). Activity counts were determined by the accelerometer based on integrated measures of amplitude and frequency of motion. Activity intensity was determined based on energy expenditure (moderate = 0.031–0.083 kcal/min/kg; vigorous >0.083 kcal/min/kg). Activity counts were recorded by the Actical in 1-minute epochs. Using time stamps from the Actical, each 1-minute activity intensity score was matched with a GPS coordinate.
GPS Locations
Each participant wore a GPS device within a vest for two 24-hour periods 5 days apart (Figure E2) as previously described, and children demonstrated excellent compliance with wearing the vest (30). The GPS device recorded longitude and latitude spatial coordinates in 1-minute epochs. Participants with less than 100 GPS points identified in a 24-hour period (n = 6) were excluded owing to insufficient data (Figure E1). Time-stamped GPS coordinates were matched with time-stamped activity intensity scores for 2 days of overlapping periods. Only GPS points that corresponded with moderate or vigorous activity (MVA) were selected for analysis.
Initially, 40.2% of all vigorous-activity minutes and 35.5% of all moderate-activity minutes across all children were matched to a GPS coordinate. This GPS signal rate is consistent with similar urban studies using GPS data (31). The missing GPS coordinates that occurred only when participants were indoors were likely due to lost GPS signal that often occurs when people are in indoor environments or outdoors only for brief periods (32). Therefore, we used detailed questionnaire data collected at the end of each 24-hour monitoring period to confirm locations for the missing GPS points. The combination of GPS-derived coordinates and questionnaire-imputed coordinates resulted in 84.2% of all vigorous- and 80.6% of all moderate-activity points being matched to a GPS coordinate. Overall, 9.9% of all GPS points collected for the n = 151 children in this study corresponded with moderate or vigorous activity and were used for this analysis (Figure E1).
GPS coordinates were mapped to built environment features defined by the NYC Department of Parks and Recreation shape files using ArcGIS (Esri). To address concerns of misclassification of location coordinates based on GPS signal scatter that is known to occur in urban environments (33), all location points that were part of a “cloud” or that did not intersect with a built environment feature were visually inspected in ArcGIS in several ways (see the details in the online supplement). Overall, 88.7% of all location points captured during MVA were mapped to a built environment feature.
Spirometry
Spirometry was performed in participants’ homes using a portable device (Koko; nSpire Health) in accordance with American Thoracic Society and European Respiratory Society guidelines (34). Studies were performed immediately following each 24-hour GPS sampling period (Figure E2) as previously published (35, 36). Spirometry outcomes that were used for analysis included forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), FEV1/FVC ratio, and forced expiratory flow, midexpiratory phase (FEF25–75). National Health and Nutrition Examination Survey (NHANES) III reference equations were applied to determine the percent predicted values based on age, sex, and height. Percent predicted lung function values were used for the analyses, and models were further adjusted for race/ethnicity with a dichotomous variable (African American or Dominican).
Air Pollution and Meteorological Parameters
Location-specific air pollution measures were collected from the New York City Community Air Survey (NYCCAS) air quality–monitoring program between 2012 and 2015. NYCCAS estimates annual average concentrations of PM2.5 and NO2 and summer ozone (O3) using land use regression modeling (37–39). Citywide 300-m Esri grid raster files of annual average predicted PM2.5, NO2 and O3 were downloaded from the NYC OpenData website (40). Air pollution grids were then converted to points, and the nearest distance of each GPS point to the nearest grid point from each predicted pollutant surface was calculated in ArcGIS.
Temporal ambient concentrations of PM2.5 (collected every 3 d) and NO2 (collected daily) were measured by the New York State Department of Environmental Conservation between 2012 and 2015 (41). Data were downloaded for the stationary site monitor in the Bronx, located within the community where the majority of participants lived. PM2.5 concentrations ±1 day of sampling date were used in analysis.
Residential indoor PM2.5 concentrations were collected over a 6-day period that included the GPS sampling period (26). Indoor air monitors were placed in a room where the child spent most of his or her time (mostly the room where the child slept).
Daily average temperature and humidity data for NYC were retrieved from the National Oceanic and Atmospheric Administration’s database between 2012 and 2015 (42).
Data Analyses
Analyses were restricted to children who had complete GPS-derived built environment feature data and spirometry, resulting in a final sample of 151 (Figure E1). Chi-square and Mann-Whitney tests were used to detect differences in MVA time between indoor and outdoor locations.
Associations between outdoor MVA time and estimated annual concentrations of air pollution were analyzed using multivariable linear regression in generalized estimating equation models. We controlled for confounders that are known to be related to both the predictors and outcomes of interest for each respective model. In adjusted model 1, to assess the relationship between outdoor MVA time and air pollution exposure (i.e., location-specific annual average concentrations of PM2.5 or NO2), we controlled for asthma diagnosis and colder (September to March) versus warmer (April to August) months of sampling. Additionally, to account for temporal variation in air pollution concentration, we controlled for daily concentrations of PM2.5 or NO2, daily average temperature, and daily average relative humidity. In adjusted model 2, to assess the relationship between outdoor MVA time and lung function, we controlled for race/ethnicity, asthma diagnosis, obesity, and warmer/colder months. Both adjusted models 1 and 2 were further stratified into colder versus warmer months (stratified model) with the exclusion of the dichotomous season variable. Next, a multiplicative interaction term (MVA time × season) was included in adjusted model 2 (interaction model) to test whether the association between outdoor MVA and lung function varied by colder versus warmer months. β-coefficients are presented for an interquartile range (IQR) increase in MVA time, equivalent to 44 minutes.
To further assess for potential mediation between outdoor MVA time and lung function by multiple pollutants, we repeated the analysis in adjusted model 2 with an adjustment for estimated location-specific annual concentrations of air pollution (i.e., PM2.5 or NO2), as well as daily temperature and daily relative humidity (mediation model). Exploratory analyses were also conducted to examine if the relationship between MVA time and lung function outcomes varied by asthma status, as children with asthma may be more susceptible to the effects of air pollution (43, 44).
Five sensitivity analyses were conducted as follows: 1) reanalysis after removing one extreme FEF25–75, data point (exceeding 200% predicted), 2) reanalysis after excluding children who had only one 24-hour observation period (Nsubject = 39), 3) reanalysis after replacing location-specific annual average NO2 with temporal daily concentrations of NO2 in the mediation model, 4) reanalysis after controlling for location-specific summertime averaged O3 concentrations to assess for mediation by high O3 in warmer months, as suggested in a previous study (9), and 5) reanalysis after controlling for residential PM2.5 concentrations to account for air pollution exposure during sedentary periods because, on average, children spent 68% (16.3 h) of their time at home (26). All analyses were performed using SPSS Version 25 (IBM Corp), and P < 0.05 was considered statistically significant.
Results
Participants Characteristics
The demographic characteristics of the children enrolled in this study are reported in Table 1. Consistent with the design of the parent study, 55% (n = 83) children had asthma. The average FEV1 for the whole sample was 84.2% predicted (SD ± 12.4, 2.48 L/s ± 0.54) (Table 1): 85.6% ± 11.3 predicted among children with no asthma and 83.0% ± 13.2 predicted among children with asthma.
Table 1.
Cohort characteristics
| Characteristic | Participants Included* (N = 151) |
|---|---|
| Maternal ethnicity | |
| Dominican | 94 (62%) |
| African American | 57 (38%) |
| Age, mean (min–max), yr | 12.5 (9.2–14.3) |
| Sex, F | 78 (52%) |
| ≥Maternal high school degree | 82 (54%) |
| Maternal asthma (+) | 44 (29%) |
| BMI, mean ± SD, z-score† | 0.85 ± 1.10 |
| Obesity (≥95th percentile) | 37 (25%) |
| Asthma‡ | 83 (55%) |
| Lung function, mean ± SD, %§ | |
| FVC | 84.9 ± 11.4 |
| FEV1 | 84.2 ± 12.4 |
| FEV1/FVC | 86.8 ± 6.8 |
| FEF25–75 | 84.1 ± 23.5 |
Definition of abbreviations: BMI = body mass index; FEF25–75 = forced expiratory flow, midexpiratory phase; FEV1 = forced expiratory volume in 1 second; FVC = forced vital capacity; GPS = global positioning system; max = maximum; min = minimum; SD = standard deviation.
Data are n (%) unless otherwise noted.
Includes only the children who had complete lung function, GPS, and accelerometer data for current analysis.
Weight (kg)/height (m)2.
Determined by a pulmonologist or allergist, and to meet enrollment criteria for the nested study, children had to report symptoms or asthma medication use in the 1 year before recruitment.
Averaged percent predicted lung function over visit 1 and visit 2; percent predicted represents adjustment for age, sex, and height.
Locations of MVA
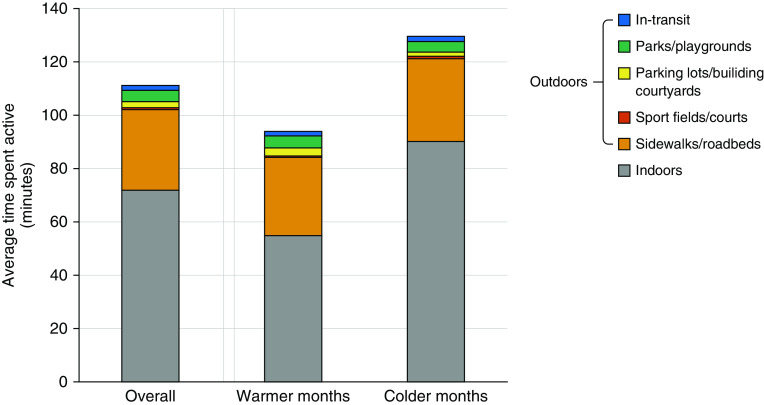
On average, children spent the majority of their overall MVA time indoors compared with outdoors (71.9 ± 74.7 min/d vs. 38.2 ± 39.6 min/d, for indoor vs. outdoor, respectively) (Figure 1). The majority of outdoor MVA occurred along sidewalks and roadbeds (30.2 ± 33.3 min/d, 76.9% of outdoor) (Figure 1).
Figure 1.
Average active time (minutes) spent in locations: overall and by warmer versus colder months. Warmer months include April to August and colder months include September to March.
When comparing physical activity by season, in general, children were more active in colder compared with warmer months (Figure 1). Indoor MVA time was greater during colder compared with warmer months (90.2 vs. 54.8 min for colder vs. warmer months, respectively, Mann-Whitney test, P = 0.002; see Table E1). However, outdoor MVA time did not differ by warmer versus colder months (Table E1).
Association between Outdoor MVA Time and Location-Specific Annual Average Concentrations of Air Pollution
During periods of outdoor MVA, exposure to annual average street-level modeled PM2.5 was highest in-transit and NO2 was highest along sidewalks/roadbeds and sports fields/courts (Kruskal-Wallis test, P < 0.01; see Figure E3). Overall, an IQR increase in MVA time (44 min) outdoors was associated with higher annual average concentrations of NO2 (β-coefficient, 0.31 ppb; 95% confidence interval [95% CI], 0.11 to 0.51; Table 2) but not PM2.5. The positive association between MVA time outdoors and location-specific annual average NO2 was more apparent in warmer months (β-coefficient, 0.31 ppb; 95% CI, 0.10 to 0.51; Figure 2B) than in colder months ((β-coefficient, 0.22 ppb; 95% CI, −0.19 to 0.63). However, interaction between MVA time and season on annual average NO2 was not significant (P value for interaction = 0.60).
Table 2.
Associations between outdoor MVA time (minutes) and location-specific annual average concentrations of air pollution
| Main Effect (Nsubjects:nvisits = 151:263) | |
|---|---|
| Air pollutants | Adjusted β-Coefficient (95% CI)* |
| PM2.5, μg/m3 | 0.00 (−0.04 to 0.04) |
| NO2, ppb | 0.031 (0.11 to 0.51)† |
Definition of abbreviations: CI = confidence interval; MVA = moderate to vigorous activity; NO2 = nitrogen dioxide; Nsubjects = number of subjects included for the analysis; nvisits = total number of visits; PM2.5 = particulate matter <2.5 microns.
β-coefficients are presented for an interquartile range increase in MVA time, equivalent to 44 minutes. Bold typeface values represent P < 0.05.
Models adjusted for asthma, daily average temperature, daily average relative humidity, temporal daily levels of PM2.5 (or NO2) at fixed monitoring site, and warmer versus colder months.
P < 0.01.
Figure 2.
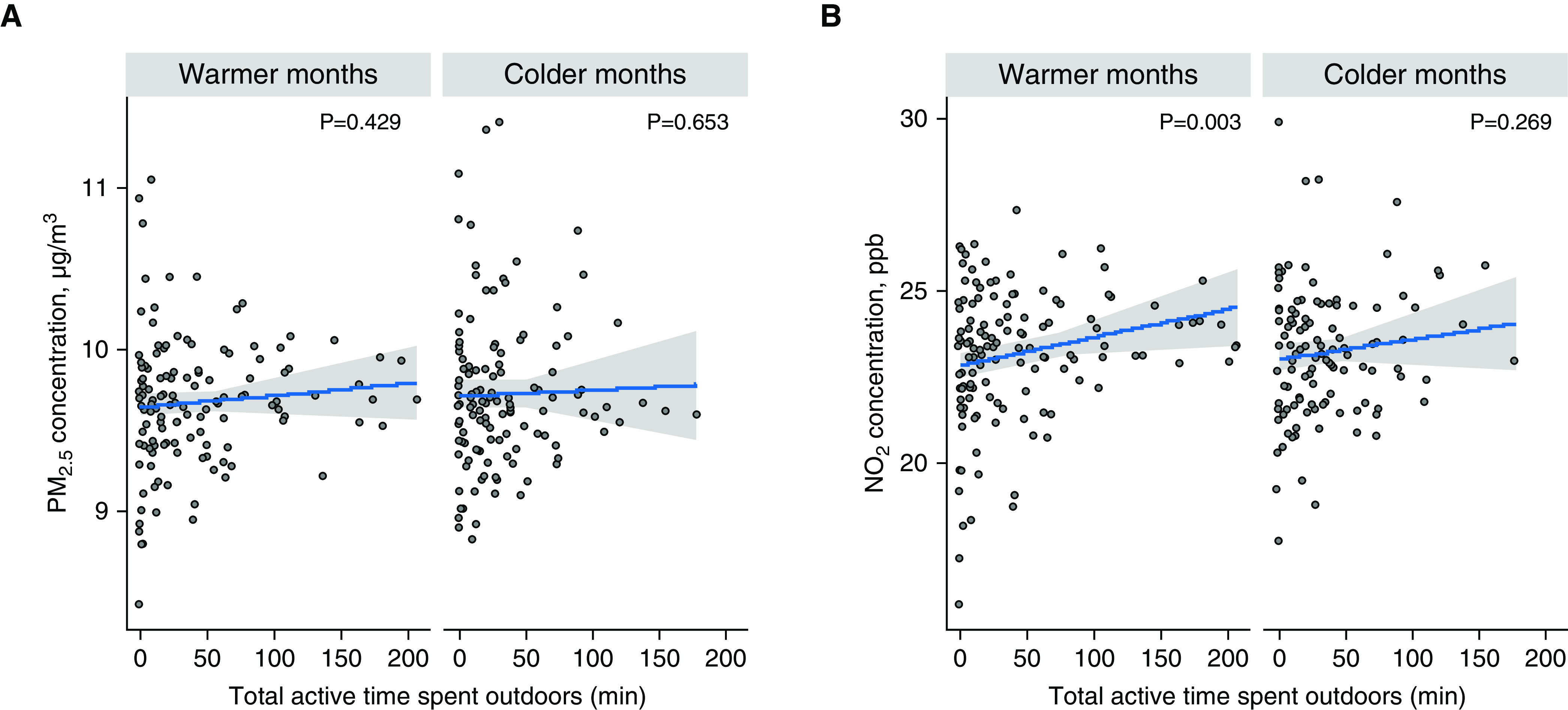
Associations between total active time (minutes) and exposure to estimated annual concentrations of (A) particulate matter <2.5 microns (PM2.5) and (B) nitrogen dioxide (NO2), stratified by warmer versus colder months. The regression line with 95% confidence interval is from univariate analysis and P values were obtained from the stratified models (controlling for asthma, daily concentrations of PM2.5 or NO2, average daily temperature, and average daily relative humidity). ppb = parts per billion.
Association between Outdoor MVA and Lung Function: Effect Modification by Warmer versus Colder Months
Overall, the amount of time spent in outdoor MVA was not associated with lung function in adjusted models (see Table E2). However, during warmer months, increased outdoor MVA time was associated with lower FEV1/FVC, and FEF25–75 (β-coefficient per IQR of MVA, −1.41%; 95% CI, −2.46 to −0.36; and −4.40% predicted; 95% CI, −8.02 to −0.78 for FEV1/FVC and FEF25–75, respectively; Figure 3 and Table E2) but not FVC or FEV1 (Figure E4). During colder months, no significant association was observed between outdoor MVA time and lung function (Table E2). In a test for effect modification, an interaction between outdoor MVA time and season on FEV1/FVC and FEF25–75 was observed (P value for interaction = 0.01 and 0.03 for FEV1/FVC and FEF25–75, respectively; Table E2). We further performed mediation analyses, which were restricted to warmer months given the observed associations between outdoor MVA time and lung function only in warmer months. After controlling for location-specific annual average concentrations of NO2, daily temperature, and daily relative humidity in an adjusted model 2, the significant associations between outdoor MVA time and lung function remained (β-coefficient per IQR of MVA, −1.28%; 95% CI, −2.28 to −0.28; and −3.74% predicted; 95% CI, −7.28 to −0.20 for FEV1/FVC and FEF25–75, respectively). Similar results were observed when location-specific annual NO2 was replaced with PM2.5 (data not shown).
Figure 3.
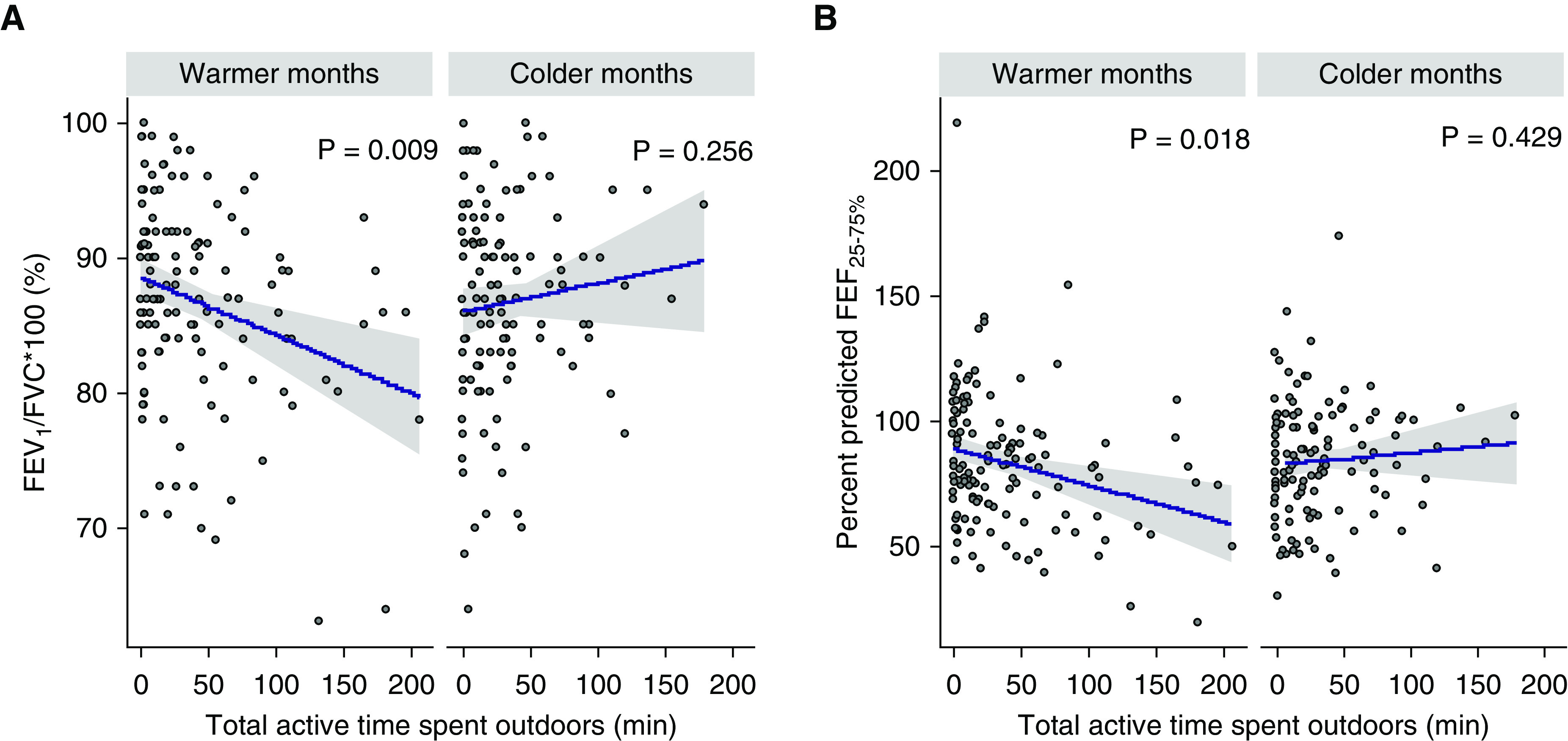
Associations between total active time (minutes) and lung function: (A) FEV1/FVC and (B) FEF25–75, stratified by warmer versus colder months. The regression line with 95% confidence interval is from univariate analysis and P values were obtained from the stratified models (controlling for race/ethnicity, asthma, and obesity). FEF25–75 = forced expiratory flow, midexpiratory phase; FEV1 = forced expiratory volume in 1 second; FVC = forced vital capacity.
In addition, to explore whether the associations between MVA time and lung function vary by asthma status, stratified analyses were repeated after adjusting for race/ethnicity, obesity, and warmer/colder months. Outdoor MVA time was not significantly associated with lung function outcomes regardless of asthma status (data not shown).
Sensitivity Analyses
First, after removing one extreme FEF25–75 data point, the association between outdoor MVA time and FEF25–75 during warmer months remained significant (β-coefficient per IQR of MVA, −3.78% predicted; 95% CI, −7.15 to −0.42). Second, after excluding 39 children with only one 24-hour observation period, the main findings between outdoor MVA time and lung function in warmer months displayed in Figure 3 persisted (β-coefficient per IQR of MVA, −1.58%; 95% CI, −2.70 to −0.47; and −5.19% predicted; 95% CI, −9.06 to −1.33 for FEV1/FVC and FEF25–75, respectively). Also, an interaction between outdoor MVA time and season on lung function was replicated when the analyses were restricted to those with two 24-hour observation periods (P value for interaction = 0.04 and 0.02 for FEV1/FVC and FEF25–75, respectively). Third, when location-specific annual average NO2 was replaced with temporal daily concentrations of NO2, the results shown in Figure 3 were replicated (data not shown). Fourth, after adjustment for location-specific summer averaged ambient ozone levels in an effort to evaluate it as a mediator, significant associations between outdoor MVA and lower FEV1/FVC and FEF25–75 remained (data not shown). Lastly, when residential PM2.5 was controlled in the model to account for pollution exposure during sedentary times, the significant associations between outdoor MVA and reduced lung function were replicated (data not shown).
Discussion
In our sample of 151 children living in NYC, we observed that children spent less time active outdoors compared with indoors, particularly in colder-weather months. When children were active outdoors, the majority of MVA time took place along sidewalks and roadbeds where annual average concentrations of NO2 were relatively high. Also, in warmer months, increased outdoor MVA time was associated with reduced lung function, specifically FEV1/FVC and FEF25–75. Location-specific concentrations of NO2 did not appear to mediate the association between increased outdoor activity and reduced lung function. Overall, our findings suggest that locations where children engage in outdoor physical activity in urban neighborhoods, particularly during warmer months, may contribute to reduced lung function.
Our approach was to identify the locations within an urban community where children spent time engaged in active behaviors in an effort to quantify exposure to ambient pollutants during those periods of activity. Others have classified locations of childhood physical activity using accelerometry and GPS devices (31, 32, 45, 46). Yet, variations in the built environment from city to city likely contribute to variability in activity patterns across different populations. For example, neighborhood safety, walkability, and amount of green space have been linked to increased outdoor physical activity in some regions (47). In the United Kingdom, children were less active in autumn and winter months compared with warmer months (24), whereas we observed greater indoor activity compared with outdoor, particularly in colder months. Indoor exposure to ambient pollutants (37–39) could result in high inhalation exposure during physical activity. However, we were particularly interested in outdoor activity because of 1) the risk for higher exposure to traffic-related air pollutants that have been linked to reduced lung function and 2) the availability of a network of street-level modeled outdoor pollution data through the NYCCAS data set.
In our sample of children living in an urban environment, the majority of outdoor activity that occurred along sidewalks and street beds might be attributed to commuting to and from school, as observed by others (24). The majority of outdoor activity that occurred near these traffic sources explains the positive association between overall outdoor MVA time and annual average NO2, an indicator of vehicular traffic that is high along busy roadways (45). Xu and colleagues recently described differences in spatial distribution between NO2 and PM2.5 in Beijing, China (46). They reported that there was less regional variation in PM2.5 than NO2 (46). Homogeneity in PM2.5 concentration also has been described across New York State (47) and could explain the lack of association between specific location of outdoor activity (predominately along streets) and PM2.5 exposure.
Although we hypothesized that exposure to ambient pollution would modify the association between locations of physical activity and reduction in lung function, we observed that this later association was independent of NO2. There are several plausible explanations for this. For one, our air pollution estimates were annual averages based on land use regression modeling derived from street-level pollution sensors deployed in 2-week intervals across each season (37–39). Although the estimates for location-specific concentrations are robust, daily fluctuations in pollution exposure are known to result from changes in temperature, humidity, and other meteorological conditions (48). Therefore, we further adjusted for daily temperature and humidity to account for temporal variability in air pollution exposure estimates across NYC. We also observed negative associations between outdoor MVA time and lung function only in warmer months. Ozone, another ambient pollutant, often peaks in summer months, is reduced in winter months, and has been associated with reduced lung function (9). However, in sensitivity analysis adjusting for street-level summer averaged ozone concentration, there was no significant difference in the association between outdoor MVA time and lung function. Additionally, other warm-weather environmental exposures that were not measured in this current study could contribute to the relationship between locations of physical activity and lung function, such as aeroallergens. It has been demonstrated that air pollutant particles can bind to and concentrate aeroallergens in the environment (49–51). Thus, future studies should address combined exposure to pollutants and aeroallergens in understanding the relationship between outdoor activity and respiratory outcomes.
To our knowledge, this is the first study to examine locations of physical activity and lung function in children. A landmark study from the Southern California Children’s Health Study identified that children who engaged in more outdoor sports and were exposed to high community-level ozone concentrations were more likely to develop asthma compared with children who were less engaged in outdoor sports activities (9). However, this large population-based study did not measure individual-level physical activity patterns. Nor did it account for specific locations where activity took place. Several adult studies have demonstrated decreased lung function following physical activity under highly polluted conditions (11, 52–55) that corroborate our findings in children. We did not observe associations between physical activity and FEV1 or FVC. However, FEV1/FVC and FEF25–75 may be more sensitive indicators of lower airway obstruction in children (56, 57). And because of the size of pollutant particles and gases in relation to the diameter of the lower respiratory tract, lower airways may be the location of lung deposition of pollutant particles and gases. Although children with asthma may be more susceptible to the effects of air pollution (43, 44), our exploratory analyses indicated that the associations between MVA time and lung function did not vary by asthma status.
It is important for us to acknowledge several limitations of our study. First, the sample size was small; therefore, we were limited in our ability to assess relationships between specific outdoor locations (e.g., sidewalks vs. parks) and lung function as not all children engaged in activity in each of those specific locations. Second, this is a selected population of minority children that live in an urban environment. Although our findings may not be generalizable to the population at large, the population to which it is generalizable represents a large burden of asthma morbidity in urban communities. Third, children in this study spent only 9.9% of time engaged in physical activity and the majority of their time at home during sedentary periods. Sensitivity analysis with an adjustment of residential PM2.5 levels showed that our findings persisted. Fourth, in adjusted model 1, we only controlled for temporal daily concentrations of air pollution, which do not reflect the fine time scale of exposure during outdoor MVA activity. Lastly, this was a cross-sectional study design in which physical activity and lung function were measured within the same 24 hours; therefore, it is plausible that reduced lung function could have resulted in reduced physical activity level. However, overall, there was no association between the amount of time children engaged in MVA and FEV1, making this less likely.
Conclusions
Because physical activity leads to increased ventilation, the ability to identify specific locations of activity, especially near sources of high pollution, can improve risk assessment for lung function impairment. Our findings of an association between outdoor MVA time and both elevated annual average NO2 concentration and reduced lung function demonstrate a need to inform individuals in urban communities about location-specific exposure risks. Our findings also support the need for continued attention toward improving air quality, especially in urban communities.
Footnotes
Supported by the Columbia University John M. Driscoll, Jr., M.D., Children’s Fund Award, 1K01HL140216, the Amos Medical Faculty Development Award, 4R01ES013163, P01ES09600, P50ES015905, P30ES09089, and U01EB021983.
Author Contributions: S.L.-D. contributed to the conception and design of the work, acquisition of funding for the research, acquisition of data, and the analysis and interpretation of the data and co-wrote the first draft of the manuscript. K.H.J. supervised and participated in data collection, analysis, and interpretation of the data and co-wrote the first draft of the manuscript. M.M., J.C., and D.S. contributed to data acquisition and analysis. J.Q. contributed to data acquisition, data analysis, and critical review of the manuscript. F.P. contributed to securing funding for the parent birth cohort study and critically reviewed the manuscript. S.N.C. contributed to interpretation of the data and critical review of the manuscript. J.G. contributed to data analysis and critical review of the manuscript. M.P. contributed to conception and design of the work, interpretation of findings, and critical review of the manuscript. A.R. contributed to conception and design of the work and interpretation of findings. R.M. contributed to acquisition of funding for the parent study, conception and design of the work, and interpretation and critical review of the manuscript.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Gehring U, Gruzieva O, Agius RM, Beelen R, Custovic A, Cyrys J, et al. Air pollution exposure and lung function in children: the ESCAPE project. Environ Health Perspect. 2013;121:1357–1364. doi: 10.1289/ehp.1306770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gauderman WJ, McConnell R, Gilliland F, London S, Thomas D, Avol E, et al. Association between air pollution and lung function growth in southern California children. Am J Respir Crit Care Med. 2000;162:1383–1390. doi: 10.1164/ajrccm.162.4.9909096. [DOI] [PubMed] [Google Scholar]
- 3.Ierodiakonou D, Zanobetti A, Coull BA, Melly S, Postma DS, Boezen HM, et al. Childhood Asthma Management Program Research Group. Ambient air pollution, lung function, and airway responsiveness in asthmatic children. J Allergy Clin Immunol. 2016;137:390–399. doi: 10.1016/j.jaci.2015.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ji J, Wang SQ, Liu YJ, He QQ. Physical activity and lung function growth in a cohort of Chinese school children: a prospective study. PLoS One. 2013;8:e66098. doi: 10.1371/journal.pone.0066098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fuertes E, Carsin AE, Antó JM, Bono R, Corsico AG, Demoly P, et al. Leisure-time vigorous physical activity is associated with better lung function: the prospective ECRHS study. Thorax. 2018;73:376–384. doi: 10.1136/thoraxjnl-2017-210947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berntsen S, Wisløff T, Nafstad P, Nystad W. Lung function increases with increasing level of physical activity in school children. Pediatr Exerc Sci. 2008;20:402–410. doi: 10.1123/pes.20.4.402. [DOI] [PubMed] [Google Scholar]
- 7.Löndahl J, Massling A, Pagels J, Swietlicki E, Vaclavik E, Loft S. Size-resolved respiratory-tract deposition of fine and ultrafine hydrophobic and hygroscopic aerosol particles during rest and exercise. Inhal Toxicol. 2007;19:109–116. doi: 10.1080/08958370601051677. [DOI] [PubMed] [Google Scholar]
- 8.Gauderman WJ, Avol E, Gilliland F, Vora H, Thomas D, Berhane K, et al. The effect of air pollution on lung development from 10 to 18 years of age. N Engl J Med. 2004;351:1057–1067. doi: 10.1056/NEJMoa040610. [DOI] [PubMed] [Google Scholar]
- 9.McConnell R, Berhane K, Gilliland F, London SJ, Islam T, Gauderman WJ, et al. Asthma in exercising children exposed to ozone: a cohort study. Lancet. 2002;359:386–391. doi: 10.1016/S0140-6736(02)07597-9. [DOI] [PubMed] [Google Scholar]
- 10.Matt F, Cole-Hunter T, Donaire-Gonzalez D, Kubesch N, Martínez D, Carrasco-Turigas G, et al. Acute respiratory response to traffic-related air pollution during physical activity performance. Environ Int. 2016;97:45–55. doi: 10.1016/j.envint.2016.10.011. [DOI] [PubMed] [Google Scholar]
- 11.McCreanor J, Cullinan P, Nieuwenhuijsen MJ, Stewart-Evans J, Malliarou E, Jarup L, et al. Respiratory effects of exposure to diesel traffic in persons with asthma. N Engl J Med. 2007;357:2348–2358. doi: 10.1056/NEJMoa071535. [DOI] [PubMed] [Google Scholar]
- 12.Sinharay R, Gong J, Barratt B, Ohman-Strickland P, Ernst S, Kelly F, et al. Respiratory and cardiovascular responses to walking down a traffic-polluted road compared with walking in a traffic-free area in participants aged 60 years and older with chronic lung or heart disease and age-matched healthy controls: a randomised, crossover study Lancet 2018391339–349.[Published erratum appears in Lancet 391:308.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA. 2018;320:2020–2028. doi: 10.1001/jama.2018.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. Geneva: WHO Press: World Health Organization; 2010. Global recommendations on physical activity for health. [PubMed] [Google Scholar]
- 15.Troped PJ, Wilson JS, Matthews CE, Cromley EK, Melly SJ. The built environment and location-based physical activity. Am J Prev Med. 2010;38:429–438. doi: 10.1016/j.amepre.2009.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJF, Martin BW Lancet Physical Activity Series Working Group. Correlates of physical activity: why are some people physically active and others not? Lancet. 2012;380:258–271. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- 17.Ding D, Sallis JF, Kerr J, Lee S, Rosenberg DE. Neighborhood environment and physical activity among youth a review. Am J Prev Med. 2011;41:442–455. doi: 10.1016/j.amepre.2011.06.036. [DOI] [PubMed] [Google Scholar]
- 18.De Nicola F, Murena F, Costagliola MA, Alfani A, Baldantoni D, Prati MV, et al. A multi-approach monitoring of particulate matter, metals and PAHs in an urban street canyon. Environ Sci Pollut Res Int. 2013;20:4969–4979. doi: 10.1007/s11356-012-1456-1. [DOI] [PubMed] [Google Scholar]
- 19.Ng WY, Chau CK. A modeling investigation of the impact of street and building configurations on personal air pollutant exposure in isolated deep urban canyons. Sci Total Environ. 2014;468-469:429–448. doi: 10.1016/j.scitotenv.2013.08.077. [DOI] [PubMed] [Google Scholar]
- 20.Weber S, Kordowski K, Kuttler W. Variability of particle number concentration and particle size dynamics in an urban street canyon under different meteorological conditions. Sci Total Environ. 2013;449:102–114. doi: 10.1016/j.scitotenv.2013.01.044. [DOI] [PubMed] [Google Scholar]
- 21.Rundell KW, Caviston R, Hollenbach AM, Murphy K. Vehicular air pollution, playgrounds, and youth athletic fields. Inhal Toxicol. 2006;18:541–547. doi: 10.1080/08958370600685640. [DOI] [PubMed] [Google Scholar]
- 22.Demant Klinker C, Schipperijn J, Toftager M, Kerr J, Troelsen J. When cities move children: development of a new methodology to assess context-specific physical activity behaviour among children and adolescents using accelerometers and GPS. Health Place. 2015;31:90–99. doi: 10.1016/j.healthplace.2014.11.006. [DOI] [PubMed] [Google Scholar]
- 23.James P, Jankowska M, Marx C, Hart JE, Berrigan D, Kerr J, et al. “Spatial energetics”: integrating data from GPS, accelerometry, and GIS to address obesity and inactivity. Am J Prev Med. 2016;51:792–800. doi: 10.1016/j.amepre.2016.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Atkin AJ, Sharp SJ, Harrison F, Brage S, Van Sluijs EMF. Seasonal variation in children’s physical activity and sedentary time. Med Sci Sports Exerc. 2016;48:449–456. doi: 10.1249/MSS.0000000000000786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Perera FP, Rauh V, Tsai WY, Kinney P, Camann D, Barr D, et al. Effects of transplacental exposure to environmental pollutants on birth outcomes in a multiethnic population. Environ Health Perspect. 2003;111:201–205. doi: 10.1289/ehp.5742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jung KH, Torrone D, Lovinsky-Desir S, Perzanowski M, Bautista J, Jezioro JR, et al. Short-term exposure to PM2.5 and vanadium and changes in asthma gene DNA methylation and lung function decrements among urban children. Respir Res. 2017;18:63. doi: 10.1186/s12931-017-0550-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lovinsky-Desir S, Jung KH, Rundle AG, Hoepner LA, Bautista JB, Perera FP, et al. Physical activity, black carbon exposure and airway inflammation in an urban adolescent cohort. Environ Res. 2016;151:756–762. doi: 10.1016/j.envres.2016.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Donohue KM, Al-alem U, Perzanowski MS, Chew GL, Johnson A, Divjan A, et al. Anti-cockroach and anti-mouse IgE are associated with early wheeze and atopy in an inner-city birth cohort. J Allergy Clin Immunol. 2008;122:914–920. doi: 10.1016/j.jaci.2008.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lovinsky-Desir S, Lawrence J, Jung KH, Rundle AG, Hoepner LA, Yan B, et al. Assessment of exposure to air pollution in children: determining whether wearing a personal monitor affects physical activity. Environ Res. 2018;166:340–343. doi: 10.1016/j.envres.2018.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lovinsky-Desir S, Folch C, Jung KH, Torrone D, Gil E, Perera F, et al. Urban adolescents readily comply with a complicated asthma research protocol. Clin Med Insights Circ Respir Pulm Med. 2014;8:5–9. doi: 10.4137/CCRPM.S13930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oreskovic NM, Blossom J, Field AE, Chiang SR, Winickoff JP, Kleinman RE. Combining global positioning system and accelerometer data to determine the locations of physical activity in children. Geospat Health. 2012;6:263–272. doi: 10.4081/gh.2012.144. [DOI] [PubMed] [Google Scholar]
- 32.Rainham DG, Bates CJ, Blanchard CM, Dummer TJ, Kirk SF, Shearer CL. Spatial classification of youth physical activity patterns. Am J Prev Med. 2012;42:e87–e96. doi: 10.1016/j.amepre.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 33.Mooney SJ, Sheehan DM, Zulaika G, Rundle AG, McGill K, Behrooz MR, et al. Quantifying distance overestimation from global positioning system in urban spaces. Am J Public Health. 2016;106:651–653. doi: 10.2105/AJPH.2015.303036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miller MR, Crapo R, Hankinson J, Brusasco V, Burgos F, Casaburi R, et al. ATS/ERS Task Force. General considerations for lung function testing. Eur Respir J. 2005;26:153–161. doi: 10.1183/09031936.05.00034505. [DOI] [PubMed] [Google Scholar]
- 35.Jung KH, Torrone D, Lovinsky-Desir S, Perzanowski M, Bautista J, Jezioro JR, et al. Short-term exposure to PM2.5 and vanadium and changes in asthma gene DNA methylation and lung function decrements among urban children. Respir Res. 2017;18:63. doi: 10.1186/s12931-017-0550-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lovinsky-Desir S, Jung KH, Jezioro JR, Torrone DZ, de Planell-Saguer M, Yan B, et al. Physical activity, black carbon exposure, and DNA methylation in the FOXP3 promoter. Clin Epigenetics. 2017;9:65. doi: 10.1186/s13148-017-0364-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Matte TD, Ross Z, Kheirbek I, Eisl H, Johnson S, Gorczynski JE, et al. Monitoring intraurban spatial patterns of multiple combustion air pollutants in New York City: design and implementation. J Expo Sci Environ Epidemiol. 2013;23:223–231. doi: 10.1038/jes.2012.126. [DOI] [PubMed] [Google Scholar]
- 38.Clougherty JE, Kheirbek I, Eisl HM, Ross Z, Pezeshki G, Gorczynski JE, et al. Intra-urban spatial variability in wintertime street-level concentrations of multiple combustion-related air pollutants: the New York City Community Air Survey (NYCCAS) J Expo Sci Environ Epidemiol. 2013;23:232–240. doi: 10.1038/jes.2012.125. [DOI] [PubMed] [Google Scholar]
- 39.Kheirbek I, Ito K, Neitzel R, Kim J, Johnson S, Ross Z, et al. Spatial variation in environmental noise and air pollution in New York City. J Urban Health. 2014;91:415–431. doi: 10.1007/s11524-013-9857-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.New York City OpenData New York: Department of Health and Mental Hygiene; 2013 [accessed 2016 Apr 25] Available from: https://data.cityofnewyork.us/Environment/NYCCAS-Air-Pollution-Rasters/q68s-8qxv.
- 41.Outdoor Air Quality Data. Research Triangle Park, NC: United States Environmental Protection Agency; 2015 [accessed 2020 Jan 10] Available from: https://www.epa.gov/outdoor-air-quality-data/download-daily-data.
- 42.Local Climatology Data Station Details. Asheville, NC: National Centers for Environmental Information; 2015 [accessed 2020 Jan 10] Available from: https://www.ncdc.noaa.gov/cdo-web/datasets/LCD/stations/WBAN:94728/detail.
- 43.Lewis TC, Robins TG, Dvonch JT, Keeler GJ, Yip FY, Mentz GB, et al. Air pollution-associated changes in lung function among asthmatic children in Detroit. Environ Health Perspect. 2005;113:1068–1075. doi: 10.1289/ehp.7533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li S, Williams G, Jalaludin B, Baker P. Panel studies of air pollution on children’s lung function and respiratory symptoms: a literature review. J Asthma. 2012;49:895–910. doi: 10.3109/02770903.2012.724129. [DOI] [PubMed] [Google Scholar]
- 45.Quigg R, Gray A, Reeder AI, Holt A, Waters DL. Using accelerometers and GPS units to identify the proportion of daily physical activity located in parks with playgrounds in New Zealand children. Prev Med. 2010;50:235–240. doi: 10.1016/j.ypmed.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 46.Grow HM, Saelens BE, Kerr J, Durant NH, Norman GJ, Sallis JF. Where are youth active? Roles of proximity, active transport, and built environment. Med Sci Sports Exerc. 2008;40:2071–2079. doi: 10.1249/MSS.0b013e3181817baa. [DOI] [PubMed] [Google Scholar]
- 47.Lovasi GS, Schwartz-Soicher O, Quinn JW, Berger DK, Neckerman KM, Jaslow R, et al. Neighborhood safety and green space as predictors of obesity among preschool children from low-income families in New York City. Prev Med. 2013;57:189–193. doi: 10.1016/j.ypmed.2013.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.DeGaetano AT, Doherty OM. Temporal, spatial and meteorological variations in hourly PM2.5 concentration extremes in New York City. Atmos Environ. 2004;38:1547–1558. [Google Scholar]
- 49.Steerenberg PA, Bischoff EW, de Klerk A, Verlaan AP, Jongbloets LM, van Loveren H, et al. Acute effect of air pollution on respiratory complaints, exhaled NO and biomarkers in nasal lavages of allergic children during the pollen season. Int Arch Allergy Immunol. 2003;131:127–137. doi: 10.1159/000070928. [DOI] [PubMed] [Google Scholar]
- 50.Knox RB, Suphioglu C, Taylor P, Desai R, Watson HC, Peng JL, et al. Major grass pollen allergen Lol p 1 binds to diesel exhaust particles: implications for asthma and air pollution. Clin Exp Allergy. 1997;27:246–251. [PubMed] [Google Scholar]
- 51.Riediker M, Monn C, Koller T, Stahel WA, Wüthrich B. Air pollutants enhance rhinoconjunctivitis symptoms in pollen-allergic individuals. Ann Allergy Asthma Immunol. 2001;87:311–318. doi: 10.1016/S1081-1206(10)62246-6. [DOI] [PubMed] [Google Scholar]
- 52.Sinharay R, Gong J, Barratt B, Ohman-Strickland P, Ernst S, Kelly FJ, et al. Respiratory and cardiovascular responses to walking down a traffic-polluted road compared with walking in a traffic-free area in participants aged 60 years and older with chronic lung or heart disease and age-matched healthy controls: a randomised, crossover study. Lancet. 2018;391:339–349. doi: 10.1016/S0140-6736(17)32643-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rundell KW, Slee JB, Caviston R, Hollenbach AM. Decreased lung function after inhalation of ultrafine and fine particulate matter during exercise is related to decreased total nitrate in exhaled breath condensate. Inhal Toxicol. 2008;20:1–9. doi: 10.1080/08958370701758593. [DOI] [PubMed] [Google Scholar]
- 54.Salvi S, Blomberg A, Rudell B, Kelly F, Sandström T, Holgate ST, et al. Acute inflammatory responses in the airways and peripheral blood after short-term exposure to diesel exhaust in healthy human volunteers. Am J Respir Crit Care Med. 1999;159:702–709. doi: 10.1164/ajrccm.159.3.9709083. [DOI] [PubMed] [Google Scholar]
- 55.Laeremans M, Dons E, Avila-Palencia I, Carrasco-Turigas G, Orjuela-Mendoza JP, Anaya-Boig E, et al. Black carbon reduces the beneficial effect of physical activity on lung function. Med Sci Sports Exerc. 2018;50:1875–1881. doi: 10.1249/MSS.0000000000001632. [DOI] [PubMed] [Google Scholar]
- 56.Lebecque P, Kiakulanda P, Coates AL. Spirometry in the asthmatic child: is FEF25-75 a more sensitive test than FEV1/FVC? Pediatr Pulmonol. 1993;16:19–22. doi: 10.1002/ppul.1950160105. [DOI] [PubMed] [Google Scholar]
- 57.Bacharier LB, Strunk RC, Mauger D, White D, Lemanske RF, Jr, Sorkness CA. Classifying asthma severity in children: mismatch between symptoms, medication use, and lung function. Am J Respir Crit Care Med. 2004;170:426–432. doi: 10.1164/rccm.200308-1178OC. [DOI] [PubMed] [Google Scholar]