The global severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic continues to progress quickly, with over 36 million people infected and over 1 million deaths associated with SARS-CoV-2 by early October 2020. Large-scale clinical trials have observed improved outcomes in some individuals with severe coronavirus disease (COVID-19) after treatment with dexamethasone and hydrocortisone (1, 2). However, no treatment has been identified that significantly reduces infection or hospitalization rates. The repurposing of many antiinflammatory or antiviral drugs has also, as yet, failed to show significant impact on disease. Therefore, there is an urgent need to improve our understanding of SARS-CoV-2 infection and pathogenesis and develop new therapeutic and preventative treatment strategies.
One approach to identify novel disease mechanisms and therapeutic targets has been large-scale screening in preclinical small animal models, particularly mice. SARS-CoV-2 cell entry is mediated by binding of the viral S (Spike) protein to hACE2 (human angiotensin-converting enzyme 2) that is broadly expressed in the respiratory, but also the nasal and gastrointestinal, epithelium (3). Unfortunately, mouse ACE2 shows limited binding to the SARS-CoV-2 S protein, meaning commercially available wild-type (WT) inbred mouse strains are not useful in the study of SARS-CoV-2 infection. In this issue of the Journal, Han and colleagues (pp. 79–88) describe a rapid mouse model of SARS-CoV-2 infection utilizing a recombinant human Ad5-hACE2 (adenovirus type 5–expressing hACE2) that results in hACE2 expression and supports SARS-CoV-2 replication in the lower respiratory tract of WT mice (4).
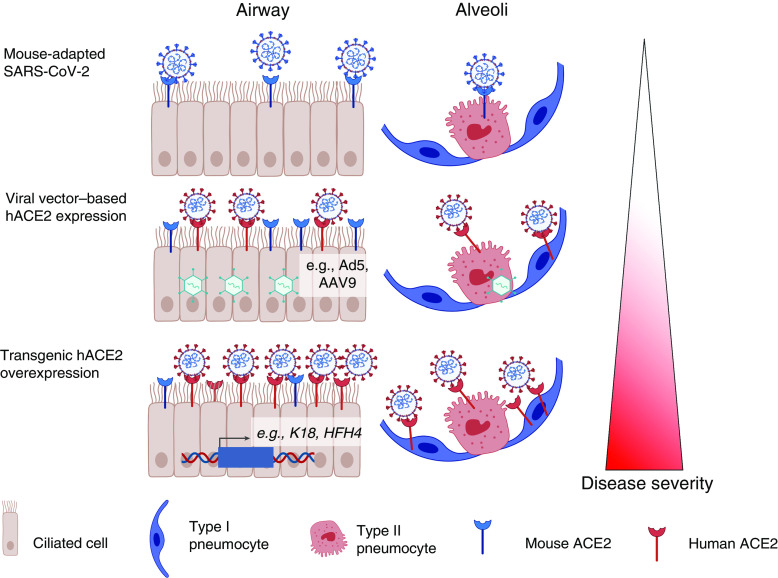
In Ad5-hACE2 mice, SARS-CoV-2 replication is restricted to the respiratory tract, especially type 2 pneumocytes, and the infection is associated with mild to moderate interstitial and perivascular inflammation localized to areas of the lungs expressing hACE2 (4). The observation that the severity of SARS-CoV-2 infection may be tightly linked to the cellular and anatomical tropism provided by hACE2 distribution is supported by other SARS-CoV-2 mouse models. For instance, hACE2 expression under the K18 (human Keratin 18) promoter leads to expression of the protein not only in the respiratory tract but also in the small intestine, kidneys, liver, and other organs and results in lethal disease associated with severe pneumonia and viral dissemination (5). However, hACE2 expression under the HFH4 (FOXJ1) promoter leads to expression in the ciliated epithelium as well as the nervous system, resulting in neuroinvasion of SARS-CoV-2 (6, 7). In contrast, knocking hACE2 into the murine Ace2 promoter results in SARS-CoV-2 replication largely restricted to the conducting airways, producing mild inflammation, as does the mouse-adapted SARS-CoV-2 with enhanced S binding to mouse ACE2, highlighting the differential expression pattern of ACE2 in mice compared with humans (6, 8, 9). Importantly there is evidence that the distribution of hACE2 can be highly influential in determining the outcome SARS-CoV-2 infection in humans and tonally regulated by underlying conditions such as chronic obstructive pulmonary disease or environmental exposures including rhinoviral infection or smoking (10–12).
These multiple approaches to generate mouse models of COVID-19 have resulted in a diverse range of models allowing researchers to mimic the different outcomes and features of SARS-CoV-2 infection in humans, from asymptomatic to severe multiorgan disease. Of these models, however, the use of adenoviral vector delivery systems has several advantages, most prominently being the ability to rapidly establish infection in a range of animal strains, including WT inbred mouse strains, genetically modified animals used for mechanistic studies, and models that mimic comorbidities such as obesity and diabetes. Caveats to this approach do exist, especially the possible antiviral immune responses elicited by the adenoviral vectors, which could alter the responses to, and replication of, SARS-CoV-2. There is also a risk of nonphysiological expression patterns of hACE2. However, two other groups have used similar Ad5-hACE2 approaches to generate a SARS-CoV-2 mouse model with similar outcomes (13, 14), indicating that the system is robustly reproducible. In addition, another study has used different adenoviral vectors, such as adenovirus-associated virus 9 (AAV9) hACE2 (15), highlighting the potential of this approach to modulate and modify the expression pattern of hACE2 in the mouse.
One biological process Han and colleagues highlight from their work as a possible determining factor of disease severity is the effects of IFNs. They find a type I IFN transcriptional signature in the SARS-CoV-2–infected Ad5-hACE2 mice (4) similar to observations in studies using Ad5-hACE2 mice (9) and AAV-hACE2 mice (15) and in patients with COVID-19 (16). Intriguingly, there are suggestions that type I IFNs are not sufficiently induced in the early days of infection, resulting in higher viral load, but that these cytokines are highly expressed later during the infection, potentially driving the inflammatory response (16). Furthermore, a recent study shows a strong genetic correlation of the type I IFN system with severe COVID-19 (17). This will be important to study in mouse models, as early studies suggest that type I IFNs can influence viral load (13) and can be drivers of inflammation during SARS-CoV-2 infection (15).
In summary, different mouse models, including the one described by Han and colleagues, are needed to aid in generating the mechanistic insight we currently lack. We do not know how an effective anti–SARS-CoV-2 response develops or anything about the early drivers of disease. The aim of these models is to replicate the human disease, or aspects thereof, as closely as possible, and although none currently utilized perfectly recapitulate either the biology or pathology of clinical infection, dependent on the question asked, the use of several animal models should prove beneficial (as summarized in Figure 1). For example, the rapidly deployable Ad- or AAV-hACE2 models may be useful in screening antivirals (4, 13, 14), whereas the K18-hACE2 mouse could be more useful in vaccine development. However, elucidating disease mechanisms is likely to require a more specific human ACE2 knock-in model or a mouse-adapted strain of SARS-CoV-2. The models in which more prolonged disease is observed may also prove advantageous in following and perhaps manipulating long-term inflammatory responses and lung tissue repair mechanisms, thereby providing insight during the puzzling “long COVID” in individuals recovering from SARS-CoV-2 infection.
Figure 1.
Mouse models of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection provide a broad range of disease phenotypes and pathologies for the study of coronavirus disease (COVID-19). The use of mouse-adapted, adenovirus-induced, and genetically overexpressed strategies, including Ad5-hACE2 (adenovirus type 5–expressing human angiotensin-converting enzyme 2) overexpression described by Han and colleagues, for promoting SARS-CoV-2 binding to ACE2 within the respiratory tract, facilitates viral replication and provides a range of viral tropisms and disease severities with which to study pathogenesis. The figure was created using Biorender. AAV9 = adenovirus-associated virus 9; HFH4 = HNF-3/forkhead homolog 4; K18 = human keratin 18.
Supplementary Material
Footnotes
Originally Published in Press as DOI: 10.1165/rcmb.2020-0456ED on November 10, 2020
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Angus DC, Derde L, Al-Beidh F, Annane D, Arabi Y, Beane A, et al. Writing Committee for the REMAP-CAP Investigators. Effect of hydrocortisone on mortality and organ support in patients with severe COVID-19: the REMAP-CAP COVID-19 corticosteroid domain randomized clinical trial. JAMA. 2020;324:1317–1329. doi: 10.1001/jama.2020.17022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, et al. RECOVERY Collaborative Group. Dexamethasone in hospitalized patients with Covid-19 - preliminary report. N Engl J Med. [online ahead of print] 17 Jul 2020; DOI: 10.1056/NEJMoa2021436. [Google Scholar]
- 3. Zhang H, Rostami MR, Leopold PL, Mezey JG, O’Beirne SL, Strulovici-Barel Y, et al. Expression of the SARS-CoV-2 ACE2 receptor in the human airway epithelium. Am J Respir Crit Care Med. 2020;202:219–229. doi: 10.1164/rccm.202003-0541OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Han K, Blair RV, Iwanaga N, Liu F, Russell-Lodrigue KE, Qin Z, et al. Lung expression of human angiotensin-converting enzyme 2 sensitizes the mouse to SARS-CoV-2 infection. Am J Respir Cell Mol Biol. 2021;64:79–88. doi: 10.1165/rcmb.2020-0354OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Winkler ES, Bailey AL, Kafai NM, Nair S, McCune BT, Yu J, et al. SARS-CoV-2 infection of human ACE2-transgenic mice causes severe lung inflammation and impaired function. [Published erratum appears in Nat Immunol 21:1470.] Nat Immunol. 2020;21:1327–1335. doi: 10.1038/s41590-020-0778-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dinnon KH, III, Leist SR, Schäfer A, Edwards CE, Martinez DR, Montgomery SA, et al. A mouse-adapted model of SARS-CoV-2 to test COVID-19 countermeasures. Nature. 2020;586:560–566. doi: 10.1038/s41586-020-2708-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jiang RD, Liu MQ, Chen Y, Shan C, Zhou YW, Shen XR, et al. Pathogenesis of SARS-CoV-2 in transgenic mice expressing human angiotensin-converting enzyme 2. Cell. 2020;182:50–58, e8. doi: 10.1016/j.cell.2020.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gu H, Chen Q, Yang G, He L, Fan H, Deng YQ, et al. Adaptation of SARS-CoV-2 in BALB/c mice for testing vaccine efficacy. Science. 2020;369:1603–1607. doi: 10.1126/science.abc4730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sun SH, Chen Q, Gu HJ, Yang G, Wang YX, Huang XY, et al. A mouse model of SARS-CoV-2 infection and pathogenesis. Cell Host Microbe. 2020;28:124–133, e4. doi: 10.1016/j.chom.2020.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Milne S, Yang CX, Timens W, Bossé Y, Sin DD. SARS-CoV-2 receptor ACE2 gene expression and RAAS inhibitors. Lancet Respir Med. 2020;8:e50–e51. doi: 10.1016/S2213-2600(20)30224-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jacobs M, Van Eeckhoutte HP, Wijnant SRA, Janssens W, Joos GF, Brusselle GG, et al. Increased expression of ACE2, the SARS-CoV-2 entry receptor, in alveolar and bronchial epithelium of smokers and COPD subjects. Eur Respir J. 2020;56:2002378. doi: 10.1183/13993003.02378-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chang EH, Willis AL, Romanoski CE, Cusanovich DA, Pouladi N, Li J, et al. Rhinovirus infections in individuals with asthma increase ACE2 expression and cytokine pathways implicated in COVID-19. Am J Respir Crit Care Med. 2020;202:753–755. doi: 10.1164/rccm.202004-1343LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sun J, Zhuang Z, Zheng J, Li K, Wong RL, Liu D, et al. Generation of a broadly useful model for COVID-19 pathogenesis, vaccination, and treatment. Cell. 2020;182:734–743, e5. doi: 10.1016/j.cell.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hassan AO, Case JB, Winkler ES, Thackray LB, Kafai NM, Bailey AL, et al. A SARS-CoV-2 infection model in mice demonstrates protection by neutralizing antibodies. Cell. 2020;182:744–753, e4. doi: 10.1016/j.cell.2020.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Israelow B, Song E, Mao T, Lu P, Meir A, Liu F, et al. Mouse model of SARS-CoV-2 reveals inflammatory role of type I interferon signaling. J Exp Med. 2020;217:e20201241. doi: 10.1084/jem.20201241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Park A, Iwasaki A. Type I and type III interferons - induction, signaling, evasion, and application to combat COVID-19. Cell Host Microbe. 2020;27:870–878. doi: 10.1016/j.chom.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zhang Q, Bastard P, Liu Z, Le Pen J, Moncada-Velez M, Chen J, et al. COVID-STORM Clinicians; COVID Clinicians; Imagine COVID Group; French COVID Cohort Study Group; CoV-Contact Cohort; Amsterdam UMC Covid-19 Biobank; COVID Human Genetic Effort; NIAID-USUHS/TAGC COVID Immunity Group. Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science. 2020;370:eabd4570. doi: 10.1126/science.abd4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.