Abstract
As the global response to COVID-19 continues, nurses will be tasked with appropriately triaging patients, responding to events of clinical deterioration, and developing family-centered plans of care within a healthcare system exceeding capacity. Predictive analytics monitoring, an artificial intelligence (AI)-based tool that translates streaming clinical data into a real-time visual estimation of patient risks, allows for evolving acuity assessments and detection of clinical deterioration while the patient is in pre-symptomatic states. While nurses are on the frontline for the COVID-19 pandemic, the use of AI-based predictive analytics monitoring may help cognitively complex clinical decision-making tasks and pave a pathway for early detection of patients at risk for decompensation. We must develop strategies and techniques to study the impact of AI-based technologies on patient care outcomes and the clinical workflow. This paper outlines key concepts for the intersection of nursing and precision predictive analytics monitoring.
Keywords: Continuous predictive analytics monitoring, Precision surveillance, Nursing, COVID-19, Clinical deterioration, Acuity assessment
What is already known about this topic?
-
•
The advent of predictive analytics allows for many applications to nursing practice and science including the use of precision predictive analytics monitoring to allow for early detection of clinical deterioration when patients are not yet showing clinical signs of impending deterioration.
-
•
Nurses are critical to move from artificial intelligence (AI) creation to implementation in a complex learning health system.
What does this paper add?
-
•
This paper introduces the concept of precision predictive analytics monitoring, or AI-based tool that translates streaming clinical data into a real-time estimation of patient risks, allows for evolving acuity assessments and detection of clinical deterioration while the patient is in pre-symptomatic states.
-
•
Here, we explore the intersections of nursing practice, nursing science, and precision predictive analytics monitoring with unique considerations during the COVID-19 pandemic.
The World Health Organization (WHO) has announced the year 2020 as Year of the Nurse and Midwife as recognition of the bicentenary celebration of Florence Nightingale's birth (Lucas and Horton, 2020; Tume and Trapani, 2020; Bell and Brysiewicz, 2020). The WHO designation recognizes the unique contribution of nurses in health care delivery and overall population health, culminating in a report highlighting the state of the global nursing workforce (Tume and Trapani, 2020). There has been an ongoing recognition of the fragility of the global nursing workforce and the simultaneous rising acuity of many patients being cared for in the hospital setting (Brugha and Crowe, 2015; Sir et al., 2015). Concurrently, 2020 is also the year that the novel Severe Acute Respiratory Syndrome Coronavirus 2 [SARS-CoV-2] also known as Coronavirus Disease 19 (COVID-19) has been named a global pandemic by the WHO (Mahase, 2020). Nurses are on the front line of care delivery and are providing care to patients at risk for uncertain trajectories of illness including rapid clinical deterioration and death within hospital units operating beyond maximum capacity (Lancet, 2020; Zhou et al., 2020). As the global response to COVID-19 continues, health care systems have encountered operations exceeding capacity and an overstretched nursing workforce (Lancet, 2020). The purpose of this manuscript is to introduce the use of artificial-intelligence (AI) based technologies at the point of care and discuss the role of nursing at the socio-technical interface of clinical care delivery, research, and AI.
1. Precision predictive analytics monitoring within a learning health system
Nursing roles and responsibilities will continue to evolve during the COVID-19 pandemic. Even when on the acute care hospital floor and intensive care unit under routine circumstances, many patients will have complications or events of rapid clinical deterioration that prolong their stay and increase their overall morbidity and mortality (Wang et al., 2017; Keim-Malpass et al., 2019; Moss et al., 2016). One way to optimize appropriate acuity assessment, accurately determine patients who are at risk for clinical deterioration and determine appropriate clinical actions is through precision predictive analytics monitoring; by this, we mean the use of quantitative tools and statistical models to detect clinical deterioration before overtly catastrophic presentations (Moss et al., 2017). Patients infected with COVID-19 have demonstrated rapid and unpredictable events of clinical deterioration leading to sepsis, intensive care unit utilization, and death, and use of precision predictive analytic systems can allow for early detection for appropriate clinical action or upgrade in care (Ruan et al., 2020). As such, these technologies have uses in a variety of settings including the acute care wards, the emergency department, and the intensive care unit (ICU).
Advances in continuous bedside monitoring technology capabilities make a wealth of data available to healthcare providers for use in patient evaluation (Moss et al., 2017; Keim-Malpass et al., 2018; Ruminski et al., 2019). These data form the foundation for computational algorithms that integrate real-time bedside physiologic monitoring data to provide early warning of potentially catastrophic clinical events, including sepsis, respiratory distress, cardiac instability, and the need to upgrade to ICU level care (Moss et al., 2016; Clark et al., 2016; Moss et al., 2014; Fairchild et al., 2013; Lake et al., 2002; Lake and Moorman, 2011; Lake et al., 2014). Precision predictive analytics monitoring involves an advanced mathematical analysis of data from a variety of inputs (including cardiorespiratory monitoring using streaming ECG data to perform additional waveform calculations such as measurement of RR intervals, measures of entropy and heart rate variability; laboratory data from the electronic medical record; and nurse entered vital signs and assessments) to derive an estimate of fold-increase in the risk of clinical deterioration that clinicians can observe in real-time in a streaming environment (Moss et al., 2017; Lake et al., 2014). In the neonatal setting, Moorman and colleagues detected abnormal heart rate characteristics in the hours preceding a clinical diagnosis of sepsis and developed a computational model that yielded the fold-increase in the risk of sepsis in the next 24 h (Moss et al., 2014; Lake et al., 2002). When 3000 very low birth weight neonates were randomized to display, or not, of the risk of imminent sepsis, there was a 20% decrease in mortality among those whose display was shown (Aschner, 2012; Moorman et al., 2011).
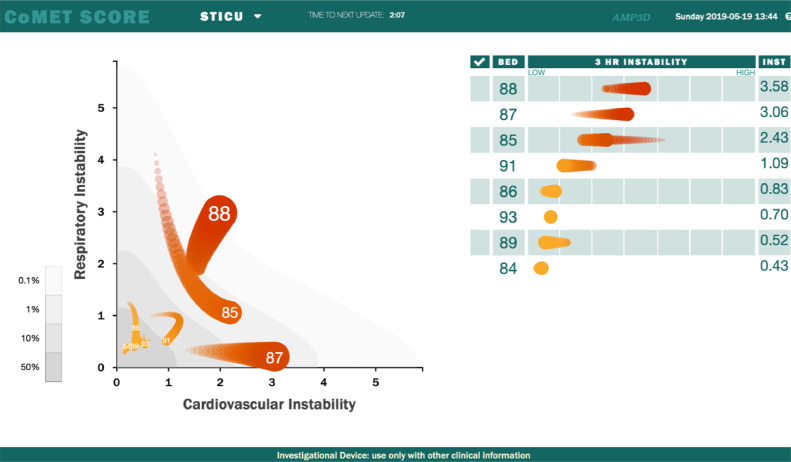
The mathematical approach of precision predictive analytics monitoring has since been extended to acute and critically ill adults and critically ill children in the pediatric intensive care unit by first determining physiologic signatures of illness (Moss et al., 2016; Spaeder et al., 2019). A unique construct inherent in this approach is the use of advanced computational analyses from ECG waveforms to allow for early detection of prodromes. These signatures of illness or prodromes can be discerned through a change in computational risk, but are often not yet able to be detected through clinical signs in early stages. In other words, an abrupt and sustained change in risk score often allows for several hours of advanced warning prior to the earliest (and often subtle) signs of clinical change (Keim-Malpass et al., 2019; Moss et al., 2016; Ruminski et al., 2019). Subsequently, validated algorithms for early detection of subacute events of clinical deterioration were developed and displayed through continuous streaming environments, called CoMET (Continuous Monitoring of Event Trajectories; Advanced Medical Predictive Devices, Diagnostics, and Displays, Charlottesville, VA) (Fig. 1) (Ruminski et al., 2019).
Fig. 1.
This figure demonstrates an example of a display of the relative risk of patients in an intensive care unit for respiratory (y-axis) and cardiovascular (x-axis) decompensation. The current risk is displayed as the head of the comet, and recent trends displayed as the 3-h tail.
Novel precision predictive analytics present a way for nurses, physicians, respiratory therapists, and clinicians at all points of care to be able to visualize changes in patients’ risks over time particularly with ever-changing clinical illness trajectories. Another unique aspect of the precision approach is that it allows for continuous predictive analytics (derived from continuous ECG waveform computations collected every 2 s with a risk score updated every 15 min) to estimate a patient's changing risk, which in turn informs clinical reasoning and decision-making (Ruminski et al., 2019). For example, a patient can have a high baseline acuity or risk score from underlying conditions, but access to novel precision predictive analytics monitoring allows clinicians to employ tailored alert or assessment strategies governed by a continual re-stratification of risk. While other forms of early warning systems also allow you to follow trends, visual analytics such as CoMET present the trend over the past three hours within the visual display of the presented (specifically the CoMET “tail), the size of the CoMET score displayed corresponds with greater risk, and the clinician can access trends over the past 72 h within on a large LCD display and touchpad. Additionally, clinicians can assess response to therapies or response to escalation in care in real-time. Precision predictive analytics monitoring offers a visual display of the patient's risk trajectory and can allow for personalized trend assessment instead of using arbitrary cut-points or alert thresholds for action (Blackwell et al., 2020). Even if the patient is not on continuous ECG monitoring within an acute care ward environment, CoMET can still incorporate the static assessments (vital sign and laboratory data when available) and visualize the risk, including the trajectory of risk and change over time.
Beyond the personalized aspect, the models themselves are based on clinical deterioration outcomes that are specific to certain clinical populations (e.g.,. acute care ward, versus ICU, versus emergency department) (Ruminski et al., 2019; Blackwell et al., 2020; Glass et al., 2020; Blackburn et al., 2017; Politano et al., 2013; Moss et al., 2015; Blackburn et al., 2018). These novel precision predictive analytics differ than most risk scores for clinical deterioration used in hospitals such as NEWS, MEWS and others that rely on static and intermittently collected nurse-entered vital sign parameters that can only be updated following vital sign collection. This means that a new risk picture is only available every 4 or 8 h on the acute care wards or every hour in the intensive care setting (The Royal College of Physicians 2012; Williams et al., 2012; Escobar and Dellinger, 2016; Escobar et al., 2012; Rothman et al., 2013; Churpek et al., 2016; Raith et al., 2017). (If they are being assessed more frequently there are likely already other indications that would lead the nurse to assume the patient is at a higher risk for decompensation and early warning is of less clinical value.) Further, most of these canonical early warning scores were trained only on one clinical deterioration outcome, a one-size-fits-all modeling approach that clinicians might question (Rothman et al., 2013; Churpek et al., 2016; Rothman et al., 2017; Physicians, 2012; Green et al., 2018). Finally, they generally use cut-offs to award points for illness severity, and lose fine degrees of changes within ranges of normal and abnormal (Blackwell et al., 2020; Giannoni et al., 2014).
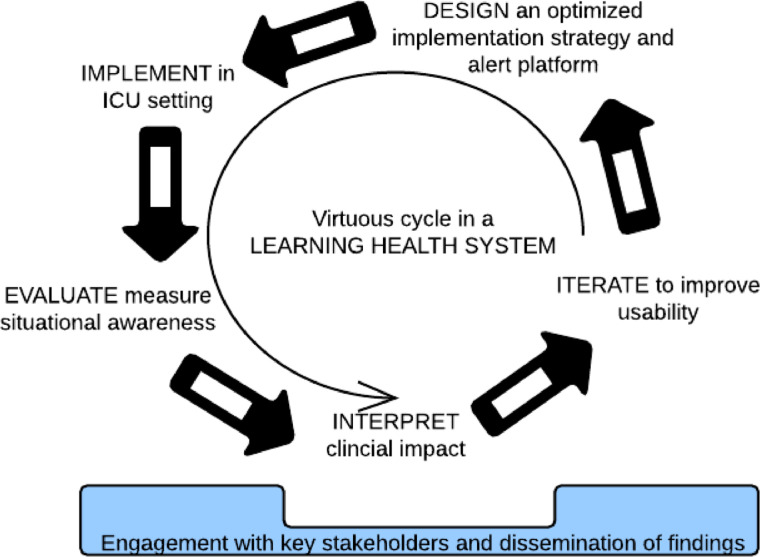
Clinicians at the point of care during a global pandemic must engage with the risk estimates in the context of a learning health system (LHS), or an integrated health system in which informatics and care culture align for optimal patient outcomes (Fig. 2) (Institute of Medicine (US), 2011; Friedman et al., 2017, 2010). As the Institute of Medicine report entitled “Digital Infrastructure for the Learning Health System” suggests, digital health infrastructures (including predictive analytics, risk predictions, and use of AI in healthcare) will be central to the healthcare of the future and necessary for continued improvement in patient outcomes (Institute of Medicine (US), 2011). It is estimated that upwards of 90% of clinical decisions will soon be supported by accurate, timely, and up-to-date digital clinical information in the near future (Institute of Medicine (US), 2011). In order to keep pace, we must simultaneously study the clinical processes necessary in responding to emerging precision predictive analytics monitoring. We must also develop innovative approaches for health systems and individual clinicians to understand the benefits and consequences of implementing and acting on risk predictions. Finally, we must be aware of the inherent pressures of an already extended clinical workforce during the global COVID-19 pandemic and work alongside nurse stakeholders to utilize models that allow them to use the correct risk scores at the right time to make the right clinical actions in a way that is synergistic to their current practices (Keim-Malpass et al., 2018). Beyond clinical use features, a LHS allows precision predictive analytics monitoring to re-train underlying statistical models and be updated while more events of COVID-19 are treated within a system.
Fig. 2.
Learning Health System Schema.
2. Situational awareness and translation from risk prediction to clinical action
Optimized use of precision continuous predictive analytics monitoring relies on theoretical underpinnings of situational analysis, as first conceptualized by Endsley (1995) and applied to the field of engineering, human factors, and ergonomics research. Endsley explored the relationship between situational awareness and environmental and individual factors that impact dynamic decision making and performance of subsequent action(s) (Endsley, 1995). Among these factors, limited attention and working memory have been identified as critical components preventing ‘operators’ from acquiring and interpreting information from the environment in real-time (Endsley, 1995). These elements have been demonstrated in a variety of settings including aviation/air traffic control, military command, and among clinicians in complex healthcare environments (Endsley, 1995). Through our preliminary qualitative research among over 40 adult surgical and neonatal clinicians, we have found that elements of situational awareness are a critical antecedent necessary prior to initiating clinical action in response to a change in risk score presented by precision continuous predictive analytics monitoring (Keim-Malpass et al., 2018; Kitzmiller et al., 2019). A balanced approach between the development of meaningful analytics and engaged situational awareness among nurses on the acute care floor or ICU is critical, so attention and working memory can be properly devoted to dynamic decision making and translation to relevant clinical actions (Stubbings et al., 2012). In the fight against COVID-19 investment in clinical decision support infrastructure and systems can allow nurses to better optimize care delivery and assessments of risk in ways that allow them to be proactive in care delivery. Fig. 3 depicts how ‘Level 3’ of situational awareness, or the projection and action based on a future status (as opposed to perception or comprehension current situation) is the most challenging level to achieve particularly in the context of dynamic acute and intensive care settings with numerous other clinical elements competing for attention. Precision predictive analytics monitoring is attempting to intervene on Level 3, and in order to be successful must add additional value to clinical decision-making while not becoming another form of technology that contributes to unnecessary alert fatigue (Keim-Malpass et al., 2019, 2018).
Fig. 3.
Conceptual model of situational awareness in dynamic decision making.
Paradoxically, the alarm and alert systems that are created to enhance patient safety have become an emerging patient safety concern. In the ICU, the bedside cardiorespiratory monitor alone generates, on average, 187 audible alarms per day averaging 1 per every 7.7 min with upwards of 90% of them being non-actionable (Drew et al., 2014; Aboukhalil et al., 2008; Joshi et al., 2017; Schondelmeyer et al., 2019; McClure et al., 2016). Clinicians become accustomed to ignoring non-actionable or false alarms and in doing so may overlook alarms in a true emergent situation, otherwise known as ‘alarm fatigue’ (Winters et al., 2018; Poole and Shah, 2018). Precision predictive analytics monitoring that rely on alert strategies must be designed to assess and account for alarm fatigue within the design and implementation in order to offset unintended consequences. Further, there is a need to examine whether some existing alarm systems can be removed when predictive analytics are added into the acute care floor ICU environment.
3. Nurses are first responders to the global pandemic – how could precision analytics help?
3.1. Nurses already are and will continue to be first responders in the context of the global
COVID-19 pandemic and pandemics of the future. In the acute and intensive care setting, clinical bedside nurses are with the patient continuously and already tasked with monitoring a diverse array of vital signs and data inputs (Kane-Gill et al., 2017; Warttig et al., 2018; Bose et al., 2016). Nurses use this information to initiate patient-centered interventions and communicate subtle changes in patient status to their physician colleagues with the ultimate goal of (1) reducing catastrophic events and complications for their patients and (2) determining overall clinical stability to promote nursing care that is beneficial to overall clinical outcomes. Precision predictive analytics monitoring demonstrates the potential to synthesize and compute diverse data inputs through visual risk estimates that nurses can interface with and transform care from reactive to proactive. In doing so, nurses can aid in the dynamic decision-making processes to pinpoint physiological acuity assessment and help to (1) refine the correct intensity of care delivery (home, acute care, intensive care); (2) determine early warning for patients at risk of clinical deterioration and refine clinical interventions; (3) define when an upgrade in intervention is needed, for instance defining the need for extracorporeal membrane oxygenation among COVID-19 patients or when a patient should be transferred to a higher level of care; (4) add additional information to inform a nurses’ worry or “gut feeling” that a patient is at risk for clinical deterioration (Douw et al., 2015; Romero-Brufau et al., 2019; Griffin et al., 2007).
4. Conclusion
Within the context of an LHS, nurses are integral in linking patient risk scores to the appropriate clinical actions based on dynamic decision-making processes, and as such they are central to understanding the correct clinical actions to take for patients at risk of clinical deterioration due to COVID-19. Beyond identifying those at risk for clinical deterioration, precision predictive analytics monitoring can also be used to assess a patient's response to therapy over time along with the overall trajectory of illness for enhanced prognostication and initiation of goal-concordant communication to family members. Precision predictive analytics monitoring can also enhance the quality of nurse assessments and interventions by adding another physiomarker component into the overall assessment that can be treated like a vital sign trend and incorporated into routine care (Keim-Malpass et al., 2018; Kitzmiller et al., 2019). Following trends in computational physiomarkers can allow for enhanced nurse autonomy in decision-making and communication processes, particularly during times when clinicians are cognitively burdened. Evolving AI frameworks that allow the nurse to be a stakeholder in development, implementation, and evaluation within a learning health system have the opportunity to optimize patient care delivery and clinical nursing practice.
The primary goal of precision predictive analytics monitoring is to draw attention to a patient who may have a change in risk, but is not exhibiting overt clinical signs that are indicative of imminent deterioration. These technologies do not operate in isolation and are only successful when paired with clinicians’ careful assessment. Perhaps a change in heart rate variability, undetected clinically but calculated computationally, leads an increase in risk score, garners the attention of the nurse to re-assess the patient, and communicate this finding with the physician team. Perhaps they were undecided about sending a blood culture earlier in the day, but this new finding pushes the decision-making towards obtaining a needed blood culture earlier than would have been obtained otherwise. In a different patient there may be a few subtle changes in vital sign characteristics and laboratory results that when assessed independently are not outside of normal limits, but when that risk is combined cumulatively represents a physiological change for that patient. The impact of precision predictive analytics monitoring technologies has the potential to change the clinical paradigm from reactive to proactive. The utility depends on situational awareness: perceiving and comprehending data, and projecting that comprehension into the future in order to alter the patient's trajectory. The implementation centers on assigning specific responsibilities and tasks: Who watches the data? (i.e., a routine bedside nurse or a clinician designated to monitor the technology from a distance, such as an eICU?) (Buchman et al., 2017) Who organizes the data into a coherent picture? An individual or a team? Who acts to change the clinical course and how? What are the trade-offs to the clinical health system? Because these forms of AI technology are new, there are many unanswered questions about the best ways to use precision predictive analytics monitoring in routine clinical practice and nurses are central to answering them through continued clinical research and integration in clinical practice through implementation science perspectives.
Nurses will be leaders in the implementation and the coupling of AI systems with human decision-making, relevant communication, and care. Beyond the critical role of learning to recognize patterns of deterioration, there is much attention needed to understand ability or willingness of the point-of-care team to comprehend and act. Indeed, the team is already overwhelmed with tasks. As such, AI-based precision predictive analytics monitoring implementation and education considerations should involve nursing as a key member of the interdisciplinary team. Precision predictive analytics monitoring have already been implemented in direct response to the COVID-19 pandemic through the use of focused implementation and education efforts and prolonged clinical engagement. As the COVID-19 pandemic continues, approaches to acuity assessment and early detection of clinical deterioration will warrant novel perspectives. Precision predictive analytics integrated within a learning health system may offer promise in optimizing clinical nursing decision-making and expand the field of nursing science.
Declaration of Competing Interest
LPM declares a conflict of interest as she is Chief Implementation Officer and shareholder in AMP3D, Charlottesville, VA, USA.
Acknowledgments
Acknowledgement
The authors would like to acknowledge and thank (1) J. Randall Moorman, MD, for his brilliant review of this manuscript – “great stuff”, and (2) Doug E. Lake, PhD, for providing the inspiration to one day use precision predictive analytics to be a top 5 finisher in the sepsis challenge.
Contribution
JKM conceptualized the manuscript. JKM and LPM wrote and edited the manuscript.
Funding
JKM was funded through the Gordon and Betty Moore Research Fund as a Betty Irene Nurse Fellow that supported this paper.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ijnsa.2021.100019.
Appendix. Supplementary materials
References
- Aboukhalil A, Nielsen L, Saeed M, Mark RG, Clifford GD. Reducing false alarm rates for critical arrhythmias using the arterial blood pressure waveform. J. Biomed. Inform. 2008;41(3):442–451. doi: 10.1016/j.jbi.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aschner Fairchild K. HeRO monitoring to reduce mortality in NICU patients. RRN. 2012:65. doi: 10.2147/RRN.S32570. [DOI] [Google Scholar]
- Bell SA, Brysiewicz P. 2020 year of the nurse and midwife: meeting new challenges. Int. Emerg. Nurs. 2020;49 doi: 10.1016/j.ienj.2020.100848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackburn HN, Clark MT, Moorman JR, Lake DE, Calland JF. Identifying the low risk patient in surgical intensive and intermediate care units using continuous monitoring. Surgery. 2018;163(4):811–818. doi: 10.1016/j.surg.2017.08.022. [DOI] [PubMed] [Google Scholar]
- Blackburn HN, Clark MT, Moss TJ, et al. External validation in an intermediate unit of a respiratory decompensation model trained in an intensive care unit. Surgery. 2017;161(3):760–770. doi: 10.1016/j.surg.2016.09.018. [DOI] [PubMed] [Google Scholar]
- Blackwell JN, Keim-Malpass J, Clark MT, et al. Early detection of in-patient deterioration. Crit. Care Explor. 2020;2(5):e0116. doi: 10.1097/CCE.0000000000000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bose E, Hoffman L, Hravnak M. Monitoring cardiorespiratory instability: current approaches and implications for nursing practice. Intensive Crit. Care Nurs. 2016;34:73–80. doi: 10.1016/j.iccn.2015.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brugha R, Crowe S. Relevance and effectiveness of the WHO global code practice on the international recruitment of health personnel-ethical and systems perspectives. Int. J. Health Policy Manag. 2015;4(6):333–336. doi: 10.15171/ijhpm.2015.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchman TG, Coopersmith CM, Meissen HW, et al. Innovative interdisciplinary strategies to address the intensivist shortage. Crit. Care Med. 2017;45(2):298–304. doi: 10.1097/CCM.0000000000002209. [DOI] [PubMed] [Google Scholar]
- Churpek MM, Wendlandt B, Zadravecz FJ, Adhikari R, Winslow C, Edelson DP. Association between intensive care unit transfer delay and hospital mortality: a multicenter investigation. J. Hosp. Med. 2016;11(11):757–762. doi: 10.1002/jhm.2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark MT, Delos JB, Lake DE, et al. Stochastic modeling of central apnea events in preterm infants. Physiol. Meas. 2016;37(4):463–484. doi: 10.1088/0967-3334/37/4/463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douw G, Schoonhoven L, Holwerda T, et al. Nurses’ worry or concern and early recognition of deteriorating patients on general wards in acute care hospitals: a systematic review. Crit. Care. 2015;19:230. doi: 10.1186/s13054-015-0950-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drew BJ, Harris P, Zègre-Hemsey JK, et al. Insights into the problem of alarm fatigue with physiologic monitor devices: a comprehensive observational study of consecutive intensive care unit patients. PLoS One. 2014;9(10) doi: 10.1371/journal.pone.0110274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endsley MR. Toward a theory of situation awareness in dynamic systems. Hum. Factors. 1995;37(1):32–64. doi: 10.1518/001872095779049543. [DOI] [Google Scholar]
- Escobar GJ, Dellinger RP. Early detection, prevention, and mitigation of critical illness outside intensive care settings. J. Hosp. Med. 2016;11(Suppl 1):S5–S10. doi: 10.1002/jhm.2653. [DOI] [PubMed] [Google Scholar]
- Escobar GJ, LaGuardia JC, Turk BJ, Ragins A, Kipnis P, Draper D. Early detection of impending physiologic deterioration among patients who are not in intensive care: development of predictive models using data from an automated electronic medical record. J. Hosp. Med. 2012;7(5):388–395. doi: 10.1002/jhm.1929. [DOI] [PubMed] [Google Scholar]
- Fairchild KD, Schelonka RL, Kaufman DA, et al. Septicemia mortality reduction in neonates in a heart rate characteristics monitoring trial. Pediatr. Res. 2013;74(5):570–575. doi: 10.1038/pr.2013.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman CP, Allee NJ, Delaney BC, et al. The science of Learning Health Systems: foundations for a new journal. Learn. Health Syst. 2017;1(1):e10020. doi: 10.1002/lrh2.10020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman CP, Wong AK, Blumenthal D. Achieving a nationwide learning health system. Sci. Transl. Med. 2010;2(57) doi: 10.1126/scitranslmed.3001456. 57cm29. [DOI] [PubMed] [Google Scholar]
- Giannoni A, Baruah R, Leong T, et al. Do optimal prognostic thresholds in continuous physiological variables really exist? Analysis of origin of apparent thresholds, with systematic review for peak oxygen consumption, ejection fraction and BNP. PLoS One. 2014;9(1):e81699. doi: 10.1371/journal.pone.0081699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass G, Hartka TR, Keim-Malpass J, Enfield KB, Clark MT. Dynamic data in the ED predict requirement for ICU transfer following acute care admission. J. Clin. Monit. Comput. 2020 doi: 10.1007/s10877-020-00500-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green M, Lander H, Snyder A, Hudson P, Churpek M, Edelson D. Comparison of the Between the Flags calling criteria to the MEWS, NEWS and the electronic Cardiac Arrest Risk Triage (eCART) score for the identification of deteriorating ward patients. Resuscitation. 2018;123:86–91. doi: 10.1016/j.resuscitation.2017.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin MP, Lake DE, O’Shea TM, Moorman JR. Heart rate characteristics and clinical signs in neonatal sepsis. Pediatr. Res. 2007;61(2):222–227. doi: 10.1203/01.pdr.0000252438.65759.af. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (US) In: Digital Infrastructure for the Learning Health System: The Foundation for Continuous Improvement in Health and Health Care: Workshop Series Summary. Grossmann C, Powers B, McGinnis JM, editors. National Academies Press (US); Washington (DC): 2011. [DOI] [PubMed] [Google Scholar]
- Joshi R, van de Mortel H., Feijs L, Andriessen P, van Pul C. The heuristics of nurse responsiveness to critical patient monitor and ventilator alarms in a private room neonatal intensive care unit. PLoS One. 2017;12(10) doi: 10.1371/journal.pone.0184567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane-Gill SL, O’Connor MF, Rothschild JM, et al. Technologic distractions (part 1): summary of approaches to manage alert quantity with intent to reduce alert fatigue and suggestions for alert fatigue metrics. Crit. Care Med. 2017;45(9):1481–1488. doi: 10.1097/CCM.0000000000002580. [DOI] [PubMed] [Google Scholar]
- Keim-Malpass J, Clark MT, Lake DE, Moorman JR. Towards development of alert thresholds for clinical deterioration using continuous predictive analytics monitoring. J. Clin. Monit. Comput. 2019 doi: 10.1007/s10877-019-00361-5. [DOI] [PubMed] [Google Scholar]
- Keim-Malpass J, Kitzmiller R, Skeeles-Worley A, et al. Advancing continuous predictive analytics monitoring: moving from implementation to clincial action in a learning health system. Crit. Care Nurs. Clin. N. Am. 2018;30(2) doi: 10.1016/j.cnc.2018.02.009. [DOI] [PubMed] [Google Scholar]
- Keim-Malpass J, Kitzmiller RR, Skeeles-Worley A, et al. Advancing continuous predictive analytics monitoring: moving from implementation to clinical action in a learning health system. Crit. Care Nurs. Clin. N. Am. 2018;30(2):273–287. doi: 10.1016/j.cnc.2018.02.009. [DOI] [PubMed] [Google Scholar]
- Kitzmiller RR, Vaughan A, Skeeles-Worley A, et al. Diffusing an innovation: clinician perceptions of continuous predictive analytics monitoring in intensive care. Appl. Clin. Inform. 2019;10(2):295–306. doi: 10.1055/s-0039-1688478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake DE, Fairchild KD, Moorman JR. Complex signals bioinformatics: evaluation of heart rate characteristics monitoring as a novel risk marker for neonatal sepsis. J. Clin. Monit. Comput. 2014;28(4):329–339. doi: 10.1007/s10877-013-9530-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake DE, Moorman JR. Accurate estimation of entropy in very short physiological time series: the problem of atrial fibrillation detection in implanted ventricular devices. Am. J. Physiol. Heart Circ. Physiol. 2011;300(1):H319–H325. doi: 10.1152/ajpheart.00561.2010. [DOI] [PubMed] [Google Scholar]
- Lake DE, Richman JS, Griffin MP, Moorman JR. Sample entropy analysis of neonatal heart rate variability. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2002;283(3):R789–R797. doi: 10.1152/ajpregu.00069.2002. [DOI] [PubMed] [Google Scholar]
- Lancet COVID-19: protecting health-care workers. Lancet. 2020;395:922. doi: 10.1016/S0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas T, Horton R. Nursing in 2020: a call for papers. Lancet. 2020;395(10217):15. doi: 10.1016/S0140-6736(19)33176-9. [DOI] [PubMed] [Google Scholar]
- Mahase E. Covid-19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ. 2020;368:m1036. doi: 10.1136/bmj.m1036. [DOI] [PubMed] [Google Scholar]
- McClure C, Jang SY, Fairchild K. Alarms, oxygen saturations, and SpO2 averaging time in the NICU. J. Neonatal Perinatal Med. 2016;9(4):357–362. doi: 10.3233/NPM-16162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moorman JR, Carlo WA, Kattwinkel J, et al. Mortality reduction by heart rate characteristic monitoring in very low birth weight neonates: a randomized trial. J. Pediatr. 2011;159(6):900–906. doi: 10.1016/j.jpeds.2011.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss TJ, Clark MT, Calland JF, et al. Cardiorespiratory dynamics measured from continuous ECG monitoring improves detection of deterioration in acute care patients: a retrospective cohort study. PLoS One. 2017;12(8) doi: 10.1371/journal.pone.0181448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss TJ, Clark MT, Lake DE, Moorman JR, Calland JF. Heart rate dynamics preceding hemorrhage in the intensive care unit. J. Electrocardiol. 2015;48(6):1075–1080. doi: 10.1016/j.jelectrocard.2015.08.007. [DOI] [PubMed] [Google Scholar]
- Moss TJ, Lake DE, Calland JF, et al. Signatures of subacute potentially catastrophic illness in the ICU: model development and validation. Crit. Care Med. 2016;44(9):1639–1648. doi: 10.1097/CCM.0000000000001738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss TJ, Lake DE, Moorman JR. Local dynamics of heart rate: detection and prognostic implications. Physiol. Meas. 2014;35(10):1929–1942. doi: 10.1088/0967-3334/35/10/1929. [DOI] [PubMed] [Google Scholar]
- Politano AD, Riccio LM, Lake DE, et al. Predicting the need for urgent intubation in a surgical/trauma intensive care unit. Surgery. 2013;154(5):1110–1116. doi: 10.1016/j.surg.2013.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poole S, Shah N. Addressing vital sign alarm fatigue using personalized alarm thresholds. Pac. Symp. Biocomput. 2018;23:472–483. doi: 10.1142/9789813235533_0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raith EP, Udy AA, Bailey M, et al. Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA. 2017;317(3):290–300. doi: 10.1001/jama.2016.20328. [DOI] [PubMed] [Google Scholar]
- Romero-Brufau S, Gaines K, Nicolas CT, Johnson MG, Hickman J, Huddleston JM. The fifth vital sign? Nurse worry predicts inpatient deterioration within 24 hours. JAMIA Open. 2019;2(4):465–470. doi: 10.1093/jamiaopen/ooz033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman MJ, Rothman SI, Beals J. Development and validation of a continuous measure of patient condition using the Electronic Medical Record. J. Biomed. Inform. 2013;46(5):837–848. doi: 10.1016/j.jbi.2013.06.011. [DOI] [PubMed] [Google Scholar]
- Rothman MJ, Tepas JJ, Nowalk AJ, et al. Development and validation of a continuously age-adjusted measure of patient condition for hospitalized children using the electronic medical record. J. Biomed. Inform. 2017;66:180–193. doi: 10.1016/j.jbi.2016.12.013. [DOI] [PubMed] [Google Scholar]
- Royal College of Physicians . England: Royal College of Physicians; London: 2012. National Early Warning Score (NEWS) - Standardising the Assessment of Acute-Illness Severity in the NHS. [Google Scholar]
- Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(5):846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruminski CM, Clark MT, Lake DE, et al. Impact of predictive analytics based on continuous cardiorespiratory monitoring in a surgical and trauma intensive care unit. J. Clin. Monit. Comput. 2019;33(4):703–711. doi: 10.1007/s10877-018-0194-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schondelmeyer AC, Daraiseh NM, Allison B, et al. Nurse responses to physiologic monitor alarms on a general pediatric unit. J. Hosp. Med. 2019;14(10):602–606. doi: 10.12788/jhm.3234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sir MY, Dundar B, Barker Steege LM, Pasupathy KS. Nurse-patient assignment models considering patient acuity metrics and nurses’ perceived workload. J. Biomed. Inform. 2015;55:237–248. doi: 10.1016/j.jbi.2015.04.005. [DOI] [PubMed] [Google Scholar]
- Spaeder MC, Moorman JR, Tran CA, et al. Predictive analytics in the pediatric intensive care unit for early identification of sepsis: capturing the context of age. Pediatr. Res. 2019;86(5):655–661. doi: 10.1038/s41390-019-0518-1. [DOI] [PubMed] [Google Scholar]
- Stubbings L, Chaboyer W, McMurray A. Nurses’ use of situation awareness in decision-making: an integrative review. J. Adv. Nurs. 2012;68(7):1443–1453. doi: 10.1111/j.1365-2648.2012.05989.x. [DOI] [PubMed] [Google Scholar]
- The Royal College of Physicians. The National Early Warning Score (NEWS) thresholds and triggers. 2012:1.
- Tume LN, Trapani J. Introduction to the WHO year of the nurse and midwife: the impact of critical care nurses and meet the new editors. Nurs. Crit. Care. 2020;25(1):6–7. doi: 10.1111/nicc.12495. [DOI] [PubMed] [Google Scholar]
- Wang J, Hahn SS, Kline M, Cohen RI. Early in-hospital clinical deterioration is not predicted by severity of illness, functional status, or comorbidity. Int. J. Gen. Med. 2017;10:329–334. doi: 10.2147/IJGM.S145933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warttig S, Alderson P, Evans DJ, Lewis SR, Kourbeti IS, Smith AF. Automated monitoring compared to standard care for the early detection of sepsis in critically ill patients. Cochrane Database Syst. Rev. 2018;6 doi: 10.1002/14651858.CD012404.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams B, Alberti G, Ball C, Bell D, Binks R, Durham L. The Royal College of Physicians; London: 2012. National Early Warning Score (NEWS): Standardising the Assessment of Acute-Illness Severity in the NHS. [Google Scholar]
- Winters BD, Cvach MM, Bonafide CP, et al. Technological distractions (part 2): a summary of approaches to manage clinical alarms with intent to reduce alarm fatigue. Crit. Care Med. 2018;46(1):130–137. doi: 10.1097/CCM.0000000000002803. [DOI] [PubMed] [Google Scholar]
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.