Abstract
Objectives:
Assess a conceptual model linking caregiving factors to care recipient mortality in a large representative sample of older adults with disability.
Design:
Descriptive longitudinal study with five-year mortality follow-up among older adults with disability. Baseline in person and telephone interviews / assessments of older adults with disability and their family caregivers carried out in 2011.
Setting:
Representative samples of older U.S. population and their family caregivers.
Participants:
U.S. representative samples of older adults with disability aged 65 and over (National Health and Aging Study [NHATS]) and their family caregivers (National Study of Caregiving [NSOC]) (www.nhats.org), (N = 1262).
Measurement:
Controlling for known risk factors for mortality in older adults, including age, gender, race, education, socioeconomic status, disability, and cognitive status, we assess the role of three caregiving factors (depression, anxiety, and burden) and three mediating factors (care recipient depression, anxiety, and unmet needs for care) as predictors of care recipient mortality.
Results:
Caregiver burden, care recipient depression, and care recipient unmet needs are independent predictors of care recipient mortality.
Conclusions:
Caregiving factors may play an important role in the survival of their care recipients. This is a relatively unexplored research area that calls for fine-grained studies capturing caregiver - care recipient health related interactions over time.
Keywords: caregiving, caregiver burden, caregiver mental health, care recipient mortality
Introduction
Much of the family caregiving literature focuses on the impact of caregiving on the care provider, including effects on psychological and physical health, social relationships, and economic well-being (1). This literature in turn has generated wide-ranging research programs to identify risk factors for adverse caregiver (CG) outcomes as well as intervention strategies to mitigate the negative effects of caregiving (2). To a lesser extent, researchers have documented the impact of caregiving on care recipient (CR) outcomes, including care recipient behavior (3), psychological symptoms such as depression (4), time to nursing home admission (5), and health care expenditures (6).
An emergent recent development in the caregiving literature is a focus on care recipient mortality as an outcome. Controlling for known risk factors for mortality in older adults (7) such as health, functional status, and demographic characteristics, what caregiving related factors contribute to survival time in the care recipient? Lwi and colleagues (8) found that poor caregiver mental health predicted mortality of patients with neurodegenerative diseases. In a small sample of dementia patients and their caregivers (n = 91), Brodaty and colleagues also (9) showed that caregiver psychological morbidity was associated with shorter patient survival times. Boele and colleagues (10) explored depression, anxiety, burden, and mastery as predictors of patient mortality in a sample of caregivers caring for patients with glioblastoma multiform (GBM). Only caregiver mastery was found to be a significant predictor of patient mortality. Pristavec and Luth (11), using a large representative sample of older adult care recipients and their caregivers, showed that older adults whose caregiver reported higher levels of burden had a significantly higher mortality risk during the six-year follow-up period.
The present study advances existing research in this area by exploring the role of caregiving factors and possible mechanisms on care recipient mortality in a large representative sample of older adults with disability and their caregivers. A preliminary conceptual model linking caregiving factors to CR mortality is presented in Figure 1. The existing literature suggests that three caregiver factors (depression, anxiety, and burden) impact CR mortality through two broad categories of mechanisms: 1) intrapsychic factors such as CR depression and anxiety; and 2) inadequate or poor quality care provided to the CR. Intrapsychic mechanisms linking caregiver status to mortality might occur through contagion of emotions or behavioral mimicry (8, 12). Individuals in close relationships have reciprocal effects on each other’s emotional status, especially when the emotions are negative (e.g., anger, fear, sadness). Thus, depressed caregivers may instigate similar affect in their care recipients, and vice versa. Inadequate or poor quality care includes failure to meet the functional and mobility needs of the CR (i.e., typically measured as unmet needs), poor medication management, missed doctor appointments, physical / psychological abuse, and failure to detect significant CR declines that require medical intervention. As shown in the model, CG depression / anxiety is thought to impact both CR depression / anxiety and the quality of care provided to the CR. Burden is thought to impact CR mortality primarily through inadequate or poor quality care.
Figure 1.
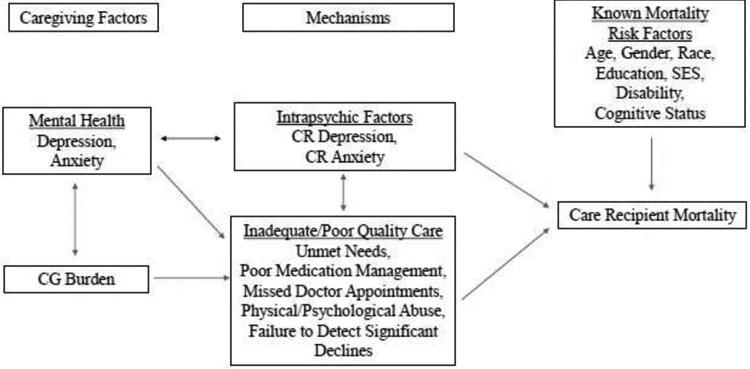
Conceptual model linking caregiving factors to care recipient mortality
Controlling for known risk factors for mortality in older adults, we assess the role of the caregiver and mediating factors as predictors of mortality. In our first Cox proportional hazards model we explore the association between the three hypothesized caregiving factors, CG depression / anxiety and burden on CR mortality, and based on the existing literature, we predict statistically significant associations between depression / anxiety, burden and survival time. In a second Cox model we test the independent effects of CR depression / anxiety and unmet needs on mortality (note the available data limited our ability to explore other indicators of inadequate / poor quality indicators), and we predict statistically significant associations between depression / anxiety, unmet needs, and survival time. In a final model, we simultaneously examine the effects of both caregiving factors and mediating factors on CR mortality. We predict that the effects of caregiving factors observed in model 1 will be attenuated such that they are no longer significant predictors of mortality, while the effects of mediating variables will remain significant.
Methods
Data
The data used in this study are publicly available, do not contain individual identifiers, and are, therefore, exempt from institutional review board review. A detailed description of the data sources for this study was provided in a recent publication (13), and much of this section is repeated from this source.
Data are drawn from the 2011 National Health and Aging Trends Study (NHATS) and the National Study of Caregiving (NSOC) (www.nhats.org), two linked national surveys that provide information regarding a well-defined population of older adults and their family caregivers. The NHATS is nationally representative of Americans 65 years and older. The NSOC is a nationally representative survey of family members and other unpaid caregivers who assist older persons with disabilities. The NSOC participants were identified from the NHATS helper roster on the basis of being a family member or an unpaid helper who provided assistance with mobility, self-care, household activities, transportation, or medically oriented tasks.
Of 7609 NHATS participants living in the community or in a residential care facility, 2423 were included in the NSOC sampling frame, and 4935 helpers met eligibility criteria for the NSOC. In cases where an NHATS care recipient was linked to more than one caregiver, the caregiver who reported providing the most hours of care per month was included in the current analyses. The base sample for this analysis was 1,348 “primary caregivers” of NHATS respondents who reported difficulty or were receiving help with at least one of 12 instrumental activities of daily living (IADL), basic activities of daily living (ADL), or mobility tasks (i.e., 18 NHATS respondents with an NSOC caregiver did not meet this criteria). The final sample consisted of the subset of 1,262 primary caregivers and care recipients who had valid data on variables included in the models (see below). Comparisons between the 86 cases with missing data versus the 1,262 included cases showed no significant differences in any of the outcome, predictor, or sociodemographic control variables.
Measures
This study included measures from both older disabled adults (NHATS) and their linked family caregivers (NSOC). Baseline NHATS and NSOC assessments were conducted in 2011.
Survival time.
The primary outcome in the analyses was care recipient five-year all-cause mortality (i.e., through NHATS Round 5 in 2016). More specifically, months from baseline assessment date to month of death (exact death dates were not available) was modeled in Cox proportional hazards models. For censored cases with complete follow-up, time to event was months between NHATS baseline and wave 5 assessment dates. For censored cases lost to follow-up, time to event was months between NHATS baseline and attrition dates. All predictors and covariates were taken from the 2011 baseline assessment.
Caregiver depression and anxiety.
Caregiver depression was measured with the two-item version of the Patient Health Questionnaire (PHQ), and a cutoff score was used to classify caregivers as at risk for depression versus not (NSOC; www.nhats.org). Similarly, caregiver anxiety was measured with the two-item version of the Patient Health Questionnaire (PHQ), and a cutoff score was used to classify caregivers as at risk for anxiety disorder versus not (NSOC; www.nhats.org).
Caregiver burden.
This was a six item index including how often (“very much,” “somewhat,” “not so much”) the caregiver reports “being exhausted when you go to bed at night,” “have more things to do than you can handle,” “don’t have time for yourself” “as soon as you get a routine going, care recipient’s needs change.” Two additional items asked if helping the recipient is emotionally and physically difficult for them (yes / no). The index (range = 0-6) consisted of a count of “very much” responses to the first four items and “yes” responses to the last two items. Three categories were created for analysis: 1) Low burden (score of 0 on the index); 2) Medium burden (score of 1 or 2); and 3) high burden (score of 3 or higher).
Care recipient adverse consequences of unmet needs.
NHATS respondents were asked single questions (for each of 4 ADL / 3 mobility / 5 IADL tasks) assessing whether during the past month they experienced a negative consequence because there was no one there to help (for those reporting that they never performed the task without help in a prior question); or it was too difficult to do by themselves without additional help (for those reporting that they performed the task by themselves at lease sometimes). Adverse consequences of unmet ADL needs included wet or soiled clothing; went without eating; went without bathing / showering; and went without getting dressed. Adverse consequences of unmet mobility needs included had to stay in bed; had to stay inside; and unable to go places in home / building. Adverse consequences of unmet IADL needs included went without clean laundry; went without groceries; went without a hot meal; went without paying bills; and made a medication mistake. For analyses, separate indicators for any ADL / mobility adverse consequences and any IADL adverse consequences were created, given that they reflect different levels of disability / needs for care and typically occur at earlier (IADL) and later (ADL / mobility) stages of the caregiving trajectory.
Caregiver sex and caregiver relationship to care recipient were also included (see Table 1 for coding).
TABLE 1.
Sample descriptive statistics (n = 1,262; unweighted); and bivariate associations between CR risk factors, CG factors, CR mechanisms and CR mortality by wave 5 (n=1,262; weighted)
| Predictor | Unweighted | CR Died Before Wave 5 (Weighted) |
||||
|---|---|---|---|---|---|---|
| N | % | % No | % Yes | χ2(df) | p | |
| CR Died Before Wave 5 | ||||||
| No | 762 | 60.4 | ||||
| Yes | 500 | 39.6 | ||||
| Months to Death (deceased CRs only) | ||||||
| 25th percentile | 10.0 | |||||
| 50th percentile | 22.0 | |||||
| 75th percentile | 34.0 | |||||
| Mean and standard deviation | 23.3 | 14.1 | ||||
| CR Sex | ||||||
| Male | 396 | 31.4 | 30.9 | 38.0 | 6.55(1) | 0.028 |
| Female | 866 | 68.6 | 69.1 | 62.0 | ||
| CR Age (mean) | 81.6 | 77.4 | 82.7 | 72.13a | <0.001 | |
| CR Race | ||||||
| White (non-Hispanic) | 790 | 62.6 | 74.6 | 82.9 | 12.24(3) | 0.017 |
| Black (non-Hispanic) | 356 | 28.2 | 12.7 | 9.7 | ||
| Hispanic | 88 | 7.0 | 9.7 | 5.8 | ||
| Other | 28 | 2.2 | 3.1 | 1.6 | ||
| CR Education | ||||||
| High school or less | 815 | 64.6 | 58.8 | 62.6 | 1.88(2) | 0.500 |
| Some college | 283 | 22.4 | 26.4 | 23.5 | ||
| Bachelor’s degree or higher | 164 | 13.0 | 14.9 | 13.9 | ||
| CR Medicaid Recipient | ||||||
| No | 961 | 76.2 | 78.5 | 82.5 | 2.93(1) | 0.119 |
| Yes | 301 | 23.9 | 21.5 | 17.5 | ||
| CR Disability Status | ||||||
| Probable dementia (only) | 239 | 18.9 | 13.8 | 20.7 | 102.38(3) | <0.001 |
| 2+ ADLs (only) | 188 | 14.9 | 14.2 | 17.1 | ||
| Both probable dementia & 2+ ADLs | 219 | 17.4 | 8.4 | 24.9 | ||
| Neither probable dementia nor 2+ ADLs | 616 | 48.8 | 63.6 | 37.3 | ||
| CG Sex | ||||||
| Male | 414 | 32.8 | 41.8 | 30.4 | 16.04(1) | <0.001 |
| Female | 848 | 67.2 | 58.2 | 69.6 | ||
| CG Relationship to CR | ||||||
| Spouse | 340 | 26.9 | 39.7 | 27.1 | 28.66(3) | <0.001 |
| Daughter / daughter-in-law / step-daughter | 490 | 38.8 | 28.7 | 41.7 | ||
| Son / son-in-law / step-son | 204 | 16.2 | 15.7 | 16.9 | ||
| Other | 228 | 18.1 | 16.0 | 14.2 | ||
| CG Depressed | ||||||
| No | 1084 | 85.9 | 86.4 | 84.7 | 0.67(1) | 0.479 |
| Yes | 178 | 14.1 | 13.6 | 15.3 | ||
| CG Anxious | ||||||
| No | 1087 | 86.1 | 86.8 | 83.1 | 3.15(1) | 0.127 |
| Yes | 175 | 13.9 | 13.2 | 16.9 | ||
| CG Burden | ||||||
| Low | 434 | 34.4 | 38.0 | 25.6 | 36.40(2) | <0.001 |
| Medium | 574 | 45.5 | 47.2 | 47.2 | ||
| High | 254 | 20.1 | 14.8 | 27.2 | ||
| CR Depressed | ||||||
| No | 887 | 70.3 | 71.4 | 64.1 | 7.23(1) | 0.022 |
| Yes | 375 | 29.7 | 28.6 | 35.9 | ||
| CR Anxious | ||||||
| No | 954 | 75.6 | 75.8 | 71.9 | 2.33(1) | 0.192 |
| Yes | 308 | 24.4 | 24.2 | 28.1 | ||
| CR Suffered Adverse Consequence of Unmet | ||||||
| IADL Need | ||||||
| No | 1073 | 85.0 | 86.6 | 81.7 | 5.50(1) | 0.044 |
| Yes | 189 | 15.0 | 13.4 | 18.3 | ||
| CR Suffered Adverse Consequence of Unmet | ||||||
| ADL/Mobility Need | ||||||
| No | 767 | 60.8 | 65.9 | 53.0 | 20.35(1) | <0.001 |
| Yes | 495 | 39.2 | 34.1 | 47.0 | ||
F(1,1206)
Care recipient mortality risk factor covariates.
Care recipient sociodemographic covariates included sex, age, race, and education (see Table 1 for coding). An indicator for whether the care recipient was receiving Medicaid was also included as a proxy for low income. We constructed a composite index of care recipient disability level by classifying older adults as having probable dementia only (14); needing help with two or more self-care (ADL) activities (toileting, eating, bathing, dressing, getting out of bed), but no dementia; having both probable dementia and needing help with two or more self-care tasks; or neither probable dementia nor needing help with two or more ADL. Care recipient depression and anxiety were assessed with the same two-item PHQ measures and cutoffs as described for caregivers.
Statistical analysis
Cox proportional hazards (CPH) models were used to estimate hazard ratios (HR) for all-cause care recipient mortality over approximately five years using baseline care recipient (NHATS) and caregiver (NSOC) variables as predictors. We report HR, 95% confidence interval for HR, Wald statistic, and p-value for each model predictor. The Breslow (15) approximation is used to handle ties in the months to event variable. CPH methods assume that the hazard ratio is constant over time. We conducted both visual [log(-log) plots)] and formal tests using scaled Schoenfeld residuals (16). Age, care recipient anxiety, and caregiver depression showed statistically significant violations in the final model. However, visual plots showed essentially parallel log(-log) plots for care recipient anxiety and caregiver depression. This suggests minor proportionality departures due to sample size and the relatively large number of covariates. Therefore, we retained all covariates due to their hypothesized importance for care recipient mortality. We considered adding time-varying covariates to the model but decided against this since only NHATS care recipients were interviewed yearly. Caregivers were only interviewed at baseline in 2011.
Summary descriptive statistics for the entire sample are presented first, followed by simple bivariate comparisons on all predictors between care recipients who died before wave 5 and those surviving until wave 5 (Table 1). We use χ2 and t-tests for bivariate comparisons. We also report unadjusted hazard ratios for all predictors (Table 2). Three multivariate CPH models were estimated (Table 2). All models included covariates assessing traditional risk factors for mortality in older adults, including a caregiver-care recipient spouse dyad indicator. First, we tested a model containing available known caregiver mortality risk factors (depression, anxiety, burden). Then, we tested a model with mechanisms thought to mediate the relation between caregiver factors and care recipient mortality (CR depression and anxiety, CR unmet needs). Finally, we tested a model entering all variables simultaneously to estimate the best predictors of care recipient mortality and the proposed mediating mechanisms. Cases where the care recipient survived to wave 5 and those who were lost to follow-up for reasons other than death were considered censored for the CPH models. Given that several previous mortality analyses have been conducted in Alzheimer’s / dementia patients, we conducted supplemental CPH analyses (testing the same models) on the subset of cases with probable dementia (n = 458). All analyses use the final NHATS analytic weight (given the focus on care recipient mortality). All analyses were conducted with statistical software (17) using survey sampling weights and procedures that account for the complex sampling strategy. Standard errors were computed using a linearized variance estimator based on a first-order Taylor series linear approximation (17).
TABLE 2.
Cox proportional hazards models testing mortality risk of CR risk factors, CG factors, and CR mechanisms (n = 1,262; weighted)
| Unadjusted | Model 1 | Model 2 | Model 3 | |
|---|---|---|---|---|
| Predictor | HR [CI] Wald; p |
HR [CI] Wald; p |
HR [CI] Wald; p |
HR [CI] Wald; p |
| CR is Female | 0.77 [0.62,0.95] 5.63; 0.018 |
0.65 [0.51,0.83] 12.01; <0.001 |
0.66 [0.51,0.84] 11.25; <0.001 |
0.66 [0.52,0.85] 10.61; 0.001 |
| CR Age | 1.06 [1.05,1.08] 71.86; <0.001 |
1.05 [1.03,1.07] 30.79; <0.001 |
1.06 [1.04,1.08] 38.95; <0.001 |
1.06 [1.04,1.08] 38.03; <0.001 |
| CR Race - Black (non-Hispanic)1 | 0.74 [0.58,0.92] 6.97; 0.008 |
0.79 [0.62,1.01] 3.68; 0.055 |
0.77 [0.60,0.99] 4.26; 0.039 |
0.78 [0.61,1.00] 3.83; 0.051 |
| CR Race – Hispanic1 | 0.67 [0.42,1.08] 2.70; 0.101 |
0.69 [0.43,1.10] 2.46; 0.117 |
0.68 [0.43,1.08] 2.67; 0.102 |
0.68 [0.43,1.08] 2.63; 0.105 |
| CR Education - Some college2 | 0.83 [0.64,1.07] 2.03; 0.154 |
0.98 [0.76,1.28] 0.01; 0.909 |
0.95 [0.73,1.23] 0.16; 0.692 |
0.96 [0.74,1.25] 0.08; 0.781 |
| CR Education - Bachelor’s degree or higher2 |
0.85 [0.63,1.17] 0.98; 0.321 |
0.70 [0.50,0.98] 4.39; 0.036 |
0.70 [0.51,0.97] 4.70; 0.030 |
0.71 [0.51,0.98] 4.27; 0.039 |
| CR on Medicaid | 0.83 [0.63,1.09] 1.90; 0.169 |
0.81 [0.62,1.07] 2.23; 0.136 |
0.76 [0.58,1.02] 3.45; 0.063 |
0.78 [0.59,1.03] 3.09; 0.079 |
| CR Disability - Probable dementia only)3 |
2.17 [1.64,2.88] 29.46; <0.001 |
1.69 [1.27,2.23] 13.25; <0.001 |
1.68 [1.26,2.23] 12.50; <0.001 |
1.65 [1.24,2.20] 11.74; <0.001 |
| CR Disability – 2+ ADLs (only)3 | 1.83 [1.34,2.50] 14.45; <0.001 |
1.73 [1.27,2.35] 12.17; <0.001 |
1.61 [1.18,2.20] 9.05; 0.003 |
1.56 [1.14,2.14] 7.71; 0.006 |
| CR Disability – Both probable dementia & 2+ ADLs3 |
3.67 [2.78,4.84] 84.95; <0.001 |
2.76 [2.07,3.67] 48.35; <0.001 |
2.49 [1.85,3.36] 35.87; <0.001 |
2.37 [1.75,3.20] 31.77; <0.001 |
| CG Relationship -- Spouse | 0.65 [0.51,0.83] 11.71; 0.001 |
0.81 [0.60,1.08] 2.10; 0.147 |
0.84 [0.63,1.12] 1.39; 0.238 |
0.84 [0.63,1.13] 1.34; 0.247 |
| CG Depressed | 1.08 [0.80,1.46] 0.27; 0.604 |
0.89 [0.64,1.23] 0.52; 0.472 |
--- | 0.82 [0.59,1.15] 1.30; 0.254 |
| CG Anxious | 1.20 [0.90,1.60] 1.61; 0.205 |
0.98 [0.72,1.33] 0.02; 0.895 |
--- | 0.98 [0.72,1.34] 0.01; 0.914 |
| CG Burden – Medium Level4 | 1.39 [1.08,1.79] 6.36; 0.012 |
1.20 [0.94,1.54] 2.13; 0.144 |
--- | 1.14 [0.89,1.47] 1.11; 0.292 |
| CG Burden – High Level4 | 2.12 [1.59,2.82] 26.71; <0.001 |
1.51 [1.13,2.02] 7.79; 0.005 |
--- | 1.39 [1.03,1.88] 4.72; 0.030 |
| CR Depressed | 1.37 [1.10,1.72] 7.73; 0.006 |
--- | 1.34 [1.05,1.71] 5.63; 0.018 |
1.34 [1.05,1.72] 5.46; 0.020 |
| CR Anxious | 1.18 [0.93,1.51] 1.85; 0.175 |
--- | 1.03 [0.79,1.33] 0.04; 0.834 |
1.03 [0.79,1.34] 0.05; 0.825 |
| CR Suffered Adverse Consequence of Unmet IADL Need |
1.21 [0.91,1.60] 1.72; 0.191 |
--- | 1.21 [0.91,1.61] 1.79; 0.181 |
1.18 [0.88,1.57] 1.21; 0.271 |
| CR Suffered Adverse Consequence of Unmet ADL Need |
1.59 [1.29,1.98] 18.11; <0.001 |
--- | 1.29 [1.03,1.62] 4.76; 0.029 |
1.27 [1.01,1.60] 4.27; 0.039 |
HR = hazard ratio; CI = 95% Confidence interval for HR
Wald Statistic Degrees of freedom = (1, 1206) for all cells.
Reference groups:
non-Hispanic White
high school or less
Neither probable dementia nor 2+ ADLs
Low CG burden
Results
Descriptive statistics
Summary descriptive statistics for the entire sample (n = 1,262) are reported in Table 1. By the wave 5 assessment, 500 (39.6%) care recipients had died (mean time to death = 23.3 months; mdn = 22.0 months); 499 (39.5%) continued to be enrolled in the study; and 263 (20.9%) were lost to follow-up for reasons other than death. The care recipients were predominantly female (68.6%) with a mean age of 81.6 years at baseline (sd = 8.3), and were predominantly white non-Hispanic (62.6%), with 28.2% African American, and 7% Hispanic. Nearly two-thirds reported a high school education or less, with 13% earning a bachelor’s degree or higher. A little less than one-fourth (23.9%) of the care recipients were enrolled in Medicaid. The disability level grouping showed that while almost half the sample had neither probable dementia nor needed help with multiple ADL tasks (48.8%), 18.9% had probable dementia, 14.9% needed help with multiple ADLs, and 17.4% had both probable dementia and multiple ADL needs. Most caregivers were also female (67.2%); the majority (55.0%) were adult children taking care of a parent; and 26.9% were taking care of a spouse. Looking at other caregiving factors, 14.1% of the caregivers met the PHQ cutoff for risk for depression, while 13.9% met the PHQ anxiety cutoff score. Approximately one in five caregivers scored high on the caregiver burden index, while a little more than one-third scored zero. In terms of possible mediating mechanisms, 29.7% of care recipients met depression risk criteria, and 24.4% met anxiety risk criteria. While only 15% of care recipients reported adverse consequences of unmet IADL needs, 39.2% said they had experienced such negative consequences from unmet ADL or mobility needs.
Bivariate tests
Bivariate baseline comparisons between sub-samples among whom the care recipients died (versus not) before wave 5 are also shown in Table 1. Looking at care recipient sociodemographic and health covariates, males, older, non-Hispanic white, and care recipients with higher disability levels (especially those with both probable dementia and multiple ADL needs) had higher mortality rates. Female caregivers and those who were daughters had recipients with higher mortality rates. While there were no mortality differences for caregiver depression and anxiety, higher caregiver burden was significantly related to subsequent care recipient mortality. Among those who died, about a quarter (27.2%) had “high burden” caregivers, versus 14.8% for those who did not die. Care recipients at risk for depression, and those reporting adverse consequences of unmet IADL and ADL / mobility needs, had higher subsequent mortality, though the ADL / mobility effect was stronger than IADL.
Multivariate Cox proportional hazards models
The unadjusted Cox proportional hazards ratio results reported in column 1 of Table 2 are quite similar to the bivariate results just described from Table 1. Note that the only exception is that the effect for adverse consequences of unmet needs for IADL is not significant (though the ADL / mobility effect remains).
The multivariate CPH models are reported in columns 2, 3, and 4 of Table 2. Model 1 (column 2) replicates previous mortality analyses for known risk factors. Being male, older, having probable dementia, needing help with two or more self-care ADLs, and the combination of needing help and having probable dementia, were risk factors for higher mortality. Also, those with a bachelor’s degree or higher had lower mortality hazard ratios. Looking at caregiving factors, those reporting high levels of caregiver burden had care recipients with higher mortality hazard ratios. Caregiver depression and anxiety were not related to recipient mortality. Model 2 (column 3) shows partial support for the proposed care recipient mechanisms. Care recipients at risk for depression and those reporting unmet ADL / mobility needs were at higher risk for mortality. Neither care recipient anxiety nor unmet IADL needs were related to mortality. Model 3 (column 4) included all variables simultaneously and shows that care recipient depression and unmet ADL / mobility needs effects remain significant. The effect of high caregiver burden on care recipient mortality, while still significant, is slightly attenuated.
Supplemental CPH models for the dementia sub-sample
Given prior analyses of dementia patient mortality, we ran the same three CPH models on the sub-sample of cases where the care recipient had probable dementia at baseline (n = 458). Results of the final model were similar to those for the full sample with one exception. Adverse consequences of unmet needs (neither ADL / mobility nor IADL) were not related to mortality among dementia care recipients.
Discussion
Mortality of older adult CRs is driven primarily by demographic and health related variables. Being male, older, having less education, being disabled, cognitively impaired, and depressed are all risk factors for increased mortality. These findings are consistent with the existing literature on predictors of mortality in older adults. In support of our model, both CR depression and unmet needs were associated with increased mortality. We also hypothesized that the effects of CG mental health and burden would be mediated through CR mental health and behaviors reflecting inadequate or poor quality care resulting in more unmet needs of the care recipient. These predictions were not supported. Instead, caregiver mental health had no impact on mortality, and burden had a direct effect on mortality. Of course, this does not rule out the possibility that emotional status and burden might contribute to other behavioral mediators, such as poor medication regimen, missed doctor appointments, or failure to detect significant care recipient declines. Caregiver burden and unmet care recipient needs may both be indicators of a “poor quality care” syndrome, additional aspects of which were not measured in this study. Caregiver depression has also been associated with potentially harmful caregiver behaviors (verbal abuse, threatening with physical force, threatening to institutionalize or abandon), which in turn may affect CR mental health and mortality (18). Our failure to find CG mental health effects on mortality was not consistent with the study by Lwi and colleagues (8) and may be due to unique sample of CRs with neurodegenerative disease included in their study.
A replication of these analyses with the subsample of care recipients with probable dementia yielded a similar pattern of results, although unmet needs did not predict mortality. This is consistent with research showing that unmet needs have low prevalence in persons with dementia unless they also have ADL or mobility limitations (19). The criteria used to classify individuals with “probable dementia” in NHATS includes individuals with moderate cognitive impairment who do not yet have ADL limitations.
The clinical implications of these findings are twofold. First, interventions that reduce caregiver burden and address CR unmet needs may also impact CR mortality. We know of three studies (9, 20, 21) that show that multi-component interventions reduced mortality among community residing CRs, although these effects are relatively small. Comprehensive multi-component approaches to treatment may impact survival time because they reduce burden and improve the quality of care provided to the CR. Second, interventions that address CR depression may enhance both the quality and duration of life. Depression is a known risk factor for mortality in older adults (22, 23) and is likely due to complex feedback loops involving functional disability, health behaviors (23) and motivational depletion (22).
Limitations
This paper has a number of limitations. Although our sample is relatively large and generally representative of white CRs over the age of 65, minority populations such as Hispanics are underrepresented. Caregiver data are based on a one-time baseline assessment and do not include possible changes in caregiver status that might have occurred between baseline assessment and CR death. Data limitations also prevented us from assessing more complex predictive mortality models. Clearly, we are in the early stages of understanding how caregiving context, processes, and individual differences might affect care recipient outcomes such as mortality. Future research should expand the range of variables examined with a greater emphasis on macro- and micro-level behavioral interactions between CG and CR. How and to what extent do caregivers regulate CR health behaviors and encounters with the health care system? What factors contribute to exemplary as opposed to inadequate or harmful care provided to the CR? What role does the emotional bond play between CG and CR in care processes and health outcomes for both members of the dyad? Answers to these questions will shape our understanding of CR health, functioning, and survival.
Highlights.
-
What is the primary question addressed by the study?
Controlling for known risk factors for mortality in older adults with disability, does caregiver mental health and burden affect survival time of the care recipient?
-
What is main finding of study?
We assess the impact on care recipient mortality of three caregiving factors (caregiver depression, anxiety, and burden) and three possible mediators (care recipient depression, anxiety, and poor quality/inadequate care). Caregiver burden, care recipient depression, and inadequate care are independent predictors of care recipient mortality.
-
What is meaning of finding?
Caregiver status and behaviors impact the survival time of their care recipients.
Acknowledgments
Funding
Preparation of this manuscript was in part supported by grants from the National Institute on Disability, Independent Living, and Rehabilitation Research (90RTGE002); the National Institute on Aging (R01AG054009); the National Institute of Nursing Research (R01NR014434); and the National Institutes on Aging (R01AG055511).
Footnotes
Disclosure / Conflict of Interest
The authors report no conflicts with any product mentioned or concept discussed in this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Richard Schulz, University of Pittsburgh, PA.
Scott R. Beach, University of Pittsburgh, PA.
Esther M. Friedman, RAND Corporation, Santa Monica, CA.
References
- 1.Schulz R, Eden J (eds): Families Caring for an Aging America. Washington, DC, The National Academies Press, 2016. doi: 10.17226/23606. [DOI] [PubMed] [Google Scholar]
- 2.Schulz R, Beach SR, Czaja SJ, et al. : Family caregiving for older adults. Annu Rev Psychol 2020; 71:635–659. doi: 10.1146/annurev-psych-010419-050754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vernon E, Cooley B, Rozum W, et al. : Caregiver-care recipient relationships are associated with neuropsychiatric symptoms in dementia. Innov Aging 2017; 1:572. 10.1093/geroni/igx004.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ejem D, Bauldry S, Bakita M, et al. : Caregiver burden, care recipient depressive symptomology, and social exchange: Does race matter? J Palliat Care 2018; 33:100–108. 10.1177/0825859718758120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Betini RSD, Hirdes JP, Lero DS, et al. : A longitudinal study looking at and beyond care recipient health as a predictor of long-term care home admission. BMC Health Serv Res 2017; 17:709. 10.1186/s12913-017-2671-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ankuda CK, Maust DT, Kabeto MU, et al. : Association between spousal caregiver well-being and care recipient healthcare expenditures. J Am Geriatr Soc 2017; 65:2220–2226. doi: 10.1111/jgs.15039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carey EC, Covinksy KE, Lui LY, et al. : Prediction of mortality in community-living frail elderly people with long-term care needs. J Am Geriatr Soc 2008; 56:68–75. doi: 10.1111/j.1532-5415.2007.01496.x. [DOI] [PubMed] [Google Scholar]
- 8.Lwi SJ, Ford BQ, Casey JJ, et al. : Caregiver mental health predicts patient mortality. Proceedings of the National Academy of Sciences July 2017; 114:7319–7324. doi: 10.1073/pnas.1701597114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brodaty H, McGilchrist C, Harris L, et al. : Time until institutionalization and death in patients with dementia: Role of caregiver training and risk factors. Arch Neurol 1993; 50:643–650. doi: 10.1001/archneur.1993.00540060073021. [DOI] [PubMed] [Google Scholar]
- 10.Boele FW, Given CW, Given BA, et al. : Family caregivers’ level of mastery predicts survival of glioblastoma patients: A preliminary report. Cancer 2017; 123:832–840. doi: 10.1002/cncr.30428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pristavec T, Luth E: The effect of caregiving experience on care recipient older adults’ mortality: A survival analysis. Innov Aging 2019; 3:S217. 10.1093/geroni/igz038.796. [DOI] [Google Scholar]
- 12.Monin JK, Schulz R: Interpersonal effects of suffering in older adult caregiving relationships. Psychol Aging 2009; 24:681–695. doi: 10.1037/a0016355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wolff A, Gooch D, Cavero Montaner JJ et al. : Creating an understanding of data literacy for a data-driven society. Journal of Community Informatics 2016; 12:9–26. [Google Scholar]
- 14.Kasper JD, Freedman VA, Spillman B: Classification of persons by dementia status in the National Health and Aging Trends Study. Technical Paper #5. Baltimore, MD: Johns Hopkins University School of Public Health, 2013; Available at www.NHATS.org [Google Scholar]
- 15.Breslow N: Covariance analysis of censored survival data. Biometrics 1974; 30:89–99. 10.2307/2529620. [DOI] [PubMed] [Google Scholar]
- 16.Grambsch PM, Therneau TM: Proportional hazards tests and diagnostics based on weighted residuals, Biometrika 1994; 81:515–526. 10.1093/biomet/81.3.515, [DOI] [Google Scholar]
- 17.StataCorp: Stata Statistical Software: Release 14. College Station, TX: StataCorp LP, 2015. [Google Scholar]
- 18.Beach SR, Schulz R, Williamson GM: Risk factors for potentially harmful caregiver behavior. J Am Geriatr Soc 2005; 53:255–261. doi: 10.1111/j.1532-5415.2005.53111.x. [DOI] [PubMed] [Google Scholar]
- 19.Beach SR, Schulz R: Family caregiver factors associated with unmet needs for care of older adults. J Am Geriatr Soc 2017; 65:560–566. doi: 10.1111/jgs.14547. [DOI] [PubMed] [Google Scholar]
- 20.Schulz R, Zdaniuk B, Belle SH, et al. : Baseline differences and trajectories of change for deceased, placed, and community residing Alzheimer’s disease patients. Alzheimer Dis Assoc Disord 2010; 24:143–150. doi: 10.1097/WAD.0b013e3181b795b7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gitlin L, Hauck W, Winter L, et al. : Effect of an in-home occupational and physical therapy intervention on reducing mortality in functionally vulnerable elders: Preliminary findings. J Am Geriatr Soc 2006; 54:950–955. doi: 10.1111/j.1532-5415.2006.00733.x. [DOI] [PubMed] [Google Scholar]
- 22.Schulz R, Beach SR, Ives DG, et al. : Association between depression and mortality in older adults: The Cardiovascular Health Study. Arch Intern Med 2000; 160:1761–1768. doi: 10.1001/archinte.160.12.1761. [DOI] [PubMed] [Google Scholar]
- 23.Blazer DG, Hybels CF, Pieper CF: The association of depression and mortality in elderly persons: A case for multiple, independent pathways. J Gerontol A Biol Sci Med Sci 2001; 56:M505–M509. 10.1093/gerona/56.8.M505. [DOI] [PubMed] [Google Scholar]


