Abstract
Objective
Obesity has been linked to cardiovascular disease, diabetes, and osteoarthritis. Obesity and overweight pose a serious threat to human health, with an estimated 190 million overweight and obese people worldwide. Thus, we investigated the influence of certain eating habits on weight among Chinese college students.
Methods
We conducted a cross-sectional survey of 536 college students in Shijiazhuang, China. The survey included questions about eating habits. We analyzed the relationship between participants’ responses and obesity.
Results
Sex, residence, speed of eating, number of meals eaten per day, and a diet high in sugar were found to be correlated with obesity. Our results suggest that increasing the number of meals per day, slowing down the pace of eating, and reducing the intake of high-sugar foods have potential benefits for reducing obesity among college students.
Conclusions
In the present study, we found that some dietary habits are related to the occurrence of obesity among college-aged individuals.
Keywords: Diet, eating habits, obesity, college students, cross-sectional survey, China
Introduction
Obesity is a common metabolic disease that involves the pathological state of excessive accumulation of adipose tissue, which can be damaging to human health. In the past few decades, the number of obese individuals has increased worldwide and obesity has become an epidemic.1 There are more than 190 million overweight and obese people globally. Compared with 1980, the number of obese individuals has doubled.2 There are 9 million adolescents in the United States with obesity. This has led to a substantially increased prevalence of cardiovascular and cerebrovascular diseases, type 2 diabetes, and osteoarthritis in adolescents, seriously affecting their physical and mental health.3,4 Factors involved in adolescent obesity cannot be ignored, such as the contribution of genes and metabolic diseases.5 However, changes in social culture represent another important factor. Social and economic development have resulted in a large number of fast food sources becoming easily available to teenagers, resulting in excessive energy intake.6 In addition, increased social activities among younger people have led to declining consumption and the associated benefits of a healthy family diet.7 Among sociocultural lifestyle changes, unhealthy eating patterns are a main reasons for the increase in obesity worldwide.8 It has been proven that less frequent consumption of fruits and vegetables and excessive intake of drinks high in sugar content as well as fast foods directly affect body mass index (BMI).9 However, the role of multiple dietary preferences related to the incidence of obesity among college students, an important group of young people, has not previously been studied.
We administered a questionnaire to college students in China. We queried their dietary habits and preferences via the survey, and then explored the relationship between students’ responses and their BMI. We aimed to identify eating habits related to weight and to then use this information to improve unhealthy eating habits and some obesity risk factors common among college students. This study provides new insights that may be helpful in exploring the relationship between dietary habits and obesity in our target age group. Our results may provide a scientific basis for interventions related to eating habits that can help to reduce and prevent obesity among college students.
Methods
Participants
Our cross-sectional study was conducted at Hebei Medical University in Shijiazhuang, the capital of Hebei Province in China. From August to September 2017, we recruited students at Hebei Medical University. The inclusion criteria for participants were Chinese college students between the ages of 18 and 25 years. Exclusion criteria included chronic diseases such as diabetes and endocrine diseases (e.g., Cushing syndrome or vacuolar sella) and long-term use of oral medication affecting body weight (e.g., estrogen or glucocorticoids). All participants gave their informed consent for inclusion before participating in the study, and they provided physical examination reports from within the previous 1 year. This study was conducted in accordance with the Declaration of Helsinki, and the study protocol was approved by the Ethics Committee of Hebei Medical University. Participants were provided with a fact sheet and instructed to follow the survey guidelines. A total of 551 questionnaires were collected, with a participation rate of 91.8% (551/600). After consulting the physical examination reports of participants, questionnaires completed by non-Chinese college students and individuals with chronic diseases were excluded. The remaining questionnaires were considered valid and were included in the study.
Anthropometric measurement
BMI is useful for estimating body fat and is calculated by dividing an individual’s weight (kg) by their height in meters squared (m2). Height and weight were measured during physical examinations. Height was measured using a portable rangefinder to the nearest 1 cm and weight was measured with a calibrated scale to the nearest 0.1 kg. According to World Health Organization definitions, individuals are classified as underweight with BMI <18.5 kg/m2, normal weight with BMI between 18.5 and 24.9 kg/m2, and overweight with BMI ≥25 kg/m2.
Self-administered questionnaire
We collected participant information using a self-administered questionnaire. Survey questions included general information: class, name, student number, dormitory number, region of residence, and sex; eating habits: speed at which meals are eaten (slow, normal, slightly fast, fast), number of times participants eat per day (twice, three times, four times, more than four times), dining at regular times (yes, no), eating breakfast (yes, no), excessive food consumption resulting in abdominal distension or discomfort (yes, no), eating snacks at night (never, once or twice a week, three to six times a week, every day), consuming high-fat foods (never, once or twice a week, three to six times a week, every day), consuming fruits and vegetables (never, a small amount, a normal amount), eating dessert (never, once or twice a week, three to six times a week, every day), drinking sugar-sweetened beverages (never, one or two servings a week, three to six servings a week, every day), exercising regularly (never, less than 1 hour per week, 1–2 hours per week, daily), and consuming alcohol (never, less than one drink per week, one or two drinks per week, more than three drinks per week).
Statistical analysis
All data were entered into a spreadsheet by the researcher and examined for validity. All statistical analyses were performed using IBM SPSS version 23.0 (IBM, Beijing, China). Measurement data are expressed as mean ± standard deviation. Pearson’s chi-squared test was used to investigate the relationship between participants’ general characteristics, dietary habits, and BMI. The alpha value was set to 0.05 for all tests.
Results
Participant characteristics
Among a total 536 participants included in this study, 257 male (22.07 ± 3.42, 47.9%) and 279 female (21.10 ± 2.73, 52.1%). Participants were age 17 to 22 years, with 254 (21.98 ± 3.46, 47.4%) from urban areas and 282 (21.19 ± 2.71, 52.6%) from rural areas. In terms of college grade, 67 were freshmen (22.41 ± 3.38, 12.5%), 202 were sophomores (21.25 ± 2.74, 37.7%), 177 were juniors (21.65 ± 3.21, 33.0%), and 90 were seniors (21.46 ± 3.41, 16.8%). Sixty-seven (17.61 ± 0.76, 12.5%) participants were underweight, 396 (21.14 ± 1.69, 73.9%) were normal weight, and 73 (27.48 ± 2.19, 13.6%) were overweight. Value in parentheses are the mean BMI ± standard deviation and rates are the proportion in each group. Participants from urban areas had a higher BMI (p = 0.019) than those from rural areas.
Relationship between BMI, pace of eating, meal frequency, and consumption of sugary foods
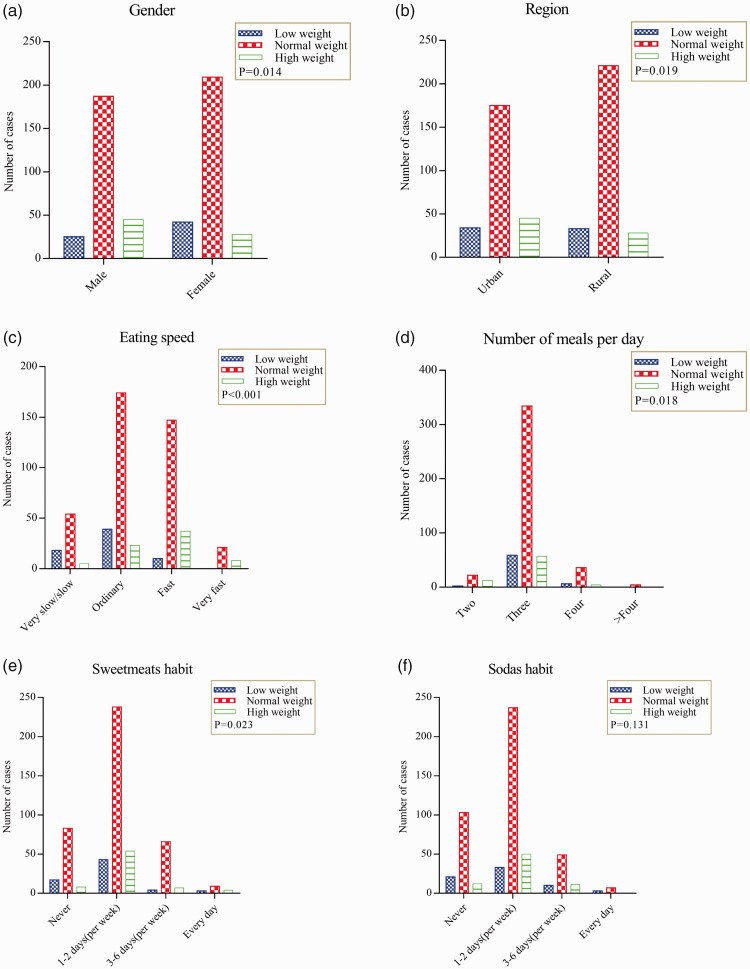
We analyzed the relationship between BMI and participants' eating habits and found that sex, residence, eating speed, daily meal frequency, habits of consuming sweets, and the number of sugar-sweetened beverages consumed per week were related to BMI. The mean levels for sex (Figure 1a), residence (Figure 1b), eating speed (Figure 1c), daily meal frequency (Figure 1d), high-sugar diet (Figure 1e), and drinking sugary beverages (Figure 1f) are depicted according to different BMI categories. Our results indicated that the number of meals eaten per day was negatively correlated with BMI (P = 0.018). Consuming a high-sugar diet was positively correlated with BMI (P = 0.023) but the effect on BMI was relatively small. Eating speed showed a significant positive correlation with BMI (P < 0.001).
Figure 1.
(a) Male and female students, according to body mass index (BMI). (b) Urban and rural residents, according to maximum weight. (c) BMI, according to eating speed. (d) BMI, according to meal frequency. (e) Weekly consumption of sweets among participants, according to BMI. (f) Weekly consumption of sugar-sweetened beverages among participants, according to BMI.
Discussion
In the present study, we conducted a questionnaire survey to assess the weight status of college students in China. Based on the results, we explored the influence of certain eating habits on the likelihood of being overweight. Shan provided a preliminary description, and we conducted a further analysis of that research.10 We revealed several main findings. First, we found that participants’ sex and region of residence affected BMI. Second, the number of meals eaten per day was negatively correlated with BMI. Third, the frequency of eating foods high in sugar content, and especially the speed at which meals are consumed, were positively correlated with BMI.
Sex increases the risk of obesity. Sex hormones, specifically regulated by related genes on the X chromosome, have an important role in maintaining energy balance.11 Participants from urban areas had a higher BMI than those from rural areas. Regarding the obvious regional differences in BMI, individuals from urban areas are more inclined to smoke and drink alcohol than those from rural regions. In addition, rural residents are more likely to attain levels of physical activity recommended by the World Health Organization than urban residents. Moreover, the intake of sweet or sugary drinks among urban residents is higher than that among residents from rural areas.12 Thus, individuals from urban areas tend to have greater energy intakes than rural residents, which may lead to the regional differences in BMI identified in our study.
The normal feasting–hunger cycle is the primary way that human physiological and metabolic balance is maintained. Satiety and appetite are affected by meal frequency, suggesting that appropriate meal frequency may help in reducing obesity.13 As an individual eats increasingly more, the thermal effect of the consumed food is considerable, resulting in a continuous increase in the body’s metabolic rate.14 These results of past studies are consistent with those of our investigation. Meal frequency can also affect gut microbes. Intestinal microorganisms indirectly affect leptin secretion by influencing circadian rhythms, which take part in the development of obesity.15,16 Irregular eating frequency also leads to differences in leptin and ghrelin secretion, reducing energy metabolism and increasing caloric intake.17
Eating sweets and desserts has a role in obesity through affecting hormones. Excessive consumption of sweet foods can substantially increase insulin resistance.18 On the one hand, the binding between insulin and its receptors on dopamine neurons is reduced, and the feeding regulation function of dopamine is weakened.19 On the other hand, overconsumption of sweets may lead to disorders of motivational behavior and reward-related mechanisms in individuals who are obese.20 In addition, dopamine activity and receptor expression are inhibited, affecting normal dietary regulation.21 Fructose is an indispensable form of sugar that can stimulate the nervous and hedonic responses of the brain and induce leptin resistance.22 However, our study findings showed the effect of consuming excessive sweets on obesity to be limited, which may be related to weak roles of insulin resistance and intestinal microorganisms in obesity.
Meal consumption speed was positively correlated with obesity, which may be linked to a number of factors. First, eating slowly means longer chewing time, which increases satiety and reduces excess energy intake.23 Second, eating slowly may reduce intestinal digestive enzyme activity and as a result, may reduce food digestion and absorption. In addition, with extended mealtimes, the brain centers will continuously respond to visual information, considerably enhancing the food intake memory function and reducing the subsequent intake of food.24 Recent research also suggests that obesity and endocrine hormones are closely related. Feeding behavior is often accompanied by olfactory and other physiological signals, which increase food intake by stimulating the dopaminergic circuit.25 The initial stage of the gastrointestinal reflex enables dopamine neurons to regulate eating behavior via the neurohumoral reflex. Spending a long time eating can lead to loss of control of this regulation mechanism, which destroys the normal feeding pattern.26 Insulin secretion in plasma is pulsed to coincide with food intake. Slowing down the rate of eating is beneficial to insulin secretion. In addition to lowering blood sugar levels, insulin can pass through the blood–brain barrier and bind to insulin receptors on dopamine neurons, increasing the release of dopamine from these neurons.19
We also found that eating at a normal speed and at a slightly faster speed were more frequent in the normal-weight group. Eating at a normal speed and slightly fast may lead to a difference in the degree of intervention by endocrine hormones related to eating, such as insulin and dopamine. Eating at a normal speed is conducive to maintenance of energy homeostasis by endocrine hormones and eating at a slightly faster speed is obviously conducive to positively increasing BMI. Surprisingly, we found that a smaller proportion of individuals with normal weight ate slowly than those who ate at a normal speed. There are several possible reasons for this finding. First, eating at a slow speed may be related to dissatisfaction with the taste of the food consumed at mealtimes, resulting in increased snacking between meals.27 Second, eating at a normal speed may be the set-point for the release of obesity-related endocrine hormones. Slow and fast eating speeds may interfere with the release of endocrine hormones and affect an individual’s weight.
Strengths and limitations of this study
After analyzing the relevant literature in relation to our study findings, we can conclude that meal speed,23 eating frequency,28 consuming a high-sugar diet,29 and an individual’s sex30 are all related to obesity. However, our study has some limitations. First, causality cannot be determined using a cross-sectional study design; for this, prospective and interventional studies are needed. Second, individuals possess a wide variety of eating habits, and we could not include them all in the present investigation. Finally, our research participants were students at Hebei Medical University in Shijiazhuang between the ages of 17 and 22 years; therefore, our study population does not represent the general population across all age groups in China. Moreover, we examined the relationship between the speed and frequency of eating meals on obesity, but we did not investigate the roles of energy intake per meal or total daily energy intake.31 Finally, the methods used to collect behavioral data may introduce the risk of bias.
Conclusions
In this study, we explored the relationship between certain eating habits and the risk of obesity among Chinese college students. Our results suggested that eating meals more frequently, slowing down the speed of eating, and reducing the intake of sweets and desserts may have potential benefits for reducing obesity among college students. Our findings provide some useful information for interventions to prevent the development of obesity and reduce the incidence of obesity-related diseases, which will have positive effects for individuals and their families. Our findings provide a scientific basis for reducing overweight and obesity among college students, as well as new ideas for studying the relationship between dietary habits and obesity in other age groups.
Acknowledgments
We thank Hui-bin Liu (Hebei Medical University) for his assistance with the statistical analysis and suggestions during the submission process.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author contributions
Meng-lei Hao and Qi-Xie were the main contributors to the writing and submission of the manuscript. Ling-bing Meng and Min-Lei made substantial contributions to the study’s conception. Yong Qiu and Xiao-qin Zuo provided assistance and suggestions during the submission process. Qiang-Wang, Na-Zhang, and Peng Guo obtained and analyzed the data. All authors read and approved the final manuscript.
ORCID iD
References
- 1.Vecchié A, Dallegri F, Carbone F, et al. Obesity phenotypes and their paradoxical association with cardiovascular diseases. Eur J Intern Med 2018; 48: 6–17. [DOI] [PubMed] [Google Scholar]
- 2.Saltiel AR, Olefsky JM. Inflammatory mechanisms linking obesity and metabolic disease. J Clin Invest 2017; 127: 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ladhani M, Craig JC, Irving M, et al. Obesity and the risk of cardiovascular and all-cause mortality in chronic kidney disease: a systematic review and meta-analysis. Nephrol Dial Transplant 2017; 32: 439–449. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Fryar CD, Hales CM, et al. Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013-2016. JAMA 2018; 319: 2410–2418. DOI: 10.1001/jama.2018.5158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ling C, Rönn T. . Epigenetics in human obesity and type 2 diabetes. Cell Metab 2019; 29: 1028–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ebbeling CB, Sinclair KB, Pereira MA, et al. Compensation for energy intake from fast food among overweight and lean adolescents. JAMA 2004; 291: 2828–2833. DOI: 10.1001/jama.291.23.2828. [DOI] [PubMed] [Google Scholar]
- 7.Shier V, Nicosia N, Datar A. Neighborhood and home food environment and children's diet and obesity: evidence from military personnel's installation assignment. Soc Sci Med 2016; 158: 122–131. DOI: 10.1016/j.socscimed.2016.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wellington N, Shanmuganathan M, de Souza RJ, et al. Metabolic trajectories following contrasting prudent and western diets from food provisions: identifying robust biomarkers of short-term changes in habitual diet. Nutrients 2019; 11: pii: E2407. DOI: 10.3390/nu11102407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khan MMA, Karim M, Islam AZ, et al. Prevalence of overweight and obesity among adolescents in Bangladesh: do eating habits and physical activity have a gender differential effect? J Biosoc Sci 2019; 51: 843–856. [DOI] [PubMed] [Google Scholar]
- 10.Shan MJ, Zou YF, Guo P, et al. Systematic estimation of BMI: a novel insight into predicting overweight/obesity in undergraduates. Medicine (Baltimore) 2019; 98: e15810. DOI: 10.1097/md.0000000000015810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang C, Xu Y. Mechanisms for sex differences in energy homeostasis. J Mol Endocrinol 2019; 62: R129–R143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Price AJ, Crampin AC, Amberbir A, et al. Prevalence of obesity, hypertension, and diabetes, and cascade of care in sub-Saharan Africa: a cross-sectional, population-based study in rural and urban Malawi. Lancet Diabetes Endocrinol 2018; 6: 208–222. DOI: 10.1016/s2213-8587(17)30432-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kerksick CM, Arent S, Schoenfeld BJ, et al. International society of sports nutrition position stand: nutrient timing. J Int Soc Sports Nutr 2017; 14: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vilela S, Correia D, Severo M, et al. Eating frequency and weight status in Portuguese children aged 3–9 years: results from the cross-sectional National Food, Nutrition and Physical Activity Survey 2015–2016. Public Health Nutr 2019; 22: 2793–2802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Voigt RM, Forsyth CB, Green SJ, et al. Circadian rhythm and the gut microbiome. Int Rev Neurobiol 2016; 131: 193–205. [DOI] [PubMed] [Google Scholar]
- 16.Pan W, Kastin AJ. Leptin: a biomarker for sleep disorders? Sleep Med Rev 2014; 18: 283–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dashti HS, Scheer FA, Jacques PF, et al. Short sleep duration and dietary intake: epidemiologic evidence, mechanisms, and health implications. Adv Nutr 2015; 6: 648–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jung CH, Choi KM. Impact of high-carbohydrate diet on metabolic parameters in patients with type 2 diabetes. Nutrients 2017; 9: pii: E322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fordahl SC, Jones SR. High-fat-diet-induced deficits in dopamine terminal function are reversed by restoring insulin signaling. ACS Chem Neurosci 2017; 8: 290–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edwin Thanarajah S, Iglesias S, Kuzmanovic B, et al. Modulation of midbrain neurocircuitry by intranasal insulin. Neuroimage 2019; 194: 120–127. [DOI] [PubMed] [Google Scholar]
- 21.Jones KT, Woods C, Zhen J, et al. Effects of diet and insulin on dopamine transporter activity and expression in rat caudate‐putamen, nucleus accumbens, and midbrain. J Neurochem 2017; 140: 728–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Isganaitis E, Lustig RH. Fast food, central nervous system insulin resistance, and obesity. Arterioscler Thromb Vasc Biol 2005; 25: 2451–2462. [DOI] [PubMed] [Google Scholar]
- 23.Shah M, Copeland J, Dart L, et al. Slower eating speed lowers energy intake in normal-weight but not overweight/obese subjects. J Acad Nutr Diet 2014; 114: 393–402. [DOI] [PubMed] [Google Scholar]
- 24.Robinson E, Aveyard P, Daley A, et al. Eating attentively: a systematic review and meta-analysis of the effect of food intake memory and awareness on eating. Am J Clin Nutr 2013; 97: 728–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thanarajah SE, Backes H, DiFeliceantonio AG, et al. Food intake recruits orosensory and post-ingestive dopaminergic circuits to affect eating desire in humans. Cell Metab 2019; 29: 695–706.e4. [DOI] [PubMed] [Google Scholar]
- 26.Boekhoudt L, Roelofs TJM, de Jong JW, et al. Does activation of midbrain dopamine neurons promote or reduce feeding? Int J Obes (Lond) 2017; 41: 1131–1140. [DOI] [PubMed] [Google Scholar]
- 27.Koopman KE, Caan MW, Nederveen AJ, et al. Hypercaloric diets with increased meal frequency, but not meal size, increase intrahepatic triglycerides: a randomized controlled trial. Hepatology 2014; 60: 545–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dallacker M, Hertwig R, Mata J. The frequency of family meals and nutritional health in children: a meta-analysis. Obes Rev 2018; 19: 638–653. [DOI] [PubMed] [Google Scholar]
- 29.van Dam RM, Rimm EB, Willett WC, et al. Dietary patterns and risk for type 2 diabetes mellitus in U.S. men. Ann Intern Med 2002; 136: 201–209. [DOI] [PubMed] [Google Scholar]
- 30.Depner CM, Melanson EL, Eckel RH, et al. Ad libitum weekend recovery sleep fails to prevent metabolic dysregulation during a repeating pattern of insufficient sleep and weekend recovery sleep. Curr Biol 2019; 29: 957–967.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fock KM, Khoo J. Diet and exercise in management of obesity and overweight. J Gastroenterol Hepatol 2013; 28: 59–63. [DOI] [PubMed] [Google Scholar]