Abstract
Objective
To evaluate the effect of different demographic, clinical and social factors on diabetic patients' quality of life (QOL).
Research design and methods
A cross sectional study conducted on patients with type 2 diabetes who attended King Abdulaziz University Hospital outpatient clinics between February and March 2017. The patients were asked about sociodemographic data including age, sex, educational level, exercise history and marital status in addition to clinical data such as duration of diabetes, presence of comorbidities as well as medication history. The patients' QOL were assessed using EQ-5D-5L Arabic version.
Results
131 participants were included in the study with a median age 55 years old. Forty five percent of participants were male. Regarding EQ-5D scores, there were significant correlation with gender, exercise, hypertension, heart disease, marital status, educational level and duration of diabetes while there was a significant difference in EQ-VAS scores with respect to heart disease, level of education and duration of diabetes.
Conclusion
More attention needs to be given to the assessment of the QOL of diabetic patients and assessing the effect of different treatment modalities on improvement of patients’ QOL.
Keywords: Saudi Arabia, Diabetes, Quality of Life
1. Introduction
Diabetes mellitus is defined as disturbances of metabolism presented by chronic hyperglycemia which is due to either impaired insulin secretion or/and action (Kerner and Brückel, 2014). The number of diabetic patients is increasing rapidly; it is expected that by 2030, there will be a 69% increase in the number of adults with diabetes in developing countries and a 20% increase in developed countries (Shaw et al., 2010). Diabetes mellitus is associated with microvascular and macrovascular complications including retinopathy, nephropathy and cardiovascular and cerebrovascular events (Chawla et al., 2016)
The increased prevalence within a progressively aging population and the presence of chronic complications will significantly increase the use of healthcare products and services and will have a negative impact on healthcare costs and patients’ quality of life (QOL) (Mata-Cases et al., 2016). Patients who perceived higher levels of QOL have shown that they had better social support, acceptance of the seriousness and consequences of the disease, and had less difficulty in managing their diabetes (Chew et al., 2015). There is a rising attention towards patient’s QOL improvements rather than patient’s life longevity (Amelia et al., 2018, Brown, 2015) For diabetic patients the importance of developing special psychometric tools to measure QOL has been given specific attention and several tools were developed to evaluate the effect of diabetes as a disease; along with it’s complications on patients’ lives (Bradley and Speight, 2002, Trikkalinou et al., 2017). This study aimed to evaluate the QOL of Saudi patients living with diabetes using the EuroQOL- 5 Dimentions 5 levels (EQ-5D-5L), and associate the effect of several social and clinical factors on their QOL assessment scores.
2. Methods
2.1. Study design and participants
This was a cross-sectional study of data gathered from adult patients with type II diabetes who attended outpatient clinics at King Abdulaziz University Hospital, Jeddah, Saudi Arabia from February to March 2017. The study was approved by the Institutional Review Board (IRB) Committee of the College of Medicine, King Abdulaziz University Hospital.
2.2. Assessment of health related QOL
Data collection and questionnaire were carried out through face-to-face interviews with the patients. Patients were asked for permission before they were interviewed. During the interview patients were asked about sociodemographic data as such as age, sex, educational level, exercise history and marital status in addition to clinical data such as duration of diabetes, presence of comorbidities and medication history. The patients' QOL were assessed using the EuroQOL- 5 Dimentions 5 levels (EQ-5D-5L) Arabic version; which is a standardized instrument for measuring generic health (Herdman et al., 2011). The test includes patients' perception of their health status in terms of five dimensions: mobility (MO), self-care (SC), usual activities (UA), pain/discomfort (P/D) and anxiety/depression (A/D). Participants rate their level of severity for each dimension using 5 levels that range from not having a problem to having an extreme problem (Sakthong et al., 2015). Patient’s responses are combined to form a five-digit score; which corresponds to a EQ-5D-5L index value set. There is no population reference valuation set for Saudi Arabia so a population reference valuation set of Thailand was used based on the location (van Reenen and Janssen, 2015). The test also includes a visual analogue scale (VAS); where participants rate their general health status on the day of the interview on a scale from 0 to 100, zero being the worst health status and 100 being the best health status.
2.3. Statistical analysis
Statistical analysis was done using SPSS version 21. Categorical data were summarized as percentages while numerical data were summarized as medians and ranges. Normality test was done using the Kolmogorov-Smirnov (K-S) Test and the Shapiro-Wilk Test and have shown that the values of EQ-5D and EQ-VAS scores are non-parametric. Association between QOL scores with gender, smoking, exercise and comorbidities were done using Mann Whitney test while association with marital status, duration of diabetes and educational level were done using Kruskal Wallis test. P-values less than 0.05 were considered significant.
3. Results
The baseline characteristics of participants are presented in Table 1. Overall 131 diabetic patients participated in the questionnaire. The median age was 55 years old. Forty five percent of participants were male and only 15.3% were smokers. Most of the patients (76.3%) were married. Eighty-four patients reported having hypertension while 26 reported having heart disease. Others reported having asthma, osteoarthritis and kidney impairments. The percentage of item reporting for each EQ-5DL-5L dimension by age group are summarized in Table 2.
Table 1.
Demographic and baseline characteristics.
| Parameter | Value |
|---|---|
| Age | |
| Median (minimum–maximum) | 55 (22–85) |
| Gender: | |
| Male: number (%) | 59 (45) |
| Female: number (%) | 72 (55) |
| Marital status | |
| Single: number (%) | 7 (5.3) |
| Married: number (%) | 100 (76.3) |
| Divorced: number (%) | 6 (4.6) |
| Widow: number (%) | 18 (13.7) |
| Educational level: | |
| Illiterate: number (%) | 20 (15.3) |
| General education: number (%) | 72 (55) |
| High education: number (%) | 39 (29.7) |
| Smoking | |
| yes: number (%) | 20 (15.3) |
| No: number (%) | 111 (84.7) |
| Exercise | |
| yes: number (%) | 68 (51.9) |
| No: number (%) | 63 (49.1) |
| Duration of diabetes: | |
| Less than one year: number (%) | 11 (8.4) |
| From one to five years: number (%) | 35 (26.7) |
| More than five years: number (%) | 85 (64.9) |
| Hypertension | |
| Yes: number (%) | 47 (35.9) |
| No: number (%) | 84 (64.1) |
| Heart disease: | |
| Yes: number (%) | 26 (19.8) |
| No: number (%) | 105 (80.2) |
| Other comorbidities: | |
| Arthritis: number (%) | 7 (5.3) |
| Osteoarthritis: number (%) | 17 (13%) |
| Kidney impairment: number (%) | 14 (10.6) |
Table 2.
Percentage of the general population sample reporting levels 1–5 by dimension and by age group.
| AGE GROUPS |
||||||||
|---|---|---|---|---|---|---|---|---|
| EQ-5D DIMENSION | 18–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70+ | TOTAL | |
| MOBILITY | No problem | 71.43% | 55.56% | 45.45% | 55.56% | 50.00% | 50.00% | 52.67% |
| Slight | 28.57% | 22.22% | 27.27% | 35.56% | 38.46% | 18.18% | 30.53% | |
| Moderate | – | 22.22% | 18.18% | 4.44% | 7.69% | 27.27% | 12.21% | |
| Severe | – | – | 4.55% | 2.22% | 3.85% | 4.55% | 3.05% | |
| Extreme | – | – | 4.55% | 2.22% | – | – | 1.53% | |
| SELF CARE | No problem | 100.00% | 88.89% | 90.91% | 82.22% | 73.08% | 63.64% | 80.15% |
| Slight | – | 11.11% | 4.55% | 8.89% | 11.54% | 18.18% | 9.92% | |
| Moderate | – | – | 4.55% | 4.44% | 7.69% | 4.55% | 4.58% | |
| Severe | – | – | 0.00% | 0.00% | 0.00% | 4.55% | 0.76% | |
| Extreme | – | – | – | 4.44% | 7.69% | 9.09% | 4.58% | |
| USUAL ACTIVITY | No problem | 100.00% | 66.67% | 68.18% | 48.89% | 53.85% | 45.45% | 56.49% |
| Slight | – | 22.22% | 27.27% | 24.44% | 19.23% | 9.09% | 19.85% | |
| Moderate | – | 11.11% | – | 13.33% | 11.54% | 4.55% | 8.40% | |
| Severe | – | – | – | 2.22% | 3.85% | 9.09% | 3.05% | |
| Extreme | – | – | 4.55% | 11.11% | 11.54% | 31.82% | 12.21% | |
| PAIN / DISCOMFORT | No problem | 85.71% | 44.44% | 31.82% | 20.00% | 23.08% | 36.36% | 30.53% |
| Slight | 14.29% | 33.33% | 45.45% | 46.67% | 34.62% | 31.82% | 38.93% | |
| Moderate | – | 11.11% | 13.64% | 20.00% | 19.23% | 9.09% | 15.27% | |
| Severe | – | 11.11% | 4.55% | 4.44% | 15.38% | 13.64% | 8.40% | |
| Extreme | – | – | 4.55% | 8.89% | 7.69% | 9.09% | 6.87% | |
| ANXIETY/DEPRESSION | No problem | 71.43% | 55.56% | 45.45% | 55.56% | 50.00% | 50.00% | 52.67% |
| Slight | 28.57% | 22.22% | 27.27% | 35.56% | 38.46% | 18.18% | 30.53% | |
| Moderate | – | 22.22% | 18.18% | 4.44% | 7.69% | 27.27% | 12.21% | |
| Severe | – | – | 4.55% | 2.22% | 3.85% | 4.55% | 3.05% | |
| Extreme | – | – | 4.55% | 2.22% | – | – | 1.53% | |
*Within each dimension, (No problem) is considered level 1 and (Extreme) is considered level 5.
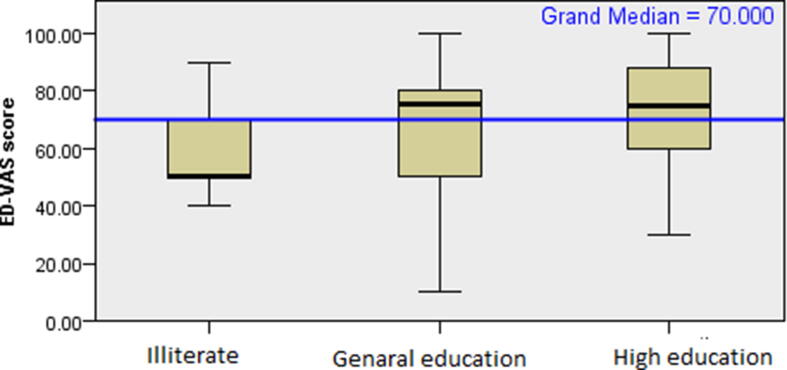
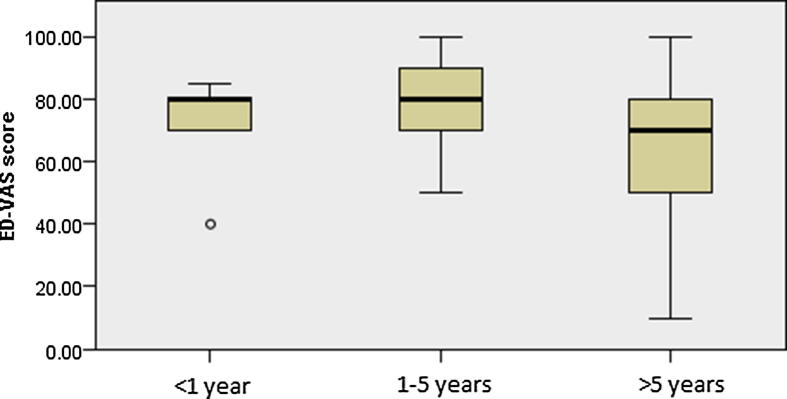
The association between EQ-VAS and EQ-5D scores with baseline characteristics and disease specific questionnaires is presented in Table 3, Table 4. With respect to the EQ-VAS, there was no significant difference in responses with respect to gender, smoking, exercise and hypertension while there was a significant difference in EQ-VAS scores between participants who had heart disease compared to those who don’t. EQ-VAS scores of illiterate participants were significantly different from those with general and high education. Also, EQ-VAS scores of patients who had diabetes for more than 5 years were significantly different from those who were more recently diagnosed with the disease (1–5 years). Regarding the EQ-5D scores, there were significant correlation with gender, exercise, hypertension, heart disease, marital status, educational level and duration of diabetes. The relationship between EQ-VAS and EQ-5D scores and educational level and duration of diabetes were represented in Fig. 1, Fig. 2, respectively.
Table 3.
Effect of gender, smoking, exercise, hypertension and heart disease on EQ-VAS and EQ-5D scores of diabetic patients.
| Parameter | EQ-VAS scores |
EQ-5D |
||
|---|---|---|---|---|
| Median (maximum-minimum) | p-value # | Median (maximum-minimum) | p-value # | |
| Gender Male Female |
70 (10–100) 72 (30–100) |
0.369 |
0.648 (−0.374–1) 0.588 (−0.105–1) |
0.024* |
| Smoking Yes No |
70 (40–95) 75 (10–100) |
0.342 |
0.705 (0.098–1) 0.604 (−0.374–1) |
0.092 |
| Exercise Yes No |
75 (40–100) 70 (10–100) |
0.072 |
0.663 (−0.374–1) 0.558 (−0.374–1) |
0.0003* |
| Hypertension Yes No |
70 (20–100) 75 (10–100) |
0.359 |
0.572 (−0.105–1) 0.648 (−0.374–1) |
0.001* |
| Heart disease Yes No |
60 (10–90) 76 (20–100) |
0.002* |
0.513 (−0.374–1) 0.617 (−0.374–1) |
0.004* |
#statistical test; Mann Whitney test.
*p-value < 0.05, significant.
Table 4.
Effect of marital status, educational level and duration of diabetes on EQ-VAS and EQ-5D scores of diabetic patients.
| EQ-VAS scores |
EQ-5D |
|||
|---|---|---|---|---|
| Parameter | Median (maximum-minimum) | p-value # | Median (maximum-minimum) | p-value # |
| Marital status Single Married Divorced Widow |
70 (30–100) 75 (10–100) 65 (50–95) 60 (40–100) |
0.521 |
1 (0.554–1) 0.617 (−0.374–1) 0.584 (0.079–1) 0.547 (−0.371–0.78) |
0.003*** |
| Educational level Illiterate General education High education |
50 (40–90) 75 (10–100) 75 (30–100) |
0.003* |
0.450 (−0.105–1) 0.618 (−0.374–1) 0.648 (−0.374–1) |
0.001**** |
| Duration of diabetes < 1 year From 1 to 5 years >5 years |
80 (40–85) 80 (50–100) 70 (10–100) |
0.001** |
0.677 (−0.105–1) 0.723 (0.040–1) 0.595 (−0.347–1) |
0.006***** |
#: statistical test; Kruskal Wallis test.
*p-value < 0.05, significant. Pairwise comparisons revealed significant difference between illiterate and general education participants and illiterate and high education participants.
**p-value < 0.05, significant. Pairwise comparisons revealed significant difference between participants with more than 5-year history of diabetes and those from 1 to 5-year history of diabetes.
***p-value < 0.05, significant. Pairwise comparisons revealed significant difference between widow-married, widow-single, divorced-single, married-single.
****p-value < 0.05, significant. Pairwise comparisons revealed significant difference between illiterate -general education and illiterate-high education.
*****p-value < 0.05, significant. Pairwise comparisons revealed significant difference between participant with more than 5-year history of diabetes and those with history of 1–5 years.
Fig. 1.
Effect of educational level on EQ-VAS scores of diabetic patients.
Fig. 2.
Effect of duration of diabetes on EQ-VAS scores of diabetic patients.
4. Discussion
Increasing attention is being given by health care professional to evaluate the QOL of diabetic patients (Bradley and Speight, 2002). Diabetes is a chronic disease that is known to cause considerable morbidity and mortality and has been reported to result in a lower QOL compared non-diabetic patients (Golicki et al., 2015). In fact, the decline in the QOL of diabetic patients over 5 a year period was found to be twice the decline among those without diabetes (Grandy and Fox, 2012).
In our study, diabetic females had lower QOL compared to males. This is in agreement with studies in other populations (Corrêa et al., 2017, Rodríguez-Almagro et al., 2018) and EQ-5D-3L (Cardoso et al., 2016, Hassali et al., 2016, Jin et al., 2018, Mata-Cases et al., 2016, Sakamaki et al., 2006). In addition, in Saudi Arabia, similar findings were obtained in Riyadh, Alkobar and Alqassim (Abdel-Gawad et al., 2002, Al-Shehri et al., 2008, Al Hayek et al., 2014, Almogbel, xxxx). A review on the gender differences in diabetic patients found that male patients were less depressed and anxious and overall living more effectively with the disease than females (Siddiqui et al., 2013). This is likely true for our population as well.
The current study demonstrated a significant association between the marital status and QOL of diabetic patients, where divorced, single and widowed patients had lower QOL scores than married. A systematic review on the effect of marital life on the QOL of diabetic patients reported similar findings where a better QOL was reported for married compared to nonmarried (single, widow) diabetics (Kiadaliri et al., 2013). This is in agreement with a study in Riyadh (Abdel-Gawad et al., 2002) However, another study in Riyadh reported that married diabetic patients had lower QOL than unmarried (Al-Shehri, 2014). This was explained by the higher responsibilities that were associated with marriage; which could add a burden to managing the disease itself. While this has not been examined in our study, the quality of marriage has been shown to play a role as well. Indeed, the American Diabetes Association examined the effect of marital status and quality measures on the glycemic control in insulin treated diabetics and found that quality of marriage affected the health related quality of life and adaptation to the disease itself (Trief et al., 2001). In addition, other studies reported that uncontrolled diabetes as a disease affected their everyday relationships and social experiences, with many patients expressing negative impacts on their social well-being (Vanstone et al., 2015).
Regarding the level of education, the current study has shown that low educational levels adversely affect patients' QOL. Illiterate patients have the worse QOL scores compared to those with higher educational levels. This is in agreement with numerous studies worldwide that demonstrate that increased patient education level among diabetic patients improves overall health outcomes including QOL (Alshayban and Joseph, 2020, Nielsen et al., 2016, Powers et al., 2016, Rodríguez-Almagro et al., 2018). In fact, Diabetes Self-management Education and Support (DSME/S) is a recognized act by the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics, that facilitates knowledge and necessary education and skills necessary for patient self-care (Powers et al., 2016).
Other factors that contribute to the poor QOL of diabetic patients in our study include comorbidities such as heart disease. It was reported from previous studies that cardiovascular disease negatively impacts the QOL of diabetic patients (de Visser et al., 2002, Wändell, 2005). Indeed, the presence of cardiovascular disease in diabetic patients goes way beyond negatively impacting quality of life, to increased risk of morbidity and mortality (Bauters et al., 2003, Savarese and Lund, 2017) Physical activity, is known to be key for the prevention and management of type 2 diabetes (Colberg et al., 2010). Our study as well as many others demonstrated that it also has a great impact on the QOL of diabetic patients (Cardoso et al., 2016, Çolak et al., 2015, Corrêa et al., 2017). It has been reported that exercising more than 3 h per week for one year significantly improved the patients' QOL (Jin et al., 2018).
Longer duration of diabetes was also associated with poor QOL for diabetic patients in our study. Not surprisingly, patients who had diabetes for more than 5 years tend to have lower health related QOL scores especially in the physical health domain (Almogbel, xxxx, Corrêa et al., 2017). It is likely that is a result of increased disease severity, which is known to negatively impact QOL of diabetic patients (Alshayban and Joseph, 2020, Scollan-Koliopoulos et al., 2013).
Despite the importance of the study, it was nonetheless limited by the small sample size of the participants. In, addition data collection was done from a single site. A multicenter data collection would represent comprehensive evaluation of the factors affecting the Saudi diabetic patients. Also, the tool used in the study EQ-5D-5L is not a specific tool for diabetic patients and hence, it can be affected by the presence of other diseases and comorbidities not only diabetes.
5. Conclusion
Several factors can affect the QOL of diabetic patients including age, gender, marital status, physical activity, presence of comorbidities and duration of diabetes. More attention needs to be given to the assessment of the QOL of diabetic patients and assessing the effect of different treatment modalities on improvement of patients' QOL.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
References
- Abdel-Gawad E.S., Braun N.M., Singh A., Wajdula J.S., Sato R. Quality of life In Saudis with diabetes. Saudi J. Disabil. 2002;8:163–168. [Google Scholar]
- Al-Shehri A.H., Taha A.Z., Bahnassy A.A., Salah M. Health-related quality of life in type 2 diabetic patients. Ann. Saudi Med. 2008;28:352–360. doi: 10.5144/0256-4947.2008.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Shehri, F.S., 2014. Quality of life among Saudi diabetics. J. Diabetes Mellit.
- Al Hayek A.A., Robert A.A., Al Saeed A., Alzaid A.A., Al Sabaan F.S. Factors associated with health-related quality of life among Saudi patients with type 2 diabetes mellitus: a cross-sectional survey. Diabetes Metab. J. 2014;38:220–229. doi: 10.4093/dmj.2014.38.3.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almogbel, E., n.d. Assessment of health-related quality of life among Saudi patients with type 2 diabetes mellitus in Qassim region—Saudi Arabia. Age (Omaha). 234, 68.
- Alshayban D., Joseph R. Health-related quality of life among patients with type 2 diabetes mellitus in Eastern Province, Saudi Arabia: A cross-sectional study. PLoS One. 2020;15:e0227573. doi: 10.1371/journal.pone.0227573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amelia R., Lelo A., Lindarto D., Mutiara E. Quality of life and glycemic profile of type 2 diabetes mellitus patients of Indonesian: a descriptive study. IOP Conf. Ser. Earth Environ. Sci. 2018;125:12171. doi: 10.1088/1755-1315/125/1/012171. [DOI] [Google Scholar]
- Bauters C., Lamblin N., Mc Fadden E.P., Van Belle E., Millaire A., de Groote P. Influence of diabetes mellitus on heart failure risk and outcome. Cardiovasc. Diabetol. 2003;2:1. doi: 10.1186/1475-2840-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley C., Speight J. Patient perceptions of diabetes and diabetes therapy: assessing quality of life. Diabetes. Metab. Res. Rev. 2002;18(Suppl 3):S64–9. doi: 10.1002/dmrr.279. [DOI] [PubMed] [Google Scholar]
- Brown G.C. Living too long: the current focus of medical research on increasing the quantity, rather than the quality, of life is damaging our health and harming the economy. EMBO Rep. 2015;16:137–141. doi: 10.15252/embr.201439518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardoso A.F., Cruz R., Queirós P., Santiago L., Ribeiro C.F., Ferreira P. Assessment of health-related quality of life using the EQ-5D-3L in individuals with type 2 diabetes mellitus. J. Diabetes Metab. Disord. Control. 2016;3:64. [Google Scholar]
- Chawla A., Chawla R., Jaggi S. Microvasular and macrovascular complications in diabetes mellitus: distinct or continuum? Indian J. Endocrinol. Metab. 2016;20:546. doi: 10.4103/2230-8210.183480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew B.-H., Mohd-Sidik S., Shariff-Ghazali S. Negative effects of diabetes-related distress on health-related quality of life: an evaluation among the adult patients with type 2 diabetes mellitus in three primary healthcare clinics in Malaysia. Health Qual. Life Outcomes. 2015;13:187. doi: 10.1186/s12955-015-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Çolak T.K., Acar G., Dereli E.E., Özgül B., Demirbüken İ., Alkaç Ç., Polat M.G. Association between the physical activity level and the quality of life of patients with type 2 diabetes mellitus. J. Phys. Ther. Sci. 2015;28:142–147. doi: 10.1589/jpts.28.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colberg S.R., Sigal R.J., Fernhall B., Regensteiner J.G., Blissmer B.J., Rubin R.R., Chasan-Taber L., Albright A.L., Braun B. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care. 2010;33:e147–e167. doi: 10.2337/dc10-9990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrêa, K., Gouvêa, G.R., Silva, M.A.V. da, Possobon, R. de F., Barbosa, L.F. de L.N., Pereira, A.C., Miranda, L.G., Cortellazzi, K.L., 2017. Qualidade de vida e características dos pacientes diabéticos. Cien. Saude Colet. 22, 921–930. [DOI] [PubMed]
- de Visser C.L., Bilo H.J.G., Groenier K.H., de Visser W., Jong Meyboom-de B. The influence of cardiovascular disease on quality of life in type 2 diabetics. Qual. life Res. an. Int. J. Qual. life Asp. Treat. care Rehabil. 2002;11:249–261. doi: 10.1023/a:1015287825660. [DOI] [PubMed] [Google Scholar]
- Golicki D., Dudzińska M., Zwolak A., Tarach J.S. Quality of life in patients with type 2 diabetes in Poland - comparison with the general population using the EQ-5D questionnaire. Adv. Clin. Exp. Med. Off. organ Wroclaw Med. Univ. 2015;24:139–146. doi: 10.17219/acem/38137. [DOI] [PubMed] [Google Scholar]
- Grandy S., Fox K.M. Change in health status (EQ-5D) over 5 years among individuals with and without type 2 diabetes mellitus in the SHIELD longitudinal study. Health Qual. Life Outcomes. 2012;10:99. doi: 10.1186/1477-7525-10-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassali M.A., Saleem F., Bashir S., Hashmi F., Aljadhey H. A cross-sectional assessment of health-related quality of life among type 2 diabetic patients in Pakistan. J. Pharm. Bioallied Sci. 2016;8:64. doi: 10.4103/0975-7406.171734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herdman M., Gudex C., Lloyd A., Janssen M.F., Kind P., Parkin D., Bonsel G., Badia X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L) Qual. life Res. 2011;20:1727–1736. doi: 10.1007/s11136-011-9903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin X., Liu G.G., Gerstein H.C., Levine M.A.H., Guan H., Li H., Xie F. Minimally important difference and predictors of change in quality of life in type 2 diabetes: A community-based survey in China. Diabetes. Metab. Res. Rev. 2018;34:e3053. doi: 10.1002/dmrr.3053. [DOI] [PubMed] [Google Scholar]
- Kerner W., Brückel J. Definition, classification and diagnosis of diabetes mellitus. Exp. Clin. Endocrinol. Diabetes Off. J., Ger. Soc. Endocrinol. [and] Ger Diabetes Assoc. 2014;122:384–386. doi: 10.1055/s-0034-1366278. [DOI] [PubMed] [Google Scholar]
- Kiadaliri A.A., Najafi B., Mirmalek-Sani M. Quality of life in people with diabetes: a systematic review of studies in Iran. J. Diabetes Metab. Disord. 2013;12:54. doi: 10.1186/2251-6581-12-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mata-Cases M., Casajuana M., Franch-Nadal J., Casellas A., Castell C., Vinagre I., Mauricio D., Bolíbar B. Direct medical costs attributable to type 2 diabetes mellitus: a population-based study in Catalonia, Spain. Eur. J. Heal. Econ. HEPAC Heal. Econ. Prev. care. 2016;17:1001–1010. doi: 10.1007/s10198-015-0742-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen H.B., Ovesen L.L., Mortensen L.H., Lau C.J., Joensen L.E. Type 1 diabetes, quality of life, occupational status and education level - A comparative population-based study. Diabetes Res. Clin. Pract. 2016;121:62–68. doi: 10.1016/j.diabres.2016.08.021. [DOI] [PubMed] [Google Scholar]
- Powers M.A., Bardsley J., Cypress M., Duker P., Funnell M.M., Fischl A.H., Maryniuk M.D., Siminerio L., Vivian E. Diabetes Self-management Education and Support in Type 2 Diabetes: A Joint Position Statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Clin. Diabetes. 2016;34:70–80. doi: 10.2337/diaclin.34.2.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Almagro J., García-Manzanares Á., Lucendo A.J., Hernández-Martínez A. Health-related quality of life in diabetes mellitus and its social, demographic and clinical determinants: A nationwide cross-sectional survey. J. Clin. Nurs. 2018;27:4212–4223. doi: 10.1111/jocn.14624. [DOI] [PubMed] [Google Scholar]
- Sakamaki H., Ikeda S., Ikegami N., Uchigata Y., Iwamoto Y., Origasa H., Otani T., Otani Y. Measurement of HRQL using EQ-5D in patients with type 2 diabetes mellitus in Japan. Value Heal. 2006;9:47–53. doi: 10.1111/j.1524-4733.2006.00080.x. [DOI] [PubMed] [Google Scholar]
- Sakthong P., Sonsa-Ardjit N., Sukarnjanaset P., Munpan W. Psychometric properties of the EQ-5D-5L in Thai patients with chronic diseases. Qual. life Res. Int. J. Qual. life Asp. Treat. Care Rehabil. 2015;24:3015–3022. doi: 10.1007/s11136-015-1038-z. [DOI] [PubMed] [Google Scholar]
- Savarese G., Lund L.H. Global public health burden of heart failure. Card. Fail. Rev. 2017;3:7. doi: 10.15420/cfr.2016:25:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scollan-Koliopoulos M., Bleich D., Rapp K.J., Wong P., Hofmann C.J., Raghuwanshi M. Health-related quality of life, disease severity, and anticipated trajectory of diabetes. Diabetes Educ. 2013;39:83–91. doi: 10.1177/0145721712467697. [DOI] [PubMed] [Google Scholar]
- Shaw J.E., Sicree R.A., Zimmet P.Z. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res. Clin. Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- Siddiqui M.A., Khan M.F., Carline T.E. Gender differences in living with diabetes mellitus. Mater. Sociomed. 2013;25:140. doi: 10.5455/msm.2013.25.140-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trief P.M., Himes C.L., Orendorff R., Weinstock R.S. The marital relationship and psychosocial adaptation and glycemic control of individuals with diabetes. Diabetes Care. 2001;24:1384–1389. doi: 10.2337/diacare.24.8.1384. [DOI] [PubMed] [Google Scholar]
- Trikkalinou A., Papazafiropoulou A.K., Melidonis A. Type 2 diabetes and quality of life. World J. Diabetes. 2017;8:120–129. doi: 10.4239/wjd.v8.i4.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Reenen, M., Janssen, B., 2015. EQ-5D-5L user guide: basic information on how to use the EQ-5D-5L instrument. Rotterdam EuroQol Res. Found
- Vanstone M., Rewegan A., Brundisini F., Dejean D., Giacomini M. Patient perspectives on quality of life with uncontrolled type 1 diabetes mellitus: a systematic review and qualitative meta-synthesis. Ont. Health Technol. Assess. Ser. 2015;15:1. [PMC free article] [PubMed] [Google Scholar]
- Wändell P.E. Quality of life of patients with diabetes mellitus an overview of research in primary health care in the Nordic countries. Scand. J. Prim. Health Care. 2005;23:68–74. doi: 10.1080/02813430510015296. [DOI] [PubMed] [Google Scholar]