Abstract
Objective
Hyperhidrosis (excessive sweating) is associated with significant quality-of-life burden yet is often undertreated. With limited FDA-approved treatments, health care providers must determine optimal treatment among approved and off-label options. Key objectives of this review were to reassess, update, and expand a previous systematic review of commonly used treatment options for primary hyperhidrosis, including consideration of aluminum and zirconium compounds.
Methods
We performed a qualitative systematic review of efficacy, health-related quality of life, satisfaction, and safety of interventions, replicating and expanding the strategy outlined in a previous systematic review, with the addition of studies utilizing a within-patient design. We performed a critical appraisal of identified studies to determine risk of bias (RoB) and strength of evidence (SOE).
Results
A total of 32 studies were eligible for critical appraisal. Only three studies – two clinical trials of glycopyrronium cloth (2.4%) and one trial of botulinum toxin A injections in axillary hyperhidrosis were rated as “low” RoB; both had SOE ratings of “moderate” for use in axillary hyperhidrosis – the highest rating included in this review.
Conclusions
Optimal treatment choice depends on several factors, including understanding the quality of evidence regarding each treatment’s efficacy and safety (considerations of convenience and cost are beyond the scope of this review). In hyperhidrosis, as in other clinical conditions, treatment decisions should be patient centered. At this time, because of the quality of evidence, only imprecise estimates of effect are possible for hyperhidrosis treatments included in this review, and statements about comparative effectiveness are not possible.
Keywords: Hyperhidrosis, evidence-based, strength of evidence, systematic review, comparative effectiveness, within-patient study design
Introduction
Primary hyperhidrosis is characterized by excessive sweating beyond what is necessary for thermal homeostasis1. It is an idiopathic condition (in contrast to secondary hyperhidrosis) that is estimated to occur in 4.8% of the U.S. population (∼15.3 million people) and most commonly affects the axillary, palmar, and plantar regions of the body1,2.
The negative impact of primary hyperhidrosis on quality of life is well established; sufferers experience embarrassment and negative effects on social and emotional health, with a disease impact similar to or greater than that of psoriasis or eczema1–4. Even so, many hyperhidrosis patients go years without seeking the help that could be afforded from prescription treatments. Many rely on over-the-counter products and employ coping strategies such as frequent showering or carrying around towels and sets of extra clothing5. In a survey conducted by the International Hyperhidrosis Society, nearly half (48.9%) of patients waited a decade or longer before seeking medical help for their excessive sweating2.
The lack of patient engagement in seeking medical help is not due to a lack of available treatment options. A diverse array of interventions has been used for the treatment of primary hyperhidrosis, including topical, oral and injectable prescription treatments as well as medical device therapies6. Specific treatment choices may be impacted by the focal area affected and intrinsic patient factors; however, given the limited number of FDA-approved treatment options for hyperhidrosis, health care providers are left to determine for each patient what might be the optimal treatment course among the approved and off-label choices available to them. Aside from prescription-strength antiperspirants, only two pharmacological agents have been approved by the FDA for the treatment of hyperhidrosis7–9.
This underscores how instructive a critical evaluation of the hyperhidrosis treatment evidence base becomes for practicing physicians trying to narrow down the best treatment decisions within a broad range of therapeutic options. Most patients and many clinicians are either unaware of the important connection between the quality of scientific studies and the reliability of the reported results, or they focus on the reported results and fail to consider the strength of the evidence (SOE) before making treatment decisions10. The reason for emphasizing evidence quality is that benefits and harms that patients may experience with various treatment choices can be more accurately predicted when evidence is at the lowest risk of bias (RoB).
A systematic review first reported by Wade et al.11 and subsequently in Wade et al.12 examined relevant evidence available in the scientific literature through July 2016 for primary hyperhidrosis treatments. However, several aspects of that analysis, including the lack of special consideration for those studies utilizing within-patient designs or with large response rates, the exclusion of aluminum/zirconium compounds commonly used for hyperhidrosis treatment, and the interim FDA approval of a new hyperhidrosis drug, warrant further exploration.
Here, we performed a qualitative systematic review of efficacy, health-related quality of life, satisfaction, and safety of commonly used interventions in the treatment of primary hyperhidrosis based on the strategy outlined by Wade et al.12. The key objectives of this review are to provide a comprehensive literature appraisal that includes the most recently published studies as well as a critical reassessment of studies evaluating hyperhidrosis treatments via within-patient designs and those with large response rates. Evidence summaries are presented to assist decision-makers in choosing optimal treatment strategies for patients seeking treatment for primary hyperhidrosis across a range of focal areas.
Methods
Eligibility criteria
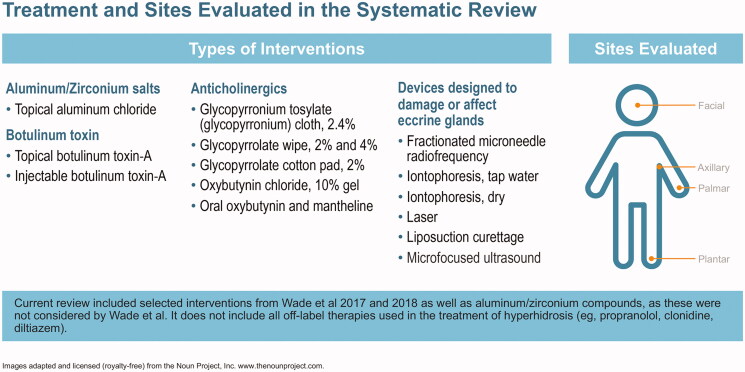
The protocol for this systematic review was registered in PROSPERO International Prospective Register of Systematic Reviews (crd.york.ac.uk/prospero/index.asp identifier CRD42018104063). Clinical trials were eligible for inclusion. Eligibility was based on the Cochrane PICO annotation system13: population (patients with primary hyperhidrosis involving axillae, palms, soles or head without age restriction), intervention (four interventions used in the treatment of primary hyperhidrosis of the head, axilla, palms and soles in children and adults – see Figure 1), comparator (placebo, no treatment or any of the commonly used treatments listed above), outcome (efficacy, safety and quality of life outcomes using a variety of tools reported in the literature). Non-English language studies were excluded. Treatments evaluated include aluminum and zirconium compounds, anticholinergics (topical and systemic), botulinum toxin, and medical device therapies designed to alter the function of sweat production or damage eccrine glands (iontophoresis, curettage, laser therapy, microwave, fractional needle radiotherapy and ultrasound; Figure 1).
Figure 1.
Hyperhidrosis treatment options and sites evaluated.
Search strategy and study selection
The following databases were searched: MEDLINE, Embase, the Cochrane Database of Systematic Reviews (CDSR) and Cochrane Central of Controlled Trials (CENTRAL). Studies were identified (1) by reviewing and assessing those included in two related publications by Wade et al. of the same search strategy and results11,12, (2) by performing an updated database search for studies published after the search date of 12 January 2016 used in the Wade et al. analysis, and (3) via PubMed and Embase searches for studies on aluminum/zirconium compounds. Search dates, terms and PubMed translations can be found in Supplementary Materials (p. 79).
Two investigators developed inclusion and exclusion criteria for study eligibility and agreed upon study inclusion. Studies considered were those studies from the Wade et al. analysis that met our inclusion criteria for critical appraisal, relevant studies obtained through database searches using the Wade et al. search terms (but published after the Wade et al. search date of 12 January 2016 and meeting our criteria), relevant studies of aluminum/zirconium salts (which were outside the scope of the Wade et al. analysis), and relevant studies identified via hand searches of retrieved study reference lists.
Trial quality was assessed in Wade et al.12 using a modified version of the Cochrane Risk of Bias tool. The Cochrane Risk of Bias tool requires that a finding of high or uncertain RoB in any review domains renders the overall study as at high or uncertain RoB14. Our assessment is that this standard is quite stringent and insufficiently contextual, which may result in the exclusion of results that are possibly reliable. For example, though studies using the “within-patient” design were included in the overall conclusions in Wade et al.12 (despite being considered to be at high RoB), the Cochrane tool cannot account for the fact that this study design has unique strengths due to protections against confounding effects and has merit for both subjective and objective outcomes. Also, many of the studies identified in Wade et al.12 reported large response rates, yet were not identified in that prior analysis as warranting special consideration, though such studies – even if they are not randomized and well controlled – may provide valid data15.
For the reasons stated above, studies using a within-patient study design and rated by Wade et al. as at high or uncertain RoB and passing a Delfini critical appraisal were included. In addition, studies rated by Wade et al.12 as being at high or uncertain RoB were retained in this current review if they reported large response rates (defined as 40% or greater). Finally, searches for studies on topical formulations of aluminum and zirconium were also conducted, as these were not considered by Wade et al.
Studies not meeting inclusion criteria were rejected following title and/or abstract review; full text was retrieved for studies selected for consideration for inclusion. All studies were found in PubMed and hand searches of retrieved study reference lists.
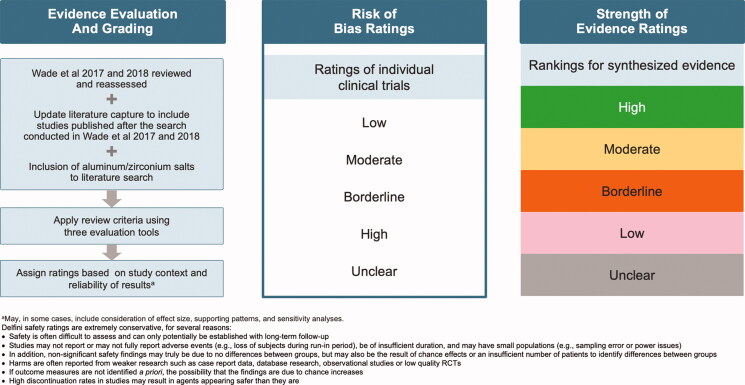
Evidence evaluation and grading
Critical appraisals were performed for all efficacy studies selected for inclusion and rated for RoB. Each eligible study was assessed for RoB using tools created by Delfini Group based on standard evidence-based medicine principles and have been used by many groups – the tools are freely available at www.delfini.org. With rare exception, critical appraisal findings were documented only sufficiently to reach a grade; for example, if a lethal threat to validity was found, that threat was considered enough to reach a rating of "high risk of bias" and render documentation of further threats unnecessary.
However, in some studies with very large response rates, despite being rated as at high RoB, the validity and clinical usefulness were taken into consideration; in these instances, an explanation for any such exceptions was provided.
Wade et al.12 was assessed for validity and clinical usefulness using a Delfini critical appraisal tool developed for assessing quality of data (http://www.delfini.org/delfiniTools.htm#catool).
All studies considered for inclusion in Wade et al.12 were reevaluated for potential critical appraisal in this analysis (note that in Wade et al.12, findings were summarized regardless of whether the study was rated as at high or unclear RoB). Key findings regarding efficacy, quality of life, satisfaction and safety were summarized narratively. The RoB ratings for individual clinical trials were assigned by Delfini as “Low,” “Moderate,” Borderline’, “High” and “Unclear” (Figure 2). For strength of evidence (SOE) classification, rankings assigned by Delfini for synthesized evidence were “High,” “Moderate,” “Borderline,” “Low,” and “Unclear” (Figure 2).
Figure 2.
Flowchart on methodology used for assigning RoB and SOE ratings.
Results
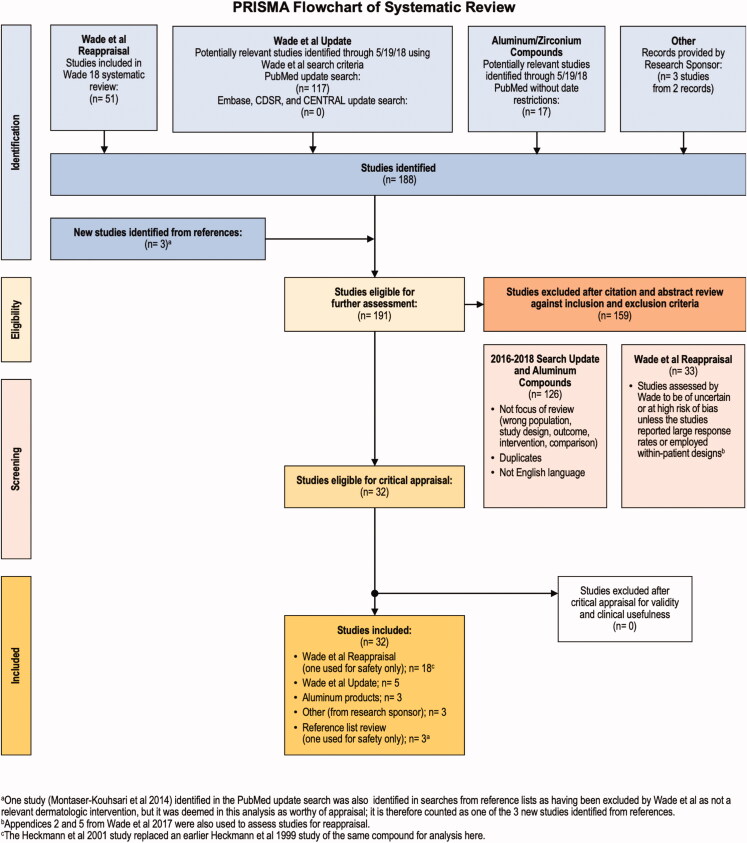
Of 191 studies eligible for screening, 159 were excluded because they had insufficient information to appraise, were at a high RoB, were superseded by a more recent study, or existed as a poster with no corresponding manuscript. A total of 32 studies were eligible for critical appraisal for validity and clinical usefulness, and all 32 met critical appraisal criteria and were included in the present analysis (Figure 3).
Figure 3.
Systematic review flowchart.
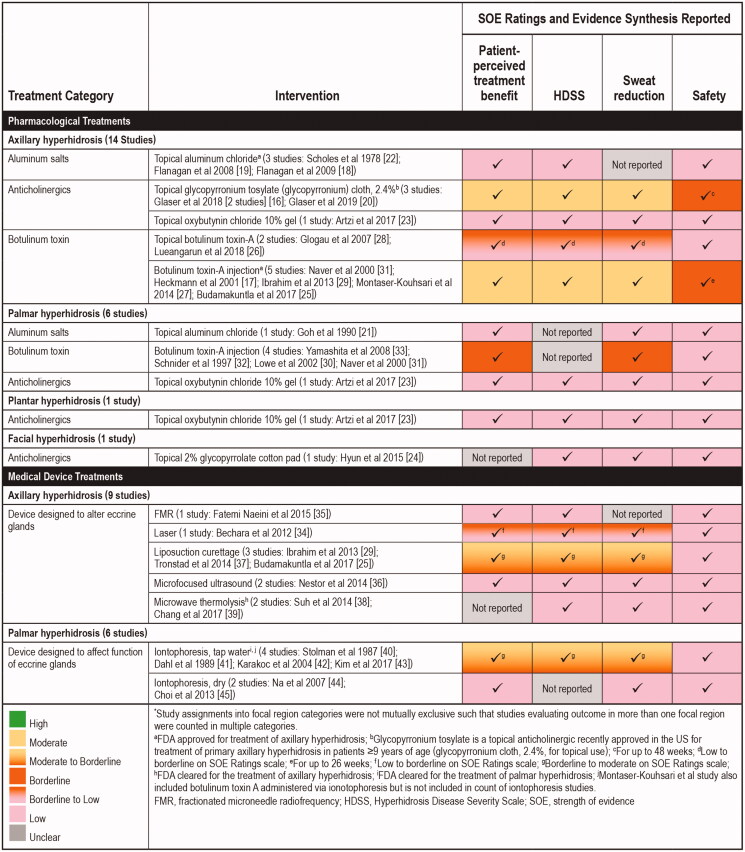
Overall summary of findings
Only three studies – a report of two clinical trials of glycopyrronium cloth (2.4%)16 and one trial of botulinum toxin A injections for the treatment of axillary hyperhidrosis17 were rated as being at “low” RoB. The overall SOE for most interventions for efficacy was weak with a large degree of heterogeneity in elements such as the study size, population studied, therapeutic interventions, study duration, endpoints reported, and effect sizes. SOE of pharmacological treatments and medical device interventions used to treat different types of hyperhidrosis are reviewed and summarized by focal region and type of intervention in Figure 4 and briefly discussed below (detailed descriptions of individual trials appear in the following section, “Individual Treatment Summaries”)16–45. Efficacy and safety findings, including effect size estimates for pharmacological treatments and medical device interventions are summarized in Tables 1–5.
Figure 4.
Overall summary of SOE ratings and evidence synthesis for unique studies identified for appraisal (n = 32)*.
Table 1.
Summary and risk of bias for aluminum salt studies.
| Study and intervention(s) | HH population and design | Risk of bias | Key results/critical appraisal findings |
|---|---|---|---|
| Flanagan et al.19 a 20% topical aluminum chloride hexahydrate (AC) vs. botulinum toxin A (BTX-A) injections |
Axillary Single-center, 12-week, randomized, parallel, open-label, study N = 50 (n = 25 AC, n = 25 BTX-A for 4 weeks); cross over at week 4 allowed for AC patients dissatisfied with treatment |
Borderline to high | 33.3% HDSS response rate (≥2 grade improvement) in AC-treated patients at week 4 vs. 91.7% in BTX-A group; 33.3% of AC-treated patients were “very satisfied” at week 4 vs. 87.5% of patients in BTX-A group Large cross-over (allowed at week 4) from AC to BTX-A therapy (71%) Safety: >50% of subjects treated with AC reported stinging, itching and redness, and >25% reported pain |
| Flanagan and Glaser18 Aluminum chloride (15% aluminum chloride (AC) in 2% salicylic acid gel base (compared to baseline) |
Axillary Prospective, open-label, uncontrolled, single-arm study (N = 30); 12-week duration |
High | 72% HDSS responders; 75% somewhat or very satisfied with treatment compared to baseline Safety: moderate to severe redness (14.3%) moderate to severe itching (28.6%), absent to mild pain (92.9%) and moderate pain (7.1%); 2 subjects did not complete trial due to moderate-to-severe axillary irritation (redness, itching, burning) |
| Goh21 Topical aluminum chloride hexahydrate 20% W/W ethanol (AC) applied to one palm No treatment applied to other palm |
Palmar Small (N = 12), W/P, single author, assessor-blinded, 6-week study |
Unclear | Approximately, two-thirds likely to experience drier palms within 24 h of AC treatment, lasting for 1–2 days Weekly mean skin vapor loss difference averaged 16.4 g water/m2/h over 4 weeks; all patients reported treated palms to be drier than untreated palms the following morning after starting treatment, and that sweating returned within 2 days of stopping treatment Safety: 1 out of 4 experienced a stinging sensation after application; one patient dropped out due to intolerable side effects |
| Scholes et al.22 20% aluminum chloride applied with a brush for 1 week |
Axillary One case series from two dermatology clinics (N = 65) |
High | Authors state that 64/65 patients had “excellent control of sweating”; however, statements appear to be authors’ interpretation from comments received from 42 patients from one clinic who completed a questionnaire 12 months after the study had concluded Safety: 29 experienced some irritation (described as “minor” by authors, but 28 subjects reported relief following application of 1% hydrocortisone cream on the morning after treatment) |
Abbreviations. AC, Aluminum chloride; AE, Adverse event; BTX-A, Botulinum toxin A; HDSS, Hyperhidrosis Disease Severity Scale; W/P, Within patient.
SOE considered for aluminum chloride body of evidence only.
Table 2.
Summary and risk of bias for anticholinergic agents.
| Study and intervention | HH population and design | Risk of bias | Key results/critical appraisal findings |
|---|---|---|---|
| Glaser et al.16 Topical 2.4% glycopyrronium tosylate (GT) pre-moistened cloth vs. vehicle (same appearance and excipient content with exception of GT) |
Axillary Two distinct 4-week, randomized, double-blind, vehicle-controlled clinical trials in patients ≥ 9 years of age (N = 697) |
Low | Nearly 75% of patients achieved a ≥50% reduction from baseline in axillary sweat production and 59% achieved a ≥2-point reduction in HDSS score by week 4 with GT (pooled results) ∼60% of patients had ≥4-point improvement on Axillary Sweating Daily Diary Item 2, indicating a clinically meaningful improvement in disease severity, and 58.1% rated their condition as much better (Patient Global Impression of Change) with GT Safety: AEs occurring in ≥5% in either pooled group included dry mouth (24.2% GT vs. 5.6% vehicle), application site pain, mydriasis, oropharyngeal pain, and headache; local skin reactions were reported in 30.8% GT vs. 30.3% vehicle and were predominantly mild to moderate in severity |
| Glaser et al.20 Topical 2.4% glycopyrronium tosylate (GT) pre-moistened cloth |
Axillary A 44-week observational open-label extension trial (N = 550) for those who completed the two trials described in Glaser 2018 |
N/A (used for safety only) | N/A for efficacy Safety: results were consistent with the findings in prior studies, with no new or unexpected findings; AEs were dry mouth (16.9%), blurred vision (6.7%), application site pain (6.4%), nasopharyngitis (5.8%) and mydriasis (5.3%) Long-term efficacy outcomes collected and supported findings in the two double-blind trials |
| Hyun et al.24 2% topical glycopyrrolate-impregnated cotton pads (not commercially available) vs. placebo |
Facial Randomized, double-blind, placebo-controlled study for 9 days investigated in subjects aged 20–66 years with facial hyperhidrosis (N = 39) *Reevaluated based on W/P design: drug/placebo split application in two halves of forehead) |
Moderate | Compared with the placebo-treated sides, topical glycopyrrolate-treated sides showed a reduction in the rate of sweat production at the forehead of 36.68 ± 11.41% on day 10 (p<.025) Safety: one patient reported transient headache following treatment |
| Artzi et al.23 Topical oxybutynin chloride 10% gel vs. placebo |
Axillary, palmar, plantar W/P, placebo-controlled comparison (2× daily application) with randomization for 4 weeks in adults (N = 61) *Newly identified relative to Wade et al.12 |
Moderate (LRR) | Palmar hyperhidrosis patients are likely to experience 25% to <50% sweat reduction as assessed by the minor starch-iodine test Approximately, three quarters (axillary), two thirds (palmar), and half (plantar) of patents reported a 1-point change in HDSS A 2-point HDSS change was reported by 9.5% (axillary), 8.3% (plantar), and 5% (palmar) Approximately, three quarters of patients reported moderate to high satisfaction Safety: Approximately, half of patients with axillary hyperhidrosis treated with oxybutynin 10% gel reported erythema and/or pruritus; patients have reported dry mouth, erythema, itching, a “sticky” feel and inconvenience of use |
Abbreviations. AE, Adverse event; GT, Glycopyrronium tosylate; HDSS, Hyperhidrosis Disease Severity Scale; LRR, Large response rates; W/P, Within patient.
Table 3.
Summary and risk of bias for botulinum toxin type A studies.
| Study and intervention | HH population and design | Risk of bias | Key results/critical appraisal findings |
|---|---|---|---|
| Lueangarun et al.26 Topical botulinum toxin type A liposomal cream (not commercially available) vs. Vehicle *Newly identified relative to Wade et al.12 |
Axillary W/P, randomized, double-blind, vehicle-controlled 8-week trial in patients ages 18–50 (N = 20) |
Moderate (LRR) | Potential for small short-term benefits of BTX-A cream based on reduced sweat production, expert panel assessments of iodine starch test, HDSS, and patient satisfaction Safety: no AEs (including local skin reactions) were observed in either treatment arm |
| Budamakuntla et al.25 Botulinum toxin A injections vs. subcutaneous curettage (appears also in Table 4 for curettage results) *Newly identified relative to Wade et al.12 |
Axillary W/P, open-label, 3-month comparative study of efficacy and safety of botulinum toxin A injections and subcutaneous curettage in adults (N = 20) |
Moderate (LRR) | Large decrease in sweat rate consistent with HDSS score decrease After BTX-A injections, mean HDSS decreased 1.75 points at month 3 (p<.0001) and by 1.35 points at month 6 (p<.0001) After suction curettage, mean HDSS decreased 1.70 points at month 3 (p<.0001) and 1.20 points at month 6 (p<.0001) Safety: after toxin injections no patients reported pain or other AEs; after the suction-curettage procedure, 2 had bruising which resolved in 3 days; one had a painful bridle (fibrosis) formation in the surgical site persisting for 2–3 months |
| Montaser-Kouhsari et al.27 a Botulinum toxin A injections, 250 MU (per side) vs. botulinum toxin A administered by iontophoresis *New study identified from reference review |
Axillary W/P, randomized trial comparing botulinum toxin A injections to botulinum toxin A administered by iontophoresis over 6 months (N = 11) |
Moderate (LRR) | Iontophoresis of BTX-A reduced sweat production (gravimetry) by 73%, 22%, and 32% after 1 week, 1 month, and 6 months, respectively; injection reduced sweat production by 84%, 76%, and 50%, respectively At month 6, all but one of the injection groups reported being very satisfied; for iontophoresis, no participant reported being very satisfied, 9 reported being satisfied, and 2 reported dissatisfaction Safety: no AEs other than pain were reported. Pain perception (VAS score 0–100) was significantly lower in with iontophoresis vs. injection (15.0 vs. 20.0, p<.05) |
| Yamashita et al.33 Botulinum toxin A 60 U in right palm injections vs. no treatment *Reevaluated based on W/P design |
Palmar W/P, non-randomized, 6-month clinical trial in adults (N = 27) |
Moderate (LRR) | Quantity of sweat on the treated hand decreased to approximately one-fifth at one month after injection. Sweat quantity increased slightly over time but remained less than half at 6 months after injection; significant difference was observed when compared to before injection. Safety data were not presented; authors note “very little effect on grip strength” |
| Schnider et al.32 Botulinum toxin A injections (BTX-A; Dysport) 120 units vs. placebo (saline) *Reevaluated based on W/P design |
Palmar W/P, randomized, double-blind, 13-week comparison in adults with socially handicapping palmar hyperhidrosis (N = 11) |
Moderate (LRR) | Mean sweat reduction of 40% from baseline (digital images) and a 40% improvement using a visual analog scale were reported at 8 weeks (p≤.002) with BTX-A; neither the objective measurement nor the subjective rating showed a statistically significant reduction of sweating in the placebo-treated palms Safety: no serious AEs; 3 patients reported minor handgrip weakness in the BTX-A-treated hand, and 3 reported injections were more painful in BTX-A-treated hands vs. placebo |
| Lowe et al.30 Botulinum toxin A injections (BTX-A) vs. placebo (normal saline) *Reevaluated based on W/P design |
Palmar W/P, randomized, 28-day comparison in adults ages 18–80 (N = 19 each group) |
Moderate (LRR) | Patients experienced a decrease in sweat production of approximately two thirds with BTX-A injections and about one third with placebo at 28 days; 17/17 rated the treatment as successful in the BTX-A-treated palm vs. 2/17 with placebo (p<.0001) Safety: no major AEs reported; 4 patients reported AEs (hand or finger numbness of short duration, pain in hand) |
| Glogau28 Topical botulinum toxin A (200 U) combined with proprietary transport peptide (not commercially available) vs. vehicle *Reevaluated based on W/P design |
Axillary W/P, randomized, vehicle-controlled 4-week trial (N = 12) |
Moderate (LRR) | Week 4 gravimetric sweat reduction was 65.3 ± 21.5% (BTX-A) vs. 25.3 ± 66.2% (vehicle; p<.05); minor’s iodine starch consistent with large response rate in BTX-A group Safety: no systemic AEs were reported. Local AEs (n = 4) occurred in vehicle-treated axillae and included mild folliculitis, tenderness, erythema, and eczema |
| Ibrahim et al.29 Onabotulinumtoxin-A injections vs. suction-curettage (appears also in Table 4 for curettage results) *Reevaluated based on W/P design |
Axillary W/P, randomized, comparative study (unblinded) in adults 18–65 with 6-month follow-up (N = 20) |
Moderate (LRR) | At month 3, toxin injections decreased sweat production by 72.1% vs. 60.4% for suction-curettage, p=.29 Duration of effect was ∼6 months Toxin injections resulted in a larger decrease in HDSS than suction-curettage by 0.80 points (month 3; p=.0002) and 0.90 points (month 6; p=.0017) Safety: after toxin injections, none of the 20 patients reported discomfort or adverse reactions; after suction-curettage, patients reported axillary discomfort for about a week; 3 patients in the suction-curettage group reported hyperpigmentation |
| Naver et al.31 Botulinum toxin A injection vs. no treatment *Reevaluated based on W/P design |
Axillary; palmar W/P, unblinded study comparing treated vs. non-treated axilla (n = 13), and/or palms (n = 19) (N = 28 total); 1-year follow-up |
Borderline (LRR) | Consistent pattern of improvement in all outcomes Sweating disappeared in 8/13 (axillary) and 5/19 (palmar) or was markedly reduced in another 5/13 (axillary) and 10/19 (palmar) Duration of effect was 2 to 5 months Safety: reduced finger grip in two-thirds of palmar patients; 2 patients with intense pain from injection |
| Heckmann et al.17 Botulinum toxin A injection vs. placebo *Reevaluated based on W/P design |
Axillary W/P, multicenter, randomized, placebo-controlled, 2-week study (26-week follow-up) (N = 145) |
Low (LRR) | Large (approximately 88%) decrease in mean rate of sweat production at week 2 in botulinum toxin A treated group; at week 24, sweat production was reduced by approximately 65% (open label after 2 weeks) Safety: no major AEs reported during first 14 weeks. Temporary adverse effects included headache in 4 patients, muscle soreness of the shoulder girdle in 2, increased facial sweating in 1, and axillary itching in 1 |
Abbreviations. AE, Adverse event; BTX-A, Botulinum toxin A; HDSS, Hyperhidrosis Disease Severity Scale; LRR, Large response rate; W/P, Within patient.
SOE considered for botulinum toxin A injection body of evidence only.
Table 4.
Summary and risk of bias for medical devices that alter eccrine glands.
| Study and intervention | HH population and design | Risk of bias | Key results/critical appraisal findings |
|---|---|---|---|
| Fatemi Naeini et al.35 Fractionated microneedle radiofrequency (FMR) vs. sham *Reevaluated based on W/P design |
Axillary (severe) W/P, single-blind, sham control (N = 25); three sessions of FMR (1 MHz) at 3-week intervals |
Moderate | HDSS scores (mean ± SD) at week 21 went from 3.46 at baseline to 1.87 ± 0.61 (FMR) and 3.38 ± 0.49 (control) (p<.001) More than three quarters of patients achieved a 1- or 2-point decrease in HDSS score (week 21) 80% of patients reported >50% satisfaction at the end of the study (week 21) Safety: most common side effects were erythema (68%) and pinpoint bleeding (56%) |
| Bechara et al.34 Laser vs. untreated *Reevaluated based on W/P design |
Axillary W/P, randomized, half-side-controlled trial (N = 21); 5 cycles of an 800-nm diode laser |
Moderate | Significant reduction in sweat rate was observed on the laser-treated side (median 89 mg/min vs. 48 mg/min; p<.001) and the untreated contralateral side (median 78 mg/min vs. median 65 mg/min; p=.04) No significant difference was found between the treated and untreated sides (p=.10) Safety: no serious complications during laser treatment were reported; one instance of axillary skin depigmentation was observed that resolved during the 12-month follow-up |
| Nestor and Park36 Microfocused ultrasound plus visualization vs. sham *Reevaluated based on W/P design |
Axillary Two W/P, randomized, double-blind, sham-controlled pilot studies (N = 14 and N = 20) |
Moderate | Study 1: ≥50% of patients achieved a ≥50% reduction in gravimetric sweat production (day 120) Study 2: HDSS response (day 60) was 67% (micro-focused ultrasound plus visualization) vs. 0% (sham) (p=.005) Study 2: HDSS response maintained (month 12) Safety: AEs were found to be mild; most common (>80%) were axilla tenderness or soreness |
| Microwave thermolysis | |||
| Suh et al.38 Microwave thermolysis Included for analysis of Safety only *New study identified from reference review |
Axillary Case report of a thin, healthy male patient diagnosed with transient median and ulnar neuropathy following microwave treatment for the treatment of axillary hyperhidrosis |
Safety only | Patient reported numbness and weakness in the first and second fingers and decreased ability to abduct his left arm Symptoms resolved at six months after intensive physical therapy |
| Chang et al.39 Microwave thermolysis Included for analysis of safety only *Newly identified relative to Wade et al.12 |
Axillary Case report of a thin, healthy female patient diagnosed with median and ulnar nerve injury following microwave treatment for the treatment of axillary hyperhidrosis (level 5 microwave for 1.5 s at a size of 140 × 80 mm2) |
Safety only | Patient experienced severe swelling, numbness and inability to raise her left arm immediately following treatment Palmar skin was noted to be discolored Sensory and motor deficits had not resolved at the 6-month follow-up |
| Liposuction curettage | |||
| Budamakuntla et al.25 Subcutaneous curettage vs. botulinum toxin A injections (appears also in Table 3 for botulinum toxin results) *Newly identified relative to Wade et al.12 |
Axillary W/P, open-label, 3-month comparative study of efficacy and safety of botulinum toxin A injections and subcutaneous curettage in adults (N = 20) |
Moderate (LRR) | The mean percent reduction in the resting sweat rate (gravimetry, weighed filter paper) 3 months after BTX-A injections was 80.32% and 3 months after the suction-curettage was 79.79%, p=.2072 After botulinum toxin A injections, mean HDSS score decreased 1.75 points at month 3 (p<.0001) and by 1.35 points at month 6 (p<.0001) After suction curettage, mean HDSS score decreased 1.70 points at month 3 (p<.0001) and 1.20 points at month 6 (p<.0001) Safety: after toxin injections no patients reported pain or other AEs; after the suction-curettage procedure, 2 patients had bruising which resolved in 3 days; one patient had a painful bridle (fibrosis) formation in the surgical site which persisted for 2–3 months |
| Ibrahim et al.29 Suction curettage vs. onabotulinumtoxin-A injections (appears also in Table 3 for botulinum toxin results) *Reevaluated based on W/P design |
Axillary W/P, randomized, comparative study (unblinded) in adults 18–65 with 6-month follow-up (N = 20) |
Moderate (LRR) | At month 3, toxin injections decreased sweat production by 72.1% vs. 60.4% for suction-curettage, p=.29 Duration of effect was ∼6 months Safety: after toxin injections, none of the 20 patients reported discomfort or adverse reactions; after suction-curettage, patients reported axillary discomfort for about a week; 3 patients in the suction-curettage group reported hyperpigmentation |
| Tronstad et al.37 a Tumescent suction curettage vs. curettage only *Reevaluated based on W/P design |
Axillary W/P, unblinded, half-side comparison randomized, controlled trial in adults (N = 22); 12-month follow-up |
Moderate | Five patients withdrew or did not meet for any follow-up examination; 17 subjects analyzed Significant reduction in sweating after both interventions lasting ≥ 12 months was found per skin conductance, gravimetry and visual analogue scale scoring Significantly better effect of tumescent suction curettage than curettage only; curettage reductions were approximately 40%, 30%, 35%; gravimetric measurements were reported as significantly lower at 6 (p<.05) and 12 months (p<.01) vs. before treatment but effect size estimates not possible from Figure 2. Safety: no infections requiring systemic antibiotics or hematoma after one week; one patient receiving suction with curettage experienced postoperative neuropathic pain, lasting through the observational period; no scarring was observed |
Abbreviations. AE, Adverse event; HDSS, Hyperhidrosis Disease Severity Scale; LRR, Large response rate; W/P, Within patient.
SOE considered for tumescent suction curettage body of evidence only.
Table 5.
Summary and risk of bias for iontophoresis studies.
| Study and intervention | HH population and design | Risk of bias | Key results/critical appraisal findings |
|---|---|---|---|
| Dahl41 Tap water iontophoresis vs. Sham *Reevaluated based on W/P design |
Palmar W/P, double-blind, randomized single center trial in adults (N = 11); 3-months duration |
Moderate | Iontophoresis-treated patients achieved a median reduction in sweating compared to the untreated side of 38% (p<.01) after a median number of 10 treatments of 4 mA of direct current compared to the untreated side (baseline sweating was not reported) 6 patients continued maintenance treatment every second week and achieved an 81% (median) reduction at 3 months (p<.05) Satisfaction: not assessed. Duration of effect: 2 weeks Safety: no AEs (e.g. soreness, erythema) reported |
| Karakoc et al.42 Direct electrical current based on tap water iontophoresis vs. placebo *Reevaluated based on W/P design |
Palmoplantar W/P, blinded, interrupted time-series study with objective measurement by non-blinded assessors (N = 15); 5 weeks duration |
Moderate | Significant change only with direct current iontophoresis treatment (baseline sweating rate approximately 3 g/h and post-treatment sweating rate <0.5 g/h, i.e. more than 80% reduction), but not with alternating current sham treatment suggesting that direct electrical current iontophoresis for palmoplantar HH is effective in reducing sweat intensity |
| Stolman40 Tap water iontophoresis (electrode exposed to 90 V and 12–12 mA direct current) vs. control hand with tap water and no electrode *Reevaluated based on W/P design |
Palmar W/P, unblinded, placebo controlled, 3-week study in adults (N = 18) |
Borderline | “Marked reduction” in sweating of the treated hand was reported by 15/18 treated subjects compared to no reduction in the untreated hand Objective assessment by starch-iodine imprint confirmed subjective reports; 2 subjects did not improve subjectively or by starch-iodine imprint Safety: 3 patients experienced slight and transient vesiculation of the skin; 12 patients reported redness for several hours after treatment; 2 patients reported intermittent hand tingling sometimes lasting several days |
| Na et al.44 Non-standard “dry-type” iontophoretic device (dry hand-held iontophoresis device; 5–15 mA direct current) *Reevaluated based on W/P design |
Palmar W/P, unblinded, 2-week trial in adults 18–34 years of age (N = 10) |
Borderline | Patients treated with 5–25 mA for 30 min daily for 1 week, then every other day for 1 week with dry-type iontophoresis reported a sweat reduction of 33–51% (average 42.7% reduction in treated palm vs. 1.8% in untreated palm) of baseline Duration of effect: 2 weeks (end of study) Safety: no major AEs; erythema, mild local burning and dark lines were reported (no numbers or percentages reported) |
| Choi et al.45 Dry iontophoresis Included for analysis of safety only *Reevaluated based on W/P design |
Palmar (N = 23) |
Safety only | N/A for efficacy Safety: two subjects dropped out after experiencing pruritic erythematous macules and asymptomatic hyperpigmented linear streaks on the treated left hands during the first week of treatment; the pruritic erythematous macules were relieved by application of a topical steroid agent for a week, and the asymptomatic hyperpigmented linear streaks disappeared spontaneously after discontinuing the electric device Safety: two cases of mild local adverse effects were noted. |
| Kim et al.43 Tap water iontophoresis vs. sham *Newly identified relative to Wade et al.12 |
Palmar Randomized, single-blind (patients only) controlled trial in adults and children ≥13 years of age (N = 29); 2 weeks of treatment with 6-week follow-up |
High | 85–90% of patients receiving iontophoresis may achieve grade 2 or 3 (mild or moderate) improvement on the starch-iodine test at 2 and 3 weeks compared to approximately 30% of patients receiving sham treatment at week 2 and 15% of sham treatment patients at week 3 Mean sweat secretion rate at week 2 decreased by 91.8% in the iontophoresis group vs. 39.1% in the sham group. At 3 weeks, the respective decreases in the mean secretion rate were 85% and 18.0% Duration of effect: 3 weeks Safety: one subject reported localized erythema of both hands. No major AEs; larger, longer studies are needed to adequately assess safety |
Abbreviations. AE, Adverse event; HDSS, Hyperhidrosis Disease Severity Scale; LRR, Large response rate; W/P, Within patient.
Efficacy findings – strength of evidence ratings
An overall summary of SOE with respect to efficacy outcomes is provided below. Of note, many of the studies had very small sample sizes (N < 50), which may lead to reporting of inflated treatment effect estimates46, and calls into question whether there was sufficient statistical power to detect significant differences between groups.
Axillary hyperhidrosis (23 studies): SOE ratings for topical glycopyrronium cloth (2.4%) and botulinum toxin A injections were “moderate” – the highest rating of any therapeutic agents included in this review. A “borderline to moderate” rating was assigned to liposuction curettage. The SOE rating for topical botulinum toxin A and laser treatments was “low to borderline.” The SOE rating was “low” for topical aluminum chloride and topical oxybutynin chloride 10% gel. SOE ratings were “low” for botulinum toxin administered via iontophoresis, microwave thermolysis, microfocused ultrasound and fractionated microneedle radiofrequency (Figure 4).
Palmar hyperhidrosis (12 studies): The highest SOE rating for pharmacological treatments for palmar hyperhidrosis was “borderline,” achieved by botulinum toxin A injections. The SOE rating for tap water iontophoresis was “borderline to moderate.” The SOE rating was “low” for topical aluminum chloride, topical oxybutynin chloride 10% gel, and dry iontophoresis (Figure 4).
Plantar hyperhidrosis (1 study): The SOE rating was “low” for topical oxybutynin chloride 10% gel (Figure 4).
Facial hyperhidrosis (1 study): The SOE rating for topical 2% glycopyrrolate-impregnated cotton pads was “low” (Figure 4).
Safety findings
The majority of trials did not provide sufficient evidence to draw firm conclusions about safety. Some studies provided few safety details and in others there was no mention of adverse events. In addition, the short duration of many studies did not allow for sufficient follow-up for reporting adverse events. The overall SOE for safety was rated as “low” for all interventions except glycopyrronium cloth 2.4%16,20 and botulinum toxin17, which were rated “borderline.” These were larger trials of higher methodological quality and longer duration (up to 48 weeks for glycopyrronium cloth 2.4% and up to 26 weeks for botulinum toxin A). Although safety information reported in the reviewed studies is included here, readers are directed to other sources for more complete safety details.
Comparative efficacy and safety findings
There is insufficient evidence to draw firm conclusions regarding the comparative efficacy and safety of commonly used therapies included in this review for the treatment of axillary, palmar, plantar, and facial hyperhidrosis. Therefore, clinicians and patients will need to consider the SOE regarding benefits and harms for each intervention along with important contextual elements when making treatment decisions.
Individual treatment summaries
Pharmacological treatments
Efficacy and safety findings for each included pharmacological intervention (aluminum salts, anticholinergics, and botulinum toxin) are summarized in Tables 1–3.
Aluminum salts
It has been proposed that the metal ions in aluminum salts reduce sweating by damaging epithelial cells along the lumen of the sweat duct, thereby creating a plug that obstructs sweat glands47. Four studies were included that investigated aluminum salts for the treatment of axillary and palmar hyperhidrosis (no studies were identified for zirconium compounds). Of these four studies, three studies with aluminum salts were identified via the database search18,19,21 and were rated as at “unclear,” “borderline to high” or “high” RoB, respectively, but with large response rates. The fourth study22 was identified using a hand search of retrieved study reference lists and was rated at “high” RoB, but with a large response rate. SOE for efficacy, quality of life, and patient satisfaction for aluminum salts (aluminum chloride hexahydrate) for treatment of both axillary and palmar hyperhidrosis was “low.”
In axillary hyperhidrosis, two trials18,19 provided striking inconsistencies in Hyperhidrosis Disease Severity Scale (HDSS) response rates for aluminum chloride (33% vs. 72%, Table 1). Data for palmar hyperhidrosis were limited to one small, within-patient study of limited duration and lacked the use of standardized scales to measure reduction in sweat production21.
Anticholinergics
Anticholinergics reduce sweat production by blocking acetylcholine, the chemical messenger that triggers sweat glands to produce perspiration48. Topical formulations include glycopyrronium tosylate (GT) pre-moistened cloth (QBREXZA7, FDA-approved for use in primary axillary hyperhidrosis), two compounds not commercially available (glycopyrrolate wipes and glycopyrrolate-impregnated cotton pads), and oxybutynin chloride gel. This review includes five studies focused on topical anticholinergics across a range of focal regions (Table 2). Of note, no studies assessing the efficacy of oral anticholinergic drugs were found to meet our inclusion criteria.
Two reports, representing three studies, of GT in primary axillary hyperhidrosis were included: Glaser et al. reported two studies16 rated at “low” RoB and with large response rates, and Glaser et al. reported an observational open-label extension phase of those studies for safety20. Based on these trials, approximately three-fourths of patients met the response criteria (defined as ≥50% reduction in axillary sweat production) within one month of starting treatment. One within-patient study of facial hyperhidrosis from the Wade et al.12 review, reevaluated in the current review was rated as “moderate” RoB24. This trial reported a reduction in the rate of sweat production at the forehead of 36.68 ± 11.41% on day 10 (p<.025). A fifth study (palmar and plantar regions) was obtained from the database search for updates23, and was rated at “moderate” RoB with large response rates.
The highest quality of evidence (“moderate” for efficacy, quality of life, and satisfaction), representing the largest studies to date in patients with axillary hyperhidrosis, evaluates topical GT pre-moistened cloth: two trials (N = 697) demonstrated that most patients will experience a meaningful reduction in axillary sweating at 4 weeks. In those trials, the most commonly reported treatment-emergent adverse events were dry mouth, application site pain, mydriasis, oropharyngeal pain, and headache, and two serious adverse events were reported with GT (mydriasis and dehydration)16. A 44-week open-label extension study is the longest clinical safety trial available for topical GT and found that no new safety signals emerged, with demonstrated consistency across efficacy outcomes20. The remaining studies evaluating the use of topical anticholinergics consist of “low” SOE for efficacy, quality of life, satisfaction, and safety.
Typical anticholinergic-related adverse events that have been reported by patients in studies of anticholinergics include dry mouth, urinary retention, constipation, blurred vision, impaired taste, rapid heart rate and heart palpitations. An unproven causal association between oral anticholinergic drugs (tertiary amines) and dementia has been reported in elderly patients receiving long-term, high-dose therapy for indications other than hyperhidrosis49. Other sources with a focus on anticholinergic safety should be consulted for detailed safety information.
Botulinum toxin
Botulinum toxin reduces sweating by blocking nerve signals responsible for producing perspiration50, and onabotulinum toxin A (BOTOX8) is FDA-approved for treatment of severe axillary hyperhidrosis. Ten studies on the efficacy and safety of botulinum toxin in hyperhidrosis treatment are included in this review (six in axillary hyperhidrosis, three in palmar hyperhidrosis, and one in both; Table 3). The literature search yielded more studies for botulinum toxin type A injections than for any other treatment; studies evaluated use of botulinum toxin A in both axillary and palmar hyperhidrosis. The evidence for the efficacy of botulinum toxin type B studies did not meet our inclusion criteria.
Specifically, two studies in axillary hyperhidrosis25,26 were both rated at “moderate” RoB and with large response rates. Another axillary study17 was obtained from Wade et al. and was rated as “low” RoB with large response rates. The axillary study by Montaser-Kouhsari et al.27 was excluded by Wade et al. as not relevant but was included in this review because we disagreed with that assessment and was rated as “moderate” RoB with large response rates. The remaining six studies are of a within-patient design and were included in Wade et al. but are reevaluated here28–33 all were rated at “moderate” RoB with large response rates with the exception of Glogau et al., which was rated at “borderline” RoB.
Although results vary across studies, there is sufficient evidence to conclude that botulinum toxin A injections are effective in reducing sweat production in the axillae by more than 50% for 6 months or longer. The study of highest quality for botulinum toxin17 (n = 145) reported a nearly 90% decrease in mean rate of sweat production at two weeks; the rate was reduced to approximately 65% at 24 weeks (open label after 2 weeks), with nearly all (98%) subjects stating they would recommend this therapy.
There is insufficient evidence to draw firm conclusions regarding the safety of botulinum toxin A injections for treatment of axillary hyperhidrosis. Data from short-term, follow-up studies and other reports suggest that patients are likely to experience injection-site pain, which is at times severe; other non-severe adverse events have been reported. In the double-blind, placebo-controlled study with injectable botulinum toxin A17, transient adverse effects included headache, muscle soreness of the shoulder girdle, increased facial sweating, and axillary itching.
The use of topical botulinum toxin A has also been studied to a limited extent in axillary hyperhidrosis. Although no commercial formulation is currently available, evidence from two trials suggests that topical application of botulinum toxin A may provide short term sweat reduction (sweat production was reduced by approximately 20% to more than 50% at 2 weeks), lasting approximately 6 weeks with acceptable patient satisfaction26,28. In addition, there is insufficient evidence to draw firm conclusions regarding the safety of topical application of botulinum toxin A for the treatment of axillary hyperhidrosis.
Evidence to support the use of botulinum toxin A injections for the treatment of palmar hyperhidrosis is more limited, but suggests that patients may achieve a reduction of approximately 25–50% or more in palmar sweating for three weeks to six months30–33 (Table 3). There is insufficient evidence to draw conclusions regarding the safety of botulinum toxin A injections for the treatment of palmar hyperhidrosis. Reported adverse events across the palmar trials include hand pain, finger numbness, thumb and finger weakness, excessively dry hands, indigestion/heartburn and slight transient reduction of power of finger grip lasting 2–5 weeks. There is uncertainty about major or long-term adverse events. Efficacy, quality of life, and patient satisfaction were rated as borderline; SOE for safety was rated as low.
Medical device treatments
Medical devices used to treat primary hyperhidrosis are designed to alter eccrine glands (curettage, laser therapy, microwave, fractional needle radiotherapy and ultrasound therapies) or affect their function (iontophoresis). This review includes 15 studies on these devices, nine in axillary and six in palmar hyperhidrosis. Efficacy and safety findings for each included medical device are summarized in Tables 4 and 5. There is insufficient evidence to draw conclusions regarding the efficacy and safety of curettage, laser therapy, fractionated microneedle radiofrequency, microwave therapy or ultrasound therapy compared to other available therapies for the treatment of axillary hyperhidrosis.
Fractionated microneedle radiofrequency
Fractional microneedle radiofrequency (FMR) is a recently developed, minimally invasive method for delivering thermal energy to the interface between the epidermis and subcutaneous tissue. This technology uses rapid penetration with microneedles, which causes irreversible thermolysis of apocrine and eccrine sweat glands without destroying the epidermis. One single-blind, within-patient, right-left comparison study in axillary hyperhidrosis was included in the present analysis35 (moderate RoB). Efficacy, quality of life, patient satisfaction, and safety SOE were rated as “low” (Table 4).
Lasers
Evidence from one within-patient, unblinded, randomized trial evaluating five cycles of an 800 nm diode laser compared to no treatment in adults with axillary hyperhidrosis was included in the present analysis34. A significant decrease in sweating rate was observed on both the laser-treated sites and the untreated sides. Post-treatment biopsy results were not consistent with tissue destruction. Efficacy, quality of life, and patient satisfaction were rated as low to borderline, and safety SOE was rated as “low” (Table 4).
Micro-focused ultrasound
Micro-focused ultrasound waves cause vibration of tissues resulting in heating and destruction of axillary sweat glands. Two randomized, within-patient, double-blind, sham-controlled pilot studies of micro-focused ultrasound plus visualization in axillary hyperhidrosis were included in the present analysis36. Efficacy, quality of life, patient satisfaction, and safety were rated as having “low” SOE (Table 4).
Liposuction curettage
Liposuction curettage is performed at the dermal–subcutaneous interface using a liposuction device and a sharp, rasping-type cannula to damage the sweat glands. Three studies evaluating curettage were included in the present analysis29,25,37 (Table 4), two of which were comparator studies of curettage and botulinum toxin29,25 (studies also are included in Table 3 for botulinum toxin arm). Efficacy, quality of life, and patient satisfaction were rated as “borderline” to “moderate”; safety was rated as having “low” SOE. There is sufficient evidence to conclude that liposuction curettage for the treatment of axillary hyperhidrosis is effective in reducing sweat production by 30% to over 80% for 6 months or more25,29,37. There is insufficient evidence to draw conclusions regarding long-term safety of subcutaneous curettage for the treatment of axillary hyperhidrosis but limited short-term evidence suggests that patients should expect to experience axillary discomfort, soreness or pain. Other reported adverse events include dysesthesias, hyperpigmentation, “bothersome” scar formation, focal hair loss, subcutaneous fibrotic bridles, seromas, wound infection, bleeding, hematoma and skin necrosis.
Microwave thermolysis
Microwave therapy devices (e.g. miraDry, FDA-cleared for treatment of primary axillary hyperhidrosis) focus heat at the skin-subcutaneous tissue interface causing irreversible thermolysis of apocrine and eccrine sweat glands. This review included two case reports for evidence synthesis of safety data38,39 (Table 4); no studies met criteria for efficacy evaluation. Efficacy, quality of life, patient satisfaction, and safety were rated as having “low” SOE. Suh et al.38 and Chang et al.39 each present a case report for ulnar and median nerve injury following microwave thermolysis, and in one patient39, significant sensory and motor deficits had not resolved at the 6-month follow-up.
Iontophoresis
Iontophoresis typically delivers electrical current (15–20 mA) through tap water to treat hyperhidrosis but very limited evidence suggests it can be performed “dry.” While the mechanism of action is not known, hypotheses include inhibition of nerve transmission, as well as inhibition or obstruction of sweat flow by altering pH or ion deposition in sweat ducts. This review includes seven studies on the use of iontophoresis to treat hyperhidrosis: six in palmar hyperhidrosis (four tap water iontophoresis40–43, two dry iontophoresis44,45 and one in axillary hyperhidrosis27 comparing the effect of botulinum toxin solution administered via iontophoresis to injected botulinum toxin; all had large response rates.
Tap water iontophoresis
Based on evidence from four trials, there is sufficient evidence (SOE rating of “borderline to moderate”) to conclude that tap water iontophoresis for the treatment of palmar hyperhidrosis is effective in producing a clinically meaningful reduction in sweat production (reported reductions of 30–90% after 1–4 weeks of treatment and lasting several weeks to several months) with acceptable patient satisfaction27,40–43. Reduction in sweating maybe maintained by repeat treatments every few days to 2 weeks. No valid evidence was found regarding the use of tap water iontophoresis for the treatment of axillary or plantar hyperhidrosis.
There is insufficient evidence to draw conclusions regarding the safety of iontophoresis for the treatment of palmar hyperhidrosis but limited short-term evidence suggests that patients are likely to experience minor discomfort. Reported adverse events include transient tingling, erythema and vesiculation of the skin. There is uncertainty about major or long-term adverse events. Efficacy, quality of life, and patient satisfaction were rated as “borderline” to “moderate,” while safety SOE was rated as “low.”
Dry iontophoresis
Based on the two studies included in the present analyses44,45 efficacy, quality of life, patient satisfaction, and safety SOE were rated as “low.”
Combined drug therapy and iontophoresis
Based on the single study included in the present analysis27 (axillary hyperhidrosis), the evidence for combining drug therapy with iontophoresis is inconclusive.
Regardless of the type of iontophoresis used, there is insufficient evidence to draw conclusions regarding the efficacy, satisfaction and safety of iontophoresis compared to other available therapies for the treatment of palmar hyperhidrosis.
Discussion
This report provides an evidence-based review of commonly used interventions for the treatment of primary hyperhidrosis. The efficacy and safety evidence provided in this review can be used to optimize treatment strategies for patients suffering from primary hyperhidrosis. To make optimal decisions, healthcare providers and patients should be informed of not only a study’s results, but also the quality of evidence supporting the results. Considering the quality of the evidence when examining the results of studies is important because bias tends to favor the treatment being studied, and lower quality studies are more likely to report inaccurate results; highly biased studies may distort results by more than 50%51–53. Shared decision-making and the use of decision support materials (often called patient decision aids) improve decision-making around many different preference-sensitive clinical choices. The SOE information included in this review, together with summarized efficacy and safety data, will be helpful in creating decision support materials, which have been shown to improve shared decision-making discussions54,55.
A key aspect of this analysis was a critical appraisal of studies of aluminum/zirconium compounds, as this was not a component of the prior Wade et al. analyses (no studies of zirconium salt compounds met our inclusion criteria). In addition, evidence from studies with large response rates and/or those that used a within-patient design were considered. Overall, there was a lack of high-quality of evidence to support use of treatments for primary hyperhidrosis; the SOE was highest for topical glycopyrronium cloth (2.4%) and botulinum toxin A injections for the treatment of axillary hyperhidrosis, which increases our confidence in the reliability of reported results for these two interventions. There were more studies identified in axillary hyperhidrosis than in other regions of the body (Figure 4).
Although there were only two studies investigating topical glycopyrronium cloth for the treatment of axillary hyperhidrosis, they were of “moderate” quality with large groups, good designs and execution for both efficacy and safety, and reported consistent results. In these two key clinical trials for glycopyrronium cloth, most treatment-emergent adverse events were transient and reversible. Anticholinergic side effects are a potential risk with glycopyrronium cloth treatment, and Glaser et al.16 noted that patients who do not wash their hands following application may inadvertently transfer the drug to another body area such as the eyes. Authors concluded that unilateral ophthalmologic events of mydriasis and blurred vision were most likely due to local exposure, whereas anticholinergic side effects such as dry mouth and urinary hesitation were likely a result of systemic exposure.
With respect to botulinum toxin A, the cumulative amount of reliable data relevant to treatment of axillary hyperhidrosis increases confidence in the results. Some studies for botulinum toxin A injections and topical treatments were of “low to borderline” quality, and most clinical trials reviewed did not provide sufficient evidence to draw firm conclusions about safety due to lack of reporting, small sample size, limitations of study design, and short study duration. Even when safety evidence is of low quality, reported adverse events and serious adverse events along with the quality of the evidence provide valuable information to healthcare providers and patients. We found two case studies of patients diagnosed with severe median and ulnar nerve injury following microwave thermolysis whose symptoms either did not resolve at a 6-month follow-up or resolved only after intensive physical therapy for 6 months38,39.
In addition to considerations of efficacy and safety, patients should also be made aware of the differences between treatment modalities that may affect their treatment choices (e.g. potential discomfort or pain, ease of application, inconvenience, cost, and ease of adherence). Patients should be provided with information sufficient to assist them in making informed decisions that satisfy their personal healthcare needs, values and preferences.
Another critical aspect of this analysis was a thorough evaluation of studies that utilized a within-patient design (in keeping with the most commonly used terminology in Wade et al.; many other synonyms exist). In this review, all but one of the studies using within-patient design were also shown to have large response rates. For the context of this analysis using hyperhidrosis studies, an understanding of the strengths of within-patient trials compared to trials utilizing a between-group design is particularly important, as the within-patient design is frequently encountered in studies of hyperhidrosis and allows comparison of treatments involving right and left axillae, palms or soles within the same patient.
When evaluated with criteria used for between-group trials, the within-patient design is likely to be rated as “at high risk of bias” for several reasons, including that they tend to be characterized by small populations and frequently lack randomization and blinding. In traditional between-group trials, such as RCTs, selection and bias are key considerations when assessing a study for RoB. However, for many dermatological conditions, including primary hyperhidrosis, within-patient designs may in fact have certain advantages in terms of establishing balanced study groups (i.e. those with balanced baseline clinical and demographic characteristics). In within-patient trials, selection bias may be reduced because one side of the body is compared to the opposite side in the same person, and demographic and clinical prognostic variables are similar or equal. For example, potential differences in age, sex, genetics, laboratory values, comorbidities and other prognostic variables are presumably less of a threat to validity using a within-patient design because there is only one body with two comparison sites. We found very little evidence in the medical literature regarding the strengths and weaknesses of the within-patient study design as there is little guidance available on critical appraisal of such studies. To facilitate our review, we developed a list of considerations (as distinguished from criteria), which is provided in Supplementary Materials (p. 81).
Some of these considerations were derived from a brief literature review, consideration of crossover-design studies, general considerations, and our knowledge of study bias and how it may affect reported results. Further well-designed and executed studies comparing outcomes from within-patient studies to outcomes from between group designs for the same conditions and treatments will be required to understand how within-patient studies might differ from between-group studies in terms of validity considerations. If the strength of the within-patient study design is confirmed, fewer study subjects would be required which would result in lowered exposure and inconvenience to study subjects, reduced study costs and minimized distortion of results due to bias.
Conclusions
Optimal treatment choice depends upon understanding the quality of the evidence regarding each treatment’s efficacy and safety (considerations of convenience, cost, etc. may also be important but are beyond the scope of this review). In this systematic review, we evaluate the efficacy, health-related quality of life, satisfaction, and safety of commonly used interventions in the treatment of primary hyperhidrosis of the head, axilla, palms, and soles in children and adults. Information provided in this review will be of use to patients and other decision-makers. We also provide detailed information about the quality of the hyperhidrosis evidence in addition to the reported results of included studies.
In hyperhidrosis, as in other clinical conditions, treatment decisions should be patient centered. At this time, because of the quality of evidence, only imprecise estimates of effect are possible for most commonly employed treatments for hyperhidrosis, and statements about comparative effectiveness are not possible.
Supplementary Material
Footnotes
Dermira Inc, Menlo Park, CA
Allergan, Inc., Irvine, CA
Miramar Labs, Inc., Santa Clara, CA
Transparency
Declaration of funding
This work was funded by Dermira Inc., a wholly-owned subsidiary of Eli Lilly and Company.
Declaration of financial/other relationships
MES and SAS: In accordance with Taylor & Francis policy and our ethical obligation as researchers, we are reporting that Dermira, Inc., a wholly owned subsidiary of Eli Lilly and company, funded this research. We have no other financial disclosures or conflicts to report. KKG: is employed by Dermira, Inc., a wholly owned subsidiary of Eli Lilly and Company. A reviewer on this manuscript has disclosed that they are a board member of international hyperhidrosis society. The other peer reviewers on this manuscript have no other relevant financial relationships or otherwise to disclose.
Acknowledgements
Medical writing support for this manuscript was provided by Amel Alqadah, PhD and Jennifer Hepker, PhD and Merrilee Johnstone, PhD of Prescott Medical Communications Group (Chicago, IL), with financial support from Dermira, Inc, a wholly owned subsidiary of Eli Lilly and Company.
References
- 1.Doolittle J, Walker P, Mills T, et al. . Hyperhidrosis: an update on prevalence and severity in the United States. Arch Dermatol Res. 2016;308(10):743–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glaser DA, Hebert A, Pieretti L, et al. . Understanding patient experience with hyperhidrosis: a national survey of 1,985 patients. J Drugs Dermatol. 2018;17(4):392–396. [PubMed] [Google Scholar]
- 3.Hamm H, Naumann MK, Kowalski JW, et al. . Primary focal hyperhidrosis: disease characteristics and functional impairment. Dermatology. 2006;212(4):343–353. [DOI] [PubMed] [Google Scholar]
- 4.Naumann MK, Hamm H, Lowe NJ.. Effect of botulinum toxin type A on quality of life measures in patients with excessive axillary sweating: a randomized controlled trial. Br J Dermatol. 2002;147(6):1218–1226. [DOI] [PubMed] [Google Scholar]
- 5.Kamudoni P, Mueller B, Halford J, et al. . The impact of hyperhidrosis on patients’ daily life and quality of life: a qualitative investigation. Health Qual Life Outcomes. 2017;15(1):121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nawrocki S, Cha J.. The etiology, diagnosis, and management of hyperhidrosis: a comprehensive review: therapeutic options. J Am Acad Dermatol. 2019;81(3):669–680. [DOI] [PubMed] [Google Scholar]
- 7.QBREXZA® (glycopyrronium) cloth [prescribing information]. Menlo Park (CA): Dermira Inc.; 2018. Available from: http://pi.dermira.com/QbrexzaPI.pdf
- 8.BOTOX® (onabotulinumtoxinA) for injection, for intramuscular, intradetrusor, or intradermal use [prescribing information]. Irvine (CA): Allergan, Inc.; 2011. Available from: https://media.allergan.com/actavis/actavis/media/allergan-pdf-documents/product-prescribing/20190620-BOTOX-100-and-200-Units-v3-0USPI1145-v2-0MG1145.pdf
- 9.Wechter T, Feldman SR, Taylor SL. The treatment of primary focal hyperhidrosis. Skin Therapy Lett. 2019;24(1):1–7. [PubMed] [Google Scholar]
- 10.Ioannidis JPA, Stuart ME, Brownlee S, et al. . How to survive the medical misinformation mess. Eur J Clin Invest. 2017;47(11):795–802. [DOI] [PubMed] [Google Scholar]
- 11.Wade R, Rice S, Llewellyn A, et al. . Interventions for hyperhidrosis in secondary care: a systematic review and value-of-information analysis. Health Technol Assess. 2017;21(80):1–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wade R, Llewellyn A, Jones-Diette J, et al. . Interventional management of hyperhidrosis in secondary care: a systematic review. Br J Dermatol. 2018;179(3):599–608. [DOI] [PubMed] [Google Scholar]
- 13.PICO annotation ; 2020; [cited 2020 Jun 30]. Available from: https://training.cochrane.org/resource/cochrane-information-specialists-handbook/12-pico-annotation
- 14.Collaboration TC . Methodological expectations of Cochrane Intervention Reviews (MECIR): standards for the reporting of plain language summaries in new Cochrane Intervention Reviews; version 1; 2013; [cited 2019 Aug 22]. Available from: https://methods.cochrane.org/sites/default/files/public/uploads/pleacs_2019.pdf
- 15.Glasziou P, Chalmers I, Rawlins M, et al. . When are randomised trials unnecessary? Picking signal from noise. BMJ. 2007;334(7589):349–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glaser DA, Hebert AA, Nast A, et al. . Topical glycopyrronium tosylate for the treatment of primary axillary hyperhidrosis: results from the ATMOS-1 and ATMOS-2 phase 3 randomized controlled trials. J Am Acad Dermatol. 2019;80(1):128–138e2. [DOI] [PubMed] [Google Scholar]
- 17.Heckmann M, Ceballos-Baumann AO, Plewig G.. Botulinum toxin A for axillary hyperhidrosis (excessive sweating). N Engl J Med. 2001;344(7):488–493. [DOI] [PubMed] [Google Scholar]
- 18.Flanagan KH, Glaser DA.. An open-label trial of the efficacy of 15% aluminum chloride in 2% salicylic acid gel base in the treatment of moderate-to-severe primary axillary hyperhidrosis. J Drugs Dermatol. 2009;8(5):477–480. [PubMed] [Google Scholar]
- 19.Flanagan KH, King R, Glaser DA.. Botulinum toxin type a versus topical 20% aluminum chloride for the treatment of moderate to severe primary focal axillary hyperhidrosis. J Drugs Dermatol. 2008;7(3):221–227. [PubMed] [Google Scholar]
- 20.Glaser DA, Hebert AA, Nast A, et al. . A 44-week open-label study evaluating safety and efficacy of topical glycopyrronium tosylate in patients with primary axillary hyperhidrosis. Am J Clin Dermatol. 2019;20(4):593–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goh CL. Aluminum chloride hexahydrate versus palmar hyperhidrosis. Evaporimeter assessment. Int J Dermatol. 1990;29(5):368–370. [DOI] [PubMed] [Google Scholar]
- 22.Scholes KT, Crow KD, Ellis JP, et al. . Axillary hyperhidrosis treated with alcoholic solution of aluminium chloride hexahydrate. Br Med J. 1978;2(6130):84–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Artzi O, Loizides C, Zur E, et al. . Topical oxybutynin 10% gel for the treatment of primary focal hyperhidrosis: a randomized double-blind placebo-controlled split area study. Acta Derm Venereol. 2017;97(9):1120–1124. [DOI] [PubMed] [Google Scholar]
- 24.Hyun MY, Son IP, Lee Y, et al. . Efficacy and safety of topical glycopyrrolate in patients with facial hyperhidrosis: a randomized, multicentre, double-blinded, placebo-controlled, split-face study. J Eur Acad Dermatol Venereol. 2015;29(2):278–282. [DOI] [PubMed] [Google Scholar]
- 25.Budamakuntla L, Loganathan E, George A, et al. . Comparative study of efficacy and safety of botulinum toxin a injections and subcutaneous curettage in the treatment of axillary hyperhidrosis. J Cutan Aesthet Surg. 2017;10(1):33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lueangarun S, Sermsilp C, Tempark T.. Topical botulinum toxin type a liposomal cream for primary axillary hyperhidrosis: a double-blind, randomized, split-site, vehicle-controlled study. Dermatol Surg. 2018;44(8):1094–1101. [DOI] [PubMed] [Google Scholar]
- 27.Montaser-Kouhsari L, Zartab H, Fanian F, et al. . Comparison of intradermal injection with iontophoresis of abobotulinum toxin A for the treatment of primary axillary hyperhidrosis: a randomized, controlled trial. J Dermatolog Treat. 2014;25(4):337–341. [DOI] [PubMed] [Google Scholar]
- 28.Glogau RG. Topically applied botulinum toxin type A for the treatment of primary axillary hyperhidrosis: results of a randomized, blinded, vehicle-controlled study. Dermatol Surg. 2007;33(s1):S76–S80. [DOI] [PubMed] [Google Scholar]
- 29.Ibrahim O, Kakar R, Bolotin D, et al. . The comparative effectiveness of suction-curettage and onabotulinumtoxin-A injections for the treatment of primary focal axillary hyperhidrosis: a randomized control trial. J Am Acad Dermatol. 2013;69(1):88–95. [DOI] [PubMed] [Google Scholar]
- 30.Lowe NJ, Yamauchi PS, Lask GP, et al. . Efficacy and safety of botulinum toxin type A in the treatment of palmar hyperhidrosis: a double-blind, randomized, placebo-controlled study. Dermatol Surg. 2002;28(9):822–827. [DOI] [PubMed] [Google Scholar]
- 31.Naver H, Swartling C, Aquilonius SM.. Palmar and axillary hyperhidrosis treated with botulinum toxin: one-year clinical follow-up. Eur J Neurol. 2000;7(1):55–62. [DOI] [PubMed] [Google Scholar]
- 32.Schnider P, Binder M, Auff E, et al. . Double-blind trial of botulinum A toxin for the treatment of focal hyperhidrosis of the palms. Br J Dermatol. 1997;136(4):548–552. [PubMed] [Google Scholar]
- 33.Yamashita N, Shimizu H, Kawada M, et al. . Local injection of botulinum toxin A for palmar hyperhidrosis: usefulness and efficacy in relation to severity. J Dermatol. 2008;35(6):325–329. [DOI] [PubMed] [Google Scholar]
- 34.Bechara FG, Georgas D, Sand M, et al. . Effects of a long-pulsed 800-nm diode laser on axillary hyperhidrosis: a randomized controlled half-side comparison study. Dermatol Surg. 2012;38(5):736–740. [DOI] [PubMed] [Google Scholar]
- 35.Fatemi Naeini F, Abtahi-Naeini B, Pourazizi M, et al. . Fractionated microneedle radiofrequency for treatment of primary axillary hyperhidrosis: a sham control study. Australas J Dermatol. 2015;56(4):279–284. [DOI] [PubMed] [Google Scholar]
- 36.Nestor MS, Park H.. Safety and efficacy of micro-focused ultrasound plus visualization for the treatment of axillary hyperhidrosis. J Clin Aesthet Dermatol. 2014;7(4):14–21. [PMC free article] [PubMed] [Google Scholar]
- 37.Tronstad C, Helsing P, Tonseth KA, et al. . Tumescent suction curettage vs. curettage only for treatment of axillary hyperhidrosis evaluated by subjective and new objective methods. Acta Derm Venereol. 2014;94(2):215–220. [DOI] [PubMed] [Google Scholar]
- 38.Suh DH, Lee SJ, Kim K, et al. . Transient median and ulnar neuropathy associated with a microwave device for treating axillary hyperhidrosis. Dermatol Surg. 2014;40(4):482–485. [DOI] [PubMed] [Google Scholar]
- 39.Chang CK, Chen CY, Hsu KF, et al. . Brachial plexus injury after microwave-based treatment for axillary hyperhidrosis and osmidrosis. J Cosmet Laser Ther. 2017;19(7):439–441. [DOI] [PubMed] [Google Scholar]
- 40.Stolman LP. Treatment of excess sweating of the palms by iontophoresis. Arch Dermatol. 1987;123(7):893–896. [PubMed] [Google Scholar]
- 41.Dahl JC, Glent-Madsen L.. Treatment of hyperhidrosis manuum by tap water iontophoresis. Acta Derm Venereol. 1989;69(4):346–348. [PubMed] [Google Scholar]
- 42.Karakoc Y, Aydemir EH, Kalkan MT.. Placebo-controlled evaluation of direct electrical current administration for palmoplantar hyperhidrosis. Int J Dermatol. 2004;43(7):503–505. [DOI] [PubMed] [Google Scholar]
- 43.Kim DH, Kim TH, Lee SH, et al. . Treatment of palmar hyperhidrosis with tap water iontophoresis: a randomized, sham-controlled, single-blind, and parallel-designed clinical trial. Ann Dermatol. 2017;29(6):728–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Na GY, Park BC, Lee WJ, et al. . Control of palmar hyperhidrosis with a new "dry-type" iontophoretic device. Dermatol Surg. 2007;33(1):57–61. [DOI] [PubMed] [Google Scholar]
- 45.Choi YH, Lee SJ, Kim DW, et al. . Open clinical trial for evaluation of efficacy and safety of a portable "dry-type" iontophoretic device in treatment of palmar hyperhidrosis. Dermatol Surg. 2013;39(4):578–583. [DOI] [PubMed] [Google Scholar]
- 46.Dechartres A, Trinquart L, Boutron I, et al. . Influence of trial sample size on treatment effect estimates: meta-epidemiological study. BMJ. 2013;346(14):f2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Holzle E, Braun-Falco O.. Structural changes in axillary eccrine glands following long-term treatment with aluminium chloride hexahydrate solution. Br J Dermatol. 1984;110(4):399–403. [DOI] [PubMed] [Google Scholar]
- 48.Brackenrich J, Fagg C.. Hyperhidrosis. Treasure Island (FL): StatPearls; 2020. [Google Scholar]
- 49.Gray SL, Anderson ML, Dublin S, et al. . Cumulative use of strong anticholinergics and incident dementia: a prospective cohort study. JAMA Intern Med. 2015;175(3):401–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grunfeld A, Murray CA, Solish N.. Botulinum toxin for hyperhidrosis: a review. Am J Clin Dermatol. 2009;10(2):87–102. [DOI] [PubMed] [Google Scholar]
- 51.Moher D, Pham B, Jones A, et al. . Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet. 1998;352(9128):609–613. [DOI] [PubMed] [Google Scholar]
- 52.Poolman RW, Struijs PA, Krips R, et al. . Reporting of outcomes in orthopaedic randomized trials: does blinding of outcome assessors matter? J Bone Joint Surg Am. 2007;89(3):550–558. [DOI] [PubMed] [Google Scholar]
- 53.Schulz KF, Chalmers I, Hayes RJ, et al. . Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273(5):408–412. [DOI] [PubMed] [Google Scholar]
- 54.Elwyn G, Frosch D, Thomson R, et al. . Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Makoul G, Clayman ML.. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;60(3):301–312. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.