Abstract
There is a wide range of emotion regulation (ER)-related impairment observed in autism spectrum disorder (ASD), which is associated with both internalizing and externalizing problems. Although the importance of ER is widely acknowledged in the ASD literature, little is known about factors associated with variability in ER impairment. Given the identified gender differences in ASD, gender may be a potential contributor to ER. This study examined gender differences in ER in an ASD inpatient psychiatric sample (n = 722; 146 females) aged 4–20 years, collected as part of the Autism Inpatient Collection. In addition, the study investigated whether age, nonverbal intelligence quotient (NVIQ), or verbal ability moderate the association between ER and gender. While both male and female inpatients with ASD presented with clinically elevated emotion dysregulation compared to general population norms, results suggest that female psychiatric inpatients have more severe dysregulation, including higher reactivity and dysphoria, than inpatient males. NVIQ and verbal ability did not moderate the association between gender and ER. Age moderated the association between gender and ER, with greater gender difference seen in older individuals, but only for dysphoria. However, overall, these effects were small. Improved understanding of ER presentation in males and females with ASD is critical, as these symptoms may differentially impact individuals with ASD and may warrant a different treatment emphasis.
Keywords: emotion regulation, autism spectrum disorder, gender differences, psychiatric inpatients, Autism Inpatient Collection
Lay Summary:
Previous research has identified several gender differences in presentation of autism spectrum disorder (ASD) symptoms, as well as difficulties with emotion regulation in individuals with ASD. In order to better understand the factors that may contribute to emotion regulation in ASD, this study examined whether psychiatrically hospitalized males and females with ASD differed in emotion regulation and what factors influenced the differences. Results suggest that females with ASD have slightly but significantly more difficulty with emotion regulation compared to males.
Introduction
Emotion regulation (ER), or ability to modify one’s arousal and emotional state to promote adaptive behavior [Gross & Thompson, 2007], is often impaired in autism spectrum disorder (ASD), and this is associated with emotional and behavioral difficulties, such as aggression, depression, and anxiety [Weiss, Riosa, Mazefsky, & Beaumont, 2017]. Although the research suggests that individuals with ASD are more likely to have ER impairments compared to their non-ASD peers [Konstantareas & Stewart, 2006; Mazefsky, Borue, Day, & Minshew, 2014; Nuske et al., 2017; Samson, Hardan, Lee, Phillips, & Gross, 2015], there is a lot of within-ASD variability in ER severity. At this time, very little is known about the factors related to ER in individuals with ASD.
Gender is one under-explored source of potential heterogeneity in ER within the ASD population. Estimates have long reflected that ASD occurs more frequently in males compared to females [Loomes, Hull, & Mandy, 2017]; the reasons for this, as well as correlates of sex differences, remain poorly understood. Emerging research also highlights differences between males and females in symptom presentation and co-occurring psychopathology [Hartley & Sikora, 2009; Mandy et al., 2012; Oswald et al., 2016; Solomon, Miller, Taylor, Hinshaw, & Carter, 2012]. Outside of ASD, gender differences are documented with girls showing greater difficulties regulating their emotions than boys [Bender et al., 2012]. At this time, no studies have explored gender differences in ER in individuals with ASD, which could lead to a better definition of treatment needs as well as identification of potential mechanistic treatment targets. We predicted that females with ASD would show greater ER difficulty compared to males within an inpatient psychiatric sample.
Prior research has pointed to additional characteristics, other than gender, that may be related to ER difficulties in ASD. For example, children with developmental delay show less effective ER strategies [Wilson, Fernandes-Richards, Aarskog, Osborn, & Capetillo, 2007] and have lower scores on the ER subscale of the Bayley Behavior Scales [Baker, Blacher, Crnic, & Edelbrock, 2002] compared to typically developing children. Prior research in the general population has found that ER improves with age [Silvers et al., 2012] and that children, especially boys, with specific language impairment, have lower ER abilities than typical children [Fujiki, Brinton, & Clarke, 2002]. Therefore, it is important to understand how IQ, age, and language ability may impact the association between gender and ER difficulties.
The goal of the present study was to examine gender differences in ER in a psychiatric inpatient sample of individuals with ASD, as this subset of the ASD population presents with more severe impairments in ER that require more individualized care [Gabriels et al., 2012] and are related to high costs of hospitalization and family stress [Marsh, Spagnol, Grove, & Eapen, 2017]. Better understanding of ER among individuals with ASD who require the most intensive services for ER-related problems has the potential to inform treatments. Other advantage of the inpatient population is the wide variability in cognitive, language, and functioning levels [Siegel et al., 2015], which provides a unique opportunity to evaluate if these factors moderate the association between ER and gender.
Method
Participants
Participants were psychiatrically hospitalized patients ages 4–20 years, with a confirmed ASD diagnosis (n = 722; 146 females) recruited from the Autism Inpatient Collection (AIC), a six-site study of patients admitted to specialized inpatient psychiatric units for youth with ASD. See Siegel et al. [2015] for a full description of study methods.
Eligibility for enrollment included: (a) ages of 4–20 years old; (b) score ≥12 on the Social Communication Questionnaire (SCQ; Rutter, Bailey, & Lord, 2003), a screener for ASD, or high suspicion of ASD from the inpatient clinical treatment team; (c) a parent or caregiver available who was proficient in English; and (d) no prisoner status. Only participants with a completed Emotion Dysregulation Inventory (EDI; described under the Measures section) were included. All participants met criteria for ASD based on the Autism Diagnostic Observation Schedule-Second Edition (ADOS-2; Lord et al., 2012), administered during their inpatient stay by a research-reliable examiner. Participant demographic characteristics are summarized in Table 1.
Table 1.
Demographic Characteristics
| Overall sample (n = 722) | Males (n = 576) | Females (n = 146) | P-value | |
|---|---|---|---|---|
| Mean (SD) [range] | ||||
| Age | 12.95 (3.41) [4.00–20.39] | 12.92 (3.48) [4.05–20.39] | 13.08 (3.12) [4.00–20.27] | 0.62 |
| ADOS Comparison Score (overall n = 634)a | 7.94 (1.62) [3–10] | 8.00 (1.61) [3–10] | 7.73 (1.63) [4–10] | 0.09 |
| SCQ (overall n = 670)b | 23.35 (6.92) [1–38] | 23.33 (7.01) [1–38] | 23.44 (6.61) [7–37] | 0.86 |
| Nonverbal IQ (overall n = 601)b | 75.11 (28.23) [30–145] | 75.27 (28.18) [30–145] | 74.45 (28.55) [31–141] | 0.78 |
| EDI Reactivity (overall n = 698)c | 0.84 (0.83) [1.99–2.11] | 0.80 (0.84) [1.99–2.11] | 0.97 (0.78) [1.54–2.11] | 0.03 |
| EDI Dysphoria (overall n = 687)c | 0.55 (0.83) [1.36–2.77] | 0.51 (0.84) [1.36–2.77] | 0.71 (0.78) [1.36–2.56] | 0.01 |
| N (%) | ||||
| Ethnicity (Non-Hispanic/Latino; overall n = 683)d | 635 (92.97) | 505 (92.49) | 130 (94.89) | 0.45 |
| Race (Caucasian) | 610 (84.49) | 483 (83.85) | 127 (86.99) | 0.44 |
| Verbal ability (Non/minimally verbal) | 347 (48.06) | 278 (48.26) | 69 (47.26) | 0.85 |
ADOS Comparison Score is missing for some subjects who were above the age range.
Several participants did not complete the SCQ and nonverbal IQ measure.
Several participants did not complete the items needed to calculate the Reactivity or Dysphoria subscale of the EDI.
Ethnicity was not reported for several of the participants.
Measures
The Autism Diagnostic Observation Schedule, Second Edition (ADOS-2) [Lord et al., 2012] is a semi-structured ASD diagnostic assessment. Two verbal ability categories were created based on which ADOS-2 module was administered, using this instrument’s established language guidelines. Participants were considered minimally verbal if they required administration of an ADOS-2 Module 1 (for preverbal/single words) or Module 2 (phrase speech). Participants were considered verbal if ADOS-2 criteria for the administration of a Module 3 or 4 (verbally fluent adolescents and adults) was met.
The Emotion Dysregulation Inventory (EDI) [Mazefsky et al., 2016; Mazefsky, Yu, White, Siegel, & Pilkonis, 2018] is a 30-item caregiver-report questionnaire that evaluates problems with ER in youth with ASD. EDI raw scores are converted to item-response theory-based theta scores (M = 0, SD = 1) that were derived in an autism sample. EDI scales include (a) Reactivity (EDI-R): poor ER and high emotional intensity and (b) Dysphoria (EDI-D): minimal positive affect and general unease. Mazefsky et al. (2018) tested for differential item functioning based on several factors, including gender, intellectual and verbal ability, finding that none of the final items demonstrated psychometric biases. Therefore, the EDI allows for measurement of emotion dysregulation across the full spectrum of verbal and cognitive abilities in individuals with ASD. Clinical cutoffs for the EDI were derived from a general sample of 1,000 youth matched to the US census on age, gender, race, ethnicity, and region. Cutoffs correspond to 1 SD above the mean in the general US sample (equivalent to a theta score of −0.364 for EDI-R and −0.311 for EDI-D generated via the autism norms) [Mazefsky, Yu, & Pilkonis, in press].
The Leiter International Performance Scale—Third Edition (Leiter-3; Roid, Miller, Pomplun, & Koch, 2013) was administered during the hospital stay by a trained research assistant or psychologist as a test of nonverbal intelligence. The Leiter-3 was not able to be administered to 16.76% of participants (n = 121 participants: 93 male, 28 female).
Data Analyses
For continuous variables, descriptive statistics were computed using means and standard deviations and independent samples t-test was utilized to explore gender differences. For categorical variables, descriptive statistics were computed using frequencies and proportions and a chi-square test was utilized to explore gender differences. Mean differences Cohen’s d was calculated to estimate effect sizes for group comparisons [Cohen, 1988].
Linear regressions were run with gender, the demographic variable of interest (age, NVIQ, and verbal ability), and the gender × demographic variable interaction as independent variables and EDI scores as the dependent variables. For ease of clinical interpretation, the demographic variables of interest were dichotomized. Age was dichotomized into <13 or ≥13, NVIQ was categorized as ≥70 or <70. SAS 9.4 (SAS Institute Inc., Cary, NC) was used for all the analyses. Statistical significance is indicated by P values ≤0.05. Subjects with missing data were excluded from corresponding analyses.
Results
Descriptive Statistics
Descriptive statistics were computed for all demographic variables to characterize the sample (Table 1). Male and female participants did not differ in age, t(720) = −0.49, P = 0.62, ethnicity (Hispanic/Latino vs. Non-Hispanic/ Latino; χ2(1) = 0.97, P = 0.45), or race (Caucasian vs. Other Race; χ2(1) = 0.87, P = 0.44). Male and female participants did not differ on SCQ (t(691) = −0.17, P = 0.86), ADOS Comparison Score (t(632) = 1.70, P = 0.09), NVIQ scores (t(599) = 0.28, P = 0.78) or verbal ability (Non/Minimally Verbal vs. Verbal; χ2(1) = 0.05, P = 0.85).
Gender Differences in Emotion Dysregulation
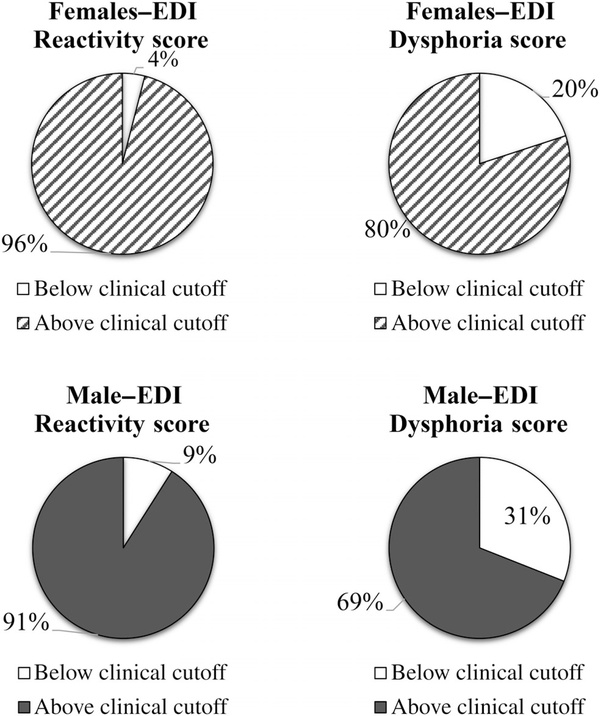
For the entire sample, participants’ scores were at least 2.5 SD higher on the EDI-R and at least 1.3 SD higher on the EDI-D compared to general US youth norms. Females had significantly higher EDI-R (t(696) = −2.24, P = 0.026, d = 0.21) and EDI-D (t(685) = −2.50, P = 0.013, d = 0.24) scores compared to males, though the difference in scores equated to a small effect size (Table 1). Female participants also had higher percentage of clinically elevated EDI-R and EDI-D scores compared to males (Fig. 1).
Figure 1.
Percent of participants with scores above the clinical cutoff (>1 SD above general population from Mazefsky et al., in press) for females (top) and males (bottom) for the reactivity (left) and dysphoria (right) subscales of the EDI.
Moderator Effects of Age, Nonverbal IQ, and Verbal Ability
Results of a model testing the main effects of gender, age, NVIQ, and verbal ability (all dichotomized) on EDI-R and EDI-D as dependent variables are shown in Table 2. Older age and female gender were associated with higher EDI-R scores. Being female and verbal were associated with higher EDI-D scores. Sensitivity analyses leaving age and NVIQ as continuous led to similar conclusions.
Table 2.
Linear Regression Main Effects Models
| Reactivity |
Dysphoria |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variables | b | SE | t | P | b | SE | t | P |
| Gender | −0.18 | 0.08 | −2.11 | 0.035 | −0.25 | 0.09 | −2.86 | 0.004 |
| NVIQ | −0.09 | 0.09 | −1.03 | 0.305 | −0.14 | 0.09 | −1.57 | 0.116 |
| Verbal ability | 0.11 | 0.09 | 1.22 | 0.221 | 0.20 | 0.09 | 2.22 | 0.027 |
| Age | −0.21 | 0.08 | −2.93 | 0.004 | −0.02 | 0.07 | −0.29 | 0.775 |
| Model summary | ||||||||
| F(3, 577) = 3.43, P = 0.009 | F(3, 565) = 3.48, P = 0.008 | |||||||
| R2 = 0.023 | R2 = 0.024 | |||||||
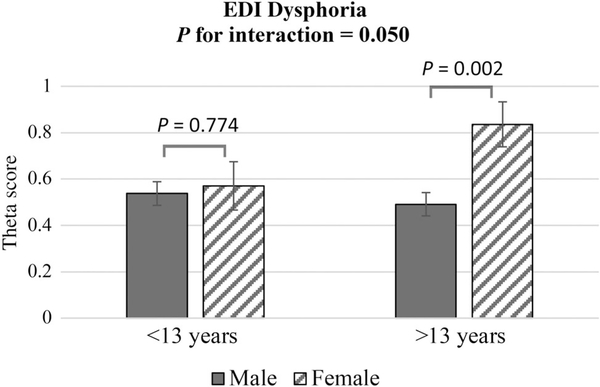
Next, we tested gender × age, gender × NVIQ, and gender × verbal ability interaction effects. We found that age did not significantly impact the association between ER and gender on EDI-R (t(694) = −0.76, P = 0.45; b = −0.12, 95% CI [−0.19, 0.42]). However, age significantly impacted the association between ER and gender on EDI-D (t(686) = −1.96, P = 0.05; b = −0.31, 95% CI [−0.62, 0.00]). As shown in Figure 2, while younger (<13 years) male and female participants did not differ significantly on the EDI-D score (t(683) = 0.29, P = 0.77, d = 0.02), older females (≥13 years) scored significantly higher on the EDI-D subscale compared to older males (t(683) = 3.16, P = 0.002, d = 0.24). This effect, however, was small, with only 1% of the variance in EDI-D scores accounted for by the model including gender, age, and the gender × age interaction effect.
Figure 2.
Theta scores for Dysphoria subscale of the EDI measure for males and females based on age (<13 years and ≥13 years).
Neither NVIQ (EDI-R: t(578) = −0.18, P = 0.86; b = −0.03; EDI-D: t(566) = 0.43, P = 0.66; b = 0.08) nor verbal ability (EDI-R: t(693) = −0.29, P = 0.77; b = −0.05; EDI-D: t(683) = −0.79, P = 0.430; b = −0.13) significantly impacted the association between gender and ER.
Discussion
This study focused on improving understanding of ER problems in a psychiatric inpatient sample with ASD. Gender differences in ER in ASD and factors that increase risk for poor ER are not well understood. Our findings suggest that, while both male and female psychiatric inpatients with ASD present with high rates of clinically elevated emotion dysregulation, females had more severe emotional dysregulation than males. This was true for both aspects of emotion dysregulation measured, suggesting greater impairment for females in terms of high emotional intensity as well as dysphoria.
Research within and outside of ASD has pointed to other factors that are associated with poor ER, including age, verbal ability, and cognitive ability. Beyond gender, we found that being 13 years or older was associated with higher reactivity and being verbal was associated with higher dysphoria. The age-related finding is in contrast to the literature on non-ASD youth which generally finds improved ER with age [Silvers et al., 2012]. However, it is in line with arguments for adolescence being a particularly vulnerable period with poor functioning for those with ASD [Picci & Scherf, 2015]. The finding that verbal youth had higher dysphoria scores supports prior work suggesting that verbal youth with ASD may be more likely to be diagnosed with depression and anxiety [Lerner et al., 2018]. This is particularly noteworthy given that questions have been raised about whether this is an artifact of difficulty detecting those symptoms in less verbal youth and our use of a measure specifically developed for use with any verbal ability and free of psychometric biases based on verbal ability.
We further sought to examine whether the effect of gender on ER was moderated by age, NVIQ, and verbal ability. NVIQ and verbal ability did not influence the association between gender and ER. However, age moderated the association between gender and ER, with greater gender difference in older females for only the dysphoria subscale of the EDI. The observed increase in dysphoria in older females corresponds to increased rates of depression reported in female compared to male adolescents with ASD [Gotham, Brunwasser, & Lord, 2015]. This finding provides further support for reported challenges with depression that females experience from adolescence into adulthood.
The results of this study should be interpreted considering several limitations. First, it is worth emphasizing that even the significant differences were small effects. As such, it will be important for future research to explore other factors that may impact ER directly or moderate gender differences in ER, such as secondary psychiatric diagnoses, adaptive behavior, differences in underlying biological factors (e.g., family history risk, physiological arousal), and other demographic factors. Such factors should be explored in future studies to fully understand ER variability within the ASD population. Future studies should also explore how gender identity compared to biological sex, may impact ER in the ASD population. In addition, all participants were psychiatrically hospitalized. Future research should explore gender differences in ER as well as factors that may contribute to these differences in both typically developing populations and nonhospitalized samples of individuals with ASD. Finally, cognitive assessments were unable to be completed on the full sample.
This is the first study to examine gender differences in ER in an ASD psychiatric sample with varying functioning. The study indicates high rates of emotion dysregulation in this psychiatric study population in general, as most children, male and female, scored above the clinical cutoff for emotion dysregulation. Results indicate the need for treatment with an emphasis on ER strategies. Although the difference in ER between genders was small, females had significantly higher emotion dysregulation in this sample than males. Given the gender disparity in diagnosis of ASD and potential differences in the manifestation of autism traits in females compared to males, there may be a delay in seeking intensive psychiatric care services for females with ASD until they present with more severe behavioral impairments. More research is needed to improve understanding of ER presentation in females with ASD to optimize treatment timing and type that may differ for males and females with ASD. In addition, future studies should employ longitudinal designs, to further explore role of age in moderating the relationship between gender and ER.
Acknowledgments
The development of the EDI was supported by the INSAR Ritvo-Slifka Award for Innovation in Autism Research (to Carla Mazefsky) and the National Institute of Child Health and Human Development (NICHD; R01HD079512 to Carla Mazefsky). The Autism Inpatient Collection (AIC) phenotypic database and biorepository are supported by a grant from the Simons Foundation Autism Research Initiative and the Nancy Lurie Marks Family Foundation (SFARI #296318 to Matthew Siegel).
Ethical Statement
The research involved human participants. The study protocol was approved by the Institutional Review Board at each of the six investigating sites: the Cincinnati Children’s Hospital Medical Center Human Research Program, the Lifespan—Rhode Island Hospital Research Protection Office, the Maine Medical Center Office of Research Compliance, the Sheppard Pratt Institutional Review Board, the University of Pittsburgh Research Conduct and Compliance Office, and the University of Colorado Denver Office of Regulatory Compliance.
Footnotes
Conflicts of Interest
The authors report no potential conflicts of interest.
Contributor Information
Andrea Trubanova Wieckowski, UPMC Western Psychiatric Hospital, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania.
Stephanie Luallin, Department of School Psy- chology, University of Northern Colorado, Greeley, Colorado.
Zhaoxing Pan, Department of Pediatrics, University of Colorado Anschutz Medical Campus, Aurora, Colorado.
Giulia Righi, Department of Psychiatry and Human Behavior, The Warren Alpert Medical School of Brown University, Providence, Rhode Island.
Robin L. Gabriels, Department of Psychiatry and Pediatrics, University of Colorado School of Medicine, Aurora, Colorado.
Carla Mazefsky, Department of Psychiatry, Univer- sity of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania.
References
- Baker BL, Blacher J, Crnic KA, & Edelbrock C (2002). Behavior problems and parenting stress in families of three-year-old children with and without developmental delays. American Journal on Mental Retardation, 107(6), 433–444. [DOI] [PubMed] [Google Scholar]
- Bender PK, Reinholdt-Dunne ML, Esbjørn BH, & Pons F (2012). Emotion dysregulation and anxiety in children and adolescents: Gender differences. Personality and Individual Differences, 53(3), 284–288. [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Earlbaum. [Google Scholar]
- Fujiki M, Brinton B, & Clarke D (2002). Emotion regulation in children with specific language impairment. Language, Speech, and Hearing Services in Schools, 33(2), 102–111. [DOI] [PubMed] [Google Scholar]
- Gabriels RL, Agnew JA, Beresford C, Morrow MA, Mesibov G, & Wamboldt M (2012). Improving psychiatric hospital care for pediatric patients with autism spectrum disorders and intellectual disabilities. Autism Research and Treatment, 2012, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotham K, Brunwasser SM, & Lord C (2015). Depressive and anxiety symptom trajectories from school age through young adulthood in samples with autism spectrum disorder and developmental delay. Journal of the American Academy of Child & Adolescent Psychiatry, 54(5), 369–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ, & Thompson RA (2007). Emotion regulation: Conceptual foundations In Gross JJ (Ed.), Handbook of emotion regulation (pp. 3–24). New York, NY: Guilford Press. [Google Scholar]
- Hartley S, & Sikora D (2009). Sex differences in autism spectrum disorder: An examination of developmental functioning, autistic symptoms, and coexisting behavior problems in toddlers. Journal of Autism and Developmental Disorders, 39, 1715–1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konstantareas MM, & Stewart K (2006). Affect regulation and temperament in children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 36(2), 143–154. [DOI] [PubMed] [Google Scholar]
- Lerner MD, Mazefsky CA, Weber RJ, Transue E, Siegel M, & Gadow KD (2018). Verbal ability and psychiatric symptoms in clinically referred inpatient and outpatient youth with ASD. Journal of Autism and Developmental Disorders, 48(11), 3689–3701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loomes R, Hull L, & Mandy WPL (2017). What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 56(6), 466–474. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore P, Risi S, Gotham K, & Bishop S (2012). Autism diagnostic observation schedule—2nd edition (ADOS-2). Los Angeles, CA: Western Psychological Corporation. [Google Scholar]
- Mandy W, Chilvers R, Chowdhury U, Salter G, Seigal A, & Skuse D (2012). Sex differences in autism spectrum disorder: Evidence from a large sample of children and adolescents. Journal of Autism and Developmental Disorders, 42(7), 1304–1313. [DOI] [PubMed] [Google Scholar]
- Marsh A, Spagnol V, Grove R, & Eapen V (2017). Transition to school for children with autism spectrum disorder: A systematic review. World Journal of Psychiatry, 7(3), 184–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA, Borue X, Day TN, & Minshew NJ (2014). Emotion regulation patterns in adolescents with high-functioning autism spectrum disorder: Comparison to typically developing adolescents and association with psychiatric symptoms. Autism Research, 7(3), 344–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA, Day TN, Siegel M, White SW, Yu L, & Pilkonis PA (2016). Development of the emotion dysregulation inventory: A PROMIS® ing method for creating sensitive and unbiased questionnaires for autism spectrum disorder. Journal of Autism and Developmental Disorders, 48 (11), 3736–3746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA, Yu L, & Pilkonis PA (in press). Psychometric properties of the emotion dysregulation inventory in a nationally representative sample of youth. Journal of Clinical Child & Adolescent Psychology, 1–13. 10.1080/15374416.2019.1703710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazefsky CA, Yu L, White SW, Siegel M, & Pilkonis PA (2018). The emotion dysregulation inventory: Psychometric properties and item response theory calibration in an autism spectrum disorder sample. Autism Research, 11(6), 928–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuske HJ, Hedley D, Woollacott A, Thomson P, Macari S, & Dissanayake C (2017). Developmental delays in emotion regulation strategies in preschoolers with autism. Autism Research, 10(11), 1808–1822. [DOI] [PubMed] [Google Scholar]
- Oswald TM, Winter-Messiers MA, Gibson B, Schmidt AM, Herr CM, & Solomon M (2016). Sex differences in internalizing problems during adolescence in autism spectrum disorder. Journal of Autism and Developmental Disorders, 46(2), 624–636. [DOI] [PubMed] [Google Scholar]
- Picci G, & Scherf KS (2015). A two-hit model of autism: Adolescence as the second hit. Clinical Psychological Science, 3 (3), 349–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roid GH, Miller LJ, Pomplun M, & Koch C (2013). Leiter-3 training DVD: Leiter International Performance Scale. Wood Dale, IL: Stoelting. [Google Scholar]
- Rutter M, Bailey A, & Lord C (2003). SCQ The Social Communication Questionnaire. Torrance, CA: Western Psychological Services. [Google Scholar]
- Samson AC, Hardan AY, Lee IA, Phillips JM, & Gross JJ (2015). Maladaptive behavior in autism spectrum disorder: The role of emotion experience and emotion regulation. Journal of Autism and Developmental Disorders, 45(11), 3424–3432. [DOI] [PubMed] [Google Scholar]
- Siegel M, Smith KA, Mazefsky C, Gabriels RL, Erickson C, Kaplan D, … Santangelo SL (2015). The autism inpatient collection: Methods and preliminary sample description. Molecular Autism, 6(1), 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silvers JA, McRae K, Gabrieli JD, Gross JJ, Remy KA, & Ochsner KN (2012). Age-related differences in emotional reactivity, regulation, and rejection sensitivity in adolescence. Emotion, 12(6), 1235–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon M, Miller M, Taylor SL, Hinshaw SP, & Carter CS (2012). Autism symptoms and internalizing psychopathology in girls and boys with autism spectrum disorders. Journal of Autism and Developmental Disorders, 42, 48–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss JA, Riosa PB, Mazefsky CA, & Beaumont R (2017). Emotion regulation in autism spectrum disorder In Essau CA, LeBlanc S, & Ollendick TH (Eds.), Emotion regulation and psychopathology in children and adolescents (pp. 235–258). New York, NY: Oxford University Press. [Google Scholar]
- Wilson BJ, Fernandes-Richards S, Aarskog C, Osborn T, & Capetillo D (2007). The role of emotion regulation in the social problems of boys with developmental delays. Early Education and Development, 18(2), 201–222. [Google Scholar]