Abstract
Background
To investigate in vivo kinematics of total knee arthroplasty (TKA) with the introduction of a mildly constrained (MC) type of polyethylene (PE). We compared the knee kinematics with a reported pattern after surgery using the same component with a conventionally constrained (CC) type of PE.
Methods
Finite element analysis (FEA) was performed to examine different peak stress distribution of both types of PE. For in vivo study, patients who underwent cruciate-retaining TKA using a total knee system with MC-PE were included. Fluoroscopic surveillance was used to measure the weight-bearing deep knee bend (squatting) using a two-dimensional/three-dimensional (2-D/3-D) registration technique.
Results
FEA analysis revealed the edge loading of the femoral component on PE in CC but not in MC. During the study period, 42 patients underwent TKA with MC-PE. Among them, 13 agreed to participate in the present study. In vivo kinematics analysis found that starting from an average external rotation of femur being 7.1° at 0° of flexion, the rotation slightly decreased to 6.8° at 10° of flexion, then increased with increasing knee flexion until it reached 10.8° at 80° of flexion, and finally decreased to 9.8° at 100° of knee flexion. The results indicate a modest medial pivot pattern. Although the overall pattern was similar for both MC-PE and CC-PE, a slight difference was observed. MC-PE showed a slight internal rotation of 0.3° from 0 to 10° of knee flexion, whereas CC-PE showed a gradual increase of external rotation in this range.
Conclusions
Change of configuration from CC to MC did not substantially affect in vivo kinematics of knees after TKA. Considering the theoretical wider range of allowance of rotation, MC-PE is easier for knee surgeons to use.
Keywords: Configuration, Finite element analysis, Fluoroscopy, Kinematics, Total knee arthroplasty, Two-dimensional/three-dimensional registration
Introduction
Growing number of total knee arthroplasties (TKA) were performed worldwide. This appears to be the result of increasing demand from the aging society. To improve clinical results after TKA, many problems have to be solved. Better range of motion (ROM), better durability, fewer complications, and better patient satisfaction have been sought, and continuous efforts have been made. In 2001, a new total knee system entered clinical use of which essential design concepts were to introduce medial pivot motion mainly by the geometry of components and polyethylene (PE). Femoral and tibial components incorporated geometric features of Japanese knees and high constraint in the medial compartment and low constraint in the lateral compartment due mainly to surface morphology of the PE insert. In addition, 3° of built-in varus slant in the PE surface that mimicked the physiological feature of a tibial plateau contributed to guide the medial pivot pattern. More than 20,000 surgeries have been performed using the system, and good middle-to-long-term clinical results have been reported.1 two-dimensional/three-dimensional (2-D/3-D) registration analysis of operated knees in vivo proved to reproduce the medial pivot pattern during squatting.2, 3, 4
One concern of the system is a small permissible zone in terms of rotational component placement to deliver ideal medial pivot motion. Finite element analysis (FEA) revealed the theoretical allowance of external rotation was 0° when the knee was loaded in full extension (data not shown).
Studies examining the rotational alignment of components found a wide range of rotation.5, 6, 7 In their case series, Nicoll et al. reported 17 tibial components of 65 were internally rotated more than 9°, and 6 were externally rotated more than 10°.5 Mitsuhashi et al. reported that even with the use of navigation, rotation of the tibial component ranged from −11.9° to 7.8°.6 Smaller variation of the rotation of the femoral component compared with the tibia was reported by Benazzo et al. who found external rotation of the femoral component ranged from −6° to 6.7 These studies led us to deduce a propensity for the malalignment of each component and the rotational mismatch of both components. PE with higher constraint would work to guide the medial pivot pattern when each component is placed in a certain range, otherwise, mechanical conflict might occur. Knees did not show a single kinematic pattern, but different kinematics depending on different activities.8,9
To lessen the concern mentioned above, a type of PE with milder constraint, hereafter referred to as “mildly constrained polyethylene (MC-PE)”, was introduced in the system in 2016. The purpose of the present study was to investigate in vivo kinematics of TKA with MC-PE by employing 2-D/3-D analysis and comparing the knee kinematics with the reported pattern using a conventionally constrained (CC) type of PE (CC-PE).
We hypothesized that no difference would be observed between the two as long as minimally required constraint existed.
Materials and methods
A prospective in vivo knee kinematic analysis was performed at a single center. The study protocol was approved by the institutional review board and written informed consent was obtained from each patient.
Finite element analysis of polyethylene
Finite element analysis (FEA; MSC. Marc; MSC Software Corp., Santa Ana, CA, USA) was used to evaluate peak contact stresses of PE surfaces in the femoral-tibial joint. The analysis did not include a bony element considering computation time. As the material constants for the Co-Cr-Mo alloy, Young’s modulus was set to 213 GPa and the Poisson ratio to 0.3. For the ultra-high molecular weight polyethylene (UHMWPE) insert, Young’s modulus was set to 1 GPa and the Poisson ratio to 0.3. The yield stresses were 450 MPa for the Co-Cr-Mo alloy and 20 MPa for UHMWPE. A standing position with an initial load of 3.5 times body weight (3.5BW: 2000 N) was vertically applied at 0° of knee flexion, and the virtual components were allowed to settle into their preferred alignments in two conditions, namely, 0° and 5° of tibial external rotation. Size M of the femoral component and the same size of the tibial component were selected for the analysis. The dimensions of the femoral component were 64.0 mm mediolaterally (ML) and 57.5 mm in anteroposteriorly (AP). In the sagittal plane, the medial femoral condyle was designed using a combination of two circles with a curvature radius of 35 mm (R35) distally and 19 mm posteriorly, and those laterally were R33 and R17. The dimensions of the tibial component were 66.0 mm ML and 44.0 mm AP. The configuration of the PE is shown in Fig. 1, and the conformity-related values are presented in Table 1, which showed milder constraint in MC-PE than CC-PE. Coordinate axes of the femoral component were defined as follows: a line connecting the center of two circles configuring the distal femoral component (R35 and R33) was defined as tentative x-axis, a sagittal line through the midpoint of ML of the distal femoral component and parallel to the upper surface of the distal femoral component was designated as contact with the distal bony surface of the femur and defined as y-axis, and a line vertical to the upper surface of the distal femoral component intersecting with the tentative x and y axes was defined as the z-axis. Finally, the tentative x-axis was translated parallel until it met with the cross point of y and z-axes to make a point of origin, and the true x-axis was defined. Coordinate axes of the tibial component were defined as follows: a tangent line to both the medial and lateral posterior surface was defined as the x-axis, a vertical line to the x-axis and through the midpoint of the component in terms of medial-to-lateral width was defined as the y-axis. When the y-axes of the femur and the tibia became concordant, the rotation was defined as 0° and rotation of the z-axis was described as external.
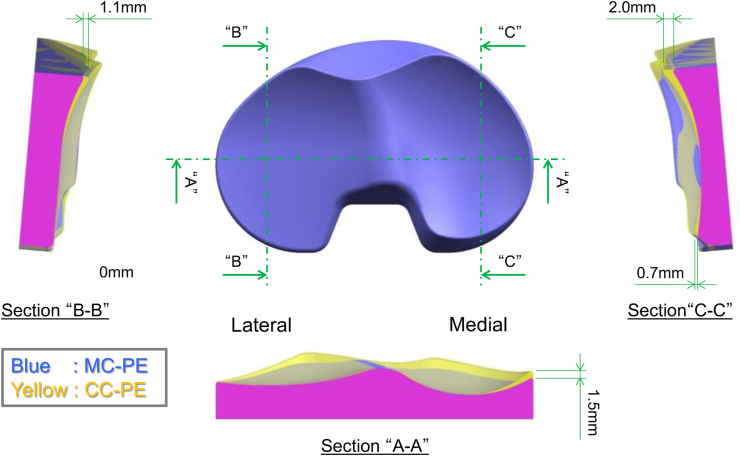
Fig. 1.
Configurations of conventional polyethylene (CC-PE) and mildly constrained PE (MC-PE).
Yellow indicates C C-PE, blue indicates MC-PE. When the two PE types are merged, the overlapping portion is indicated in pink. A-A section has a higher lip for CC-PE (1.5mm medially). B-B and C-C sections also have a higher lip for CC-PE (2.0mm antero-medially, 0.7mm antero-posteriolly, and 1.1mm antero-laterally). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Table 1.
Conformity of conventional polyethylene (PE) and mildly constrained PE.
| CC-PE | MC-PE | ||
|---|---|---|---|
| Coronal | Medial | 0.97 | 0.79 |
| Lateral | 0.97 | 0.94 | |
| Sagittal | Medial (anterior) | 0.97 | 0.94 |
| Lateral (anterior) | 0.97 | 0.94 | |
| Medial (posterior) | 0.77 | 0.43 | |
| Lateral (posterior) | ∞ | ∞ |
Conformity = (radius of the femoral component)/(radius of the polyethylene). ∞Due to the flat nature of the lateral posterior portion, the value was infinite.
In vivo kinematics of knees after TKA with MC polyethylene
Participants
Included were patients who underwent (1) CR TKA using the FINE total knee system (Teijin-Nakashima, Okayama, Japan) with MC-PE between June 2016 and April 2018, (2) follow up of more than 6 months, and (3) had a passive flexion angle of more than 110°. Patients who suffered from an infection after the surgery were excluded.
Age, sex, BMI, operative side, diagnosis (OA or ON), preoperative Kellgren-Lawrence (KL) grade, and preoperative femorotibial angle (FTA) were extracted from patient records.
Surgeries had been performed employing a precut technique, where a slight amount of posterior femur was cut after having acquired a planned amount of extension gap. Then a tentative partial femoral component was inserted along with a tentative tibial component and a trial PE that mimicked the status of completion with both components in place with the remaining posterior condylar bone. Then, the thickness of the PE was changed to determine the ligament balance of the knee in extension and flexion to assess the final amount of bone to be removed.10 The surgical epicondylar axis and the Akagi’s line were used to determine rotational alignment of femoral and tibial component.11
Component alignment
Component alignments were checked using x-ray as shown in Fig. 2. Specifically, the femoral component valgus angle (α) was defined as the angle between the femoral axis and the line connecting the farthest medial point of the component with the farthest lateral point, and the tibial component valgus angle (β) as the angle between the tibial axis and the plateau of the tibial component (Fig. 2-A). The femoral component flexion angle (γ) was defined as the angle between the femoral axis and the femoral component peg, and the tibial component posterior slope angle (δ) as the angle between the tibial axis and the plateau of the tibial component (Fig. 2-B).
Fig. 2.
Component alignment.
The dotted lines show bone axes and the solid reference lines of the components. α, the femoral component valgus angle; β, the tibial component valgus angle; γ, the femoral component flexion angle; δ, the tibial component posterior slope angle.
2-D/3-D analysis
Fluoroscopic surveillance was used to measure weight-bearing deep knee bending (squatting). In detail, each patient was instructed to squat, that is, a motion from extension to maximum flexion. The sequential motion was recorded as digital x-ray images (1024 × 1024 × 12 bits/pixel, 7.5 Hz serial spot images), using a Digital Imaging and Communications in Medicine file with a 17-inch flat-panel detector system (DREX-ZX80: Canon Medical Systems, Tokyo, Japan). To estimate the spatial position and orientation of each component, a 2-D/3-D registration technique was used.12,13 This technique was developed from a contour-based registration algorithm using single fluoroscopic images and 3-D computer-aided design (CAD) models. The estimated accuracy of the relative motion between metal components was about 0.5° in rotation and 0.4 mm in translation except for out-of-plane translation.13 In the femoral coordinate system, the origin was defined as the center of gravity for the component. In the tibial coordinate system, the origin was defined as the center of the tibial tray surface. We evaluated the flexion angles between the femoral and tibial components, femoral external rotation (ER) angles relative to the tibial component, and anteroposterior (AP) translation of medial (MAP) and lateral (LAP) sides. The flexion and ER angles were described using the Grood and Suntay joint rotation convention.14 AP translation was defined as the nearest point from the femoral component to the tibial axial plane on both the medial and lateral sides. Each contact point was expressed as mean ± standard deviation (SD).
Results
Finite element analysis of polyethylene
FEA showed a peak von Mises stress in 0° of tibial external rotation in knee extension of 19.7 MPa at the PE insert in the medial plateau and 12.5 MPa in the lateral plateau of CC-PE (Fig. 3-A), whereas the stresses were 14.1 and 15.8 MPa in MC-PE (Fig. 3-B). By contrast, the von Mises stress in 5° tibial external rotation was 21.1 MPa at the UHMWPE insert in the lateral plateau and 14.6 MPa in the medial plateau in CC-PE (Fig. 3-C), whereas the stresses in MC-PE were 12.1 and 22.5 MPa (Fig. 3-D). Locations of maximum stress for CC-PE were close to the edge of the PE.
Fig. 3.
Stress distribution on PE derived from finite element analysis in knee extension.
The highest stress was observed in the medial compartment of MC-PE in 5°of external position, but the concern of edge loading in CC-PE in 5°of external position is shown. (Scale: yellow indicates higher stress and blue lower). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
In vivo kinematics of knees after TKA with MC polyethylene
Participants
A total of 42 patients underwent TKA with MC-PE, and 34 met inclusion criteria. Among them, 13 patients agreed to participate in the study. Their general clinical background is presented in Table 2. At the time of the investigation, the passive ROM of the knee joint of included patients was from an extension of −0.4 ± 1.7° (mean ± SD) to flexion of 118.1 ± 6.6°. The active ROM of the knee joint at fluoroscopic surveillance in squatting was from an extension of −1.8 ± 7.5° to flexion of 100.4 ± 9.0°.
Table 2.
Patient demographics.
| Parameters | Average | SD |
|---|---|---|
| Age (years) | 68.7 | 6.4 |
| BMI (kg/m2) | 25.1 | 4.1 |
| Sex (male:female) | 5:7 | |
| Side (right:left) | 6:6 | |
| Preoperative FTA (°) | 186.6 | 5.9 |
| Follow up (months) | 13.3 | 6.6 |
BMI, body mass index; FTA, femorotibial angle; SD, standard deviation.
Component alignment
Coronal and sagittal component alignment was checked with x-ray images as shown in Table 3. Obtained data were within the range of previous reports. The standard deviation in sagittal alignments appeared as higher, but also comparable to previous reports.15,16
Table 3.
Component alignment.
| Parameter | Mean | SD |
|---|---|---|
| α (°) | 97.6 | 2.6 |
| β (°) | 89.6 | 1.8 |
| γ (°) | 4.9 | 2.9 |
| δ (°) | 84.8 | 4.2 |
SD, standard deviation.
In vivo kinematics of knees after TKA with MC polyethylene
The average AP position of the medial contact points was −4.3 mm at 0° of knee flexion and remained around the same position until 40° of flexion, and then a gradual increase was observed until reaching −2.4 mm at 90° of flexion, then a decrease to −3.2 mm at 100° of flexion. The transition of the lateral was −9.5 mm at 0°, slightly increased to −9.1 mm at 10°, then stayed at around the same position until it reached 80° of flexion, then a slight increase to −10.4 mm at 90° of flexion (Fig. 4-A). Patterns of AP transition due to knee flexion for each case were also presented (Fig. 4-B, C), and no significant deviations were observed at any flexion angle.
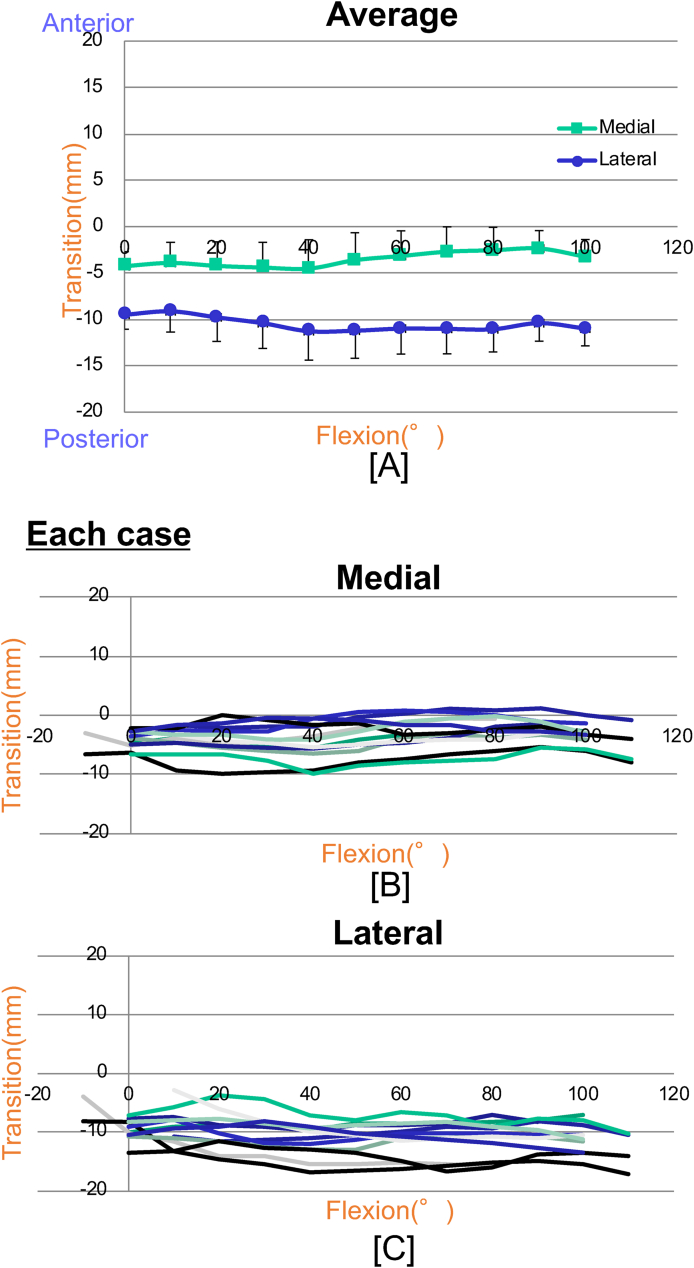
Fig. 4.
Kinematics with MC-PE knees while squatting (anteroposterior transition).
The average contact point of both lateral and medial femoral condyle on PE is plotted with standard deviation (A). The pattern for each case is presented as a different color (B: for medial, C: for lateral) where no obvious outlier was found. . (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
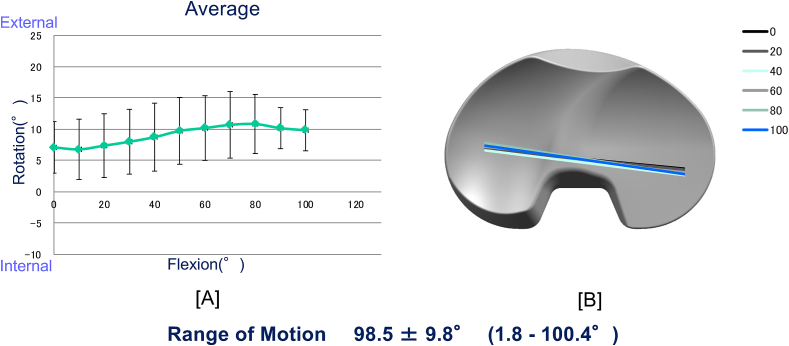
The average external rotation of 7.1° at 0° of flexion slightly decreased to 6.8° at 10° of flexion, then increased as knee flexion increased until it reached 10.8° at 80° of flexion, then finally decreased to 9.8° at 100° of knee flexion (Fig. 5-A). The results are also expressed as colored lines, which indicated a modest medial pivot pattern (Fig. 5-B).
Fig. 5.
Kinematics with MC-PE knees while squatting (rotation).
Average rotation of the femoral component on PE is plotted and standard deviations of each value are indicated by black lines (A). Rotational movement on PE is plotted at every 20° from 0 to 100° using different colored lines (B).
Discussion
In the present study, FEA analysis of peak stress distribution on PE and in vivo kinematics of CR TKA with a modification of PE configuration are presented. We found that the newly introduced MC-PE that was designed as less constraining of the components showed almost identical kinematics to that of knees after surgery with an original CC-PE,3 where both PE types resulted in a mild medial pivot pattern as much as 3° of external rotation from extension to flexion of the knee. Although the present study had only a single arm, a strength was the employment of the same methodology to compare the kinematics of the knees with the same design of femoral and tibial components with the modification of only PE configuration. To our knowledge, the present study is the first study in vivo in this regard.
Although the overall pattern was similar for both PEs, a slight difference was observed. MC-PE showed a slight internal rotation of 0.3° from 0 to 10° of knee flexion, whereas CC-PE showed a gradual increase of external rotation in this range. In addition, maximum external rotation was observed at 80° of flexion in MC-PE, but 100° in CC-PE. These two differences might be attributable to the difference in constraints, but because of the relatively large deviation of values that are reported for this type of study we could not determine the true cause. Thus, we considered that there was no big difference between the two PEs in the overall pattern.
The PE configuration has a large impact on kinematics patterns of the knees. In their 2-D/3-D analysis, Tamai et al. found 2 different patterns with the use of totally flat PE. Eight of 16 knees exhibited a medial pivot pattern, and 8 knees a lateral pivot pattern.17 The design of femoral and tibial components might affect kinematics, but as long as PE was totally flat, speculating that ligament balance would be the primal determinant of kinematics would be reasonable. In other words, nearly half of the cases might have a conflict between naïve knee kinematics and PE guided kinematics. Shu et al. reported the effect of sagittal conformity on knee kinematics in their computer simulation in vitro validation study. They showed different kinematics among 3 models (high constraint both in medial and lateral compartments (CPCR), low constraint in both compartments (UPCR), and high constraint in medial and low in lateral compartments (MPKP: medial pivot knee prosthesis) during various activities including squatting. In the flexion phase, CPCR showed a mild medial pivot with maximum external rotation of 3.8°, UPCR combined roll-back and external rotation, and MPKP a clear medial pivot pattern of 11.3°. They showed a degree of conformity with a radial quotient between the femoral component and PE. Conformity of 0.99 was used as representative of high conformity and 0.30 low conformity. Compared with the conformity of MC-PE in the present study where medial was 0.94 and lateral was 0.43, MC-PE might be around midway between CPCR and MPKP, and the resultant pattern between CPCR and MPKP was also similar.18
Not only conformity, but also other factors affect kinematics of the knee, including coronal and sagittal alignment of the components. Fujito et al. reported no significant difference in the posterior slope of the tibial component between knees that had more than 8° of posterior slope tibial component (average of 9.8°) and those with less than 7° (average of 5.6°) in deep knee bending under weight-bearing conditions using the same TKA system with CC-PE.3 By contrast, Fujimoto et al. reported a posterior slope of the tibia affected knee kinematics through gravity, where knees with large posterior slope showed posterior displacement of the medial femoral condyle.19 The extent of the posterior slope was not significantly different between the two reports; thus, the different results might be attributable to different TKA systems. Koh et al. examined the effect of coronal alignment on kinematics and found restoration of naïve knee kinematics was achieved using a kinematically aligned surgical technique, but not with mechanically aligned surgery using cadaveric knees.20
Kinematics of knees after TKA are multifactorial, and other factors such as surgical technique, patella replacement, and inherent geometry of the patient’s knee were efficient and larger than factors mentioned above.
One of characteristic of the present study was presenting the dimensions of the two PEs. Most of the TKA systems were categorized as a cruciate substitute (CS), medial pivot type by the expected motion pattern due to the degree of constraint. However, most did not open the degree of conformity with substantial evidence, which has not yet been generalized and has no available legitimate definition. We consider that expressing conformity in actual values will allow further understanding of TKA kinematics.
Although FEA analysis elucidated possible edge loading in CC-PE, good middle to long term clinical results have been reported using the TKA system with CC-PE.1 FEA settings might not reflect the actual status of TKA joint or infrequent occurrence of edge loading might not affect the clinical results. Thus we cannot recommend which type of PE should be chosen simply from the result of the present study.
Several limitations of the present study should be highlighted. First, the number of cases was small, although comparable to those used in most of the previous studies.3,9,17,21, 22, 23 Because we started to use MC-PE 2 years ago and deliberately used MC-PE by observing the basic clinical course, especially in the first year, the number of cases was not many as found currently. Second, kinematics while squatting alone under weight-bearing conditions was examined to compare our findings with those of previous reports. In other types of activities, there might be a difference. Third, we used CR TKA, and this was not the case with PS TKA, incorporating different status of individual posterior cruciate ligament as another factor. Fourth, only 100° of knee flexion was presented due to the ability of participants; most had a larger knee flexion (average of 118.1 ± 6.6° in nonwearing condition), but the patients dared not perform what they had not done in daily activities. Fifth, five surgeons performed surgeries in this series, including inexperienced surgeons supervised by a senior surgeon.
In conclusion, despite the change in PE configuration, in vivo kinematics of knees after CR TKA was not affected. Knee surgeons can select either type of PE depending on their preference.
Declaration of competing interest
The authors have no conflicts of interest relevant to this article.
Acknowledgements
The authors thank Yuya Ogawa, Aya Sadamasu, Ono Yoshimasa, Hiroaki Hosokawa, Manato Horii, Masashi Shinohara, and Satoshi Yamaguchi for their cooperation with this research and their constructive comments.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.asmart.2020.11.002.
Funding/support statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors, and no material support of any kind was received.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Nakamura J., Inoue T., Suguro T. A comparative study of flat surface design and medial pivot design in posterior cruciate-retaining total knee arthroplasty: a matched pair cohort study of two years. BMC Muscoskel Disord. 2018;19:1–7. doi: 10.1186/s12891-018-2138-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miyazaki Y., Nakamura T., Kogame K., Saito M., Yamamoto K., Suguro T. Analysis of the kinematics of total knee prostheses with a medial pivot design. J Arthroplasty. 2011;26:1038–1044. doi: 10.1016/j.arth.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Fujito T., Tomita T., Yamazaki T., Oda K., Yoshikawa H., Sugamoto K. Influence of posterior tibial slope on kinematics after cruciate-retaining total knee arthroplasty. J Arthroplasty. 2018;33:3778–3782. doi: 10.1016/j.arth.2018.07.029. e1. [DOI] [PubMed] [Google Scholar]
- 4.Tomita T., Futai K., Yamazaki T., Kunugiza Y., Yoshikawa H., Sugamoto K. In vivo kinematics after FINE TKA with deep knee bending motion and stair activities. Bone Jt Nerve. 2015;5:27–33. ([In Japanese]) [Google Scholar]
- 5.Nicoll D., Rowley D.I. Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Jt Surg - Ser B. 2010;92:1238–1244. doi: 10.1302/0301-620X.92B9.23516. [DOI] [PubMed] [Google Scholar]
- 6.Mitsuhashi S., Akamatsu Y., Kobayashi H., Kusayama Y., Kumagai K., Saito T. Combined CT-based and image-free navigation systems in TKA reduces postoperative outliers of rotational alignment of the tibial component. Arch Orthop Trauma Surg. 2018;138:259–266. doi: 10.1007/s00402-017-2837-1. [DOI] [PubMed] [Google Scholar]
- 7.Benazzo F., Rossi S.M.P., Danesino G., Klersy C., Perelli S., Ghiara M. Computed tomography evaluation of total knee arthroplasty implants position after two different surgical methods of implantation. Int Orthop. 2019;43:139–149. doi: 10.1007/s00264-018-4180-8. [DOI] [PubMed] [Google Scholar]
- 8.Kono K., Tomita T., Futai K. In vivo three-dimensional kinematics of normal knees during different high-flexion activities. Bone Jt J. 2018;100B:50–55. doi: 10.1302/0301-620X.100B1.BJJ-2017-0553.R2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moewis P., Hommel H., Trepczynski A., Krahl L., von Roth P., Duda G.N. Weight bearing activities change the pivot position after total knee arthroplasty. Sci Rep. 2019;9:1–8. doi: 10.1038/s41598-019-45694-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaneyama R., Higashi H., Oinuma K., Miura Y., Tamaki T., Shiratsuchi H. Improvement of the gap adjustment in total knee arthroplasty using the posterior condylar pre-cut technique. J Knee Surg. 2019;32:1001–1007. doi: 10.1055/s-0038-1675420. [DOI] [PubMed] [Google Scholar]
- 11.Akagi M., Mori S., Nishimura S., Nishimura A., Asano T., Hamanishi C. Variability of extraarticular tibial rotation references for total knee arthroplasty. Clin Orthop Relat Res. 2005;172–6 doi: 10.1097/01.blo.0000160027.52481.32. [DOI] [PubMed] [Google Scholar]
- 12.Yamazaki T., Watanabe T., Nakajima Y. Improvement of depth position in 2-D/3-D registration of knee implants using. IEEE Trans Med Imag. 2004;23:602–612. doi: 10.1109/TMI.2004.826051. [DOI] [PubMed] [Google Scholar]
- 13.Yamazaki T., Watanabe T., Nakajima Y. Visualization of femorotibial contact in total knee arthroplasty using X-ray fluoroscopy. Eur J Radiol. 2005;53:84–89. doi: 10.1016/j.ejrad.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 14.Grood E.S., Suntay W.J. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105:136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 15.Mason J.B., Fehring T.K., Estok R., Banel D., Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 2007;22:1097–1106. doi: 10.1016/j.arth.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 16.Shoji H., Teramoto A., Suzuki T., Okada Y., Watanabe K., Yamashita T. Radiographic assessment and clinical outcomes after total knee arthroplasty using an accelerometer-based portable navigation device. Arthroplast Today. 2018;4:319–322. doi: 10.1016/j.artd.2017.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tamai H., Suzuki M., Tsuneizumi Y. Knee kinematics do not influence the long-term results in posterior cruciate-retaining total knee arthroplasties. Chiba Med J. 2008;84:269–276. [Google Scholar]
- 18.Shu L., Yamamoto K., Kai S., Inagaki J., Sugita N. Symmetrical cruciate-retaining versus medial pivot prostheses: the effect of intercondylar sagittal conformity on knee kinematics and contact mechanics. Comput Biol Med. 2019;108:101–110. doi: 10.1016/j.compbiomed.2019.03.005. [DOI] [PubMed] [Google Scholar]
- 19.Fujimoto E., Sasashige Y., Tomita T., Iwamoto K., Masuda Y., Hisatome T. Significant effect of the posterior tibial slope on the weight-bearing, midflexion in vivo kinematics after cruciate-retaining total knee arthroplasty. J Arthroplasty. 2014;29:2324–2330. doi: 10.1016/j.arth.2013.10.018. [DOI] [PubMed] [Google Scholar]
- 20.Koh I.J., Lin C.C., Patel N.A. Kinematically aligned total knee arthroplasty reproduces more native rollback and laxity than mechanically aligned total knee arthroplasty: a matched pair cadaveric study. Orthop Traumatol Surg Res. 2019;105:605–611. doi: 10.1016/j.otsr.2019.03.011. [DOI] [PubMed] [Google Scholar]
- 21.Khasian M., LaCour M.T., Coomer S.C., Bolognesi M.P., Komistek R.D. In vivo knee kinematics for a cruciate sacrificing total knee arthroplasty having both a symmetrical femoral and tibial component. J Arthroplasty. 2020;35:1712–1719. doi: 10.1016/j.arth.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 22.Sumino T., Tomita T., Sugamoto K., Yamazaki T., Okazaki K. Semi-constrained posterior stabilized total knee arthroplasty reproduces natural deep knee bending kinematics. BMC Muscoskel Disord. 2020;21:1–8. doi: 10.1186/s12891-020-3059-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marcheggiani Muccioli G.M., Pizza N., Di Paolo S. Multi-radius posterior-stabilized mobile-bearing total knee arthroplasty partially produces in-vivo medial pivot during activity of daily living and high demanding motor task. Knee Surg Sports Traumatol Arthrosc. 2020 doi: 10.1007/s00167-020-05846-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.