Abstract
Background:
Care homes are vulnerable to widespread transmission of severe acute respiratory coronavirus virus 2 (SARS-CoV-2) with poor outcomes for staff and residents. Infection control interventions in care homes need to not only be effective in containing the spread of coronavirus disease 2019 (COVID-19) but also feasible to implement in this special setting which is both a healthcare institution and a home.
Methods:
We developed an agent-based model that simulates the transmission dynamics of COVID-19 via contacts between individuals, including residents, staff members, and visitors in a care home setting. We explored a representative care home in Scotland in our base case and explore other care home setups in an uncertainty analysis. We evaluated the effectiveness of a range of intervention strategies in controlling the spread of COVID-19.
Results:
In the presence of the reference interventions that have been implemented in many care homes, including testing of new admissions, isolation of symptomatic residents, and restricted public visiting, routine testing of staff appears to be the most effective and practical approach. Routine testing of residents is no more effective as a reference strategy while routine testing of both staff and residents only shows a negligible additive effect. Modeling results are very sensitive to transmission probability per contact, but the qualitative finding is robust to varying parameter values in our uncertainty analysis.
Conclusions:
Our model predictions suggest that routine testing should target staff in care homes in conjunction with adherence to strict hand hygiene and using personal protective equipment to reduce risk of transmission per contact.
As of July 15, 2020, ~24 million people had been infected with severe acute respiratory coronavirus virus 2 (SARS-CoV-2) worldwide, and 3.4% of those infected have died.1 Many studies have demonstrated that comorbidity and old age are associated with poor outcomes among coronavirus disease 2019 (COVID-19) patients.2,3 Care homes across the globe, where most residents are elderly and have complex medical and care needs, have suffered devastating outcomes.4,5 High rates of mortality involving COVID-19 have been attributed to residents in this setting (eg, 40%–70% in Canada,6 33%–64% in European countries,5 and 47% in Scotland7).
Care homes are integral to the wider healthcare system, and it is essential that they continue to function safely and effectively amid the COVID-19 pandemic to avoid increasing the pressure on the acute-care sector. If care homes stop admitting patients discharged from hospitals, patients have to stay in hospitals longer than they need, putting them at greater risk, adding to the pressure on hospitals, and causing tremendous distress for many individuals. Because vaccination for COVID-19 is currently unavailable, infection control interventions within care homes and across settings are vitally important to protect the vulnerable residents and healthcare workers.
Agent-based models (ABMs) have been used to study epidemic behavior and interventions and to mitigate them in the past couple of decades, leading to new insights. Although compartmental models have been popularly used to simulate transmission dynamics of infectious diseases at the population level, ABMs have been useful for understanding the effects of heterogeneous individual characteristics and behavior in conjunction with the stochasticity of transmission events. They have shown that individual characteristics such as age, comorbidity, and socio-spatial structures and contact patterns in different settings influence disease spread and the effectiveness of interventions.8–12 Many of these factors are important in the care-home setting and for COVID-19 specifically. Influenza and COVID-19 pandemic ABMs have studied disease dynamics and interventions at the population level,10,13–15 and a number of recent ABMs have investigated how interventions in small-scale settings, such as schools and workplaces, would influence the behavior of epidemics in wider communities.10,16,17 None of these models explores the care-home setting, and many measures implemented schools and workplaces, such as closure and social distancing, are not suitable for care homes that also act as a residence and where staff interaction with residents is often unavoidable.
Many studies have investigated the spread of SARS-CoV-2 in the general population, but research on the unique transmission dynamics and interventions for COVID-19 in healthcare settings, and care homes in particular, is scarce. We searched PubMed, MedRxiv, and BioRxiv for papers published between January 1, 2020, and July 15, 2020, that contained the terms (COVID OR coronavirus OR nCoV OR SARS-CoV-2) AND (care home* OR nursing home* OR skilled nursing facility* OR long-term care OR LTCF* OR residential care). We identified 152 preprints and articles published in academic journals, mostly outbreak reports, point prevalence surveys, commentary and editorial papers that discuss the importance and challenges of controlling the spread of SARS-CoV-2 in this setting. They describe experiences of containing spread in some specific care homes and a need for improved control interventions, and they call for more attention and a plan from governments. We found 1 preprint modeling study18 that evaluates the capability of surveillance strategies to detect simulated outbreaks under limited testing capacity in a long-term care hospital. This paucity suggests a lack of research on the transmission dynamics of SARS-CoV-2 and the effectiveness of infection control interventions in this setting. Therefore, we investigated the transmission dynamics of SARS-CoV-2 in a care home and the effectiveness of a range of infection control intervention strategies using agent-based modeling.
Methods
Model
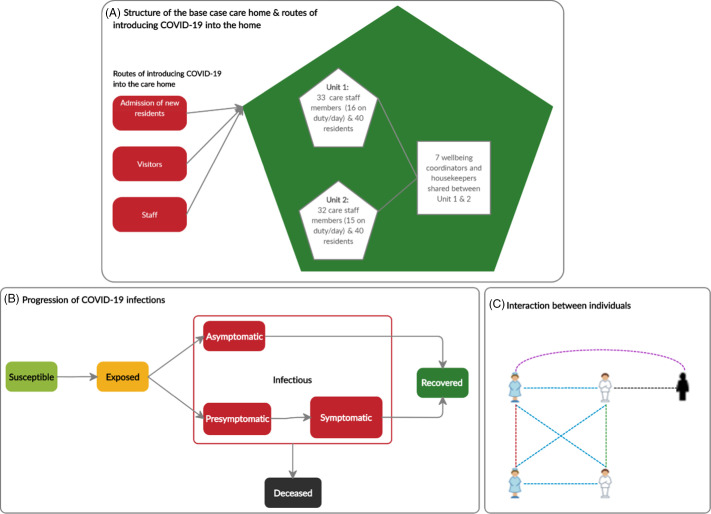
We developed an ABM that simulates the transmission dynamics of SARS-CoV-2 via contacts between individual agents, including residents, staff members, and visitors within a care home. We assumed that all rooms are single occupancy because the vast majority of rooms in Scottish care homes are of this type19 and, based on discussions with care-home stakeholders, single occupancy has been a consensus practice during the COVID-19 pandemic. The model structure (Fig. 1) is described in detail in the ‘ODD’ (overview, design concepts, and details) protocol (Appendix S1 online). In brief, susceptible individuals may acquire the infection when exposed to infectious sources. They are infected but not yet infectious (exposed). Once exposed, individuals become infectious, they can either remain asymptomatic for the entire infectious period or develop symptoms after a presymptomatic period. Symptoms could be mild or severe and require hospitalization. Infectious individuals eventually recover or die. Infections can be imported into the care home by infected residents upon admission (from hospitals and the community) and staff or visitors who acquired the infection elsewhere. The COVID-19 prevalence in hospitals and the community determine the probability at which these individuals introduce the infection into the care home. Transmission events occur through contacts made between susceptible and infectious (presymptomatic, asymptomatic, and symptomatic) individuals at risk, determined by the infection probability per contact. We assumed that recovered individuals are immune to reinfection throughout the simulated time. As we examined the spread of SARS-CoV-2 once infection already exists in the care home, 1 random resident is infected at the beginning of the simulation; staff and other residents are susceptible.
Fig. 1.
Overview of the model structure. (A) The structure of the care home and routes of introducing SARS-CoV-2 into the home. The base case care home, representative of a care home in North Lanarkshire, Scotland, has 80 residents and a team of 72 staff members. It is split into 2 units containing 40 residents and 16 and 15 care staff members on duty per unit per day. The staff pools for the 2 units contain 33 and 32 care staff members respectively. A group of 7 well-being coordinators and housekeepers is shared between the 2 units. (B) The progression of COVID-19 cases. Susceptible people may acquire the infection when exposed to infectious sources. They are infected but not yet infectious (exposed state). Once exposed people become infectious, they can either remain asymptomatic for the entire infectious period or develop symptoms after a pre-symptomatic period. Symptoms could be mild or severe and require hospitalizations. Infectious people will eventually recover or die. (C) Interactions between residents, staff and visitors in a care home. The dashed lines linking individuals denote their possible ways of interaction. Different colours are used for these lines to distinguish different types of interaction: blue, staff-resident interaction; green, resident-resident interaction; red, staff–staff interaction; black, resident-visitor interaction; and purple, staff–visitor interactions.
Data collection and parameters
We interviewed care-home stakeholders including managers, staff in different roles, and we had regular discussions with representatives from the Health and Social Care Partnerships and Public Health in Lanarkshire to analyze the problem, build the model, and design the intervention strategies. The interviews were semistructured, and each lasted ~45–60 minutes. We also conducted literature reviews to obtain the values for parameters characterizing the transmission of SARS-CoV-2 and the disease progression. Other parameters are based on national data for Scotland and regional data for North Lanarkshire where available. Model input parameters used for the base case simulation are presented in Table 1.
Table 1.
Input Parameters for Base Case Simulation and Distributions of Parameters
| Input Parameter | Base Case Value | Sensitivity/Uncertainty Analysis | Source |
|---|---|---|---|
| Infection prevalence in the hospital | 0.02 | Triangular distribution (min = 0, max = 0.5, mode = 0.2) | National Records Scotland,7 Public Health Scotland,22Scottish government31(estimated) |
| Infection prevalence in the community | 0.05 | Triangular distribution (min = 0, max = 0.2, mode = 0.05) | Perez-Reche and Strachan21 |
| The probability that an infected resident dies (age-specific) | Drawn for each individual resident from empirical distribution by age: 80+ y: 11% 70–79 y: 6.0% 60–69 y: 2.6% 50–59 y: 0.71% 40–49 y: 0.18% 30–49 y: 0.09% 20–29 y: 0.04% 18–20 y: 0.007% |
No (This parameter does not impact our main model output, the number of infected residents, significantly.) | Ferguson et al,13Kulu and Dorey32
The Infection Fatality Rate (IFR) for Scotland is adjusted based on the overall aged-adjusted IFR value for the UK and the relative IFR value (=1.18) for other urban areas in Scotland. Most of the population (>80%) in North Lanarkshire live in areas classified as other urban areas. |
| The probability that an infected staff member dies | Drawn for each individual staff member from a uniform distribution (0.0003–0.022) | No | Ferguson et al,13Kulu and Dorey32 |
| The no. of contacts that a resident has with other residents per day | Drawn for each individual resident from a Poisson distribution with a mean of 3.9 contacts per resident per day |
Mean of the Poisson distribution is drawn from a triangular distribution (min, 1; max, 5; mode = 3.9) | Van den Dool et al,11Chamchod and Ruan33 |
| The no. of contacts that a staff has with other staff per day | Drawn for each individual staff member from a Poisson distribution with a mean of 7.3 contacts per staff member per day | Mean of the Poisson distribution is drawn from a triangular distribution (min, 1; max, 10; mode, 7.3) | Van den Dool et al11 |
| The no. of contacts that a staff has with residents per day | Drawn for each individual staff member from a Poisson distribution with a mean of 16.2 contacts per staff per day | Mean of the Poisson distribution is drawn from a triangular distribution (min, 10; max, 20; mode, 16.2) | Van den Dool et al,11Chamchod and Ruan33 |
| The no. of contacts that a staff has with visitors per day | 5.0 contacts per staff member per day | Triangular distribution (min, 0; max, 10; mode, 5.0) | Discussions with the manager and staff of the representative care home |
| The probability that a resident comes into contact with another resident in the other unit | 20% | Triangular distribution (min, 0; max, 0.5; mode, 0.2) | Discussions with the manager and staff of the representative care home |
| The average no. of people visiting a resident per day | 1.0 visitor per resident per day | Triangular distribution (min, 0; max, 2.0; mode, 1.0) | Van den Dool et al,11Port et al34 |
| The rate at which residents leave the care home because of deaths caused by other reasons, moving to another facility, admitted to hospitals, or returning to their own home (rare) | 0.005 deaths or discharges per resident per day | Triangular distribution (min, 0.001; max, 0.005; mode, 0.004) | Scotland Information Services19 (Calculated from data for care homes in North Lanarkshire) |
| Staff turnover rate | 24% per year | Triangular distribution (min, 0.1; max, 0.5; mod, 0.24) | Scottish Care35 |
| The probability that an infected resident will develop symptoms | Drawn for each individual resident from empirical distribution: 80+ y: 0.9 70–79 y: 0.85 60–69 y: 0.8 50–59 y: 0.75 40–49 y: 0.7 30–49 y: 0.65 20–29 y: 0.6 18–20 y: 0.55 |
Triangular distribution (min, 0.5; max, 0.9; mode, 0.8) | Ferguson et al,13Verity et al36 |
| The probability that an infected staff member will develop symptoms | 0.7 | Triangular distribution (min, 0.5; max, 0.9; mode, 0.7) | Ferguson et al,13Verity et al36
(for a population like the United Kingdom or the United States) |
| The probability that a symptomatic resident has severe symptoms | Drawn for each individual resident from empirical distribution: 80+ y: 0.28 70–79 y: 0.25 60–69 y: 0.17 50–59 y: 0.11 40–49 y: 0.05 30–49 y: 0.03 20–29 y: 0.01 18–20 y: 0.001 |
No (This parameter does not affect no. of infections significantly given the assumptions that symptomatic individuals are isolated) | Ferguson et al,13Kulu and Dorey32
The proportion of symptomatic cases requiring hospitalizations for Scotland is adjusted based on the overall aged-adjusted value for the United Kingdom |
| The probability that a symptomatic staff member has severe symptoms | Drawn for each individual staff member from a uniform distribution (0.01–0.17) | No | Ferguson et al,13Kulu and Dorey32 |
| The probability that an individual (resident or staff) is infected after coming into contact with another infectious individual (resident, staff or visitor) | 0.02 | Triangular distribution (min, 0.001; max, 0.1; mode, 0.02) | Ferguson et al,13Wang et al,37Tang et al38 |
| The time elapsed between first exposure and becoming infectious | Lognormal (μ = 1.16, σ = 0.85) | No (This parameter does not significantly affect number of infections as exposed individuals are not infectious. Also, values for this parameter are relatively consistent across studies.) | Lauer et al,39McAloon et al,40Nishiura et al41 (log normal mean, 4.6; SD, 4.8) |
| The time elapsed between becoming infectious and onset of symptoms | Discrete uniform distribution (1,3) | No (Values for this parameter are consistent across studies.) | He et al,42 Gatto et al,43 Byrne et al44 |
| The time elapsed between onset of symptoms and recovery (or recovery time for those who remain asymptomatic) | Asymptomatic: log normal (μ = 2.049, σ = 0.246) Symptomatic: Mild: log normal (μ = 2.049, σ = 0.246) Severe: log normal (μ = 2.624, σ = 0.170) |
No (There is a strong consensus about the distribution of this parameter in literature.) | Kerr et al,17 Wölfel et al45 |
| The reduction of resident–resident and staff–staff interactions when social distancing is implemented | 0.75 | Triangular distribution (min, 0.2; max, 0.9; mode, 0.75) | Assumed (based on other models’ assumption13,46 and discussions with care home staff and managers) |
| The sensitivity of RT-PCR test | 0.7 | Triangular distribution (min, 0.6; max, 0.98; mode, 0.7) | Watson et al,47 Arevalo-Rodriguez et al48 |
| The lag between testing and test result | 1 day | No (implemented in scenario-based uncertainty analysis) | Discussion with representatives from Public Health Medicine (NHS Lanarkshire) and Lanarkshire Health and Social Care Partnership |
| Effectiveness of isolation of infected residents | 100% | 50%, 75%, and 100% | Assumed (based on other models’ assumptions13,46) |
Intervention scenarios
We considered the impact of 9 different intervention strategies summarized in Table 2. The reference intervention strategy (Inter1) was based on discussions with local care-home stakeholders in Lanarkshire and aligned with the guidance from the Scottish government for controlling SARS-CoV-2. Interventions such as hand hygiene and using personal protective equipment (PPE) change the infection probability per contact, representing the reduction in transmission risk and an increase in compliance. Residents and staff members who are symptomatic or tested positive are isolated and excluded from work respectively the day after being tested because we assumed it would take 1 day for results to be returned in base-case simulations. Because standard RT-PCR testing is highly specific,20 we assumed perfect specificity. The COVID-19 epidemic in the general population was assumed to be ongoing at a constant prevalence within the simulated time (1 year) because we focused on interventions that do not shield the care home from the external world. Finally, the intervention strategies we examined were in force during this period.
Table 2.
Summary of Intervention Strategies Considered
| Intervention Strategy | Description |
|---|---|
| Inter0 | No intervention |
| Inter1 | Isolation of symptomatic cases & testing of new admissions (2 tests) and social distancing and restricted visiting (referred to as the reference intervention). |
| Inter2 | Inter1 and 14-d compulsory isolation for new admissions regardless of the result of their tests |
| Inter3 | Inter1 and adaptive testing (ie, testing staff and residents and the care home is closed to new admissions when there is a symptomatic case, reopening when all symptomatic and confirmed residents recover) |
| Inter4 | Inter3 and 14-d compulsory isolation for new admissions |
| Inter5 | Inter1 and weekly testing of residents |
| Inter6 | Inter1 and weekly testing of staff |
| Inter7 | Inter1 and weekly testing of staff and residents |
| Inter8 | Inter6 and 14-d compulsory isolation for new admissions |
| Inter9 | Inter7 and 14-d compulsory isolation for new admissions |
Outcomes
A stochastic ABM produces different outputs for the same parameter set; therefore, it requires a large number of simulations to gain an understanding of the behavior of the system over time. We ran 300 simulations for each scenario because the mean outputs converged after this number of simulations. The outcomes we considered in the results were the prevalence of infected residents over time (means and distribution of prevalence at peak) and the cumulative number of infected residents (means, medians, interquartile ranges [IQRs], and 1.5×IQRs).
Uncertainty and sensitivity analyses
We performed global probabilistic sensitivity analyses for parameter uncertainty for the reference intervention (Inter1) and weekly testing of staff strategies (Inter6). The probability distributions of the analyzed parameters are summarized in Table 1. We adopted the Latin hypercube sampling (LHS) method to generate 300 sets of samples, and we performed 100 iterations for each set (ie, 30,000 simulations in total). We calculated the partial rank correlation coefficient (PRCC) to determine the strength of the relationship between each LHS parameter and each outcome measure. We also examined how robust the relative effectiveness of interventions were with respect to the most impactful uncertain parameters determined in the PRCC analysis.
We assessed the impact of the testing interval between 1 and 30 days on the effectiveness of routine testing interventions (Inter6, Inter7, Inter8, and Inter9). We also tested the robustness of the findings to the care home’s capacity, structure, and staff pooling system (Supplementary Table S4-1 in Appendix S4 online). Finally, we examined model outputs with infection prevalence in the community set to historical daily data in Scotland adjusted for undetected cases and start the simulation without a seeded infection.21,22
Statistical analysis
We used the Welch t test at a significant level of α = 0.05 to perform hypothesis testing for difference in the mean cumulative numbers of infections after 90 and 180 days between scenarios (Appendix S2 online). We also adopted the Bonferroni correction method in which the P values were multiplied by the number of tests to counteract the potential type 1 error in multiple comparisons.
Results
Spread of COVID-19
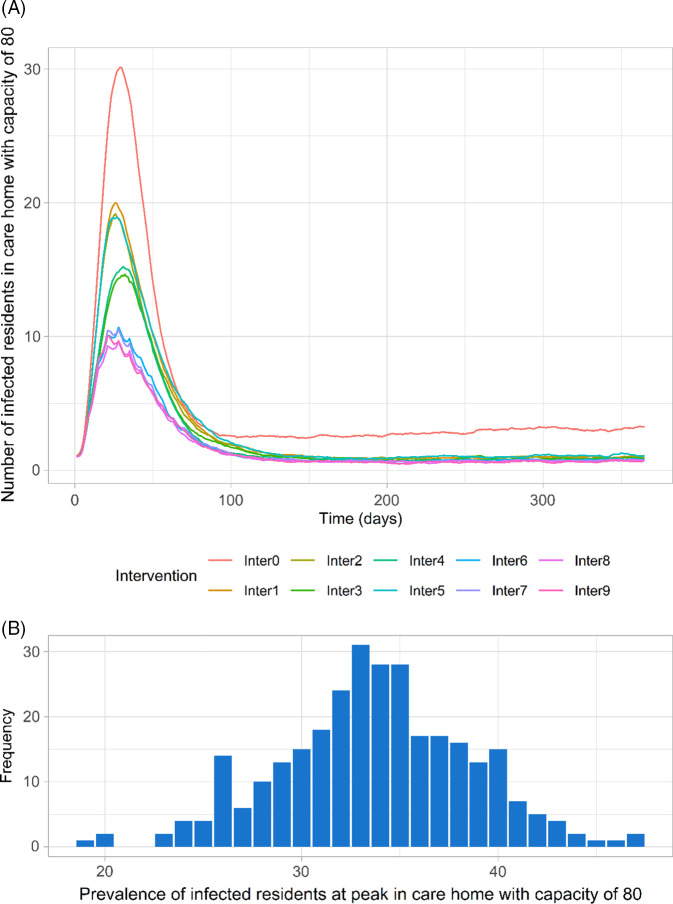
In all scenarios, the mean prevalence of infected residents peaked ~30 days after the first infection in the care home, decreased, then stabilized after around ~90 days (Fig. 2A). The distribution of prevalence at peak (mean, 34; standard deviation [SD], 4.9; range, 19–47) in the no intervention scenario is illustrated in Figure 2B. Relatively large variations in prevalence values are due to stochastic uncertainty of interactions within the care home and disease progression.
Fig. 2.
Time series of COVID-19 prevalence among residents in care home with capacity of 80 residents across all scenarios using the base case parameters (means of 300 simulations for each scenario) (A) and distribution of the prevalence at peak for no intervention scenario (Inter0) using the base case parameters for 300 simulations (B). (Inter0: No intervention; Inter1: Reference intervention (isolation of symptomatic/confirmed residents, testing of new admissions, closed to visitors, social distancing); Inter2: Inter 1 + isolation upon admission; Inter3: Inter1 + adaptive testing strategy; Inter4: Inter3 + isolation upon admission; Inter5: Inter1 + Weekly testing for residents; Inter6: Inter1 + weekly testing for staff; Inter7: Inter1 + weekly testing for staff and residents; Inter8: Inter6 + isolation upon admission; Inter9: Inter7 + isolation upon admission).
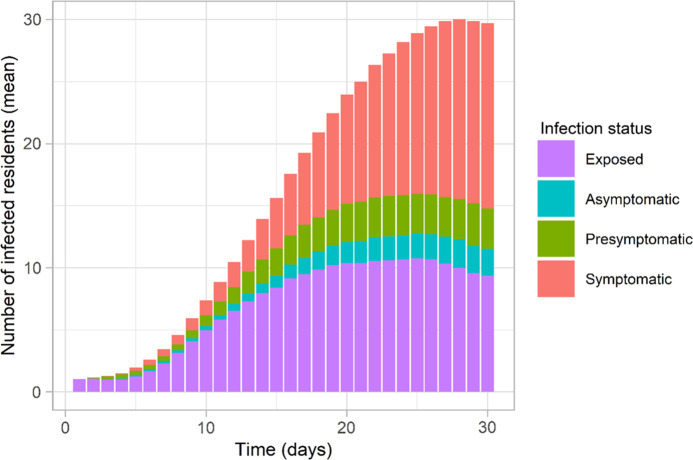
In the absence of any control measures and spontaneous changes in the behaviors of individuals, the introduction of a single infected resident resulted in an outbreak (ie, at least 2 residents are infected) in 99.7% of simulations (299 of 300); in 1 simulation, transmission died out quickly. By the time that any infected residents manifested COVID-19 symptoms, an average of 6 residents (SD, 4.2; range, 1–23) had acquired the infection but may not (yet) have shown symptoms. Infected cases that did not (yet) display symptoms made up approximately half of all infections among residents (Fig. 3), which aligns with reported data.23 Additionally, the proportion of asymptomatic cases among infected residents in our study (7%; range, 4%–10%) shows a good approximation of observed data for long-term aged care (8%; range, 3%–18%).24-26
Fig. 3.
Time series of prevalence of infected residents (mean) in different infection status across 300 simulations when no intervention is implemented (Inter0) using the base case parameters.
Effectiveness of the examined intervention strategies
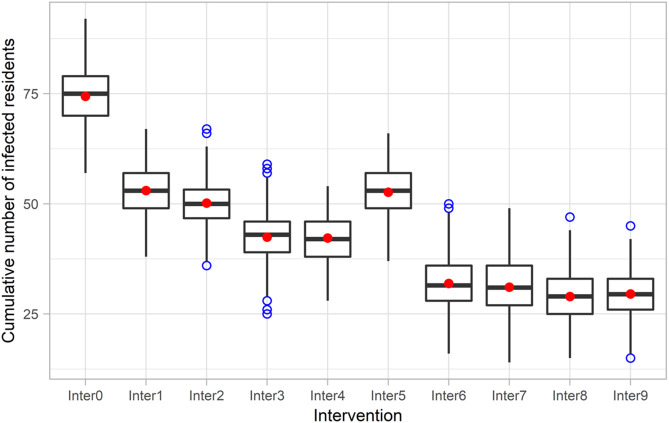
Implementing the reference intervention, which combines isolation of symptomatic residents, testing of new admissions, social distancing, and restricted visiting (Inter1), clearly lowered the peak and reduced the cumulative number of infections after 90 days compared to the no intervention scenario (Inter0) (Fig. 2A and Fig. 4). There was very strong evidence (P < .001) for rejecting the null hypothesis in favor of the alternative hypothesis that the mean cumulative number of infected residents for the reference intervention scenario was lower than the mean when doing nothing (95% CI of the difference, 20.4–22.4 [90 days]).
Fig. 4.
Box plot of cumulative numbers of infected residents 90 days after a resident is infected at the start of the simulation in nine intervention scenarios using the base case parameters (The result is presented as a box plot − lower hinge: 25% quantile; lower whisker: smallest observation greater than or equal to lower hinge − 1.5×IQR; middle: median; upper hinge: 75% quantile; upper whisker: largest observation less than or equal to upper hinge + 1.5×IQR; red dot: mean; blue dot: outlier). Note. IQR, interquartile range.
Adding the 14-day compulsory isolation of new admissions (Inter2) slightly decreased the number of infections compared to the reference intervention strategy (P < .001; 95% CI of the difference, 1.9–3.7 [90 days]). Replacing the isolation of new admissions in strategy Inter3 with or adding the adaptive testing intervention (Inter4) further improved the outcomes. However, because the care home was closed to new admissions for part of the time in these scenarios, the total number of residents were smaller than those in other scenarios, contributing to the lower infections shown in Figure 4 for interventions Inter3 and Inter4. Furthermore, weekly resident testing (Inter5) did not lead to lower infections when compared with the reference intervention (Inter1) (P ~ 1.0).
Weekly testing of staff in the presence of the reference intervention strategy (Inter6) was more effective than Inter2–Inter5, significantly reducing the peak and the cumulative number of infected residents. This intervention strategy reduced the cumulative infections among residents by ~20 cases after 90 days compared to the reference intervention (Inter1) and by ~10 cases compared to adaptive testing (Inter4) (P < .001). A more stringent strategy that involves routine testing for both residents and staff (Inter7) showed little evidence in improving the outcomes (P ~ 1.0; 95% CI of the difference: –0.1 to 1.8 [90 days]). Supplementing these routine testing interventions with isolation of new admissions (Inter8 and Inter9) only slightly reduced the peak and cumulative outcomes. Additional plots of modeling results for different time intervals are included in Appendix S3 (online).
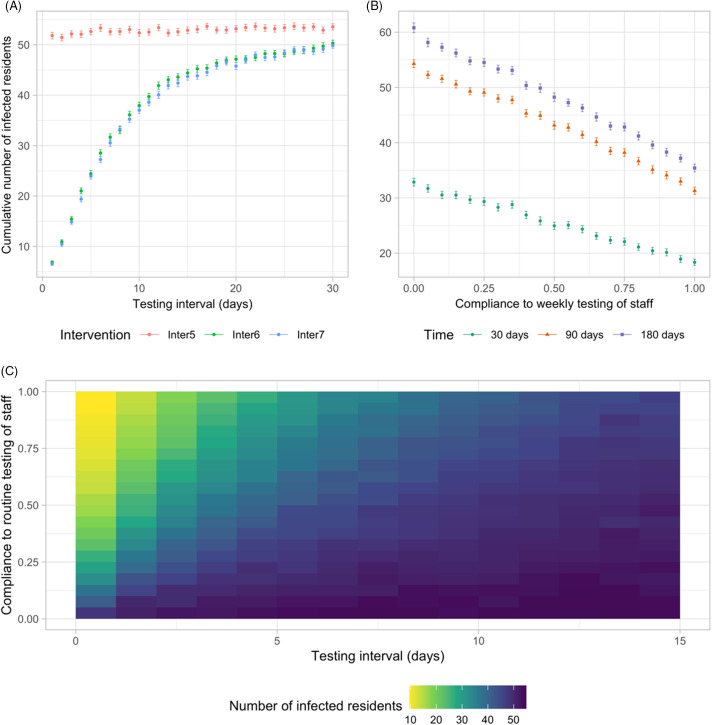
Effectiveness of various routine testing strategies and compliance
Routine testing of residents (Inter5) was predicted to be no more effective than the reference intervention strategy (Inter1) regardless of testing frequency (P ~ 1.0; 95% CI of the difference, –0.1 to 2.1 [180 days]). The effectiveness of routine testing of staff (Inter6) and of staff and residents (Inter7) decreased nonlinearly with increased testing intervals (Fig. 5A). The difference between the 2 interventions (Inter6 and Inter7) reduced as the infection probability reduced (Fig. S4-3 online). Increasing compliance to routine testing of staff linearly reduced the cumulative number of infected residents (Fig. 5B). Moreover, compliance with routine testing of staff had a significant effect on the model outcome when a testing interval was <10 days (Fig. 5C).
Fig. 5.
Effectiveness of different routine testing strategies and compliance. (A) The impact of different testing intervals in routine testing scenarios on the cumulative number of infections after 90 days. (B) The impact of compliance to weekly testing of staff (Inter6) on the cumulative number of infections after 30, 90, and 180 days. Other parameters take the values at base case. (Dots denote the mean values of 300 simulations and error bars represent 95% confidence interval of the mean.) (C) Heatmap plot for the impact of testing interval and compliance to routine testing of staff (Inter6) on the cumulative number of infections after 90 days.
Sensitivity and uncertainty analyses
Outputs from the PRCC analyses are summarized in Appendix S4 (online). The PRCC values measure the associations between each of the parameters and the cumulative number of infected residents after 90 days. The infection probability per contact, the infection prevalence in the community, and the average staff–resident contact rate were the highest contributors to uncertainty in the cumulative prevalence of COVID-19 in care homes in both scenarios. Additionally, the outcomes in testing scenarios were sensitive to test sensitivity. Increasing these parameters led to an increase in cumulative COVID-19 prevalence in care homes. Due to the large correlation between the infection probability and the outcomes, measures including individuals’ hand hygiene and PPE that reduce the risk of transmission are highlighted as extremely important for COVID-19 prevalence.
The examined outcomes were also sensitive to the infection prevalence in the community and staff–resident contact rate but to a significantly lesser extent. The model outcomes were sensitive to the staff–resident contact rate but not to staff–staff and resident–resident contact rates in both scenarios. The difference in sensitivity to different types of contacts ocurred because a social distancing measure was implemented in the reference intervention, and we assumed that the intervention reduced staff–staff and resident–resident contact while staff–resident contact rates remained unchanged. Test sensitivity affected the effectiveness of routine testing of staff strategy. The model outcomes were not sensitive to the number of visitors allowed. Across values of the most impactful parameters, the relative effectiveness of intervention strategies remained unchanged (Supplementary Fig. S4-3 in Appendix 4 online).
The findings regarding the relative effectiveness of interventions were robust when modifying the structures (unit size and residents-per-staff ratio) and capacity of the care home. Unit size or residents-per-staff ratio did not significantly impact the cumulative number of infected residents. Neither did care-home capacity affect the proportion of infections among residents. Furthermore, when we used the daily data of Scotland adjusted for undetected cases21,22 and started the simulation without a seeded infection, the order of the impact of strategies remained robust.
Discussion
We present an ABM that captures heterogeneity and stochasticity of individuals’ disease progression and interaction patterns and their effect on transmission dynamics of SARS-CoV-2 and the effectiveness of control interventions in a care-home setting. Care homes are diverse in terms of their resident population, structure and management, and ABMs have more flexibility compared to simpler epidemiological compartment models to reflect this variation and to examine how it influences findings. The stochastic feature of ABM is well-suited for simulating a small population in an intricate setting like a care home, where chance events can lead to major effects. Furthermore, while deterministic compartment models yield a single output for each parameter set, an ABM produces a distribution of outputs accounting for stochastic uncertainty of interactions within the care home and disease progression.
Our simulations show that once SARS-CoV-2 is introduced into care homes, it spreads very quickly and stopping the spread is very difficult. Because risk of transmission per contact appears to be the most impactful factor on the prevalence and cumulative prevalence of infections among residents, interventions such as hand hygiene and PPE that reduce this risk are crucial for controlling the spread of SARS-CoV-2. The importance of these measures in controlling COVID-19 should be emphasized and reinforced among staff in care homes as they may become less compliant when community transmission improves and interventions are relaxed.
Among the examined SARS-CoV-2 testing strategies, routine testing of staff appears to be the most effective and practical approach in the presence of the reference intervention strategy. When the risk of transmission per contact is reduced by enhancing compliance to hand hygiene and PPE use, the strategy of routine testing of staff is as effective as more stringent interventions strategies. This includes the combination of this strategy and 14-day compulsory isolation of new admissions, routine testing of both staff and residents with/without isolation of new admissions. Routine testing of residents does not show additional effect compared to the reference intervention strategy. Therefore, our model predictions suggest that routine testing should target staff in care homes in conjunction with encouragement and support to enhance compliance to hand hygiene and using PPE.
Our modeling results on the effectiveness of routine testing of staff and residents are supported by a number of recently published studies. Weekly universal testing of all staff and residents irrespective of symptoms conducted in 123 West Virginia nursing homes showed that this intervention was more effective in lowering the prevalence of COVID-19 than daily symptom-based resident and staff screening.27 Other empirical studies in nursing homes in the United States and France also reported that routine universal testing helped identify cases among staff and residents more quickly and interrupted transmission in the facility.28-30 These studies, however, did not examine the impact of routine testing targeting staff only and compared it to resident testing, which is easier to study in a simulation model such as ours than designing a controlled experiment.
Regarding testing intervals, our model predictions, along with discussions with local experts and management regarding feasibility, suggest that routine testing of staff should be carried out every 7–10 days. Although more frequent intervals of testing of staff result in better outcomes, this may not be feasible and is costly. The adverse effects of more frequent testing of staff include increased workload, time pressure, worsened staff shortages, and decreasing tolerance; therefore, they may lead to reduced compliance to testing among staff members. Increasing workload and time pressure may, in turn, affect other care activities provided to residents and staffs’ compliance with testing and hand hygiene, which has greatest impact on the transmission of SARS-CoV-2. A more frequent testing policy could be tailored to care homes with outbreaks to achieve the best outcomes at an acceptable cost. At this stage, we did not explicitly consider the implications of these additional costs in our model.
Care homes are interested in developing strategies for visitors, which is important for the welfare of residents. The model outcomes are not sensitive to the number of visitors allowed because staff that interact with residents more frequently also provide an entry point for infection. This finding suggests that relaxing the visiting policy, will not significantly impact the effectiveness of the examined interventions. However, the assumption that the model starts with a seeded infection limits this interpretation. Further work is required to combine a model such as the one we present with a model of prevalence in the community over time to explore the effect of relaxing visiting under different scenarios of infection prevalence in the community.
This work has a number of limitations. First, we assumed that the level of COVID-19 in the community is static. However, varying this parameter or using time series data of Scotland did not affect the intervention ranking. Second, the model does not account for the potential that residents with atypical symptoms are not successfully detected and, therefore, isolated in a timely manner. However, we conducted sensitivity analysis to consider varying values of the probability residents develop symptoms to reflect this uncertainty because we modeled atypical symptomatic residents who are not detected as asymptomatic residents. We found that this parameter does not affect the outcomes. Third, although we carried out uncertainty and sensitivity analyses on a care home’s size and structure, the diversity of this setting in terms of characteristics of resident populations, health and care services provided, and management would limit the generalization of our findings. Finally, we have not evaluated the cost-effectiveness of the examined interventions which would impact the feasibility of implementation.
In conclusion, our analysis sheds light on the transmission dynamics of COVID-19 in care homes. The effectiveness evaluation of different infection control intervention strategies has potentially significant implications for public health policy making. Infection control interventions in care homes need to be both effective in containing the spread of COVID-19 and also feasible to implement in this setting which has a dual nature: a healthcare institution and a home. Routine testing that targets staff is most effective and practical, and more rigorous testing strategies may not induce additional impact. We also emphasize the importance of interventions such as hand hygiene and using PPE that reduce risk of transmission in inter-individual contacts on the spread of SARS-CoV-2 and the COVID-19 pandemic.
Acknowledgments
We thank Health and Social Care Partnerships and Public Health Medicine - NHS Lanarkshire (Judy Allison, David Cromie, Jim White), and Jennifer McKellar and other staff members in Highgate care home for helpful discussion. We also thank Dr Sarah J.E. Barry from Department of Mathematics and Statistics—University of Strathclyde for reviewing the statistical methods and results of the study.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/ice.2020.1369.
click here to view supplementary material
Financial support
This work was funded by the University of Strathclyde as part of L.L.K.N.’s doctoral project.
Conflicts of interest
All authors declare no potential conflicts of interest related to this article.
References
- 1.Coronavirus disease (COVID-19) pandemic. World Health Organization website. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Published 2020. Accessed 15 July, 2020.
- 2. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA 2020;323:1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McMichael TM, Currie DW, Clark S, et al. Epidemiology of covid-19 in a long-term care facility in King County, Washington. N Engl J Med 2020;382:2005–2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Comas-Herrera A, Zalakain J, Litwin C, Hsu AT, Fernandez-Plotka J-L. Mortality associated with COVID-19 outbreaks in care homes: early international evidence. LTC Responses to COVID website. https://ltccovid.org/2020/04/12/mortality-associated-with-covid-19-outbreaks-in-care-homes-early-international-evidence/?subscribe=success#blog_subscription-3 Published 2020. Accessed 19 April, 2020.
- 6. Hsu AT, Lane N. Impact of COVID-19 on residents of Canada’s long-term care homes — ongoing challenges and policy response. LTC Responses to COVID website. https://ltccovid.org/2020/04/15/impact-of-covid-19-on-residents-of-canadas-long-term-care-homes-ongoing-challenges-and-policy-response/ Published 2020. Accessed 15 April, 2020.
- 7.Deaths involving coronavirus (COVID-19) in Scotland. National Records of Scotland website. https://www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/vital-events/general-publications/weekly-and-monthly-data-on-births-and-deaths/deaths-involving-coronavirus-covid-19-in-scotland Published 2020. Accessed 20 June, 2020.
- 8. Adiga A, Chu S, Eubank S, et al. Disparities in spread and control of influenza in slums of Delhi: findings from an agent-based modelling study. BMJ Open 2018;8:e017353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. He T, Li K, Roberts MS, et al. Prevention of hepatitis C by screening and treatment in US prisons. Ann Intern Med 2016;164:84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hoertel N, Blachier M, Blanco C, et al. A stochastic agent-based model of the SARS-CoV-2 epidemic in France. Nat Med 2020;26:1417–1421. [DOI] [PubMed] [Google Scholar]
- 11. van den Dool C, Bonten MJM, Hak E, Heijne JCM, Wallinga J. The effects of influenza vaccination of healthcare workers in nursing homes: insights from a mathematical model. PLoS Med 2008;5(10):e200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stephenson B, Lanzas C, Lenhart S, et al. Comparing intervention strategies for reducing Clostridioides difficile transmission in acute healthcare settings: an agent-based modeling study. BMC Infect Dis 2020;20:799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ferguson N, Laydon D, Nedjati Gilani G, et al. Report 9: Impact of Non-Pharmaceutical Interventions (NPIs) to Reduce COVID19 Mortality and Healthcare Demand. London: Imperial College London 2020. doi: 10.25561/77482.
- 14. Halloran ME, Ferguson NM, Eubank S, et al. Modeling targeted layered containment of an influenza pandemic in the United States. Proc Nat Acad Sci 2008;105:4639–4644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ferguson NM, Cummings DA, Cauchemez S, et al. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature 2005;437:209–214. [DOI] [PubMed] [Google Scholar]
- 16. Panovska-Griffiths J, Kerr CC, Stuart RM, et al. Determining the optimal strategy for reopening schools, the impact of test and trace interventions, and the risk of occurrence of a second COVID-19 epidemic wave in the UK: a modelling study. Lancet Child Adolescent Health 2020;4:817–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kerr CC, Stuart RM, Mistry D, et al. Covasim: an agent-based model of COVID-19 dynamics and interventions. medRxiv 2020. doi: 10.1101/2020.05.10.20097469. [DOI] [PMC free article] [PubMed]
- 18. Smith DR, Duval A, Pouwels KB, et al. How best to use limited tests? Improving COVID-19 surveillance in long-term care. medRxiv 2020. doi: 10.1101/2020.04.19.20071639. [DOI]
- 19. Care Home Census for Adults in Scotland, 2016. Scotland Information Services Division website. http://www.isdscotland.org/Health-Topics/Health-and-Social-CommunityCare/Publications/2016-10-25/2016-10-25-CHCensus-Report.pdf. Published 2016. Accessed December 10, 2020.
- 20. Corman VM, Landt O, Kaiser M, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Eurosurveillance 2020;25(3):2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Perez-Reche F, Strachan N. Importance of untested infectious individuals for the suppression of COVID-19 epidemics. medRxiv 2020. doi: 10.1101/2020.04.13.20064022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coronavirus (COVID-19) data. Public Health Scotland website. https://publichealthscotland.scot/our-areas-of-work/sharing-our-data-and-intelligence/coronavirus-covid-19-data/ Published 2020. Accessed 20 June, 2020.
- 23. Kimball A, Hatfield KM, Arons M, et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility—King County, Washington, March 2020. Morbid Mortal Wkly Rept 2020;69:377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Byambasuren O, Cardona M, Bell K, Clark J, McLaws M-L, Glasziou P. Estimating the extent of true asymptomatic COVID-19 and its potential for community transmission: systematic review and meta-analysis. medRxiv 2020. doi.org/ 10.1101/2020.05.10.20097543. [DOI] [PMC free article] [PubMed]
- 25. Arons MM, Hatfield KM, Reddy SC, et al. Presymptomatic SARS-CoV-2 infections and transmission in a skilled nursing facility. N Engl J Med 2020;382:2081–2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Freitas F. COVID-19 pandemic: true asymptomatic cases among SARS-CoV-2–infected individuals. SSRN 2020. doi: l10.2139/ssrn.3590123.
- 27. McBee SM, Thomasson ED, Scott MA, et al. Notes from the field: universal statewide laboratory testing for SARS-CoV-2 in nursing homes—West Virginia, April 21–May 8, 2020. Morbid Mortal Wkly Rept 2020;69:1177–1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dora AV, Winnett A, Jatt LP, et al. Universal and serial laboratory testing for SARS-CoV-2 at a long-term care skilled nursing facility for veterans—Los Angeles, California, 2020. Morbid Mortal Wkly Rept 2020;69:651–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sacco G, Foucault G, Briere O, Annweiler C. COVID-19 in seniors: findings and lessons from mass screening in a nursing home. Maturitas 2020;141:46–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hatfield KM, Reddy SC, Forsberg K, et al. Facility-Wide testing for SARS-CoV-2 in nursing homes - seven US jurisdictions, March–June 2020. Morbid Mortal Wkly Rept 2020;69:1095–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coronavirus (COVID-19): daily data for Scotland. Scottish Government website. https://www.gov.scot/publications/coronavirus-covid-19-daily-data-for-scotland/ Published 2020. Accessed 9 August, 2020.
- 32. Kulu H, Dorey P. The contribution of age structure to the number of deaths from COVID-19 in the UK by geographical units. medRxiv 2020. doi: 10.1101/2020.04.16.20067991. [DOI]
- 33. Chamchod F, Ruan S. Modeling the spread of methicillin-resistant Staphylococcus aureus in nursing homes for elderly. PloS One 2012;7(1):e29757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Port CL, Hebel JR, Gruber-Baldini AL, et al. Measuring the frequency of contact between nursing home residents and their family and friends. Nurs Res 2003;52:52–56. [DOI] [PubMed] [Google Scholar]
- 35.Care home workforce data report. Scottish Care website. https://scottishcare.org/wp-content/uploads/2019/11/Care-Home-Workforce-Data-2018.pdf Published 2018. Accessed August 15, 2020.
- 36. Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis 2020;20:669–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wang K, Lu Z, Wang X, et al. Current trends and future prediction of novel coronavirus disease (COVID-19) epidemic in China: a dynamical modeling analysis. Math Biosci Engin 2020;17(4):3052. [DOI] [PubMed] [Google Scholar]
- 38. Tang B, Bragazzi NL, Li Q, Tang S, Xiao Y, Wu J. An updated estimation of the risk of transmission of the novel coronavirus (2019-nCov). Infect Dis Model 2020;5:248–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med 2020. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed]
- 40. McAloon CG, Collins A, Hunt K, et al. The incubation period of COVID-19: a rapid systematic review and meta-analysis of observational research. BMJ Open 2020;10:e039652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Nishiura H, Linton NM, Akhmetzhanov AR. Serial interval of novel coronavirus (COVID-19) infections. Int J Infect Dis 2020;93:284–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. He X, Lau EH, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med 2020;26:672–675. [DOI] [PubMed] [Google Scholar]
- 43. Gatto M, Bertuzzo E, Mari L, et al. Spread and dynamics of the COVID-19 epidemic in Italy: effects of emergency containment measures. Proc Nat Acad Sci 2020;117:10484–10491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Byrne AW, McEvoy D, Collins A, et al. Inferred duration of infectious period of SARS-CoV-2: rapid scoping review and analysis of available evidence for asymptomatic and symptomatic COVID-19 cases. BMJ Open 2020;10:e039856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature 2020;581:465–469. [DOI] [PubMed] [Google Scholar]
- 46. Matrajt L, Leung T. Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerg Infect Dis 2020;26:1740–1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Watson J, Whiting PF, Brush JE. Interpreting a COVID-19 test result. BMJ 2020;369. doi: 10.1136/bmj.m1808. [DOI] [PubMed]
- 48. Arevalo-Rodriguez I, Buitrago-Garcia D, Simancas-Racines D, et al. False-Negative results of initial RT-PCR assays for COVID-19: a systematic review. medRxiv 2020. doi: 10.1101/2020.04.16.20066787. [DOI] [PMC free article] [PubMed]
- 49.COVID-19 pandemic planning scenarios. Centers for Disease Control and Prevention website. https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios.html Published 2020. Accessed June 13, 2020.
- 50.National clinical and practice guidance for adult care homes in Scotland during the COVID-19 pandemic. Scottish Government website. https://www.gov.scot/publications/coronavirus-covid-19-clinical-and-practice-guidance-for-adult-care-homes/ Updated May 15, 2020. Accessed December 10, 2020.
- 51. Taylor R. Interpretation of the correlation coefficient: a basic review. J Diagn Med Sonogr 1990;6:35–39. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/ice.2020.1369.
click here to view supplementary material