Abstract
Background
The coronavirus diseases of 2019 (COVID-19) pandemic was classified as one of the worst pandemics in the 21st century. Its rapid transmission, unpredicted mortality rate, and the uncertainty surrounding its transmission method have evoked additional fear and anxiety. Nonetheless, to the best of our knowledge, no prior study has explored PTSD prevalence three months after the start of the quarantine procedures in Saudi Arabia nor has examined PTSD prevalence by three different methods.
Objective
This observational cross-sectional study aimed to identify the prevalence, severity, and influencing factors of PTSD in different regions of Saudi Arabia three months after the onset of the quarantine procedures related to the COVID-19 pandemic.
Methods
Through the month of June 2020, 1374 people (49.05% men and 50.95% women) completed a 35-item, 10-minute online. The prevalence of PTSD was measured using PCL-S (specific for COVID-19) that assesses the 17 symptoms of PTSD. Resilience was measured using 2-items Arabic version of the Connor-Davidson Resilience Scale 2 (CD-RISC 2).
Results
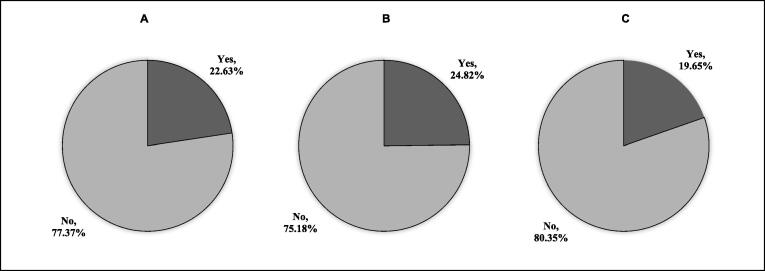
We calculated the prevalence by three methods, namely, PTSD cut-off score, criteria, and combined, and the prevalence was 22.63%, 24.8%, and 19.6%, respectively. Female participants showed higher prevalence than male. As well, participants who were either tested positive or suspected of having been infected with COVID-19 showed higher PTSD prevalence. Higher resilience was associated with lower PTSD prevalence.
Conclusions
This was the first study to report PTSD prevalence by three differential methods three months after the onset of the quarantine procedures related to the COVID-19 pandemic in Saudi Arabia. We observed a significant impact of the COVID-19 pandemic in the Saudi population; therefore, great attention should be performed in implementing new procedures that deal with the highlighted risk factors, especially in vulnerable groups, to overcome the psychological impact of the COVID-19 pandemic.
Keywords: Mental health, Post-traumatic stress disorder, COVID-19, Resilience, Disease prevalence, Saudi Arabia
1. Introduction
Many Saudis still remember the psychological trauma caused by the Middle East respiratory syndrome-related coronavirus (MERS-CoV) outbreak in 2012, especially survivors and those who had direct contact with infected patients (Zaki et al., 2012). Several studies have reported that MERS-CoV survivors suffered social stigmatization and traumatic fear (Almutairi et al., 2018). The general public also showed higher levels of distress and anxiety attributable to susceptibility to infection (Al Najjar et al., 2016). Correlatively, the novel coronavirus disease of 2019 (COVID-19) presented a new global threat owing to its dangerous characteristics (e.g., rapid transmission, unpredictable mortality rate, and the uncertainty about its transmission method, incubation period, and manifestation), which rapidly evoked fear and anxiety in the Saudi population and worldwide. As a safety measure to deal with the COVID-19 pandemic, the Saudi government imposed several precautionary rules to the entire country (e.g., quarantine, 24-hour curfew, and lockdown) to reduce the fast spread of the contagious disease (Al-Tawfiq and Memish, 2020, Yezli and Khan, 2020). Logically, these precautionary measures and the COVID-19 pandemic have a significant impact on mental health, leading to widespread fear, stress, anxiety, and depression (Al Sulais et al., 2020, AlHumaid et al., 2020). Together, these factors could increase the prevalence of post-traumatic stress disorder (PTSD) caused by the quarantine and experiences related to the COVID-19 pandemic.
Cumulative reports have found that natural disasters can be significant traumatic stressors, causing survivors to experience PTSD (Galea et al., 2005, Neria et al., 2008, Sprang and Silman, 2013). In 2003, the Severe Acute Respiratory Syndrome (SARS) outbreak was defined as a bio-disaster, having a severe impact on survivors owing to the traumatic situations they have experienced (Cheng et al., 2006, Chong et al., 2004). A study measured PTSD incidence related to the SARS outbreak, showing that the numbers were equivalent to those reported for natural disasters (Hawryluck et al., 2004). Another study showed that SARS survivors faced traumatic experiences related to dealing with a new deadly infection, witnessing unknown adverse events, an uncertain prognosis, and high risk of intensive care unit admission (Wu et al., 2005b). SARS survivors reportedly presented PTSD symptoms (i.e., increased anxiety and depression) in the early stages of recovery (CHENG et al., 2004, Wu et al., 2005b). Moreover, societal stigma was reported, with people tending to avoid and socially exclude SARS survivors (Lee et al., 2005). Additionally, a study examining SARS survivors’ psychological characteristics 30 months after recovery reported that they had long-term PTSD symptoms, further confirming it as the most prevalent long-term psychiatric condition in this population (Mak et al., 2009). In SARS survivors, PTSD symptom severity was correlated with quarantine length (Hawryluck et al., 2004). Moreover, studies show that other disease outbreaks have caused similar effects; for example, Ebola survivors reportedly had a risk of developing PTSD owing to having been exposed to severe traumatic events related to distress thoughts about having a higher mortality rate (Hugo et al., 2015).
Several studies have suggested that most individuals experience trauma have a psychological balance that prevents and protects the overall mental health (Bonanno, 2004, Bonanno et al., 2006). Therefore, researchers have dedicated great attention to exploring the correlation of individual strengths and adaptational responses facing environmental adversity and trauma (Russo et al., 2012, Wu et al., 2013). Resilience is known as the ability to adapt to trauma, tragedy, or extreme threats (Charney, 2004). In fact, resilience is an essential part of coping, and adjustment experience in trauma recovery process (Anderson & Danis, 2006) A wide range of studies suggested that individuals with higher resilience traits are less susceptible to PTSD symptoms (Bensimon, 2012, Lepore and Revenson, 2006, Levine et al., 2009). Then, suggesting that if an individual experienced extreme stressor or trauma and did not show any PTSD symptoms, resilience is present. Consequently, the adaptability against trauma and extreme stressor such as COVID-19 pandemic is an essential factor that needs to be investigated.
Given the background above and the characteristics of the COVID-19 pandemic, it is reasonable to infer that it may evoke traumatic stressors similar to those related to the SARS epidemic. Untreated PTSD symptoms are unlikely to disappear and can contribute to drug abuse, depression, and sleep problems, all of which negatively influence people’s communication and productivity (DANSKY et al., 1998, Goenjian et al., 2005, Kobayashi et al., 2007). Several sociodemographic factors have been suggested to play an essential role in developing PTSD. For instance, gender has a significant role in this matter, with higher chances of developing PTSD-related symptoms in females as compared to males in response to severe stressful experiences (Luxton et al., 2010, Norris et al., 2002, Olff et al., 2007). As well, healthcare providers who work in close contact with MERS and SARS patients were at higher risk of developing PTSD (Lee et al., 2018, Su et al., 2007). Similarly, patients with a history of psychiatric conditions are at high risk of developing PTSD than healthy individuals (Kmett Danielson et al., 2010, Naeem et al., 2011, Oh et al., 2016). Due to the lack of previous research studies exploring the impact of COVID-19 pandemic on mental health and PTSD; this study aimed to identify the prevalence, severity, and influencing factors of PTSD in different regions of Saudi Arabia three months after the onset of the quarantine procedures related to the COVID-19 pandemic.
2. Methods
2.1. Questionnaire
This cross-sectional study was conducted through the whole month of June 2020; namely, approximately three months after the onset of the quarantine procedures in Saudi Arabia related to the COVID-19 pandemic. The PTSD symptoms usually begin within the first three months after experiencing stressful trauma; however, the degree of severity can differ from one individual to another (Carty et al., 2006, Dunmore et al., 1999, Mayou et al., 2002, Sadeghi-Bazargani et al., 2011). We distributed a survey through different social media platforms. Participants consent was completed at the beginning of the survey. The study inclusion criteria were: Being aged 18 years or older and be currently living in Saudi Arabia. Respondents were asked to complete a 10-minute online survey through the Survey Monkey platform (https://www.surveymonkey.com) regarding the following topics in the context of the COVID-19 pandemic: Sociodemographic data, Psychological impact, PTSD symptoms, and resilience. The significant impact of the COVID-19 pandemic in the Saudi population was investigated among different variables identified as risk factors, such as gender, family death, social stigma toward COVID-19 patients/survivors/suspected patients, marital status, chronic illness such as diabetes mellitus, hypertension, cancer or pulmonary diseases, and current/previous psychiatric condition. In total, 1374 people completed a 35-item questionnaire.
2.2. Instruments
We used a specific version of the PTSD checklist in the Diagnostic and Statistical Manual of Mental Disorders (DSM) survey (PCL-S) was used as a self-report tool to measure the 17 PTSD symptoms described in the DSM-V (Weathers et al., 1993). The PCL-S is a widespread and validated screening tool for making a provisional PTSD diagnosis for a specific event (Boals & Schuettler, 2011). We utilized a version that was translated from English to Arabic and compared it to a validated PCL-C Arabic version (Alhalal et al., 2017). Participants were asked to rate their experiences with the COVID-19 pandemic during the last month. Participants responded through a 5-point scale, ranging from 1 (Not at all) to 5 (Extremely). Their scores were calculated by different methods, which are described hereinafter.
The first method is named PTSD cut-off score; it measures participants’ symptomatic severity through a score range of 17–85. Prior researches show that a cut-off score of 45 or higher should be used when measuring PTSD symptoms through the PCL-S score because it minimizes false-positive diagnoses (Blanchard et al., 1996); thus, we utilized this well-established cutoff score to determine if participants were within the severity threshold of a PTSD diagnosis.
The second method is named PTSD criteria; it was used to check whether participants met the DSM-V symptom criteria for PTSD. Namely, participants must have had at least one symptom from the B category (items 1–5), three from the C category (items 6–12), and at least two from the D category (items 13–17) to meet the criteria. Responses in the range of 3–5 denoted that patients had the symptom described in each of the aforementioned items; participants who had scores for all the aforementioned items in the range of 3–5 were deemed as having the symptomatic pattern of a PTSD diagnosis.
The third method is named PTSD combined; to ensure result reliability, we combined the first and second methods, in that participants had to meet both the severity threshold and the symptomatic pattern described above to be diagnosed with PTSD. All three methods were approved and validated by the National Center for PTSD (Weathers).
We measured resilience using the Arabic version of the Connor-Davidson Resilience Scale 2 (CD-RISC 2)©(Vaishnavi et al., 2007); we obtained the Arabic version with the permission from Dr. Jonathan R.T. Davidson. Resilience was scored with a total of two items, on a five-point scale from 0 (rarely true) to 4 (true nearly all of the time). The 2-item CD-RISC 2 includes two statements; ('Able to adapt to change') and ('Tend to bounce back after illness or hardship') with a higher score of 8 reflecting greater resilience. The shortened version CD-RISC 2 was introduced to the reduced time needed to complete the scale and therefore increased total usages by participants.
2.3. Statistical analysis
We reported participants’ descriptive statistics as frequencies and percentages. We applied a Chi-square test to examine the association between sociodemographic data and PTSD cut-off score, criteria and combined. We used stepwise multivariable logistic regression analyses to explore whether the four aforementioned variables were predictors of PTSD. The models were adjusted for several predictor variables including: age, gender, education level, monthly income, marital status, employment, working outside home during COVID-19, location, lockdown neighbors, infected with COVID-19, quarantine, and family death. We calculated the odds ratio (OR) and 95% confidence interval (CI) by the probability of having PTSD based on the three analysis methods. We set statistical significance as P < 0.05 for all analyses, and these were performed using SAS software.
3. Results
3.1. Sociodemographic data
Participants’ sociodemographic data are shown in Table 1. Among the 1374 participants, we observed similar distributions by gender (49.05% men and 50.95% women). Most participants were aged between 25 and 34 years (37.05%), married (53.28%), worked in governmental jobs (38.72%), and had a university or college degree (61.86%). The survey sample showed a diversity regarding participants monthly income, with higher percentage of participants reported lower income than 1000 SAR monthly (37.48%). Participants were divided into five categories by resident location in Saudi Arabia (i.e., East, Middle, North, South, and West), and most resided in the West (54.37%). Regarding quarantine measurements, (2.77%) of participants reported living in complete lockdown areas, and (9.61%) were isolated from others due to COVID-19 related safety measurements. Approximately 3.71% positive test for COVID-19, (1.97%) were suspected; however, most participants have not been infected with COVID-19 (94.32%). Moreover, 4% of the participants reported previous psychiatric conditions, whereas 12.66% reported a history of chronic health illnesses such as DM, HTN, cancer, or pulmonary diseases.
Table 1.
Sociodemographic data and quarantine related psychosocial variables.
| Variables | All sample | ||
|---|---|---|---|
| Age | 18–24 | N | % |
| 342 | 24.89 | ||
| 25–34 | 509 | 37.05 | |
| 35–44 | 348 | 25.33 | |
| 45–55 | 138 | 10.04 | |
| More than 55 | 37 | 2.69 | |
| Gender | Male | 674 | 49.05 |
| Female | 700 | 50.95 | |
| Education level | Below high school | 31 | 2.26 |
| High school | 225 | 16.38 | |
| University or college | 850 | 61.86 | |
| Postgraduate or above | 268 | 19.51 | |
| Monthly income | Less than 1000 SAR | 515 | 37.48 |
| 1000–5000 | 195 | 14.19 | |
| 5001–10,000 | 217 | 15.79 | |
| 10,001–20,000 | 305 | 22.20 | |
| More than 20,000 | 142 | 10.33 | |
| Marital status | Single | 595 | 43.30 |
| Married | 732 | 53.28 | |
| Divorced/ Widowed | 47 | 3.42 | |
| Employment | Government | 532 | 38.72 |
| Private | 173 | 12.59 | |
| Freelancer | 30 | 2.18 | |
| Student | 275 | 20.01 | |
| Retired | 30 | 2.18 | |
| Unemployed | 334 | 24.31 | |
| Did your work outside your home during COVID 19? | Yes | 382 | 27.8 |
| Location | Eastern Region | 90 | 6.55 |
| Middle Region | 241 | 17.54 | |
| North Region | 157 | 11.43 | |
| South Region | 139 | 10.12 | |
| Western Region | 747 | 54.37 | |
| Living in total lockdown isolated neighbors | Yes | 38 | 2.77 |
| Are you, or have you been, infected with COVID-19? | Confirmed | 51 | 3.71 |
| No / Don't know | 1296 | 94.32 | |
| Suspected | 27 | 1.97 | |
| Did you infect others with COVID-19 | Yes | 13 | 0.95 |
| Do you know people in your immediate social environment who are or have been infected with COVID-19? | Confirmed | 514 | 37.41 |
| No / Don't know | 826 | 60.12 | |
| Suspected | 34 | 2.47 | |
| Death related to COVID-19 in family or friends | Yes | 165 | 12.01 |
| Have you been isolated because of COVID-19 pandemic? | Yes | 132 | 9.61 |
| Previous psychiatric condition before COVID-19 | Yes | 55 | 4.00 |
| Do you have a chronic illness such as DM, HTN, Cancer or pulmonary disease | Yes | 174 | 12.66 |
3.2. PTSD prevalence
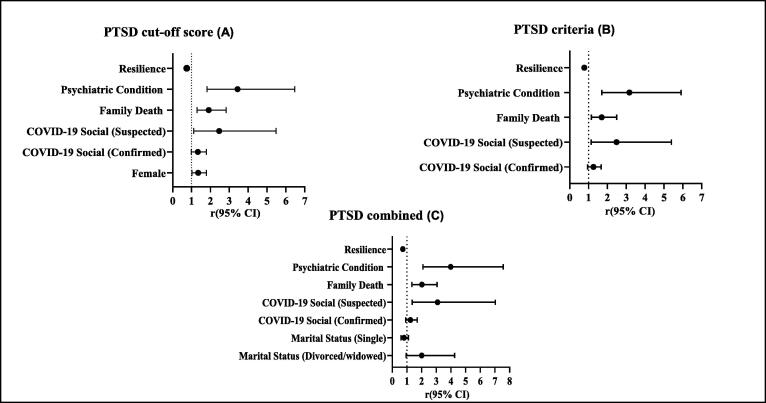
The overall prevalence of PTSD cut-off score, criteria, and combined were 22.63%, 24.8%, and 19.6%, respectively (Fig. 1). Table 2 shows the association between sociodemographic data, predictor variables, and PTSD prevalence, and Fig. 2 shows the results of the regression analysis. We observed a significant association between gender and PTSD prevalence: Females participants showed higher prevalence than males (coefficients; P ≤ 0.05). Moreover, participants who were either confirmed or suspected of having been infected with COVID-19 showed higher PTSD prevalence (coefficients; P ≤ 0.05) than their non-confirmed/suspected counterparts (coefficients; P ≤ 0.05). Single participants showed a higher PTSD prevalence (coefficients; P ≤ 0.05) compared to their divorced/widowed counterparts (coefficients; P ≤ 0.05). Participants who experienced a family member die owing to COVID-19 (coefficients; P ≤ 0.05) and who had previous psychiatric conditions (coefficients; P ≤ 0.05) showed higher PTSD prevalence compared to their counterparts (i.e., participants without family member deaths: coefficients; P ≤ 0.05; without psychiatric conditions: coefficients; P ≤ 0.05). Conversely, participants with high resilience scores showed lower PTSD prevalence (coefficients; P ≤ 0.05) compared to their lower resilience counterparts (coefficients; P ≤ 0.05).
Fig. 1.
The prevalence of PTSD according to three different scoring parameters. A) The prevalence of PTSD as calculated with cut-off score of 45, B) The prevalence of PTSD as calculated with specific criteria as described participants must have had at least one symptom from the B category (items 1–5), three from the C category (items 6–12), and at least two from the D category (items 13–17) to meet the criteria, C) The prevalence of PTSD combined as calculated the first and second methods.
Table 2.
Sociodemographic data and PTSD scoring using PCL-S.
| Variables | PTSD cut-off score | PTSD cut-off score | P value | PTSD criteria | PTSD criteria | P value | PTSD combined | PTSD combined | P value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | |||||||||||
| Age | Less than 18 | N | % | N | % | N | % | N | % | N | % | N | % | |||
| 18–24 | 77 | 24.76 | 265 | 24.93 | 0.62 | 87 | 25.51 | 255 | 24.69 | 0.708 | 64 | 23.7 | 278 | 25.18 | 0.72 | |
| 25–34 | 125 | 40.19 | 384 | 36.12 | 133 | 39 | 236 | 36.4 | 107 | 39.63 | 402 | 36.41 | ||||
| 35–44 | 76 | 24.44 | 272 | 25.59 | 84 | 24.63 | 264 | 25.56 | 70 | 25.93 | 278 | 25.18 | ||||
| 45–55 | 26 | 8.36 | 112 | 10.54 | 28 | 8.21 | 110 | 10.65 | 22 | 8.15 | 116 | 10.51 | ||||
| More than 55 | 7 | 2.25 | 30 | 2.82 | 9 | 2.64 | 28 | 2.71 | 7 | 2.59 | 30 | 2.72 | ||||
| Gender | Male | 140 | 45.02 | 560 | 52.68 | 0.017 | 163 | 47.8 | 537 | 51.98 | 0.18 | 126 | 46.67 | 574 | 51.99 | 0.11 |
| Female | 171 | 54.98 | 503 | 47.32 | 178 | 52.2 | 496 | 48.02 | 144 | 53.33 | 530 | 48.01 | ||||
| Education level | Below high school | 7 | 2.25 | 24 | 2.26 | 0.94 | 7 | 2.05 | 24 | 2.32 | 0.83 | 6 | 2.22 | 25 | 2.26 | 0.97 |
| High school | 49 | 15.76 | 176 | 16.56 | 61 | 17.89 | 164 | 15.88 | 46 | 17.04 | 179 | 16.21 | ||||
| University or college | 197 | 63.34 | 653 | 61.43 | 206 | 60.41 | 644 | 62.34 | 164 | 60.74 | 686 | 62.14 | ||||
| Postgraduate or above | 58 | 18.65 | 210 | 19.76 | 67 | 19.65 | 201 | 19.65 | 54 | 20 | 214 | 19.38 | ||||
| Monthly income | Less than 1000 SAR | 123 | 39.55 | 392 | 36.88 | 0.16 | 133 | 39 | 382 | 36.98 | 0.70 | 103 | 38.15 | 412 | 37.32 | 0.57 |
| 1000–5000 | 55 | 17.68 | 140 | 13.17 | 53 | 15.54 | 142 | 13.75 | 46 | 17.04 | 149 | 13.5 | ||||
| 5001–10,000 | 43 | 13.83 | 174 | 16.37 | 51 | 14.96 | 166 | 16.07 | 39 | 14.44 | 178 | 16.12 | ||||
| 10,001–20,000 | 61 | 19.61 | 244 | 22.95 | 74 | 21.7 | 231 | 22.36 | 57 | 21.11 | 248 | 22.46 | ||||
| More than 20,000 | 29 | 9.32 | 113 | 10.63 | 30 | 8.8 | 112 | 10.84 | 25 | 9.26 | 117 | 10.6 | ||||
| Marital status | Single | 134 | 43.09 | 461 | 43.37 | 0.01 | 147 | 43.11 | 448 | 43.37 | 0.015 | 114 | 42.22 | 481 | 43.57 | |
| Married | 158 | 50.8 | 574 | 54 | 174 | 51.03 | 55 | 54.02 | 139 | 51.48 | 593 | 53.71 | ||||
| Divorced/ Widowed | 19 | 6.11 | 28 | 2.63 | 20 | 5.87 | 27 | 2.61 | 17 | 6.3 | 30 | 2.72 | ||||
| Employment | Government | 107 | 34.41 | 425 | 39.98 | 0.123 | 119 | 34.9 | 413 | 39.98 | 0.34 | 96 | 35.56 | 436 | 39.49 | 0.11 |
| Private | 40 | 12.86 | 133 | 12.51 | 46 | 13.49 | 127 | 12.29 | 34 | 12.59 | 139 | 12.59 | ||||
| Freelancer | 10 | 3.22 | 20 | 1.88 | 10 | 2.93 | 20 | 1.94 | 10 | 3.7 | 20 | 1.81 | ||||
| Student | 57 | 18.33 | 218 | 20.51 | 66 | 19.35 | 209 | 20.23 | 46 | 17.04 | 229 | 20.74 | ||||
| Retired | 6 | 1.93 | 24 | 2.26 | 6 | 1.76 | 24 | 2.32 | 6 | 2.22 | 24 | 2.17 | ||||
| Unemployed | 91 | 29.26 | 243 | 22.86 | 94 | 27.57 | 240 | 23.23 | 78 | 28.89 | 256 | 23.19 | ||||
| Did your work outside your home during COVID 19? | Yes | 75 | 24.12 | 236 | 75.88 | 0.099 | 81 | 23.75 | 260 | 76.25 | 0.054 | |||||
| Location | Eastern Region | 29 | 9.32 | 61 | 5.74 | 0.0589 | 31 | 9.09 | 59 | 5.71 | 0.135 | 26 | 9.63 | 64 | 5.8 | 0.04 |
| Middle Region | 64 | 20.58 | 177 | 16.65 | 65 | 19.06 | 176 | 17.04 | 56 | 20.74 | 185 | 16.76 | ||||
| North Region | 34 | 10.93 | 123 | 11.57 | 33 | 9.68 | 124 | 12 | 28 | 10.37 | 129 | 11.68 | ||||
| South Region | 26 | 8.36 | 113 | 11.57 | 36 | 10.56 | 103 | 9.97 | 20 | 7.41 | 119 | 10.78 | ||||
| Western Region | 158 | 50.8 | 589 | 55.41 | 176 | 51.61 | 571 | 55.28 | 140 | 51.85 | 607 | 54.98 | ||||
| Living in total lockdown isolated neighbors | Yes | 9 | 2.89 | 302 | 97.11 | 0.875 | 11 | 3.23 | 330 | 96.77 | 0.55 | 8 | 2.96 | 262 | 97.04 | 0.82 |
| Are you, or have you been, infected with COVID-19? | Confirmed | 12 | 3.86 | 39 | 3.67 | 0.074 | 14 | 4.11 | 37 | 3.58 | 0.29 | 12 | 4.44 | 39 | 3.53 | 0.14 |
| No / Don't know | 288 | 92.6 | 1008 | 94.83 | 317 | 92.96 | 979 | 94.77 | 249 | 92.22 | 1047 | 94.84 | ||||
| Suspected | 11 | 3.54 | 16 | 1.51 | 10 | 2.93 | 17 | 1.65 | 9 | 3.33 | 18 | 1.63 | ||||
| Did you infect others with COVID-19 | Yes | 1 | 0.32 | 310 | 99.68 | 0.319 | 3 | 0.88 | 338 | 99.12 | 0.88 | 1 | 0.37 | 269 | 99.63 | 0.48 |
| Do you know people in your immediate social environment who are or have been infected with COVID-19? | Confirmed | 136 | 43.73 | 378 | 35.56 | 0.003 | 144 | 42.23 | 370 | 35.82 | 0.004 | 116 | 42.96 | 398 | 36.05 | 0.003 |
| No / Don't know | 163 | 52.41 | 663 | 62.37 | 183 | 53.67 | 643 | 62.25 | 142 | 52.59 | 684 | 61.96 | ||||
| Suspected | 12 | 3.86 | 22 | 2.07 | 14 | 4.11 | 20 | 1.94 | 12 | 4.44 | 22 | 1.99 | ||||
| Death related to COVID-19 in family or friends | Yes | 55 | 17.68 | 256 | 82.32 | 0.0005 | 57 | 16.72 | 284 | 83.28 | 0.002 | 50 | 18.52 | 220 | 81.48 | 0.0002 |
| Have you been isolated because of COVID-19 pandemic? | Yes | 38 | 12.22 | 273 | 87.78 | 0.075 | 43 | 12.61 | 298 | 87.39 | 0.03 | 34 | 12.59 | 236 | 87.41 | 0.0633 |
| Previous psychiatric condition before COVID-19 | Yes | 31 | 9.97 | 280 | 90.03 | <0.0001 | 31 | 9.09 | 310 | 90.91 | <0.0001 | 30 | 11.11 | 240 | 88.89 | <0.0001 |
| Do you have a chronic illness such as DM, HTN, Cancer or pulmonary disease | Yes | 45 | 14.47 | 266 | 85.53 | 0.276 | 49 | 14.37 | 292 | 85.63 | 0.274 | 42 | 15.56 | 228 | 84.44 | 0.11 |
Fig. 2.
Forest plot of odds ratio and 95% confidence interval. A) represents several predictors associated with PTSD as calculated with cut-off score of 45, B) represents several predictors associated with PTSD as calculated with specific criteria as described participants must have had at least one symptom from the B category (items 1–5), three from the C category (items 6–12), and at least two from the D category (items 13–17) to meet the criteria, C) represents several predictors associated with PTSD combined the first and second methods.
4. Discussion
This study aimed to investigate the prevalence, severity, and influencing factors of PTSD in different Saudi Arabia regions three months after the onset of the quarantine procedures related to the COVID-19 pandemic. Our results showed that the prevalence by the three methods of PTSD cut-off score, criteria, and combined were 22.63%, 24.8%, and 19.6%, respectively. Several studies using PTSD cut-off score to report on PTSD prevalence showed similar or higher results: In the USA (31.8%) (C. H. Liu et al., 2020), Italy (29.5%) (Forte et al., 2020), and Spain (15.8%) (González-Sanguino et al., 2020); others have reported lower prevalence, such as in China, in which it ranged from 2.7% to 12.8% (Liang et al., 2020, Liu et al., 2020b, Tang et al., 2020). These differential results could be explained, for example, by shorter periods between the onset of the COVID-19 outbreak and data collection, different sample sizes, or even a different method of analysis. Nonetheless, our study stressed a negative influence of the quarantine owing to the COVID-19 pandemic in Saudi Arabia on people’s psychological health, specifically regarding PTSD symptoms. Correlatively, in the Lebanese population, it was reported that PTSD symptoms were correlated with quarantine length (Fawaz & Samaha, 2020).
Our results emphasized that women had a greater propensity to experience PTSD symptoms than men. Confirming, several studies have reported that disease outbreaks have a higher effect on women than on men, demonstrating that women are at higher risk of developing PTSD symptoms (Lai et al., 2020, Liu et al., 2020b, Mak et al., 2010). Further, reports have shown that women respond differently to extremely stressful events compared with men: Women with PTSD experience greater brainstem activation in response to threats (i.e., they may respond more intensely and abruptly and less reflectively under these conditions), while men showed greater capacity to contextualize fear-related stimuli (Felmingham et al., 2010). Others have justified gender differences by hormones, in that estrogen—which is generally less present in men than in women—could be a great influencing factor of women’s responses to trauma and to PTSD symptoms (Glover et al., 2012, Lebron-Milad et al., 2012). However, regardless of the several studies that have provided evidence on these influencing factors, they are not sufficient to explain why women have presented higher risk of developing PTSD symptoms than men in our study; thus, further research is warranted to explore this topic.
Our results also demonstrated a higher prevalence of PTSD in COVID-19 survivors/suspected patients. Correlatively, the COVID-19 infection made patients and survivors experience psychological outcomes associated with PTSD symptoms (Bo et al., 2020). Similar experiences have been reported for SARS survivors: A study highlighted that they reported increased anxiety, depression, and PTSD symptoms owing to the epidemic (Wu et al., 2005a), and another that they had higher stress levels one year after the SARS outbreak (Lee et al., 2007). Therefore, COVID-19 survivors may be at higher risk of developing PTSD, possibly owing to experiences related to prolonged stress and fear.
Our results also demonstrated that family death owing to COVID-19 was a substantial risk factor for PTSD. Generally, family death or loss of a loved one can cause depression in family members close to the deceased (Pochard et al., 2005). The funeral process and receiving grieving support were both shown to help family members in their recovery and healing process (Gamino et al., 2000). However, owing to the COVID-19 pandemic and social distancing requirements, funeral practices have been restricted internationally and in Saudi Arabia (Yezli & Khan, 2020); in addition to such hindrances and their consequent limited social support, people have also had to endure the enforcement of quarantines around the world. Several studies have shown that the quarantine, in itself, can increase psychological stress and aggravate mental health (Brooks et al., 2020, Lei et al., 2020, Picaza Gorrochategi et al., 2020). As highlighted by our study results, all of these factors add insult to injury and may exacerbate PTSD prevalence. Therefore, grieving support and proper communication opportunities should be provided for families who lost a loved one during the COVID-19 pandemic.
In the literature, people’s ability to recover from trauma, and extremely stressful experiences has been measured by different resilience scales (Connor and Davidson, 2003, Waaktaar and Torgersen, 2010). In our study, participants who had positive acclimatization to stressful life experiences (e.g., a pandemic) were shown to be at a lower risk of developing PTSD symptoms. Conceptualizing, resilience is a dynamic process that can act as a defense mechanism against mental health disturbances (Rutten et al., 2013). Cumulative reports have suggested that resilience is linked to many variables, such as genetics, environment, and social interactions (Bonanno et al., 2001, Brown and Westaway, 2011, Feder et al., 2009). Moreover, people have different nervous systems that thereby respond differently toward similar stressful stimuli, which denotes that resilience may also be affected by it; for example, a study measuring the cortisone levels of participants who experienced an acute stressor (i.e., a public speech task) revealed a strong association between activity in the hypothalamic-pituitaryadrenal axis (which plays an essential role in response to stress), cortisone levels, and resilience (Mikolajczak et al., 2008). Thus, many researchers/clinicians are trying to develop new strategies to identify risk factors of diminished resilience and preventable measures to enhance it (Horn et al., 2016, Horn and Feder, 2018, Iacoviello and Charney, 2014). We believe that resilience may be vital in preventing PTSD due to disease outbreaks, so we suggest that studies focus on resilience in future researches.
Several limitations could affect the interpretation of the study. The recruited sample in this study does not represent the entire population of Saudi Arabia. Social media was used to recruit the participants because of the exceptional circumstance of COVID-19 and strict government measurements to ensure personal distancing. However, individuals with no internet access and no social media accounts, cell phones, or computers cannot participate; thus, the sample does not represent the whole population of Saudi Arabia. The survey was distributed in the Arabic language, which neglected non-Arabic speakers. The recruited sample in this study was collected as a convenience sample, and a substantial consideration should be given not to generalize these data to the broader population other than Saudi Arabia. The study did not examine young individuals less than 18. As well, the study did not examine older adults (over the age of 55) due to limited responses. Also, self-report surveys itself has limitations, as a misinterpretation of the questions could happen. Further studies are still warranted to cover most of these limitations.
Concluding, this was, to the best of our knowledge, the first study to report on PTSD prevalence in Saudi Arabia during the COVID-19 pandemic. Our results demonstrated a significant impact of the COVID-19 pandemic in the Saudi population, and those multiple variables were identified as risk factors, such as gender, family death, social stigma toward COVID-19 patients/survivors/suspected patients, marital status, and psychiatric condition. We suggest that officials in the Ministry of Health in Saudi Arabia implementing new procedures that deal with the highlighted risk factors, especially in vulnerable groups, to overcome the psychological impact of the COVID-19 pandemic.
Authorship and copyright
All authors the work described has not been published previously and it is not under consideration for publication elsewhere. This manuscript is approved by all authors and tacitly and explicitly by the responsible authorities where the work was carried out. It will not be published elsewhere in the same form, in English or in any other language, including electronically without the written consent of the copyright-holder.
Ethics approval
The Biomedical Committee of Research Ethics at the faculty of medicine at Umm Al-Qura University approved the study (Approval no. HAPO-02-K-012-2020-06-394).
Author contribution
Fahad Alshehri, Yasser AlAtawi, Badrah Alghamdi, Abdullah Alhifany, Adnan Alharbi participated protocol design, data collection and in conducting the study. Fahad Alshehri wrote the manuscript. Yasser AlAtawi analyzed the data. All authors reviewed the approved the final manuscript.
Funding
This work was funded by the Research and Development Grants Program for National Research Institutions and Centers (GRANTS), Target Research Program, Infectious Diseases Research Grant Program, King Abdulaziz City for Science and Technology (KACST), Kingdom of Saudi Arabia under grant [5-20-01-007-0021].
Declaration of Competing Interest
No potential competing interest was reported by the authors.
Footnotes
Peer review under responsibility of King Saud University.
References
- Al-Tawfiq J.A., Memish Z.A. COVID-19 in the Eastern Mediterranean Region and Saudi Arabia: prevention and therapeutic strategies. Int. J. Antimicrob. Agents. 2020;55(5):105968. doi: 10.1016/j.ijantimicag.2020.105968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Najjar N.S., Attar L.M., Farahat F.M., Al Thaqafi A. Psychobehavioural responses to the 2014 Middle East respiratory syndrome-novel corona virus [MERS CoV] among adults in two shopping malls in Jeddah, western Saudi Arabia. EMHJ-Eastern Mediterranean Health J. 2016;22(11):817–823. doi: 10.26719/2016.22.11.817. https://apps.who.int/iris/handle/10665/260277 [DOI] [PubMed] [Google Scholar]
- Al Sulais E., Mosli M., AlAmeel T. The psychological impact of COVID-19 pandemic on physicians in Saudi Arabia: A cross-sectional study. Saudi J. Gastroenterol. 2020;26(5):249–255. doi: 10.4103/sjg.SJG_174_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhalal E., Ford-Gilboe M., Wong C., AlBuhairan F. Reliability and validity of the Arabic PTSD Checklist Civilian Version (PCL-C) in women survivors of intimate partner violence. Res. Nurs. Health. 2017;40(6):575–585. doi: 10.1002/nur.21837. [DOI] [PubMed] [Google Scholar]
- AlHumaid J., Ali S., Farooq I. The psychological effects of the COVID-19 pandemic and coping with them in Saudi Arabia. Psychol. Trauma. 2020;12(5):505–507. doi: 10.1037/tra0000623. [DOI] [PubMed] [Google Scholar]
- Almutairi A.F., Adlan A.A., Balkhy H.H., Abbas O.A., Clark A.M. It feels like I’m the dirtiest person in the world. J. Infect. Public Health. 2018;11(2):187–191. doi: 10.1016/j.jiph.2017.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson K.M., Danis F.S. Adult Daughters of Battered Women: Resistance and Resilience in the Face of Danger. Affilia. 2006;21(4):419–432. doi: 10.1177/0886109906292130. [DOI] [Google Scholar]
- Bensimon M. Elaboration on the association between trauma, PTSD and posttraumatic growth: The role of trait resilience. Personality Individ. Differ. 2012;52(7):782–787. doi: 10.1016/j.paid.2012.01.011. [DOI] [Google Scholar]
- Blanchard E.B., Jones-Alexander J., Buckley T.C., Forneris C.A. Psychometric properties of the PTSD checklist (PCL) Behav. Res. Ther. 1996;34(8):669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Bo H.X., Li W., Yang Y., Wang Y., Zhang Q., Cheung T., Wu X., Xiang Y.T. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol. Med. 2020;1–2 doi: 10.1017/S0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boals A., Schuettler D. A double-edged sword: Event centrality, PTSD and posttraumatic growth. Appl. Cognit. Psychol. 2011;25(5):817–822. doi: 10.1002/acp.1753. [DOI] [Google Scholar]
- Bonanno G.A. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am. Psychol. 2004;59(1):20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- Bonanno G.A., Galea S., Bucciarelli A., Vlahov D. Psychological Resilience After Disaster: New York City in the Aftermath of the September 11th Terrorist Attack. Psychol. Sci. 2006;17(3):181–186. doi: 10.1111/j.1467-9280.2006.01682.x. [DOI] [PubMed] [Google Scholar]
- Bonanno G.A., Papa A., O'Neill K. Loss and human resilience. Appl. Prevent. Psychol. 2001;10(3):193–206. doi: 10.1016/S0962-1849(01)80014-7. [DOI] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown K., Westaway E. Agency, Capacity, and Resilience to Environmental Change: Lessons from Human Development, Well-Being, and Disasters. Annu. Rev. Environ. Resour. 2011;36(1):321–342. doi: 10.1146/annurev-environ-052610-092905. [DOI] [Google Scholar]
- Carty J., O'Donnell M.L., Creamer M. Delayed-onset PTSD: A prospective study of injury survivors. J. Affect. Disord. 2006;90(2-3):257–261. doi: 10.1016/j.jad.2005.11.011. [DOI] [PubMed] [Google Scholar]
- Charney D.S. Psychobiological Mechanisms of Resilience and Vulnerability: Implications for Successful Adaptation to Extreme Stress. AJP. 2004;161(2):195–216. doi: 10.1176/appi.ajp.161.2.195. [DOI] [PubMed] [Google Scholar]
- CHENG S.K.W., WONG C.W., TSANG J., WONG K.C. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS) Psychol. Med. 2004;34(7):1187–1195. doi: 10.1017/S0033291704002272. [DOI] [PubMed] [Google Scholar]
- Cheng S.K.W., Chong G.H.C., Chang S.S.Y., Wong C.W., Wong C.S.Y., Wong M.T.P., Wong K.C. Adjustment to severe acute respiratory syndrome (SARS): Roles of appraisal and post-traumatic growth. Psychol. Health. 2006;21(3):301–317. doi: 10.1080/14768320500286450. [DOI] [Google Scholar]
- Chong M.-Y., Wang W.-C., Hsieh W.-C., Lee C.-Y., Chiu N.-M., Yeh W.-C., Huang T.-L., Wen J.-K., Chen C.-L. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry. 2004;185(2):127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- Connor K.M., Davidson J.R.T. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC) Depress. Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- DANSKY B., BRADY K., SALADIN M. Untreated Symptoms of PTSD Among Cocaine-Dependent IndividualsChanges Over Time. J. Subst. Abuse Treat. 1998;15(6):499–504. doi: 10.1016/S0740-5472(97)00293-6. [DOI] [PubMed] [Google Scholar]
- Dunmore E., Clark D.M., Ehlers A. Cognitive factors involved in the onset and maintenance of posttraumatic stress disorder (PTSD) after physical or sexual assault. Behav. Res. Ther. 1999;37(9):809–829. doi: 10.1016/S0005-7967(98)00181-8. [DOI] [PubMed] [Google Scholar]
- Fawaz M., Samaha A. COVID-19 quarantine: Post-traumatic stress symptomatology among Lebanese citizens. Int. J. Soc. Psychiatry. 2020;66(7):666–674. doi: 10.1177/0020764020932207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feder A., Nestler E.J., Charney D.S. Psychobiology and molecular genetics of resilience. Nat. Rev. Neurosci. 2009;10(6):446–457. doi: 10.1038/nrn2649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felmingham K., Williams L.M., Kemp A.H., Liddell B., Falconer E., Peduto A., Bryant R. Neural responses to masked fear faces: sex differences and trauma exposure in posttraumatic stress disorder. J. Abnorm. Psychol. 2010;119(1):241–247. doi: 10.1037/a0017551. [DOI] [PubMed] [Google Scholar]
- Forte G., Favieri F., Tambelli R., Casagrande M. COVID-19 Pandemic in the Italian Population: Validation of a Post-Traumatic Stress Disorder Questionnaire and Prevalence of PTSD Symptomatology. Int. J. Environ. Res. Public Health. 2020;17(11):4151. doi: 10.3390/ijerph17114151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Nandi A., Vlahov D. The Epidemiology of Post-Traumatic Stress Disorder after Disasters. Epidemiol. Rev. 2005;27(1):78–91. doi: 10.1093/epirev/mxi003. [DOI] [PubMed] [Google Scholar]
- Gamino L.A., Easterling L.W., Stirman L.S., Sewell K.W. Grief adjustment as influenced by funeral participation and occurrence of adverse funeral events. OMEGA-J. Death Dying. 2000;41(2):79–92. doi: 10.2190/2FQMV2-3NT5-BKD5-6AAV. [DOI] [Google Scholar]
- Glover E.M., Jovanovic T., Mercer K.B., Kerley K., Bradley B., Ressler K.J., Norrholm S.D. Estrogen Levels Are Associated with Extinction Deficits in Women with Posttraumatic Stress Disorder. Biol. Psychiatry. 2012;72(1):19–24. doi: 10.1016/j.biopsych.2012.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goenjian A.K., Walling D., Steinberg A.M., Karayan I., Najarian L.M., Pynoos R. A Prospective Study of Posttraumatic Stress and Depressive Reactions Among Treated and Untreated Adolescents 5 Years After a Catastrophic Disaster. AJP. 2005;162(12):2302–2308. doi: 10.1176/appi.ajp.162.12.2302. [DOI] [PubMed] [Google Scholar]
- González-Sanguino C., Ausín B., Castellanos M.Á., Saiz J., López-Gómez A., Ugidos C., Muñoz M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect Dis. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn S.R., Charney D.S., Feder A. Understanding resilience: New approaches for preventing and treating PTSD. Exp. Neurol. 2016;284(Pt B):119–132. doi: 10.1016/j.expneurol.2016.07.002. [DOI] [PubMed] [Google Scholar]
- Horn S.R., Feder A. Understanding Resilience and Preventing and Treating PTSD. Harvard Rev. Psychiatry. 2018;26(3):158–174. doi: 10.1097/HRP.0000000000000194. [DOI] [PubMed] [Google Scholar]
- Hugo M., Declerck H., Fitzpatrick G., Severy N., Gbabai O.-B.-M., Decroo T., Van Herp M. Post-Traumatic Stress Reactions in Ebola Virus Disease Survivors in Sierra Leone. Emergency Med.: Open Access. 2015;05(06):1–4. doi: 10.4172/2165-7548.1000285. [DOI] [Google Scholar]
- Iacoviello B.M., Charney D.S. Psychosocial facets of resilience: implications for preventing posttrauma psychopathology, treating trauma survivors, and enhancing community resilience. Europ. J. Psychotraumatol. 2014;5(1):23970. doi: 10.3402/ejpt.v5.23970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kmett Danielson C., Macdonald A., Amstadter A.B., Hanson R., de Arellano M.A., Saunders B.E., Kilpatrick D.G. Risky Behaviors and Depression in Conjunction With—or in the Absence of—Lifetime History of PTSD Among Sexually Abused Adolescents. Child Maltreat. 2010;15(1):101–107. doi: 10.1177/1077559509350075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi I., Boarts J.M., Delahanty D.L. Polysomnographically measured sleep abnormalities in PTSD: A meta-analytic review. Psychophysiology. 2007;44(4):660–669. doi: 10.1111/j.1469-8986.2007.537.x. [DOI] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMANetw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebron-Milad K., Graham B.M., Milad M.R. Low Estradiol Levels: A Vulnerability Factor for the Development of Posttraumatic Stress Disorder. Biol. Psychiatry. 2012;72(1):6–7. doi: 10.1016/j.biopsych.2012.04.029. [DOI] [PubMed] [Google Scholar]
- Lee A.M., Wong J.G., McAlonan G.M., Cheung V., Cheung C., Sham P.C., Chu C.-M., Wong P.-C., Tsang K.W., Chua S.E. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can. J. Psychiatry. 2007;52(4):233–240. doi: 10.1177/2F070674370705200405. [DOI] [PubMed] [Google Scholar]
- Lee S., Chan L.Y.Y., Chau A.M.Y., Kwok K.P.S., Kleinman A. The experience of SARS-related stigma at Amoy Gardens. Soc. Sci. Med. 2005;61(9):2038–2046. doi: 10.1016/j.socscimed.2005.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.M., Kang W.S., Cho A.-R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei L., Huang X., Zhang S., Yang J., Yang L., Xu M. Comparison of Prevalence and Associated Factors of Anxiety and Depression Among People Affected by versus People Unaffected by Quarantine During the COVID-19 Epidemic in Southwestern China. Med. Sci. Monit. 2020;26 doi: 10.12659/MSM.924609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lepore, S. J., Revenson, T. A., 2006. Resilience and Posttraumatic Growth: Recovery, Resistance, and Reconfiguration.
- Levine S.Z., Laufer A., Stein E., Hamama-Raz Y., Solomon Z. Examining the relationship between resilience and posttraumatic growth: Resilience and Growth. J. Traum. Stress. 2009;22(4):282–286. doi: 10.1002/jts.20409. [DOI] [PubMed] [Google Scholar]
- Liang L., Gao T., Ren H., Cao R., Qin Z., Hu Y., Li C., Mei S. Post-traumatic stress disorder and psychological distress in Chinese youths following the COVID-19 emergency. J Health Psychol. 2020;25(9):1164–1175. doi: 10.1177/1359105320937057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C.H., Zhang E., Wong G.T.F., Hyun S., Hahm H.“. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290:113172. doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., Wu L., Sun Z., Zhou Y., Wang Y., Liu W. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luxton D.D., Skopp N.A., Maguen S. Gender differences in depression and PTSD symptoms following combat exposure. Depress. Anxiety. 2010;27(11):1027–1033. doi: 10.1002/da.20730. [DOI] [PubMed] [Google Scholar]
- Mak I.W.C., Chu C.M., Pan P.C., Yiu M.G.C., Chan V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry. 2009;31(4):318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak I.W.C., Chu C.M., Pan P.C., Yiu M.G.C., Ho S.C., Chan V.L. Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. Gen. Hosp. Psychiatry. 2010;32(6):590–598. doi: 10.1016/j.genhosppsych.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayou R.A., Ehlers A., Bryant B. Posttraumatic stress disorder after motor vehicle accidents: 3-year follow-up of a prospective longitudinal study. Behav. Res. Ther. 2002;40(6):665–675. doi: 10.1016/S0005-7967(01)00069-9. [DOI] [PubMed] [Google Scholar]
- Mikolajczak MoÏra, Roy E., Luminet O., de Timary P. Resilience and hypothalamic-pituitary-adrenal axis reactivity under acute stress in young men: Short Communication. Stress. 2008;11(6):477–482. doi: 10.1080/10253890701850262. [DOI] [PubMed] [Google Scholar]
- Naeem F., Ayub M., Masood K., Gul H., Khalid M., Farrukh A., Shaheen A., Waheed W., Chaudhry H.R. Prevalence and psychosocial risk factors of PTSD: 18months after Kashmir earthquake in Pakistan. J. Affect. Disord. 2011;130(1-2):268–274. doi: 10.1016/j.jad.2010.10.035. [DOI] [PubMed] [Google Scholar]
- Neria Y., Nandi A., Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol. Med. 2008;38(4):467–480. doi: 10.1017/S0033291707001353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris, F. H., Foster, J. D., Weisshaar, D. L., 2002. The epidemiology of gender differences in PTSD across developmental, societal, and research contexts.
- Oh W., Muzik M., McGinnis E.W., Hamilton L., Menke R.A., Rosenblum K.L. Comorbid trajectories of postpartum depression and PTSD among mothers with childhood trauma history: Course, predictors, processes and child adjustment. J. Affect. Disord. 2016;200:133–141. doi: 10.1016/j.jad.2016.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olff M., Langeland W., Draijer N., Gersons B.P. Gender differences in posttraumatic stress disorder. Psychol Bull. 2007;133(2):183–204. doi: 10.1037/0033-2909.133.2.183. [DOI] [PubMed] [Google Scholar]
- Picaza Gorrochategi M., Eiguren Munitis A., Dosil Santamaria M., Ozamiz Etxebarria N. Stress, Anxiety, and Depression in People Aged Over 60 in the COVID-19 Outbreak in a Sample Collected in Northern Spain. Am. J. Geriatric Psychiatry. 2020;28(9):993–998. doi: 10.1016/j.jagp.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pochard F., Darmon M., Fassier T., Bollaert P.E., Cheval C., Coloigner M., Merouani A., Moulront S., Pigne E., Pingat J., Zahar J.R., Schlemmer B., Azoulay E., French F.s.g. Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death. A prospective multicenter study. J Crit Care. 2005;20(1):90–96. doi: 10.1016/j.jcrc.2004.11.004. [DOI] [PubMed] [Google Scholar]
- Russo S.J., Murrough J.W., Han M.-H., Charney D.S., Nestler E.J. Neurobiology of resilience. Nat. Neurosci. 2012;15(11):1475–1484. doi: 10.1038/nn.3234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutten B.P.F., Hammels C., Geschwind N., Menne‐Lothmann C., Pishva E., Schruers K., den Hove D., Kenis G., Os J., Wichers M. Resilience in mental health: linking psychological and neurobiological perspectives. Acta Psychiatr. Scand. 2013;128(1):3–20. doi: 10.1111/acps.12095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeghi-Bazargani H., Maghsoudi H., Soudmand-Niri M., Ranjbar F., Mashadi-Abdollahi H. Stress disorder and PTSD after burn injuries: a prospective study of predictors of PTSD at Sina Burn Center, Iran. Neuropsychiatr. Dis. Treat. 2011;7:425. doi: 10.2147/NDT.S23041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprang G., Silman M. Posttraumatic Stress Disorder in Parents and Youth After Health-Related Disasters. Disaster Med. Public Health Prep. 2013;7(1):105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Su T., Lien T., Yang C., Su Y., Wang J., Tsai S., Yin J. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: A prospective and periodic assessment study in Taiwan. J. Psychiatr. Res. 2007;41(1-2):119–130. doi: 10.1016/j.jpsychires.2005.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang W., Hu T., Hu B., Jin C., Wang G., Xie C., Chen S., Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaishnavi S., Connor K., Davidson J.R.T. An abbreviated version of the Connor-Davidson Resilience Scale (CD-RISC), the CD-RISC2: Psychometric properties and applications in psychopharmacological trials. Psychiatry Res. 2007;152(2-3):293–297. doi: 10.1016/j.psychres.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waaktaar T., Torgersen S. How resilient are resilience scales? The Big Five scales outperform resilience scales in predicting adjustment in adolescents. Scand. J. Psychol. 2010;51(2):157–163. doi: 10.1111/j.1467-9450.2009.00757.x. [DOI] [PubMed] [Google Scholar]
- Weathers, F. W., Litz, B. T., Herman, D. S., Huska, J. A., Keane, T. M., 1993. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Annual convention of the international society for traumatic stress studies, San Antonio, TX,
- Weathers, F. W., Litz, B.T., Keane, T.M., Palmieri, P.A., Marx, B.P., Schnurr, P.P., 2013. The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov.
- Wu G., Feder A., Cohen H., Kim J.J., Calderon S., Charney D.S., Mathe A.A. Understanding resilience. Front. Behav. Neurosci. 2013;7:10. doi: 10.3389/fnbeh.2013.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu K.K., Chan S.K., Ma T.M. Posttraumatic stress after SARS. Emerg Infect Dis. 2005;11(8):1297–1300. doi: 10.3201/eid1108.041083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu K.K., Chan S.K., Ma T.M. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS) J. Traum. Stress. 2005;18(1):39–42. doi: 10.1002/jts.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yezli S., Khan A. COVID-19 social distancing in the Kingdom of Saudi Arabia: Bold measures in the face of political, economic, social and religious challenges. Travel Med. Infect. Dis. 2020;37:101692. doi: 10.1016/j.tmaid.2020.101692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaki A.M., van Boheemen S., Bestebroer T.M., Osterhaus A.D.M.E., Fouchier R.A.M. Isolation of a Novel Coronavirus from a Man with Pneumonia in Saudi Arabia. N Engl. J. Med. 2012;367(19):1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]