Abstract
Objective
Critically ill patients often require emergency endotracheal intubation and mechanical ventilation. When esophageal intubation is not confirmed early, treatment may be delayed, even for life-threatening conditions. We examined the accuracy of bedside real-time airway ultrasonography in confirming the endotracheal tube (ETT) position during emergency endotracheal intubation in patients in the intensive care unit (ICU).
Methods
This single-center prospective observational study included 118 patients who underwent urgent endotracheal intubation in the ICU of Taizhou Hospital of Integrated Traditional Chinese and Western Medicine. Tracheal ultrasonography was used to confirm the ETT position during endotracheal intubation, after which fiberoptic bronchoscopy was performed. The accuracy of bedside real-time tracheal ultrasonography in determining the ETT position was examined.
Results
Twelve (10.2%) patients underwent endotracheal intubation. The kappa value was 0.844, indicating perfect consistency between tracheal ultrasonography and fiberoptic bronchoscopy in identifying esophageal intubation. The sensitivity, specificity, and positive and negative predictive values of tracheal ultrasonography in determining the ETT position were 75.0%, 100%, 100%, and 97.2%, respectively.
Conclusions
Bedside real-time tracheal ultrasonography accurately assesses the ETT position in the ICU and can identify the ETT position during intubation. These findings have important clinical applications and are of great significance for treatment of ICU patients.
Keywords: Tracheal ultrasonography, tracheal intubation, fiberoptic bronchoscopy, esophageal intubation, intensive care unit, emergency
Introduction
Patients in the intensive care unit (ICU) often require emergency endotracheal intubation and mechanical ventilation; however, endotracheal intubation is often difficult because of unfavorable conditions. Proper placement of an endotracheal tube (ETT) is a key step in airway management, and inappropriate ETT placement can lead to severe complications. The most serious of these complications is esophageal intubation, which occurs at incidences as high as 6% to 16%.1,2 If esophageal intubation is not confirmed early, treatment can be delayed, even for life-threatening conditions.3,4 Current guidelines recommend that the ETT position should be confirmed as soon as possible while minimizing interference with other rescue efforts.5 Therefore, endotracheal intubation for emergency airway management should focus on early confirmation of esophageal intubation.
Several methods are used in clinical practice to judge the ETT position, such as auscultation of breath sounds, fiberoptic bronchoscopy, direct viewing of the ETT through the glottis, chest radiographs, and observation of thoracic undulations during respiratory sac-assisted ventilation. The accuracy varies among these different methods, and each method has its own limitations.6,7 Because of the impact of the rescue environment and personal experiences, these traditional methods often provide inaccurate information on the ETT position, which can cause treatment delays in critically ill patients. To increase the success rate of endotracheal intubation, the American Heart Association recommends the use of end-tidal carbon dioxide (ETCO2) monitoring to confirm the ETT location.3 However, continuous ETCO2 monitoring is prohibited for some patients, especially those with cardiac arrest and large-scale pulmonary embolisms.8–10 Moreover, continuous ETCO2 monitoring is not commonly used. Furthermore, many doctors in hospitals that are clinically eligible to use ETCO2 technology have poor compliance. In 2005, a survey showed that only 14% of doctors “always” applied this technology that and 57% of doctors “never” or “rarely” used it.11 Many primary-level hospitals do not yet carry this technology.
Any delay in confirmation of esophageal intubation may result in the occurrence of severe complications and increased mortality. Therefore, accurate and timely confirmation of the ETT position is of particular importance. Confirmation of the ETT position by ultrasonography has become increasingly popular because of the advantages of ultrasonography, which include high accuracy, cost-effectiveness, high speed, ease of transport, and high feasibility during intubation.12 Several studies have confirmed the safety and effectiveness of ultrasonography in confirming the ETT location in rescue patients in the operating room and emergency department as well as during out-of-hospital emergencies.13–16 In these studies, the accurate position of the ETT was determined within a short time after endotracheal intubation using ultrasonography to avoid delays in rescue. Few clinical studies have focused on the use of real-time tracheal ultrasonography for confirming the ETT position in the ICU, especially with respect to real-time tracheal ultrasonography assessment of the airway during endotracheal intubation.3,17 The present study was performed to examine the accuracy of bedside real-time tracheal ultrasonography in determining the ETT position in patients in the ICU.
Patients and methods
Study design and subjects
This single-center prospective observational study included 129 patients who underwent urgent endotracheal intubation in the ICU of Taizhou Hospital of Integrated Traditional Chinese and Western Medicine from January 2016 to March 2019. Patients who underwent endotracheal intubation under direct laryngoscopy were considered for inclusion. Patients who met one or more of the following conditions were excluded from this study: age of <18 years, cervical spine injury, neck tumor, subcutaneous emphysema of the neck, history of neck surgery or radiotherapy, and family members’ refusal to allow the patient to participate in this study. This study was approved by the Hospital Medical Ethics Committee.
Methods and outcome measures
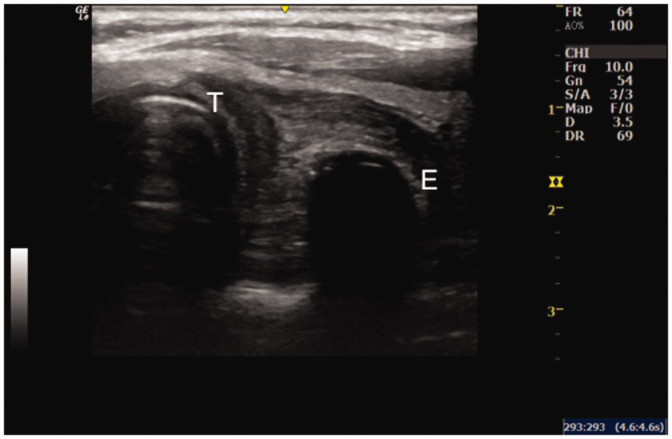
An ultrasonography study group was established. This group included three attending physicians who had more than 3 years of experience in ultrasonography application in critically ill patients, had completed tracheal application training for critically ill patients, and had obtained a certificate of qualification. Tracheal ultrasonography was performed using a portable ultrasound machine (LOGIQ; GE Healthcare, Chicago, IL, USA) with a high-frequency probe (6–13 MHz). During treatment in the ICU, the ultrasonography study group was notified once there was an indication for emergency endotracheal intubation. Anesthesiologists performed the endotracheal intubation, and patients who could not cooperate were sedated. During endotracheal intubation, the members of the ultrasonography study group placed the transducer laterally, more than 2 cm above the sternal notch, and moved the device to the left until the trachea and esophagus were clearly displayed (Figure 1). When the ETT was placed under the laryngoscope, the members of the ultrasonography study group determined whether the ETT was in the trachea or the esophagus. On ultrasonography scans, esophageal intubation is characterized by esophageal dilation or a “double-track sign” in the esophagus (Figure 2). Endotracheal intubation shows a transient artifact, and tracheal ultrasonography shows no findings of esophageal intubation when the ETT enters the trachea.3 In the present study, this process was performed when the ETT was placed and before fiberoptic bronchoscopy was completed to facilitate blind processing. After endotracheal intubation, the position of the ETT was confirmed by fiberoptic bronchoscopy (BF-XP40; Olympus, Tokyo, Japan). If the ICU medical team felt that the presence of the ultrasonography study group interfered with the patient’s treatment, the ultrasonography study group members immediately discontinued the procedure. During the procedure, we tried to ensure that the ultrasonography study group members and the fiberoptic bronchoscope operators were unaware of the ETT position. If the fiberoptic bronchoscopy confirmed that the ETT was in the esophagus, endotracheal intubation guided by fiberoptic bronchoscopy was performed immediately to increase the efficiency of patient rescue.
Figure 1.
Tracheal ultrasonography reveals the trachea and esophagus. T, trachea; E, esophagus.
Figure 2.
Esophageal intubation. A dilated esophagus and esophageal “double-track sign” were observed. T, trachea; E, esophagus.
Basic patient information, indications for endotracheal intubation, drugs for rapid induction of endotracheal intubation, body mass index, ETT model, and the results of the ETT position confirmation were collected for both methods.
Statistical analysis
The sample size required for this study was estimated to be 114 patients, and according to the study by Gottlieb et al.,18 the sensitivity and specificity of tracheal ultrasonography in determining the ETT position was expected to be 92%. When performing endotracheal and esophageal intubations, the maximum allowable error for tracheal ultrasonography and fiberoptic bronchoscopy was 0.05, and the confidence interval was calculated as 95%. This simple nomogram is based on the sample size and is used to estimate the sensitivity and specificity of medical tests.19 All data were first tested for normality, and the normally distributed measurement data are expressed as mean ± standard deviation. Data that were not normally distributed or had unequal variances are expressed as median (interquartile range). Count data are expressed as the rate/percentage/composition ratio, and the chi-square test was used to compare data between groups. At an alpha level of 0.05, P values of <0.05 were considered statistically significant. The fiberoptic bronchoscopy results were used as the gold standard for determining the ETT position, and the sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of bedside real-time tracheal ultrasonography were calculated. The kappa statistic was used to examine the consistency between bedside tracheal ultrasonography and fiberoptic bronchoscopy in confirming the ETT position. The kappa results were interpreted as follows: 0.81 to 1.00, almost perfect consistency; 0.61 to 0.80, substantial consistency; 0.41 to 0.60, moderate consistency; 0.21 to 0.40, fair consistency; and <0.20, no to slight consistency.20 SPSS 19.0 software (IBM Corp., Armonk, NY, USA) was used for statistical analyses and figure preparation.
Results
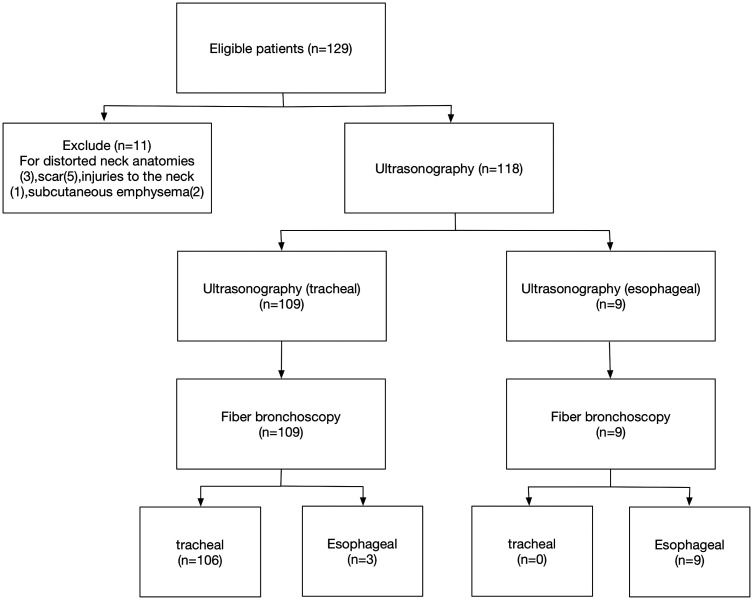
The study flow chart is shown in Figure 3. In total, 118 patients were included in the study, of whom 71 (60.2%) were men and 47 (39.8%) were women. The patients had an average age of 71.5 years (range, 59.0–82.0 years). Coma was the main reason for endotracheal intubation and was present in 45 (38.1%) patients (Table 1). During intubation, 14 (11.9%) patients did not use sedative drugs. Midazolam was the main sedative drug and was used by 65 (55.1%) patients (Table 2). The tracheal ultrasonography results showed that among the 109 patients who underwent endotracheal intubation, esophageal intubation occurred in 3 patients (Table 3). The accuracy of endotracheal ultrasonography in identifying esophageal intubation was 97.4%, with a kappa value of 0.844; this suggests that endotracheal ultrasonography and fiberoptic bronchoscopy had almost perfect consistency in identifying esophageal intubation. The fiber bronchoscopy results were used as the gold standard for determining esophageal intubation. The sensitivity, specificity, positive predictive value, and negative predictive value of bedside real-time tracheal ultrasonography were 75.0%, 100%, 100%, and 97.2%, respectively. No related complications occurred during the study.
Figure 3.
Study flow chart.
Table 1.
Basic information of 118 patients included in this study.
| Basic information | Value |
|---|---|
| Patients, n | 118 |
| Age, years | 71.5 (59.0–82.0) |
| Male sex | 71 (60.2) |
| Female sex | 47 (39.8) |
| Body mass index, kg/m2 | 21.6 ± 2.7 |
| Cause of intubation | |
| Coma | 45 (38.1) |
| Acute respiratory failure | 34 (28.8) |
| Shock | 33 (28.0) |
| Others | 6 (5.1) |
Data are presented as n, n (%), median (interquartile range), or mean ± standard deviation.
Table 2.
Characteristics and results of intubation operations.
| Characteristics | Value |
|---|---|
| Number of intubations | 1.0 (1.0–1.0) |
| Sedative drug use | |
| No use | 14 (11.9) |
| Midazolam | 65 (55.1) |
| Propofol | 21 (17.8) |
| Dexmedetomidine | 38 (38.2) |
| Diameter of ETT, mm | 8.0 (7.5–8.5) |
| Number of patients who underwent esophageal intubation | 12 (10.2) |
| Number of patients who underwent endotracheal intubation | 106 (89.8) |
Data are presented as median (interquartile range) or n (%).
ETT, endotracheal tube.
Table 3.
Identification of esophageal and tracheal intubation using bedside real-time tracheal ultrasonography.
|
Fiberoptic bronchoscopy |
|||
|---|---|---|---|
| Tracheal ultrasonography | Tracheal intubation | Esophageal intubation | Total |
| Tracheal intubation | 106 | 3 | 109 |
| Esophageal intubation | 0 | 9 | 9 |
| Total | 106 | 12 | 118 |
Discussion
The results of the current study indicate that bedside real-time tracheal ultrasonography can effectively identify endotracheal intubation and esophageal intubation with an accuracy of 97.2% and has good consistency with fiberoptic bronchoscopy (kappa value of 0.844). These findings are consistent with the results reported by Arya et al.21 Moreover, bedside real-time tracheal ultrasonography also shortens the time needed for determining the ETT position. Tracheal ultrasonography can identify esophageal intubation by revealing esophageal dilatation and the double-track sign produced by the adjacent trachea. Compared with traditional methods of confirming the ETT position, tracheal ultrasonography is simple and convenient and can guide clinical decision-making in real time. Clinically, if real-time tracheal ultrasonography is used to detect esophageal intubation, the operator can make appropriate decisions immediately without waiting for confirmation by other methods. In this study, the negative predictive value of bedside real-time tracheal ultrasonography was 97.2%. Therefore, once real-time tracheal ultrasonography confirmed intratracheal intubation, the likelihood of esophageal intubation was only 2.8%.
During ICU rescue, the ETT position must be identified quickly and accurately. Many methods are available for clinical confirmation of the ETT position, but each has its limitations. ETCO2 monitoring provides false-negative and false-positive results and has an accuracy of only 67.9% in patients with respiratory arrest.22 Tracheal ultrasonography compensates for this deficiency without affecting cardiopulmonary resuscitation. However, Karacabey et al.23 showed that the accuracy of tracheal ultrasonography in identifying the ETT position in patients with cardiac arrest was 76.7% because it was affected by cardiopulmonary resuscitation. We also found that some differences influence the results obtained from each method. First, there are inherent differences between the methods themselves. Notably, Karacabey et al.23 used static methods to evaluate the ETT position after intubation; however, dynamic methods may be better than static methods for confirming the ETT position in patients with cardiac arrest. Second, prior studies reported higher rates of esophageal intubation (38.0%) than our study (10.2%), which could be due to the impact of false-positive and false-negative findings during esophageal intubation. Additionally, tracheal ultrasonography can identify the ETT position in the absence of mechanical ventilation, and there is no risk of acute gastric dilatation or aspiration due to inappropriate ETT positioning. However, in special circumstances, such as emergency control, disaster scenes, and areas where medical resources are scarce, conventional equipment for detection of the ETT position is difficult to acquire or transport or is not allowed.24 Tracheal ultrasonography can be effectively applied in these cases because of its simplicity, convenience, portability, and repeatability.
Clinically, static tracheal ultrasonography has been used to confirm the ETT position. Usually, after tracheal intubation, a linear probe is used to examine the cross section of the trachea. A double-track sign in the trachea suggests endotracheal intubation, the lack of an intratracheal double-track sign suggests dilatation of the esophagus, and a double-track sign in the esophagus suggests esophageal intubation. A study by Bin Osman et al.10 suggested that the sensitivity and specificity of static tracheal ultrasonography in determining the ETT position were 98% and 100%, respectively, and that static tracheal ultrasonography could be performed in only 16.4 ± 7.33 seconds. Gottlieb et al.18 used dynamic and static methods to evaluate 240 ETT locations, and their results showed that the sensitivity and specificity of the static evaluation method in determining the ETT locations were 93.6% and 98.3%, respectively. The corresponding sensitivity and specificity for dynamic evaluation methods were 92.1% and 91.2%, respectively, and no statistically significant differences were found between the sensitivity and specificity of dynamic and static evaluation methods.18 Dynamic real-time evaluation involves real-time operation, which reduces the time required to identify the ETT position and saves valuable rescue time. The sensitivity of tracheal ultrasonography in the present study was only 75.0%, which is significantly lower than the sensitivity of 93.6% reported in the study referenced above. The main reasons for this difference are as follows. First, the above study was performed with cadavers, which have an anatomical structure different from that of living patients. Second, some patients in the present study were not well sedated or did not take sedative drugs, which could have led to coughing and swaying during intubation, thus affecting imaging results. Furthermore, some scholars have indirectly evaluated the ETT position by observing pleural patency through the intercostal space or by observing diaphragmatic activity under the right rib. However, these two methods are susceptible to the effects of mechanical ventilation pressure, tidal volume, and lung lesions (such as pneumothorax, lung consolidation, and pleural thickening), which limit their application.25,26
Tracheal ultrasonography misclassified esophageal intubation as endotracheal intubation in only three cases in the present study. In two of these cases, obvious coughing occurred during intubation, which prevented the acquisition of high-quality images. In the last case, the error was caused by a laterally bending esophageal anomaly. The double-track sign was not seen during intubation because the ETT caused a shift in the esophageal position and was thus inserted into the esophagus. We observed the double-track sign on the other side of the neck with tracheal ultrasonography.
This study has several limitations. First, although the members of the ultrasound study group had undergone relevant training, their actual operating experience and skill level may have affected the evaluation results. Second, the patients included in this study were in urgent need of rescue, and the double-blind principle was not well implemented. Third, the different sedation statuses of the patients may have affected the test results because of coughing and irritability, which affect the imaging quality. Fourth, the proportion of obese patients in this study was not high, which may have increased the sensitivity and specificity of the detection method.
Overall, the results from this study suggest that it is feasible to perform bedside real-time tracheal ultrasonography to identify the ETT position in patients in the ICU. Bedside real-time tracheal ultrasonography can identify the ETT position during intubation, which is of great significance for the emergency rescue of ICU patients and is worthy of clinical application. A multicenter large-scale study is needed to further validate the clinical value of applying of bedside real-time tracheal ultrasonography.
Authors’ contributions
Weiting Chen conceived and designed the study. Hehao Wang participated in the data analysis. Junbo Chen collected the data. Yingzi Chen drafted the manuscript, and all authors critically revised the manuscript for intellectual content. All authors have read and approved the final version of this manuscript.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
All authors have reviewed and approved the manuscript for publication.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Ethics approval and consent to participate
The study protocol was approved by the ethics committee of our hospital. All patients provided written informed consent.
Funding
This work was supported by the Science and Technology Project of Wenling (2018C310025) and Clinical Research Projects of the Zhejiang Medical Association (2018ZYC-A003).
ORCID iD
Weiting Chen https://orcid.org/0000-0001-5993-0737
References
- 1.Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med 2001; 37: 32–37. [DOI] [PubMed] [Google Scholar]
- 2.Jones JH, Murphy MP, Dickson RLet al. Emergency physician–verified out‐of‐hospital intubation: miss rates by paramedics. Acad Emerg Med 2004; 11: 707–709. [DOI] [PubMed] [Google Scholar]
- 3.Das SK, Choupoo NS, Haldar Ret al. Transtracheal ultrasound for verification of endotracheal tube placement: a systematic review and meta-analysis. Can J Anaesth 2015; 62: 413–423. [DOI] [PubMed] [Google Scholar]
- 4.Wirtz DD, Ortiz C, Newman DHet al. Unrecognized misplacement of endotracheal tubes by ground prehospital providers. Prehosp Emerg Care 2015; 11: 213–218. [DOI] [PubMed] [Google Scholar]
- 5.Link MS, Berkow LC, Kudenchuk PJet al. Part 7: adult advanced cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2010; 122: S685. [DOI] [PubMed] [Google Scholar]
- 6.Lei P, Yan-Hua F, Hai-Chun Met al. Fiberoptic bronchoscopy-assisted endotracheal intubation in a patient with a large tracheal tumor. Int Surg 2015; 100: 589–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rudraraju P, Eisen LA. Analytic review: confirmation of endotracheal tube position: a narrative review. J Intensive Care Med 2009; 24: 283–292. [DOI] [PubMed] [Google Scholar]
- 8.Takeda T, Tanigawa K, Tanaka Het al. The assessment of three methods to verify tracheal tube placement in the emergency setting. Resuscitation 2003; 56: 153–157. [DOI] [PubMed] [Google Scholar]
- 9.Cook TM, Nolan JP. Use of capnography to confirm correct tracheal intubation during cardiac arrest. Anaesthesia 2011; 66: 1183–1184. [DOI] [PubMed] [Google Scholar]
- 10.Bin Osman A, Chuan T, Manikam R. A feasibility study on bedside upper airway ultrasonography compared to waveform capnography for verifying endotracheal tube location after intubation. Crit Ultrasound J 2013; 5: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deiorio NM. Continuous end-tidal carbon dioxide monitoring for confirmation of endotracheal tube placement is neither widely available nor consistently applied by emergency physicians. J Emerg Med 2005; 22: 490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sustić A. Role of ultrasound in the airway management of critically ill patients. Crit Care Med 2007; 35: S173–S177. [DOI] [PubMed] [Google Scholar]
- 13.Milling TJ, Jones M, Khan Tet al. Transtracheal 2-D ultrasound for identification of esophageal intubation. J Emerg Med 2007; 32: 409–414. [DOI] [PubMed] [Google Scholar]
- 14.Werner SL, Smith CE, Goldstein JRet al. Pilot study to evaluate the accuracy of ultrasonography in confirming endotracheal tube placement. Ann Emerg Med 2007; 49: 75–80. [DOI] [PubMed] [Google Scholar]
- 15.Pfeiffer P, Rudolph SS, BRglum Jet al. Temporal comparison of ultrasound vs. auscultation and capnography in verification of endotracheal tube placement. Acta Anaesthesiol Scand 2011; 55: 1190–1195. [DOI] [PubMed] [Google Scholar]
- 16.Zadel S, Strnad M, Prosen Get al. Point of care ultrasound for orotracheal tube placement assessment in out-of-hospital setting. Resuscitation 2015; 87: 1–6. [DOI] [PubMed] [Google Scholar]
- 17.Chou EH, Dickman E, Tsou PYet al. Ultrasonography for confirmation of endotracheal tube placement: a systematic review and meta-analysis. Resuscitation 2015; 90: 97–103. [DOI] [PubMed] [Google Scholar]
- 18.Gottlieb M, Nakitende D, Sundaram Tet al. Comparison of static versus dynamic ultrasound for the detection of endotracheal intubation. West J Emerg Med 2018; 19: 412–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou XH, Obuchowski NA, McClish D. Statistical methods in diagnostic medicine. Introduction 2011; 1–11.
- 20.Altman D. Statistics in medical journals: developments in the 1980s. Stat Med 1991; 10: 1897–1913. [DOI] [PubMed] [Google Scholar]
- 21.Arya R, Schrift D, Choe Cet al. Real-time tracheal ultrasound for the confirmation of endotracheal intubations in the intensive care unit: an observational study. J Ultrasound Med 2019; 38: 491–497. [DOI] [PubMed] [Google Scholar]
- 22.Li J. Capnography alone is imperfect for endotracheal tube placement confirmation during emergency intubation. J Emerg Med 2001; 20: 223–229. [DOI] [PubMed] [Google Scholar]
- 23.Karacabey S, Sanrı E, Gencer EGet al. Tracheal ultrasonography and ultrasonographic lung sliding for confirming endotracheal tube placement: speed and reliability. Am J Emerg Med 2016; 34: 953–956. [DOI] [PubMed] [Google Scholar]
- 24.Chun R, Kirkpatrick A, Sirois Met al. Where's the tube? Evaluation of hand-held ultrasound in confirming endotracheal tube placement. Prehosp Disaster Med 2004; 19: 366–369. [DOI] [PubMed] [Google Scholar]
- 25.Weaver B, Lyon M, Blaivas M. Confirmation of endotracheal tube placement after intubation using the ultrasound sliding lung sign. Acad Emerg Med 2006; 13: 239–244. [DOI] [PubMed] [Google Scholar]
- 26.Seyedhosseini J, Talebian TM, Ghafari HMet al. Secondary confirmation of endotracheal tube position by diaphragm motion in right subcostal ultrasound view. Int J Crit Illn Inj Sci 2013; 3: 113–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.