Abstract.
Among the types of acute thyroiditis, subacute thyroiditis (SAT) is rare in children, and there is limited knowledge regarding its characteristics in pediatric cases. We present a case of SAT in a 6-yr-old boy who was brought to our hospital with high fever and pain in the front portion of the neck. Acute suppurative thyroiditis (AST), which is common in children, was suspected initially. Tenderness observed in the thyroid corresponded to a hypoechoic region on ultrasonography. The tenderness subsequently shifted to the isthmus, which was evident as a hypoechoic region on ultrasonography. Movement of hypoechoicity is typical of creeping thyroiditis, wherein the pain and tenderness can be unilateral or may start on one side and subsequently shift to the contralateral side after days or even weeks. Based on this characteristic and changes in laboratory parameters, the patient was diagnosed as a case of creeping thyroiditis. Improvement was observed in the patient without the use of anti-inflammatory drugs. At the 2-yr follow-up, the patient did not have thyrotoxicosis or relapse. Although AST is more prevalent than SAT in children, ultrasonography findings of creeping thyroiditis may be an important indicator for the diagnosis of SAT in pediatric patients.
Keywords: pediatric, subacute thyroiditis, ultrasonography, creeping thyroiditis
Introduction
Subacute thyroiditis (SAT) is thought to be caused by viral infection; however, the condition rarely occurs in children. Moreover , the clinical features of SAT in the pediatric population are not well-understood (1). Creeping thyroiditis, a condition in which pain and tenderness gradually shifts to the opposite lobe of the thyroid gland, is a feature of adult SAT (2, 3). In this report, we present a rare case of SAT in a young boy who experienced unilateral pain in the neck that shifted to the opposite side before resolving spontaneously.
Case Report
A previously healthy 6-yr-old boy with no family history of thyroid disorders presented with a 2-d history of high fever followed by pain in the front portion of the neck. He had mild throat pain that had persisted for a week before presentation.
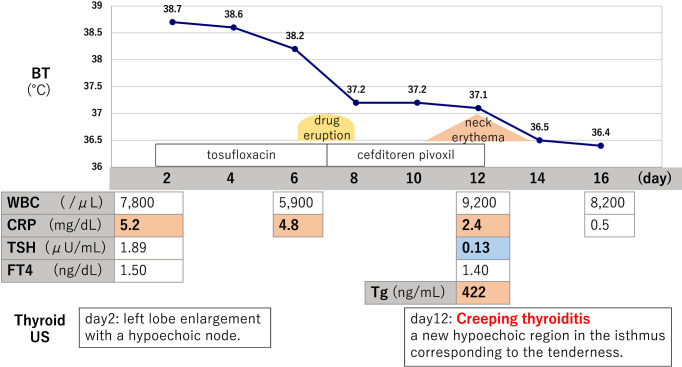
Physical examination revealed that his body temperature was 38.7ºC. Slight enlargement of the entire thyroid gland and left lobe tenderness were observed. Systemic examination was unremarkable. Laboratory tests showed normal white blood cell count (7,800 cells/μL; neutrophils, 73%) and elevated C-reactive protein (CRP) level (5.2 mg/dL). Thyroid function test revealed normal levels of free thyroxine (fT4) (1.5 ng/dL; normal range: 0.83–1.63 ng/dL) and thyroid stimulating hormone (TSH) (1.89 μU/mL; normal range: 0.38–4.31 μU/mL). Thyroid ultrasonography (US) revealed enlargement of the left lobe with a hypoechoic node (Fig. 1).
Fig. 1.
Ultrasonography (US) showing left lobe enlargement with a hypoechoic region (yellow arrow). The image on the right is an enlarged view of the left lobe.
Based on physical examination and results of laboratory investigations, a presumptive diagnosis of acute suppurative thyroiditis (AST) was made, and treatment was initiated with tosufloxacin. However, the fever persisted (38.6ºC), and cervical magnetic resonance imaging (MRI) taken on day 3 did not reveal any abscess or pyriform sinus fistula. On day 6, a skin rash appeared on the patient’s stomach, back, and thighs. Under the assumption that this was a drug-related eruption, tosufloxacin was discontinued and cefditoren pivoxil was prescribed. The patient became afebrile on day 7, and the skin rash disappeared a day later (day 8). However, on day 10, he developed anterior neck erythema, and the tenderness in the left lobe shifted to the median aspect. The patient had sensory sensitivity and mild irritability.
Laboratory tests on day 12 revealed a decline in CRP level (2.4 mg/dL) and TSH suppression (0.13 μU/mL). Moreover, although the level of fT4 was normal (1.5 ng/dL), and no anti-thyroid antibodies were detected, the level of thyroglobulin (Tg) was elevated (422 ng/mL; normal range: 0.0–33.7 ng/mL). US revealed a new hypoechoic region in the isthmus corresponding to the tenderness (Fig. 2). WBC count remained in the normal range during the acute phase (days 2–10). This information led us to conclude that the moving tenderness was creeping thyroiditis. Thus, we diagnosed the patient as a case of SAT. The prevailing physical status of the patient was good; therefore, we discontinued antibiotic therapy and continued follow-up without any additional treatment. The neck erythema resolved on day 14, and the patient remained afebrile. After 3 wk, CRP and TSH levels returned to normal. Tg level also normalized after 3 months, and no hypoechoic region was noted in the isthmus on follow-up US (Fig. 3). The patient remained healthy, and thyrotoxicosis or relapse was not observed two years after the onset. The clinical course of the acute phase is shown blow (Fig. 4).
Fig. 2.
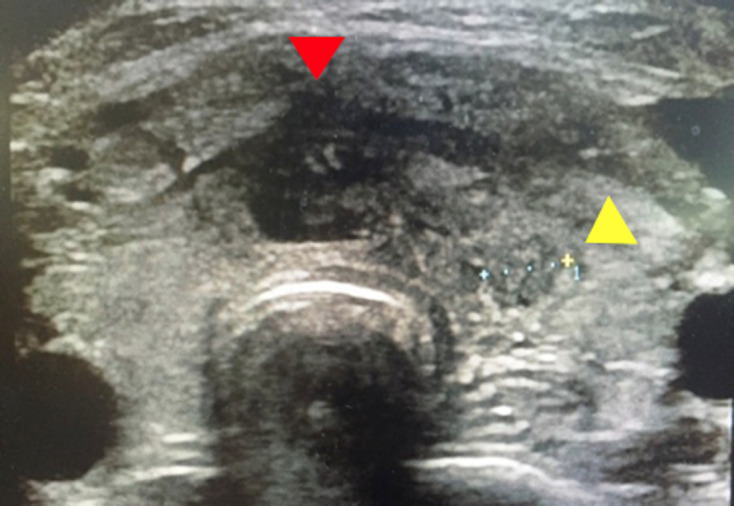
Ultrasonography (US) showing a new hypoechoic region in the isthmus that corresponded to the tenderness (red arrow), and reduction in the former hypoechoic region (yellow arrow).
Fig. 3.
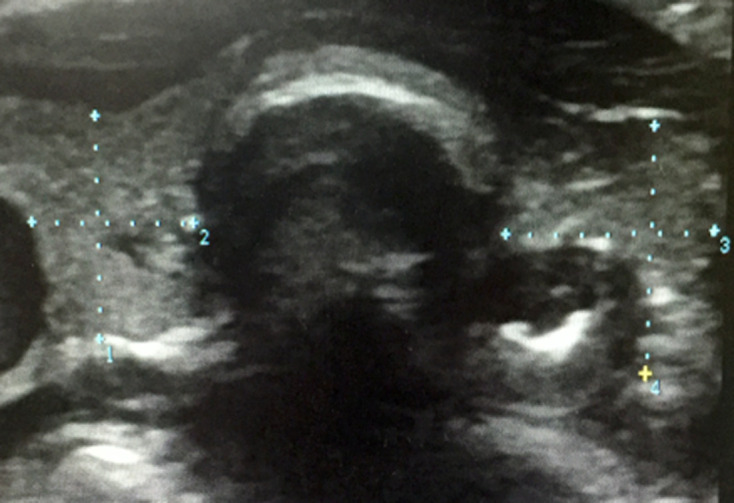
Ultrasonography (US) showing no abnormal findings. Both hypoechoic regions resolved after 3 mo.
Fig. 4.
Clinical course
Discussion
Patients with AST and SAT present with similar symptoms (fever, anterior cervical pain, thyroid swelling/tenderness) as well as similar imaging findings, thereby posing difficulties in distinguishing between the two conditions (4, 5). However, the two diseases differ considerably in severity. SAT is a self-limiting disease that often resolves spontaneously without the use of anti-inflammatory drugs in mild cases (6). In contrast, AST, which occurs more frequently in children, can be fatal, requiring antimicrobial therapy, drainage, and surgery (7). Delay in the diagnosis of AST can be dangerous. In one particular case, the initial diagnosis of SAT was changed to AST after abscess formation, which necessitated drainage, eventual removal, and intravenous broad-spectrum antibiotics (8). Thus, it is prudent to initiate antimicrobial therapy in ambiguous cases (6, 9), as was done in this case.
At the onset of moving tenderness, erythema appeared in the anterior neck region, which is generally suggestive of AST. Although there are no reports of erythema in patients with SAT, it resolved spontaneously a day after discontinuation of antimicrobial therapy, which does not support the finding of AST. In addition, cervical MRI taken on day 3 did not reveal any abscess or pyriform sinus fistula. US findings of AST are usually unifocal, while the spread to multiple lobes is characteristic of SAT (5). Thus, we judged the US findings to be consistent with that of SAT.
We diagnosed this patient as a case of SAT considering the painful goiter swelling, hypoechoic area within the thyroid consistent with the tenderness, elevated CRP level, moving tenderness, thyrotoxicosis, and antecedent upper airway symptoms. Usually, suppressed TSH and elevated fT4 levels are observed in thyrotoxicosis; however, fT4 level was normal in the present case. The American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis states that SAT is associated with mild thyrotoxicosis and elevated fT4 level may or may not be observed (10).
Another method to distinguish between AST and SAT was outlined by Ogawa et al., who suggested that the features of AST include leukocytosis and the absence of thyrotoxicosis (1). We diagnosed our patient as a case of SAT considering the absence of leukocytosis and the presence of mild thyrotoxicosis.
A study reported that 15.4% of the adult patients with SAT had findings of creeping thyroiditis (3). To the best of our knowledge, there are no reports of creeping thyroiditis in pediatric patients with SAT; therefore, the present case may be considered rare. Although there is no significant difference in the symptoms of SAT between adults and children (1), a possible reason why creeping thyroiditis is rarely reported in children may be that they cannot accurately describe changes in the location of tenderness in the thyroid gland due to fever and/or sore throat. Therefore, repeated US is considered an important objective indicator for diagnosis.
This report has some limitations. First, the causative virus of SAT was not identified. Second, we cannot conclusively state that all cases of childhood SAT would show the same symptoms as those observed in this patient. The incidence of SAT in children remains unclear, and further studies are required to identify the incidence and clinical features of SAT in the pediatric population.
Conclusion
In conclusion, although AST with pyriform sinus fistula is more common in children than SAT, moving tenderness and corresponding US findings may provide useful information for the diagnosis of SAT in the pediatric population. Thus, we suggest that careful physical examination of the neck and repeated thyroid US should be performed to identify creeping thyroiditis, which is one of the features of SAT.
Declaration of conflict of interests
None of the authors have any potential conflicts of interest to declare that are relevant to this report.
References
- 1.Ogawa E, Katsushima Y, Fujiwara I, Iinuma K. Subacute thyroiditis in children: patient report and review of the literature. J Pediatr Endocrinol Metab 2003;16: 897–900. doi: 10.1515/JPEM.2003.16.6.897 [DOI] [PubMed] [Google Scholar]
- 2.Guideline for the diagnosis of subacute thyroiditis (acute phase) [homepage on the internet]. Japan: Japan Thyroid Association, Inc. Available from: http://www.japanthyroid.jp/doctor/guideline/english.html#akyuu.
- 3.Arao T, Okada Y, Torimoto K, Kurozumi A, Narisawa M, Yamamoto S, et al. Prednisolone dosing regimen for treatment of subacute thyroiditis. J UOEH 2015;37: 103–10. doi: 10.7888/juoeh.37.103 [DOI] [PubMed] [Google Scholar]
- 4.Bilbao NA, Kaulfers AD, Bhowmick SK. Subacute thyroiditis in a child. AACE Clin Case Rep 2019;5: e184–6. doi: 10.4158/ACCR-2018-0211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Masuoka H, Miyauchi A, Tomoda C, Inoue H, Takamura Y, Ito Y, et al. Imaging studies in sixty patients with acute suppurative thyroiditis. Thyroid 2011;21: 1075–80. doi: 10.1089/thy.2010.0366 [DOI] [PubMed] [Google Scholar]
- 6.Volta C, Carano N, Street ME, Bernasconi S. Atypical subacute thyroiditis caused by Epstein-Barr virus infection in a three-year-old girl. Thyroid 2005;15: 1189–91. doi: 10.1089/thy.2005.15.1189 [DOI] [PubMed] [Google Scholar]
- 7.Paes JE, Burman KD, Cohen J, Franklyn J, McHenry CR, Shoham S, et al. Acute bacterial suppurative thyroiditis: a clinical review and expert opinion. Thyroid 2010;20: 247–55. doi: 10.1089/thy.2008.0146 [DOI] [PubMed] [Google Scholar]
- 8.Szabo SM, Allen DB. Thyroiditis. Differentiation of acute suppurative and subacute. Case report and review of the literature. Clin Pediatr (Phila) 1989;28: 171–4. doi: 10.1177/000992288902800403 [DOI] [PubMed] [Google Scholar]
- 9.Al Maawali A, Al Yaarubi S, Al Futaisi A. An infant with cytomegalovirus-induced subacute thyroiditis. J Pediatr Endocrinol Metab 2008;21: 191–3. doi: 10.1515/JPEM.2008.21.2.191 [DOI] [PubMed] [Google Scholar]
- 10.Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, et al. 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid 2016;26: 1343–421. doi: 10.1089/thy.2016.0229 [DOI] [PubMed] [Google Scholar]