Abstract
OBJECTIVES
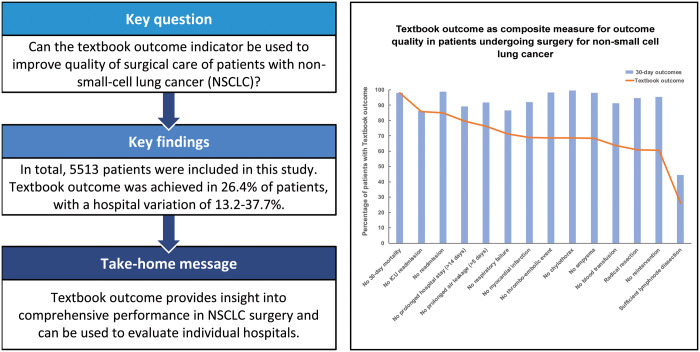
Quality assessment is an important element in providing surgical cancer care. The main objective of this study was to develop a new composite measure ‘textbook outcome’, to evaluate and improve quality of surgical care for patients undergoing a resection for non-small-cell lung cancer (NSCLC).
METHODS
All patients undergoing an anatomical resection for NSCLC from 2012 to 2016 registered in the nationwide Dutch Lung Cancer Audit were included in an analysis to assess usefulness of a composite measure as a quality indicator. Based on expert opinion, textbook outcome was defined as having a complete resection (negative resection margins and sufficient lymph node dissection), plus no 30-day or in-hospital mortality, no reintervention in 30 days, no readmission to the intensive care unit, no prolonged hospital stay (<14 days), no hospital readmission after discharge and no major complications. The percentage of patients with a textbook outcome was calculated per hospital. Between-hospital variation in textbook outcome was analysed using case-mix adjustment models.
RESULTS
In total, 5513 patients were included in this study. Textbook outcome was achieved in 26.4% of patients. Insufficient lymph node dissection had the most substantial effect on not realizing textbook outcome. If ‘sufficient lymph node dissection’ was not included as a criterion, textbook outcome would be 60.7%. Case-mix adjusted textbook outcome proportions per hospitals varied between 13.2% and 37.7%.
CONCLUSIONS
In contrast to focusing on a single aspect, the composite measure textbook outcome provides insight into comprehensive performance in NSCLC surgery. It can be used to evaluate both individual hospitals and national performance and provides the opportunity to give benchmarked feedback to thoracic surgeons.
Keywords: Non-small-cell lung cancer, Textbook outcome, Surgery, Clinical auditing, Postoperative outcome
INTRODUCTION
Clinical auditing is considered an important instrument for quality assessment and improvement of quality of care [1]. National registrations provide data to evaluate the multidimensional quality of cancer care [2]. Traditionally, quality indicators mainly focused on hospital volume and 30- or 90-day mortality [3–6]. To this day, most of these quality indicators are 1-dimensional and will potentially be insufficient to monitor the multidimensional process of lung cancer surgery. Additionally, morbidity and mortality in lung cancer surgery are low; therefore, these outcome indicators have a less discriminating impact and impel less to quality improvement.
Textbook outcome as a multidimensional outcome indicator, indicating the most desirable outcome for a patient, is already being used in other fields of surgery, like colorectal, upper gastrointestinal and elective aneurysm surgery [7–9]. A textbook outcome indicator has not yet been developed for oncological lung surgery.
The main purpose of this study was to develop a new composite quality measure ‘textbook outcome’ for non-small-cell lung cancer (NSCLC) surgery and to analyse hospital variations related to this new quality indicator.
MATERIALS AND METHODS
Data source and study population
Data were derived from the Dutch Lung Cancer Audit—Surgery (DLCA-S) [10]. In 2012 the Dutch Association of Lung Surgeons and the Dutch Association of Cardiothoracic Surgery initiated the DLCA-S. This nationwide, mandatory clinical registry includes all patients undergoing surgery for NSCLC in the Netherlands. Its main purpose is to provide caregivers with feedback on quality of care and to enable a national benchmark. All patients with NSCLC clinical stage IA–IIIA who underwent a parenchymal resection [pneumonectomy, (bi)lobectomy or anatomical segmental resection] from 1 January 2012 to 31 December 2016 were included. A minimum number of items obligatory for each patient for analysis included date of birth, date of surgery, type of parenchymal resection and 30-day mortality or at hospital discharge. Patients with previous thoracic surgery on the ipsilateral side, acute surgery or neoadjuvant induction therapy were excluded. Missing items in comorbidity were considered as no comorbidity. Due to the nature of this study, no patient informed consent or approval of the medical ethical commission was necessary.
Definitions
The definition of ‘textbook outcome’, reflecting an uneventful course after parenchymal lung resection, was based on the expert opinion of the DLCA-S scientific committee. Textbook outcome is achieved when all of the following desired outcomes are realized: a complete resection (negative resection margins [11] and sufficient lymph node dissection), no 30-day or in-hospital mortality, no reintervention [reoperation (video-assisted thoracoscopic surgery/thoracotomy), bronchoscopy for atelectasis, percutaneous drainage] within 30 days after the primary operation, no readmission to the intensive care unit (ICU) or prolonged stay due to complications, no prolonged hospital stay (<14 days), no hospital readmission after discharge, no major complications [defined as prolonged air leakage (≥5 days), respiratory failure (acute respiratory distress syndrome, pulmonary oedema), myocardial infarction, thromboembolic complications, chylothorax, empyema, blood transfusion]. A sufficient lymph node dissection was defined as a dissection or a sampling of a minimum of 3 mediastinal lymph node stations (including at least the subcarinal station) and the hilar and intrapulmonary lymph nodes [12].
Analysis
The proportion of patients achieving a textbook outcome was calculated on both the national and the individual hospital level and for consecutive study years. The χ2 test was used for time trend analysis. Parameters were placed in order of clinical relevance as defined by expert opinion. If data on one of the selected outcome parameters were missing, the patient was considered not to have a textbook outcome.
The proportion of each individual outcome parameter included in the textbook outcome was calculated together with the proportion of patients in whom each subsequent parameter was realized, with the condition that all previous criteria were complied with.
To study the association between patient, tumour and treatment characteristics and textbook outcome, these characteristics were compared between the groups with and without textbook outcome using the χ2 test. Subsequently, patient and tumour covariates in the multivariable logistic regression model were selected based on known factors in the literature and on expert opinion and entered at a P-value of 0.05 using the ENTER method for variable selection in our model. Subgroups with ≤5% missing items were excluded from logistic regression analysis; patients with more than 5% missing items were analysed as a separate group. A multicollinearity test was performed to test collinearity between the covariates. Between-hospital variation in textbook outcome was demonstrated using funnel plots with 95% confidence intervals. For fair between-hospital comparisons, results were case mix adjusted by calculating observed/expected outcome ratios of the covariates from the multivariable logistic regression model [13]. The observed outcome was the number of patients with textbook outcome in a hospital, and the expected outcome was the sum of all patients’ estimated probabilities for textbook outcome. Patient probability estimates were calculated using an Enter model. An observed/expected ratio above 1 suggested a better hospital performance than average; an observed/expected ratio below 1 suggested a worse performance. For each hospital, the 95% confidence interval was calculated and plotted.
No corrections for multiple testing were done. Hospitals with fewer than 20 parenchymal lung resections a year were excluded from the analysis because they did not meet the minimal volume requirement applicable in the Netherlands to minimize statistical artefacts. A P-value <0.05 was considered statistically significant. Statistical analyses were performed in PASW Statistics version 22.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
In total, 5513 patients with stage IA–IIIA NSCLC who had an anatomical parenchymal resection between 2012 and 2016 and who were registered in the DLCA-S were included for analysis. A textbook outcome was achieved in 1430 patients (26.4%) and did not significantly differ among the 4 consecutive years (P = 0.44). Thirty-four patients (0.6%) did not achieve a textbook outcome due to missing data on included outcome parameters.
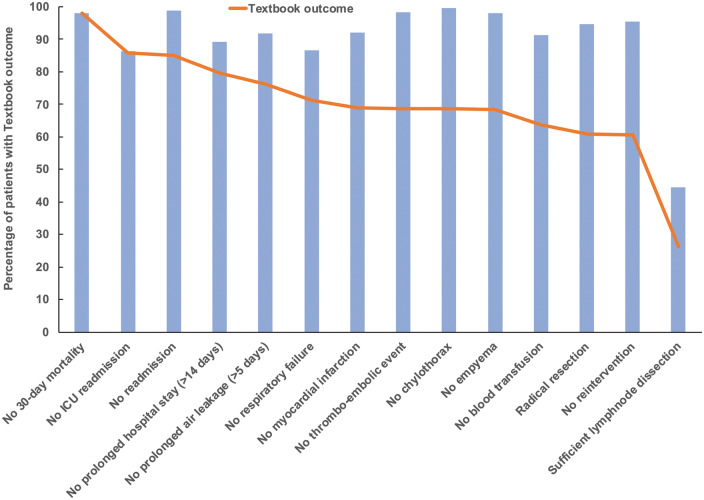
Results for the overall textbook outcome result and the individual outcome parameters are presented in Fig. 1. The most substantial decrease in textbook outcome was due to insufficient lymph node dissection (55.5%), followed by readmission or prolonged stay in the ICU (13.8%) and respiratory failure (13.3%). When lymph node dissection was excluded from the definition, a textbook outcome was achieved in 60.7% of the patients. Patient, tumour and treatment characteristics of patients with and without a textbook outcome are shown in Table 1. Significant differences between the 2 groups were found in sex, age, American Society of Anesthesiologists physical status classification system, cardiac and pulmonal comorbidity, pulmonary function test results and surgical approach, but none were found in other comorbidities, clinical stage or type of resection.
Figure 1:
Diagram representing textbook outcome as composite measure of outcome parameters in patients undergoing surgery for non-small-cell lung cancer (2012–2016). Blue bar: percentage of outcome parameter; orange line: textbook outcome. ICU: intensive care unit.
Table 1:
Tumour and treatment characteristics of patients with textbook outcomes after surgery for non-small-cell lung cancer
| Textbook outcome | No textbook outcome | P-valuea | |
|---|---|---|---|
| (n = 1430), n (%) | (n = 4083), n (%) | ||
| Sex | |||
| Male | 720 (50.3) | 2339 (57.3) | <0.001 |
| Female | 710 (49.7) | 1744 (42.7) | |
| Age (years) | |||
| 20–59 | 329 (23) | 791 (19.4) | 0.003 |
| 60–69 | 561 (39.2) | 1573 (38.5) | |
| 70–79 | 472 (33) | 1459 (35.7) | |
| >80 | 68 (4.8) | 260 (6.4) | |
| ASA group | |||
| I–II | 1120 (78.3) | 3015 (73.8) | <0.001 |
| III–IV | 888 (21.7) | 1068 (26.2) | |
| Charlson score | |||
| 0 | 500 (35) | 1290 (31.6) | 0.055 |
| 1 | 412 (28.8) | 1207 (29.6) | |
| 2+ | 518 (36.2) | 1586 (38.8) | |
| Cardiac comorbidity | |||
| No | 1087 (76) | 2939 (72.0) | 0.003 |
| Yes | 343 (24) | 1144 (28) | |
| Pulmonary comorbidity | |||
| No | 989 (69.2) | 2525 (61.8) | <0.001 |
| Yes | 441 (30.8) | 1558 (38.2) | |
| Diabetes mellitus | |||
| No | 1252 (87.6) | 3533 (86.5) | 0.33 |
| Yes | 178 (1.4) | 550 (13.5) | |
| Neurological comorbidity | |||
| No | 1223 (85.5) | 3478 (85.2) | 0.099 |
| Yes | 207 (14.5) | 605 (14.8) | |
| Thrombotic comorbidity | |||
| No | 1382 (96.6) | 3950 (96.7) | 0.74 |
| Yes | 48 (3.4) | 133 (3.3) | |
| Vascular comorbidity | |||
| No | 908 (63.5) | 2490 (61) | 0.097 |
| Yes | 522 (36.5) | 1593 (39) | |
| DLCO | |||
| >40% | 700 (49) | 2076 (50.8) | <0.001 |
| <40% | 14 (1) | 69 (1.7) | |
| Missing | 716 (50.1) | 1938 (47.5) | |
| FEV1 | |||
| >40% | 456 (31.9) | 1511 (37) | <0.002 |
| <40% | 8 (0.6) | 40 (1) | |
| Missing | 966 (67.6) | 2532 (62) | |
| Clinical stageb | |||
| IA | 586 (41.0) | 1657 (40.6) | 0.96 |
| IB | 319 (22.3) | 934 (22.9) | |
| IIA | 233 (16.3) | 647 (15.8) | |
| IIB | 182 (12.7) | 513 (12.6) | |
| IIIA | 110 (7.7) | 332 (8.1) | |
| Previous thoracic surgery | |||
| No | 1401 (98) | 4013 (98.3) | 0.44 |
| Yes | 29 (2) | 70 (1.7) | |
| Resection | |||
| Pneumonectomy | 118 (8.3) | 281 (6.9) | 0.099 |
| Bilobectomy | 74 (5.2) | 254 (6.2) | |
| Lobectomy | 1201 (84.4) | 3465 (84.9) | |
| Segmental resection | 37 (2.6) | 83 (2) | |
| Approach | |||
| Video-assisted thoracoscopic surgery | 1009 (70.6) | 2762 (67.6) | <0.001 |
| Thoracotomy | 379 (26.5) | 1156 (28.3) | |
| Robot-assisted thoracic surgery | 38 (2.7) | 57 (1.4) | |
| Missing | 4 (0.3) | 108 (2.6) | |
χ 2 test for trend.
TNM 7th edition.
ASA: American Society of Anesthesiologists; DLCO: diffusing capacity of the lung for carbon monoxide (preoperative); FEV1: forced expired volume in 1 s (preoperative).
Multivariable analysis
Independently associated factors, found in the multivariable analysis for achieving textbook outcome for patients with NSCLC, were female gender, young age, American Society of Anesthesiologists score I-II, no pulmonary comorbidity and forced expiratory volume in 1 s >40% (Table 2). No collinearity between the parameters in the multivariable analysis was found.
Table 2:
Multivariable logistic regression analysis of textbook outcome
| OR | 95% confidence interval |
P-value | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Sex | ||||
| Male | REF | 0.001 | ||
| Female | 1.21 | 1.06 | 1.37 | |
| Age (years) | ||||
| 20–59 | REF | 0.016 | ||
| 60–69 | 0.87 | 0.74 | 1.03 | |
| 70–79 | 0.83 | 0.69 | 0.99 | |
| >80 | 0.62 | 0.01 | 0.85 | |
| ASA score | ||||
| I–II | REF | 0.026 | ||
| III–IV | 0.86 | 0.73 | 0.99 | |
| Cardiac comorbidity | ||||
| No | REF | 0.090 | ||
| Yes | 0.88 | 0.76 | 1.02 | |
| Pulmonary comorbidity | ||||
| No | REF | 0.001 | ||
| Yes | 0.75 | 0.65 | 0.86 | |
| Diabetes mellitus | ||||
| No | REF | |||
| Yes | 1.03 | 0.89 | 1.25 | 0.74 |
| DLCO | ||||
| >40% | REF | 0.060 | ||
| ≤40% | 0.56 | 0.32 | 1.02 | |
| Missing | 0.89 | 0.75 | 1.05 | |
| FEV1 | ||||
| >40% | REF | 0.039 | ||
| ≤40% | 0.69 | 0.32 | 1.49 | |
| Missing | 1.19 | 1.02 | 1.37 | |
| Previous thoracic surgery | ||||
| No | REF | 0.43 | ||
| Yes | 1.20 | 0.76 | 1.90 | |
| Clinical stage | ||||
| IA | REF | 0.78 | ||
| IB | 1.01 | 0.89 | 1.19 | |
| IIA | 1.06 | 0.87 | 1.27 | |
| IIB | 1.13 | 0.88 | 1.38 | |
| IIIA | 1.06 | 0.82 | 1.35 | |
ASA: American Society of Anesthesiologists; DLCO: Diffusing capacity for carbon monoxide; FEV1: forced expiratory volume in 1 s; OR: odds ratio.
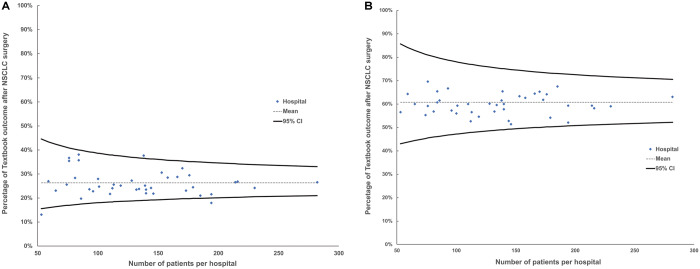
Textbook outcome rates for each hospital in the Netherlands performing NSCLC resections, after case-mix adjustment, are plotted in Fig. 2A. The range of the adjusted textbook outcome of hospitals varied between 13.2% and 37.7%. One hospital with a significantly higher textbook outcome and 2 hospitals with significantly lower rates compared to the national mean textbook outcome, were identified. Figure 2B displays textbook outcome rates with sufficient lymph node dissection excluded. No significant variation was found among the hospitals.
Figure 2:
(A) Funnel plot presenting hospital variation: case-mix adjusted textbook outcome rates for individual hospitals (2012–2016). (B) Funnel plot presenting hospital variation: case-mix adjusted textbook outcome rates for individual hospitals without sufficient lymph node dissection (2012–2016). Blue dot: hospital; 95% CI: 95% confidence interval; NSCLC: non-small-cell lung cancer.
DISCUSSION
To our knowledge, this study is the first to describe a multidimensional outcome measure, textbook outcome, for the assessment of quality of care in lung cancer surgery. This composite measure, including all key surgical outcome parameters, provides insight into the overall quality of surgical care. It can be used to detect potential variations between hospitals, but most importantly to give feedback on overall performance to teams performing thoracic surgery.
Textbook outcome was realized in only 26.4% of the patients after parenchymal lung resection for a stage IA–IIIA NSCLC in our study. The main reasons why textbook outcome could not be achieved were insufficient lymph node dissection and readmission or prolonged stay in the ICU (13.8%), with a median extra admittance of 2 days. The majority of hospitals did not significantly differ in textbook outcome after case-mix adjustment, despite the range of 13.2–38.1%.
Traditionally, 1-dimensional postoperative outcome measures, such as postoperative mortality and morbidity, are considered important indicators to describe the quality of lung surgery. However, event rates of these outcomes are relatively low, which makes them less suitable to detect hospital variation. For example, overall 30-day mortality in this study is 2.1% and comparable with international described rates (2.7%, range 1.5–4.2%) [14, 15]. A composite measure like textbook outcome has a higher event rate and therefore potentially has more discriminative power to identify hospital variations in patient outcomes. Previous studies have presented alternative ways to define composite measures. Nolan and Berwick [16] noted in 2006 new ways to use composite quality indicators, by using the ‘all or nothing’ approach. This concept is also the basis of the textbook outcome concept, which reflects the desired outcome of the patient after treatment. In other words, every step or complication is equally important for the outcome of the patient. Shahian et al. [17] described a set of quality indicators for the development of a composite quality measure for cardiac surgery. Recently, 3 Dutch studies investigated textbook outcome as a composite measure for colorectal surgery, abdominal aorta aneurysm repair and upper gastrointestinal surgery [7–9]. All 3 authors described how the use of a composite measure can help evaluate hospital performance on the overall quality of surgical care and to identify between-hospital variations. For oesophageal and gastric cancer surgery in our country, textbook outcomes increased over the last 5 years from 30% to 44%, mostly by improving lymph node dissections by providing benchmarked feedback to the surgical teams [18]. Mehta et al. [19] described textbook outcome between the top 20 best performing hospitals versus the rest of the hospitals in the USA for oesophageal, liver, colorectal, pancreas and lung surgery. The total textbook outcome for lung surgery in this study was 66.2%. Mehta et al. did not include oncological outcomes as we did in our study; after excluding sufficient lymph node dissections, we achieved a textbook outcome of 60%. Nevertheless, our opinion is that radicality and sufficient lymph node dissection are beneficial for the patient and of importance in textbook outcome.
Yet, our study shows a limited discriminative effect of textbook outcome among hospitals in the Netherlands, because all hospitals have similar moderate results. By presenting hospitals results to the participating centres, comparable improvement of textbook outcomes, like those achieved for oesophageal and gastric cancer, could be pursued. Moreover, if, in an ideal situation, adequate lymph node dissection could be performed in 100% of patients in our country, there would still be substantial room for improvement, if one considers that 40% of the patients in our study also had other reasons for not being considered a textbook outcome.
Textbook outcome provides comprehensive outcome information for caregivers and patients in addition to the already frequently used 1-dimensional outcome measures. Because in the representation of a textbook outcome (Fig. 1), information on the various components is included, it can be used to direct specific improvement potential for hospitals, whereas the composite part puts the information in a broader perspective of quality evaluation. To inform patients, a composite measure may also be more understandable than separate 1-dimensional outcome measures.
Limitations
This study has several limitations. First, the DLCA-S relies on data entered by the hospitals themselves, which could potentially cause (selection) bias. However, to minimalize incomplete or unreliable data entry, several measures like internal and external quality control of the data have been taken, as reported earlier by Hoeijmakers et al. [2, 20].
Second, the textbook outcome definition was based on individual outcome indicators defined in the national lung cancer registry, DLCA-S. The definition of these individual outcome indicators can be discussed, for example, the definition of prolonged hospital stay (>14 days). As an alternative definition, the seventy fifth percentile can be used, which is 10 days, with a median of 7 days in our population. Instead of 89.3% of the patients in the 14-day definition, 79.5% of the patients will have a hospital stay of 10 days or less. This will result in a textbook outcome of 25.1%. In addition, the definition of the European Society of Thoracic Surgeons for sufficient lymph node dissection was used in our analysis. However, other lymph node dissection definitions are used, for example, the National Comprehensive Cancer Network definition, the American Cancer Society definition or that of the International Association for the Study of Lung Cancer [11, 21, 22].
In addition, the quality of the individual lymph node dissection has to be defined. Different definitions of this item make international benchmarking a challenge.
Third, the absence of long-term follow-up data in our definition of textbook outcome can be debated. Because the composite measure is meant for short-cycled feedback on performance to the hospitals participating in the DLCA-S, long-term survival was excluded. Nevertheless, textbook outcome could very well be associated with long-term survival. Recently, van der Werf et al. [23] found a positive correlation between textbook outcome and improved long-term survival for patients who had surgery for oesophageal or gastric cancer. Fourth, the definition used in our study is likely to be insufficient to comprise textbook outcome for the complete spectrum of lung cancer treatments provided to patients. Patients with neoadjuvant therapy, for example, radiotherapy and/or chemotherapy, were excluded, and adjuvant treatments were left out of our study. As of 2016, pulmonologists and radiotherapists joined the DLCA, together encompassing the whole care path of lung cancer patients in Dutch hospitals. This multidisciplinary registration will provide a more comprehensive view on the care path for lung cancer patients and potentially a more complete definition of textbook outcome in the future.
Fifth, in our current definition of textbook outcome, patient-reported outcomes (PROs) were not included because they are not yet included in the DLCA. PROs could give additional information on the outcomes of the care process as experienced and reported by patients, for example, chronic pain due to intercostal nerve damage. However, to implement PROs, an alternative textbook outcome has to be defined with the goal of measuring patient functional outcomes after lung cancer treatment. Additional research will help to determine if PROs will give more profound information to measure quality of care [24].
Finally, textbook outcome as defined in this study does not consider the ‘weight’ of individual parameters in the calculation of the final composite measure.
Future perspectives
The mean national percentage of patients in which textbook outcome was achieved (26.4%) is fairly disappointing and emphasizes the need for quality improvement in lung cancer surgery in the Netherlands. Lymph node sampling, ICU readmission and respiratory failure are particular areas that need attention. In order to improve textbook outcome at both the hospital and the national level, the results will be presented to participating hospitals using the already existing secured web-based environment called MyDLCA-S. Results of individual hospitals will be benchmarked against the national mean and outliers will be offered a visit from the DLCA auditing committee.
Moreover, targeted improvement programmes, like enhanced recovery after thoracic surgery, are developed to focus on the areas that need improvement, to decrease postoperative complications and to improve patient outcomes [25, 26].
A single international supported definition for sufficient lymph node dissection should be developed to enhance international benchmarking and quality improvement.
Future studies, with the collaboration of caregivers and patients, are needed for a more weighted textbook outcome and for more information about the association between textbook outcome and long-term results like survival.
CONCLUSION
In conclusion, textbook outcome is a new composite measure to assess quality in NSCLC surgery. It can be used to evaluate both individual hospital and national performances and between-hospital variations, with the potential to improve the overall quality of NSCLC surgery in the Netherlands.
ACKNOWLEDGEMENTS
The authors thank all surgeons, registrars and administrative nurses who registered patients in the DLCA, as well as the DLCA Scientific Committee.
Conflict of interest: none declared.
Author contributions
Martijn G. ten Berge: Conceptualization; Data curation; Formal analysis; Methodology; Validation; Writing—original draft; Writing—review & editing. Naomi Beck: Conceptualization; Formal analysis; Investigation; Methodology; Writing—original draft; Writing—review & editing. Willem Hans Steup: Conceptualization; Methodology; Validation; Writing—review & editing. Ad F.T.M. Verhagen: Conceptualization; Methodology; Validation; Writing—review & editing. Thomas J. van Brakel: Conceptualization; Methodology; Validation; Writing—review & editing. Wilhelmina H. Schreurs: Conceptualization; Investigation; Methodology; Project administration; Supervision; Validation; Writing—original draft; Writing—review & editing. Michel W.J.M. Wouters: Conceptualization; Formal analysis; Investigation; Methodology; Project administration; Supervision; Validation; Writing—original draft; Writing—review & editing.
Reviewer Information
European Journal of Cardio-Thoracic Surgery thanks Georges Decker, Tomasz Grodzki, Miguel Congregado and the other, anonymous reviewer(s) for their contribution to the peer review process of this article.
ABBREVIATIONS
- DLCA-S
Dutch Lung Cancer Audit—Surgery
- ICU
Intensive care unit
- NSCLC
Non-small-cell lung cancer
- PROs
Patient-reported outcomes
Presented at the 27th European Conference on General Thoracic Surgery, Dublin, Ireland, 9–12 June 2019.
REFERENCES
- 1. Dijs-Elsinga J, Otten W, Versluijs MM, Smeets HJ, Kievit J, Vree R. et al. Choosing a hospital for surgery: the importance of information on quality of care. Med Decis Making 2010;30:544–55. [DOI] [PubMed] [Google Scholar]
- 2. Beck N, van Bommel AC, Eddes EH, van Leersum NJ, Tollenaar RA, Wouters MW.. The Dutch Institute for clinical auditing. Ann Surg 2020;271:627–31. [DOI] [PubMed] [Google Scholar]
- 3. Donabedian A. Evaluating the quality of medical care. Milbank Q 2005;83:691–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Birkmeyer JD, Dimick JB, Birkmeyer N.. Measuring the quality of surgical care: structure, process, or outcomes? J Am Coll Surg 2004;198:626–32. [DOI] [PubMed] [Google Scholar]
- 5. Mainz J, Hansen A, Palshof T, Bartels PD.. National quality measurement using clinical indicators: the Danish National Indicator Project. J Surg Oncol 2009;99:500–4. [DOI] [PubMed] [Google Scholar]
- 6. von Meyenfeldt EM, Gooiker GA, van Gijn W, Post PN, van de Velde CJH, Tollenaar R. et al. The relationship between volume or surgeon specialty and outcome in the surgical treatment of lung cancer: a systematic review and meta-analysis. J Thorac Oncol 2012;7:1170–8. [DOI] [PubMed] [Google Scholar]
- 7. Kolfschoten NE, Kievit J, Gooiker GA, Van Leersum NJ, Snijders HS, Eddes EH. et al. Focusing on desired outcomes of care after colon cancer resections; Hospital variations in “textbook outcome”. Eur J Surg Oncol 2013;39:156–63. [DOI] [PubMed] [Google Scholar]
- 8. Karthaus EG, Lijftogt N, Busweiler LAD, Elsman BHP, Wouters M, Vahl AC. et al. Textbook outcome: a composite measure for quality of elective aneurysm surgery. Ann Surg 2017;266:898–904. [DOI] [PubMed] [Google Scholar]
- 9. Busweiler LAD, Schouwenburg MG, van Berge Henegouwen MI, Kolfschoten NE, de Jong PC, Rozema T. et al. ; the Dutch Upper Gastrointestinal Cancer Audit (DUCA) Group. Textbook outcome as a composite measure in oesophagogastric cancer surgery. Br J Surg 2017;104:742–50. [DOI] [PubMed] [Google Scholar]
- 10. ten Berge M, Beck N, Heineman DJ, Damhuis R, Steup WH, van Huijstee PJ. et al. Dutch Lung surgery audit: a national audit comprising lung and thoracic surgery patients. Ann Thorac Surg 2018;106:390–7. [DOI] [PubMed] [Google Scholar]
- 11. Rami-Porta R, Wittekind C, Goldstraw P; International Association for the Study of Lung Cancer (IASLC) Staging Committee. Complete resection in lung cancer surgery: proposed definition. Lung Cancer 2005;49:25–33. [DOI] [PubMed] [Google Scholar]
- 12. De Leyn P, Lardinois D, Van Schil PE, Rami-Porta R, Passlick B, Zielinski M. et al. ESTS guidelines for preoperative lymph node staging for non-small cell lung cancer. Eur J Cardiothorac Surg 2007;32:1–8. [DOI] [PubMed] [Google Scholar]
- 13. Daley J, Khuri SF, Henderson W, Hur K, Gibbs JO, Barbour G. et al. Risk adjustment of the postoperative morbidity rate for the comparative assessment of the quality of surgical care: results of the National Veterans Affairs Surgical Risk Study. J Am Coll Surg 1997;185:328–40. [PubMed] [Google Scholar]
- 14.ESTS Silverbook. 2015. http://www.ests.org (29 May 2020, date last accessed).
- 15. Rich AL, Tata LJ, Stanley RA, Free CM, Peake MD, Baldwin DR. et al. Lung cancer in England: information from the National Lung Cancer Audit (LUCADA). Lung Cancer 2011;72:16–22. [DOI] [PubMed] [Google Scholar]
- 16. Nolan T, Berwick DM.. All-or-none measurement raises the bar on performance. J Am Med Assoc 2006;295:1168–70. [DOI] [PubMed] [Google Scholar]
- 17. Shahian DM, Edwards FH, Ferraris VA, Haan CK, Rich JB, Normand SLT. et al. Quality measurement in adult cardiac surgery: part 1—conceptual framework and measure selection. Ann Thorac Surg 2007;83 (4 Suppl):S3–12. [DOI] [PubMed] [Google Scholar]
- 18.Dutch Institute for Clinical Auditing. Dutch Inst. Clin. Audit. http://www.dica.nl (29 May 2020, date last accessed).
- 19. Mehta R, Tsilimigras DI, Paredes AZ, Sahara K, Moro A, Farooq A. et al. Comparing textbook outcomes among patients undergoing surgery for cancer at U. S. News & World Report ranked hospitals. J Surg Oncol 2020;121:927–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hoeijmakers F, Beck N, Wouters M, Prins HA, Steup WH.. National quality registries: how to improve the quality of data? J Thorac Dis 2018;10:S3490–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Comprehensive Cancer Network Non-Small Cell Lung Cancer Guidelines version 2. 2012. Principles of Surgical Therapy. http://www.nccn.org (29 May 2020, date last accessed).
- 22. Darling GE, Allen MS, Decker PA, Ballman K, Malthaner RA, Inculet RI. et al. Randomized trial of mediastinal lymph node sampling versus complete lymphadenectomy during pulmonary resection in the patient with N0 or N1 (less than hilar) non-small cell carcinoma: results of the American College of Surgery Oncology Group Z0030 trial. J Thorac Cardiovasc Surg 2011;141:662–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. van der Werf LR, Wijnhoven BPL, Fransen LFC, van Sandick JW, Nieuwenhuijzen GAP, Busweiler LAD. et al. A national cohort study evaluating the association between short-term outcomes and long-term survival after esophageal and gastric cancer surgery. Ann Surg 2019;270:868–76. [DOI] [PubMed] [Google Scholar]
- 24. Mak KS, Van Bommel ACM, Stowell C, Abrahm JL, Baker M, Baldotto CS. et al. Defining a standard set of patient-centred outcomes for lung cancer. Eur Respir J 2016;48:852–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ljungqvist O, Scott M, Fearon KC.. Enhanced recovery after surgery a review. JAMA Surg 2017;152:292–8. [DOI] [PubMed] [Google Scholar]
- 26. Batchelor TJP, Rasburn NJ, Abdelnour-Berchtold E, Brunelli A, Cerfolio RJ, Gonzalez M. et al. Guidelines for enhanced recovery after lung surgery: recommendations of the Enhanced Recovery after Surgery (ERAS®) Society and the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg 2019;55:91–115. [DOI] [PubMed] [Google Scholar]