Abstract
Objective
We evaluated hybrid nonbridging external fixation (NBEF) supplemented by K-wires as an effective and safe treatment option for osteoporotic distal radius fractures (DRFs) in a retrospective case series.
Methods
Sixteen extra-articular and one intra-articular DRF were treated by NBEF from 2016 to 2018 (mean patient age, 61.8 years; 15 women, 1 man). Radiographic parameters (volar tilt, radial inclination, and ulnar variance), range of motion, grip power, the visual analog scale score, and the Disabilities of the Arm, Shoulder and Hand (DASH) score were assessed at 4 weeks, 6 weeks, 6 months, and 12 months postoperatively.
Results
The volar tilt and radial inclination were restored after surgery and maintained well. The mean visual analog scale score was 4 ± 1 at 4 weeks. Range of motion was restored to 79% to 91% at 6 weeks. The DASH score was good before NBEF device removal. Two superficial pin-tract infections were easily treated with antibiotics.
Conclusions
Hybrid NBEF transfixes DRFs in a multiplanar fashion, and augmentation with percutaneous K-wires provides direct fixation in radial shift and withstands axial loads in fracture fragments. It allows early mobilization with rigid fixation. Hybrid NBEF is reliable for unstable extra-articular and simple intra-articular DRFs in older patients.
Clinical Study registration number
ChiCTR1900021712
Keywords: Nonbridging external fixation, distal radius fractures, osteoporotic, K-wire, early mobilization, older patients
Introduction
Distal radius fractures (DRFs) are the second most common fracture type in people of advanced age, and the incidence of DRFs sharply increases among women aged >50 years.1 With the baby boomers beginning to age and advanced-age individuals having a more active life than any previous generation, >10% of the advanced-age population will sustain a DRF caused by a fall from a standing height or other low-energy trauma.2 New concerns are arising regarding the optimal treatment for osteoporotic DRFs.
The functional demands in treating osteoporotic fractures have been improved with the development of living standards and surgical techniques. A pain-free wrist with adequate stability and motion is required for patients of advanced age because it allows an early return to daily activities with a minimum chance of degenerative change and stiffness. However, patients aged >50 years have a higher risk of secondary displacement than do patients aged <50 years because of the instability of osteoporotic fracture fragments.3 How to maintain the reduction of osteoporotic DRFs and avoid their secondary displacement with minimally invasive methods remains a dilemma in the treatment of osteopenic DRFs.
Closed reduction with plaster or K-wire immobilization has been the treatment of choice for decades, but these fractures are unstable and most will redisplace with compaction of osteoporotic trabeculae in a cast. Additionally, prolonged immobilization might lead to joint stiffness, which is unacceptable for advanced-age patients in the later years of their life.4 Open reduction and internal fixation with a locking plate restores the anatomic reduction of the radius but has a high cost and requires a second procedure to remove the plate.5 Furthermore, although traditional joint-bridging external fixation can maintain the radial length with minimal injury and allow limited postoperative adjustments, excessive distraction can lead to persistent motion restriction of the wrist and severe reflex sympathetic dystrophy.6
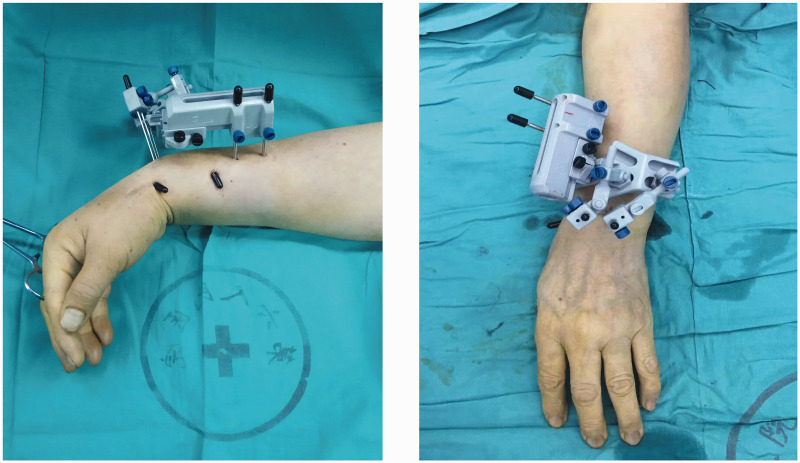
Nonbridging external fixation for DRFs combines closed reduction and early immobilization, and this technique has been recommended for DRFs with broad and rigid fracture fragments to accommodate several fixator pins, which is limited in osteoporotic fractures.7 We have used a hybrid nonbridging external fixation (NBEF) technique (Zimmer-Centerpulse AG, Zurich, Switzerland) supplemented by K-wires in the treatment of unstable osteoporotic extra-articular and simple intra-articular DRFs in patients of advanced age (Figure 1). The technique is based on combining the advantages of nonbridging external fixation and K-wires with the ability to allow immediate postoperative mobilization and prolonged fracture fixation in older patients. In this study, we evaluated the results of unstable DRFs treated with hybrid NBEF in terms of standard radiographic parameters [volar tilt (VT), radial inclination (RI), and ulnar variance (UV)], grip power, range of motion, the visual analog scale (VAS) score, and the Disabilities of the Arm, Shoulder and Hand (DASH) score.
Figure 1.
Hybrid nonbridging external fixation supplemented by K-wires in fixation of a distal radius fracture.
Patients and methods
Patients
This retrospective case-series study was performed to evaluate the safety and efficacy of hybrid NBEF supplemented by K-wires in the treatment of osteoporotic DRFs. We reviewed all patients who underwent hybrid NBEF from February 2016 through March 2018. All operations were performed by a single surgeon (C.H.) at our institution. The inclusion criteria were unstable DRFs with radial shortening of >5 mm, marked dorsal comminution, and angular deformity of >10°. The exclusion criteria were open fractures, postoperative follow-up time of <12 months, and age of <50 years. The study conformed to the Helsinki Declaration and was approved by the ethics committee of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital. Written informed consent was obtained from each participant according to institutional guidelines.
Surgical procedure
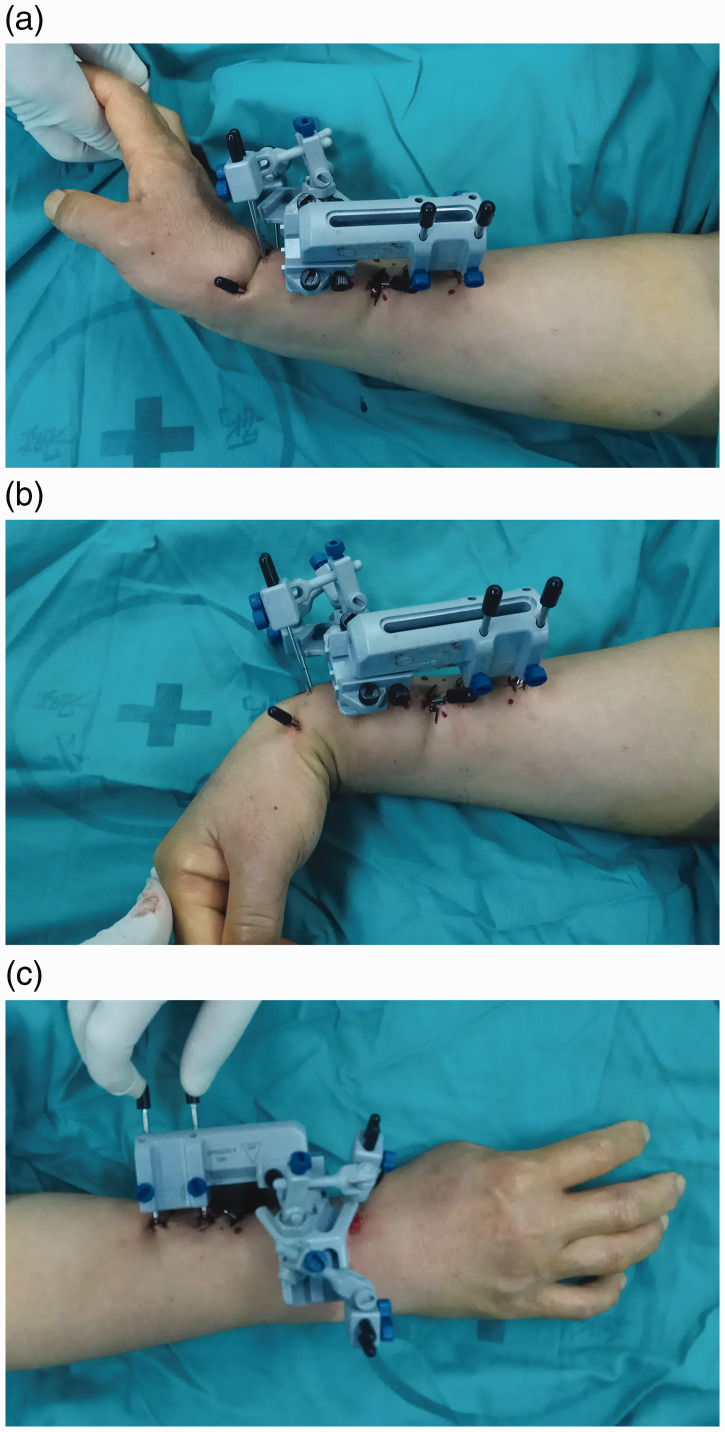
Surgical treatments were performed within 48 hours after the injury during a short hospital stay. The operations were performed under general or brachial plexus anesthesia. Closed reduction was achieved to align the fracture fragments with longitudinal traction and to restore the radial length and inclination under intraoperative fluoroscopic control. Alignment was maintained with percutaneous K-wires, allowing positioning of the wrist in slight extension. Two 2.0-mm K-wires were inserted with a mini-incision approach. One was positioned at the tip of the radial styloid and gained purchase in the strong diaphyseal ulnar cortex of the radial shaft through the fracture line. The other was positioned at the proximal end of the radius and driven to the lunate fossa. A preliminary nonbridging external fixator device (Zimmer-Centerpulse AG) was constructed after the anatomic reduction and percutaneous fixation. Initially, two proximal pins were driven through the tissue protector precisely in the mid-lateral border of the radius and drilled across two cortices of the shaft. A small stab wound was made before drilling, and the subcutaneous tissue under the incisions was carefully retracted while avoiding injury to the extensor tendons or the superficial radial nerve. All proximal pins were then tensioned to the external fixator body and its adapters. Bicortical purchase and the positions of the external fixators were again confirmed with fluoroscopy. In the next step, two 1.5-mm K-wires were inserted into the subchondral bone and engaged the volar ulnar lip of the distal radius, with one pin placed in the radial styloid fragment and the other pin placed in the distal radioulnar fragment. The tendon of the long extensor of the thumb was protected. In the third step, the K-wires were affixed to the adjustable K-wire fixators, and the external fixator device was placed in the oblique plane midway between the coronal and sagittal planes of the forearm. Extra pins were added in the distal fragments only if loosening of the implant–bone interlock occurred. The free movement of the wrist and the stability of the distal radioulnar joint were checked (Figure 2). After fixation, fluoroscopy was used to check the restoration of RI, radial height, palmar tilt, UV, articular joint congruency, and external fixator placement.
Figure 2.
Free movement of wrist in: (a) extension, (b) flexion, and (c) pronation during surgery.
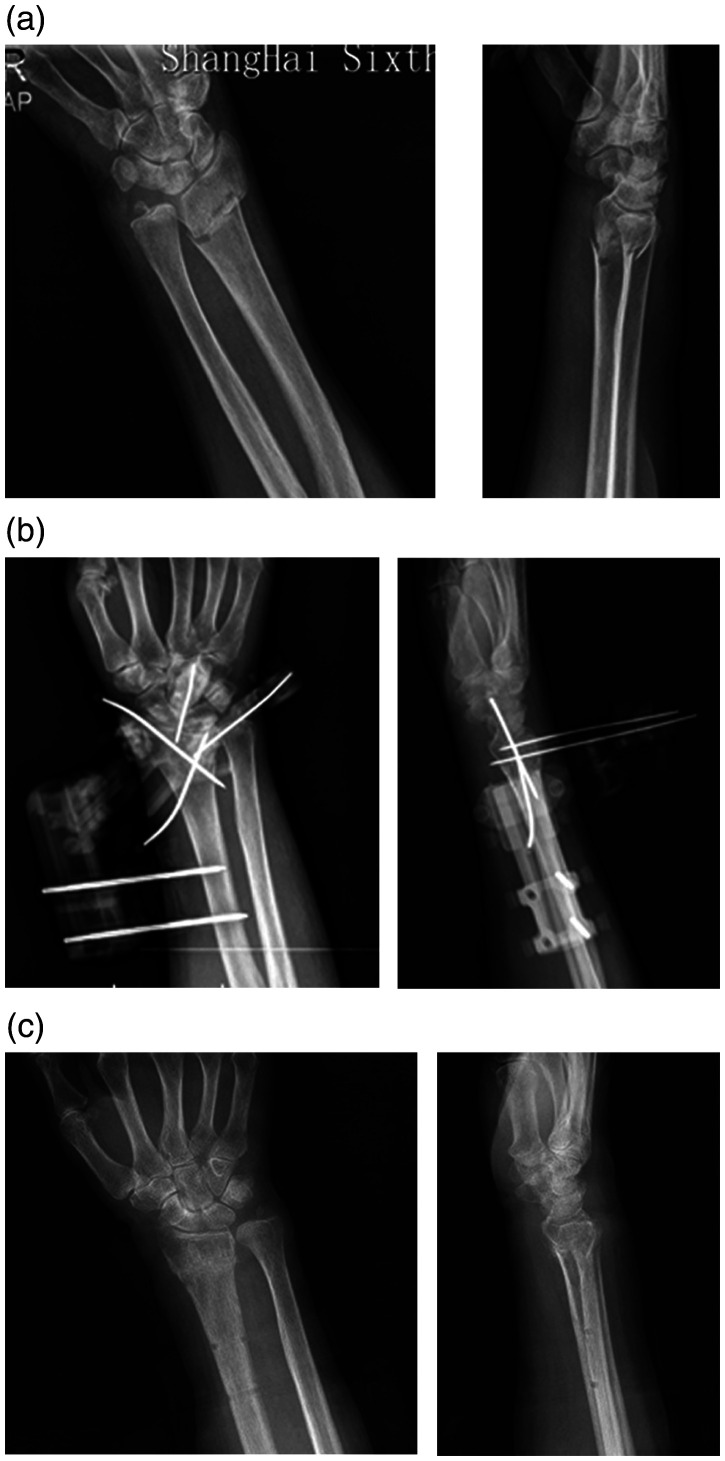
The external fixator devices were removed 4 to 5 weeks after surgery as an outpatient procedure, and the remaining K-wires were extracted 2 to 3 weeks later. The exact timing varied depending on the pin site integrity, presence of metaphyseal comminution, and radiographic evidence of healing (Figure 3).
Figure 3.
Patient with an AO type 23 A2.2 distal radius fracture: (a) before surgery, (b) 1 day after surgery, and (c) after removal of K-wires 6 weeks after surgery.
All patients underwent a similar rehabilitation program consisting of assisted and active exercises for 3 months. Digital motion exercises were begun immediately after surgery. All patients were encouraged to perform non-weight-bearing passive activities using the injured wrist and hand at the fist postoperative visit. Occupational therapy began during hospitalization and was performed three times per week. All outpatients were encouraged to begin a formal home exercise program for the wrist and fingers after removal of the external fixator devices.
Fracture healing and maintenance of fracture reduction were checked with standard radiographs of the wrist, ROM, grip power, VAS scores, and DASH scores8 at 4 weeks, 6 weeks, 6 months, and 12 months after surgery by an independent orthopedic surgeon. The ROM (extension, flexion, radial and ulnar abduction, pronation, and supination) of both wrists and grip power were measured using a goniometer and a hand dynamometer. Standard radiographic parameters of the distal radius (VT, RI, and UV) were measured preoperatively, immediately postoperatively, and 12 months postoperatively. Complications were recorded throughout the whole observation period.
Statistical analysis
Statistical tests were selected based on the distribution and type of data. A P value of ≤0.05 was considered statistically significant. Summary measurements are presented as median ± interquartile range (percentage of uninjured side) because 17 patients were included in the case series and the data were normally distributed. All statistical analyses were performed using the statistical software SPSS Version 19.0 (IBM Corp., Armonk, NY, USA).
Results
Seventeen patients (2 men and 15 women) with unstable DRFs were treated using hybrid NBEF supplemented by K-wires in our center (Table 1). All patients’ fractures were classified according to the AO classification system. Sixteen patients had an extra-articular fracture (AO type A2.2, n=10; A3.1, n=6), and one patient had an articular fracture (AO type C1). Fifteen patients had sustained their fractures by falling from a standing height, and two patients had sustained their fractures by falling from a height of 4 feet. The patients’ ages ranged from 51 to 83 years (mean, 61.8 years).
Table 1.
Preoperative patient data and 12-month postoperative complications and grip power.
| Patient no. | Sex | Age (y) | AO Classification | Smoking history | Pin-tract infection | Grip power (N) |
|---|---|---|---|---|---|---|
| 1 | F | 64 | A2.2 | N | N | 28 |
| 2 | F | 56 | A2.2 | N | N | 25 |
| 3 | F | 65 | A3.1 | N | N | 15 |
| 4 | F | 61 | A3.1 | N | N | 29 |
| 5 | F | 61 | A3.1 | N | N | 32 |
| 6 | F | 71 | A2.2 | N | N | 33 |
| 7 | F | 60 | A3.1 | N | N | 31 |
| 8 | F | 60 | A3.1 | N | N | 37 |
| 9 | F | 83 | A2.2 | N | N | 23 |
| 10 | F | 56 | A3.1 | N | N | 25 |
| 11 | M | 53 | A2.2 | N | N | 48 |
| 12 | F | 69 | A2.2 | N | N | 22 |
| 13 | F | 62 | A2.2 | N | N | 29 |
| 14 | F | 71 | C1.1 | N | N | 25 |
| 15 | M | 53 | A2.2 | Y | Y | 29 |
| 16 | F | 55 | A2.2 | N | N | 26 |
| 17 | F | 51 | A2.2 | N | N | 24 |
F, female; M, male; N, no; Y, yes.
The radiological parameters are listed in Table 2. The VT of the distal radius was restored from −18° ± 4° preoperatively to 5° ± 1° immediately postoperatively (P<0.05) and was maintained at 2° ± 3° at the final follow-up. The RI also recovered from 18° ± 1° preoperatively to 22° ± 2° immediately postoperatively (P<0.05) and was maintained at 22° ± 1° at the final follow-up. The difference in the VT and RI between the injured wrist and contralateral wrist significantly decreased after surgery, and these parameters were similar between the two wrists at 12 months postoperatively, suggesting that the reduction of the DRFs was well maintained during the healing process. The distal radius was kept in a good position, and the fracture line finally obtused. No aseptic pin loosening occurred in our study.
Table 2.
Radiographic parameters of distal radius preoperatively, immediately postoperatively, and 12 months postoperatively.
| Measurements | Volar tilt | Radial inclination | Ulnar variance (mm) |
|---|---|---|---|
| Prior to reduction | −18° ± 4° | 18° ± 1° | 0 ± 0 |
| Difference from contralateral wrist | −28° ± 5° | −7° ± 2° | −2 ± 1 |
| Immediately postoperatively | 5° ± 1° | 22° ± 2° | 2 ± 1 |
| Difference from contralateral wrist | −6° ± 3° | −2° ± 1° | 0 ± 0 |
| 12 months postoperatively | 2° ± 3° | 22° ± 1° | 0 ± 0 |
| Difference from contralateral wrist | −6° ± 0° | −4° ± 3° | −1 ± 1 |
Values are reported as median ± interquartile range.
All DRFs in our study healed, and the results of the radiological and functional evaluations are shown in Table 3. We recorded two superficial pin-tract infections, both of which healed within 1 week by local pin care and broad-spectrum systemic antibiotics (Patients 15 and 8). No patient developed irritation of the superficial radial nerve or extensor tendinitis. Furthermore, no reflex sympathetic dystrophy occurred in our study.
Table 3.
Range of motion, VAS scores, and DASH scores of patients at each follow-up.
| Wrist motion | 4 Weeks after surgery | 6 Weeks after surgery | 6 Months after surgery | 12 Months after surgery |
|---|---|---|---|---|
| Flexion | 55° ± 6° (82%) | 60° ± 5° (89%) | 63° ± 4° (94%) | 65° ± 3° (97%) |
| Extension | 46° ± 6° (79%) | 50° ± 4° (86%) | 54° ± 4° (93%) | 56° ± 4° (96%) |
| Radial deviation | 20° ± 4° (71%) | 22° ± 6° (79%) | 27° ± 9° (97%) | 27° ± 8° (97%) |
| Ulnar deviation | 17° ± 3° (74%) | 20° ± 3° (87%) | 22° ± 4° (96%) | 23° ± 5° (98%) |
| Pronation | 73° ± 8° (86%) | 75° ± 9° (88%) | 80° ± 6° (94%) | 82° ± 5° (96%) |
| Supination | 74° ± 8° (88%) | 77° ± 6° (91%) | 80° ± 7° (95%) | 81° ± 5° (96%) |
| VAS score | 4 ± 1 | 1 ± 1 | 0 ± 1 | 0 ± 1 |
| DASH score | 40 ± 13 | 18 ± 6 | 4 ± 5 | 3 ± 2 |
Values are reported as median ± interquartile range (percentage of uninjured side).
VAS, visual analog scale; DASH, Disabilities of the Arm, Shoulder and Hand.
The ROM was also well restored. Four weeks after surgery, the patients were able to perform passive activities with 55° ± 6° (82%) in palmar flexion, 46° ± 6° (79%) in extension, and 20° ± 4° (71%)/17° ± 3° (74%) in radial/ulnar deviation. Almost normal function was reached at 6 weeks after surgery, with palmar flexion at 60° ± 5° (89%), extension at 50° ± 4.0° (86%), and pronation/supination at 22° ± 6°/20° ± 3° (79%/87%). The forearm motion was 75° ± 9° (88%)/77° ± 6° (91%) in pronation/supination. No significant difference was noted at 6 and 12 months after surgery between the injured and uninjured sides.
Early joint movement did not correlate with high pain scores. VAS pain scores decreased continuously from 4 ± 1 on the first postoperative day to 1 ± 1 at 6 weeks (P<0.05). Few pain scores were recorded at the subsequent follow-ups. Grip power was also restored well, with a mean of 28.3 N.
The postoperative DASH score indicated good surgical outcomes in all 17 patients. Hand dominance did not have a significant influence on the subjective results. The DASH score reached 19.2 at 6 weeks before the removal of pins and was maintained at 19.2 at 12 months postoperatively.
Discussion
The hybrid NBEF technique proves to reliably maintain the alignment and position of unstable extra-articular and simple intra-articular DRFs until union in patients of advanced age. In the present study, the functional results with respect to ROM, grip power, pain scores, and DASH scores were consistently restored within 6 weeks postoperatively, and the subjective assessment 12 months postoperatively among all 17 patients showed excellent results in 14 patients and good results in 3 patients. Consistent with these findings, a meta-analysis of 46 articles describing 28 external fixation studies and 18 internal fixation studies revealed no clinically or statistically significant difference in the functional results.9
Early mobilization is the most obvious advantage of hybrid NBEF compared with conservative treatment involving plaster or bridging external fixation techniques. Hybrid NBEF allows early motion exercises of the metacarpophalangeal and interphalangeal joints immediately after surgery, which is beneficial for the resolution of edema and improvement of the ROM; it also avoids problems associated with forced and prolonged immobilization of the hand.10 Plaster keeps the wrist immobilized and partially impedes free metacarpophalangeal joint movement because it extends beyond the flexor crease. Skin care is also impossible because of the plaster. The application of transarticular external fixation is frequently threatened by overdistraction and injury to the median nerve, which might induce dysesthesia, increased median nerve pressure with pain and paresthesia, and reflex sympathetic dystrophy.11 All of these conditions cause dysfunction, stiffness, and pain. Hybrid NBEF supplemented by K-wires is used to achieve neutralization without distraction, and the wrist is fixed in neutral flexion. The incidence of stiffness, reflex sympathetic dystrophy, and other complications was limited in our study.
Hybrid NBEF is effective in the presence of radial and dorsal shift, one of the major obstacles to external fixation of DRFs in older patients, because hybrid NBEF transfixes the fragment in a multiplanar fashion with high axial flexibility. The distal pins mounted to the fixator are dorsally placed into the stout volar metaphyseal cortex through the dense subchondral bone with crossing angles of 90° on the dorsal side.12 This directly opposes the high dorsally deforming forces of the wrist and digital extensors and effectively corrects the dorsal tilt.13 Augmentation with percutaneous K-wires provides fixation to neutralize the axial loads of the osteoporotic fracture fragments and decreases the dependency of radial shift by ligamentotaxis from the brachioradialis.14 An augmented percutaneous K-wire is as valuable as a K-wire attached to fixators according to a previous report.15 In the present study, the hybrid NBEF device maintained mechanical rigidity during fixation of the osteoporotic fractures.
Augmentation with percutaneous K-wire fixation provides direct fixation in radial shift and withstand axial loads in DRFs. Hybrid NBEF supplemented with K-wires distributes the load in the wrist, about 100 to 180 pounds in the postoperative phase.16 The configuration of the NBEF device transfixes the bone in a multiplanar and coaxial fashion, and its relative axial flexibility is considered beneficial for uniform callus formation. Considering the high incidence of refracture and slow healing rate in patients with osteoporosis, we prefer gradual removal of the hybrid NBEF system. After removal of the external fixators 4 weeks postoperatively, the remaining K-wires can support the fixation stability of the fracture fragments with aggressive wrist exercises such as lifting, squeezing, and forceful rotation. Histologic studies by Gradl et al.17 showed increased bone porosity and intracortical new bone formation that continued throughout the first 4 months of bony healing. This is consistent with our study, which showed radiographic evidence of increased bone density bony callus formation from 1 to 6 months postoperatively.
In a randomized controlled trial of 166 patients with displaced intra-articular DRFs who had been randomized to treatment with either a volar locking plate or percutaneous pinning augmented external fixation, Hammer et al.18 found that the volar locking plate was equal to augmented external fixation in terms of RI and radial length maintenance as shown in the radiographic evaluation. Gereli et al.19 also reported that the combination of an external fixator augmented with K-wires approached a strength of a 3.5-mm dorsal AO plate. These findings were corroborated by the radiological parameters in the present study. Both the VT and RI of the distal radius were significantly restored after surgery (−18° ± 4° to 5° ± 1° and 18° ± 1° to 22° ± 2°, respectively), and satisfactory reduction was well maintained at the final follow-up. No obvious change was observed in UV, partially because of the limited radial shortening preoperatively. Hybrid NBEF supplemented by K-wires maintained mechanical rigidity in fixation of osteoporotic fractures for 12 months after surgery, which allowed early motion exercises of the wrist joint and supported good function as indicated by the DASH scores, ROM, grip power, and pain scores during follow-up.
Flinkkilä et al.20 described the use of uniplanar nonbridging external fixators in the treatment of DRFs. This technique prevents dorsal angulation well but is less effective with radial or dorsal shift. The pins of the Ilizarov fixator are perpendicular to the long axis of the bone, and this configuration unloads the fracture. The hybrid NBEF device shares the load on the fracture fragments and reduces the risk of nonunion because of stress shielding.21 Hybrid NBEF leads to a broad load distribution along the fracture line and adds to the stability with the osteoporotic bony fragments. In addition, K-wires with smaller diameters in the distal fragment do not adversely affect early wrist motion and cause no damage to the extensor tendons. Therefore, hybrid NBEF supplemented by K-wires also appears to be a reasonable technique with which to resolve the complications associated with other external fixation methods.
The present study had some limitations. The patients were mainly those with extra-articular DRFs; only one patient had an intra-articular fracture (AO type C1). No comminuted DRFs or complicated intra-articular fractures were included in our study. Additionally, the results of application of hybrid NBEF in the presence of severe intra-articular comminution or metaphyseal comminution remains unknown. Finally, the sample size was limited in our study.
Hybrid NBEF allows early mobilization with rigid fixation of fracture fragments and has advantages over the traditional external fixation techniques with respect to complications such as wrist stiffness and reflex sympathetic dystrophy. The NBEF device transfixes the DRFs in a multiplanar and coaxial fashion with high flexibility. Augmentation with K-wires is critical in maintaining stability after removal of the fixators considering the high incidence of refracture and slow healing rate in patients with osteoporosis.
Data availability statement
All clinical data used to support the findings of this study are included within the article.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This work was sponsored by the Natural Science Foundation of China (No. 81702183) and Shanghai Sailing Program (No. 17YF1414100).
ORCID iD
Pengfei Cheng https://orcid.org/0000-0002-8597-9603
References
- 1.Porrino JA. Jr, Maloney E, Scherer K, et al. Fracture of the distal radius: epidemiology and premanagement radiographic characterization. AJR Am J Roentgenol 2014; 203: 551–559. [DOI] [PubMed] [Google Scholar]
- 2.Cummings SR, Black DM, Rubin SM. Lifetime risks of hip, Colles', or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med 1989; 149: 2445–2458. [PubMed] [Google Scholar]
- 3.Leone J, Bhandari M, Adili A, et al. Predictors of early and late instability following conservative treatment of extra-articular distal radius fractures. Arch Orthop Trauma Surg 2004; 124: 38–41. [DOI] [PubMed] [Google Scholar]
- 4.Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am 2009; 91: 1868–1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spiteri M, Ng W, Matthews J, et al. Functional outcome of fixation of complex intra-articular distal radius fractures with a variable-angle distal radius volar rim plate. J Hand Microsurg 2017; 9: 11–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fakoor M, Fakoor M, Mohammadhoseini P. Displaced intra-articular fractures of the distal radius: open reduction with internal fixation versus bridging external fixation. Trauma Mon 2015; 20: e17631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gausepohl T, Worner S, Pennig D, et al. Extraarticular external fixation in distal radius fractures pinplacement in osteoporotic bone. Injury 2001; 32: SD79–SD85. [DOI] [PubMed] [Google Scholar]
- 8.Gartland JJ, Jr, Werley CW. Evaluation of healed Colles' fractures. J Bone Joint Surg Am 1951; 33-A: 895–907. [PubMed] [Google Scholar]
- 9.Margaliot Z, Haase SC, Kotsis SV, et al. A meta-analysis of outcomes of external fixation versus plate osteosynthesis for unstable distal radius fractures. J Hand Surg Am 2005; 30: 1185–1199. [DOI] [PubMed] [Google Scholar]
- 10.Ishikawa J, Iwasaki N, Minami A. Influence of distal radioulnar joint subluxation on restricted forearm rotation after distal radius fracture. J Hand Surg Am 2005; 30: 1178–1184. [DOI] [PubMed] [Google Scholar]
- 11.Grala P, Zielinski W. Hybrid external fixation for neglected fractures of the distal radius: results after one year. J Orthop Traumatol 2008; 9: 195–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duyck J, Vandamme K. The effect of loading on peri-implant bone: a critical review of the literature. J Oral Rehabil 2014; 41: 783–794. [DOI] [PubMed] [Google Scholar]
- 13.Dodds SD, Cornelissen S, Jossan S, et al. A biomechanical comparison of fragment-specific fixation and augmented external fixation for intra-articular distal radius fractures. J Hand Surg Am 2002; 27: 953–964. [DOI] [PubMed] [Google Scholar]
- 14.Wolfe SW, Austin G, Lorenze M, et al. A biomechanical comparison of different wrist external fixators with and without K-wire augmentation. J Hand Surg Am 1999; 24: 516–524. [DOI] [PubMed] [Google Scholar]
- 15.Wolfe SW, Swigart CR, Grauer J, et al. Augmented external fixation of distal radius fractures: a biomechanical analysis. J Hand Surg Am 1998; 23: 127–134. [DOI] [PubMed] [Google Scholar]
- 16.Ruschel PH, Albertoni WM. Treatment of unstable extra-articular distal radius fractures by modified intrafocal Kapandji method. Tech Hand Up Extrem Surg 2005; 9: 7–16. [DOI] [PubMed] [Google Scholar]
- 17.Gradl G, Steinborn M, Wizgall I, et al. Acute CRPS I (morbus sudeck) following distal radial fractures–methods for early diagnosis. Zentralbl Chir 2003; 128: 1020–1026. [DOI] [PubMed] [Google Scholar]
- 18.Hammer OL, Clementsen S, Hast J, et al. Volar locking plates versus augmented external fixation of intra-articular distal radial fractures: functional results from a randomized controlled trial. J Bone Joint Surg Am 2019; 101: 311–321. [DOI] [PubMed] [Google Scholar]
- 19.Gereli A, Nalbantoglu U, Kocaoglu B, et al. Comparison of palmar locking plate and K-wire augmented external fixation for intra-articular and comminuted distal radius fractures. Acta Orthop Traumatol Turc 2010; 44: 212–219. [DOI] [PubMed] [Google Scholar]
- 20.Flinkkila T, Ristiniemi J, Hyvonen P, et al. Nonbridging external fixation in the treatment of unstable fractures of the distal forearm. Arch Orthop Trauma Surg 2003; 123: 349–352. [DOI] [PubMed] [Google Scholar]
- 21.Tyllianakis M, Mylonas S, Saridis A, et al. Treatment of unstable distal radius fractures with Ilizarov circular, nonbridging external fixator. Injury 2010; 41: 306–311. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All clinical data used to support the findings of this study are included within the article.