The coronavirus disease 2019 (COVID-19) pandemic (caused by severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2]) has led to a dramatic loss of lives and presented an unprecedented challenge to public health and economic systems worldwide. To date, >58.7 million people globally have been infected with the SARS-CoV-2 virus, and >1.39 million individuals have died (https://covid19.who.int/, last accessed November 24, 2020). Among patients with chronic illness, including patients with kidney failure and those with kidney transplants, the impact is even more substantial. The estimated incidence of SARS-CoV-2 infection and COVID-19 in patients on dialysis and with kidney transplants exceeds that of the general population by as much as 15-fold.1 The risk of complications and death associated with COVID-19 is also considerably higher among kidney transplant recipients.2 Reasons for the observed differences between transplant recipients and the general population may be attributed to multiple comorbidities, and the suppressed immune system in these vulnerable patients.
Sex as a risk factor for COVID-19 infection and outcomes in transplant recipients
Sex (a biologically determined variable defined by genetics, hormones, and anatomy) may impact outcomes in kidney transplantation and may also affect survival from SARS-CoV-2 infection and COVID-19. The incidence of COVID-19 in the general population is overall similar between the sexes, with sex variation within different countries possibly reflecting differential sex-biased access to testing. Likewise, accounting for the higher proportion of transplant recipients who are male, the incidence of COVID-19 after kidney transplantation also appears to be similar in both sexes.1 However, after controlling for age and comorbidities, COVID-19–attributable mortality rates in the general population are 1.5-fold to 2.0-fold higher in males than females.3 In contrast, although kidney transplantation has been associated with as much as a 10-fold higher mortality with COVID-19 compared with the general population,2 no consistent sex differences in COVID-19–related mortality have been observed in kidney transplant recipients.1 Although sex differences in case fatality rates in the transplant population may emerge as more data accumulate, the apparent lack of sex differences in case fatality rates in transplant patients to date may reflect sex-related differences in the effects of immunosuppression.
Mechanistic pathways of sex differences in COVID-19 outcomes in transplant recipients
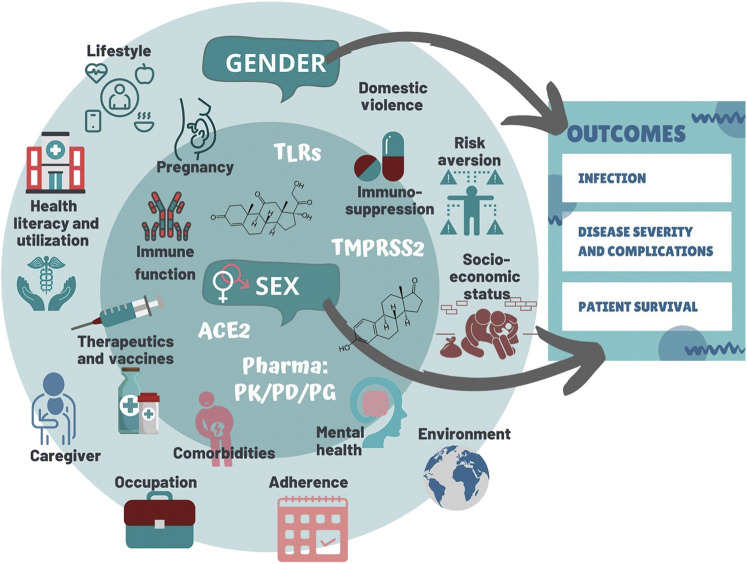
SARS-CoV-2 infection has 2 distinct phases: initial viral infection and subsequent systemic inflammatory and endothelial responses. The immune dysregulation by SARS-CoV-2 infection may be a consequence of the zoonotic origin of this virus, and therefore, sex differences may be more prominent compared with other infections. In general, females generate a greater innate and adaptive antiviral immune response than males, owing in part to estrogens increasing T-cell and antibody responses, and to the potential for females to express greater numbers of X-linked immune-related genes due to incomplete X-inactivation.4 Therefore, immunocompetent females may demonstrate enhanced local clearance of viruses when compared with males (Figure 1 ).4 Conversely, SARS-CoV-2 clearance may be relatively impaired in males, in part due to the immune-suppressing properties of testosterone. As testosterone levels decline in older age, however, males begin to experience more dysregulated innate immunity and inflammatory pathology (“inflamm-aging”)3 as well as reduced adaptive immunity compared with age-matched females. These findings correspond with the higher likelihood among older immunocompetent males than females of a catastrophic dysregulated immune response to COVID-19 (i.e., “cytokine storm”) and death. Emerging evidence suggests a potential role for type I interferons in protecting against SARS-CoV-2 infection, with patients having neutralizing anti-interferon autoantibodies experiencing more severe disease. Although, in general, autoimmunity is more frequently observed in females, autoantibodies against type I interferon have been shown to be more common in SARS-CoV-2 infected males.5 In the transplant population, immunosuppression may lead to decreased viral clearance.4 Yet, at the same time, immunosuppression may paradoxically protect against fatal immune dysregulation in the second phase of infection. The significantly lower 28-day mortality in patients with severe COVID-19 courses treated with dexamethasone in the Randomised Evaluation of COVID-19 Therapy (RECOVERY) trial6 supports this notion. Interestingly, although the interaction between sex and steroid therapy did not reach statistical significance, the survival benefit demonstrated with dexamethasone was primarily observed in males. The apparent lack of a higher COVID-19–related mortality risk in male than female transplant recipients may be similarly explained by the effect of maintenance immunosuppression dampening down the dysregulated inflammatory effects observed more commonly in immunocompetent males than females. Calcineurin inhibitors, the cornerstone of maintenance immunosuppressive therapy in transplant patients, are also being explored for their potential action against SARS-CoV-2 infection through inhibition of the immunophilin pathway (https://clinicaltrials.gov/ct2/show/NCT04341038). Sex differences in the pharmacokinetics and possibly the pharmacodynamics of calcineurin inhibitors might contribute to the comparable COVID-19 mortality rates observed in male and female transplant recipients. These sex differences emphasize the need for clinical trials that allow sex-stratified analyses.
Figure 1.
The roles of sex, gender, and transplantation in coronavirus disease 2019 (COVID-19). ACE2, angiotensin-converting enzyme 2; PD, pharmacodynamics; PG, pharmacogenomics; PK, pharmacokinetics; TLR, toll-like receptor; TMPRSS2, transmembrane protease serine 2.
Gender, COVID-19, and transplantation
In addition to determining the impact of biologic sex on response to viral infection, it is also important to consider the role of gender (Figure 1)—a sociocultural construct relating to identities, norms, and behaviors—on viral exposure, access to care, and social impacts. Gender differences in risk and self-management behavior may have also contributed to the observed differences in survival by gender. People who identify as masculine may be more likely to smoke, may be more likely to display worse hand hygiene, and tend to be less health care seeking than individuals who identify as feminine. Conversely, individuals engaged in traditionally feminine occupations, like frontline health care workers and caregivers for the ill, are at a heightened risk for viral exposure. During the pandemic, women have been more likely to become unemployed, resulting in differential economic hardships for men and women.7 Furthermore, longer time at home due to social distancing and isolation measures has placed some people in vulnerable situations, with women being at a greater risk for experiencing domestic violence. Importantly, although individuals who identify as women are more likely to seek medical attention, they are less likely to be offered diagnostic testing and evidence-based treatment interventions than are those identifying as men.8
Although data in the transplant population are lacking, patients with rheumatic disease, many of whom are immunosuppressed, were nearly twice as likely to adhere to strict social distancing recommendations than were healthy controls. Likewise, one might expect that when contrasted with the general population, male transplant patients may be less vulnerable to the impacts of masculinity, as represented by behavioral choices due to a heightend awareness of their suppressed immune status and associated risks of contracting infections. Whether male transplant patients are more likely than male patients in the general population to participate in preventive strategies, adhere to social distancing, and exercise better hand hygiene requires further study.
Policy and research implications of COVID-19 in transplant recipients
The comparable mortality rates between male and female kidney transplant recipients may represent a relatively better survival in transplanted males in contrast to the male-biased mortality risk observed in the general population. Thus, thoughtful consideration of the impact of sex and gender on the pathogenesis, diagnosis, treatment, and prevention of COVID-19 in kidney transplant recipients has the potential to benefit personalized care and improve outcomes among transplant recipients. It is critical that future research allows for sex-disaggregated analyses in both observational and interventional studies. There are data to suggest a protective effect of endogenous estrogens on the immune response to the SARS-CoV-2 virus.7 Therefore, given the impact of age on levels of circulating sex hormones, it is also important that future research consider the potential modifying effects of age. Moreover, information regarding menopausal status and exogenous hormone replacement therapy (in cisgender and transgender individuals) may also be relevant and must be sought.
Early observations regarding sex differences in COVID-19 outcomes are important in the development of future preventive and treatment strategies. Females generally display superior vaccine efficacy compared with males but a higher rate of vaccine-related adverse outcomes.4 Among the list of promising drugs against COVID-19, historical data have shown that females may have a higher risk for medication-related complications than males, likely related to sex-mediated differences in pharmacokinetics, pharmacodynamics, body mass and composition, and drug bioavailability.9 For example, females are known to experience more hydroxychloroquine-associated QT prolongation and fatal ventricular arrhythmias than males.7 Although this therapy has been explored in clinical trials for the treatment of SARS-CoV-2 infection and COVID-19, no sex-stratified analyses have been planned. This risk may be further exaggerated in the setting of standard maintenance immunosuppressive therapy among transplant recipients as calcineurin inhibitors may further potentiate QT prolongation. Also, females may demonstrate an attenuated response to certain drugs, such as colchicine,7 which is being evaluated for the treatment of advanced COVID-19 in the large-scale Colchicine Coronavirus SARS-CoV2 Trial (COLCORONA; https://clinicaltrials.gov/ct2/show/NCT04322682). However, current and ongoing COVID-19 trials have not ensured sex-disaggregated data collection. More important, sex was not included as a stratifying variable during the randomization process. In clinical trials and observational studies, the lack of assessment and the lack of reporting on the impact of sex as intervention modifiers have posed major impediments in understanding the biology of sex differences in response to treatments. Females have also been traditionally underrepresented in randomized controlled trials, and only a minority of COVID-19–related clinical trials include equal representation of both sexes. We strongly recommend that the potential impact of sex on vaccine responses and on specific drug-drug interactions, especially in immunosuppressed patients, requires consideration when designing clinical trials.
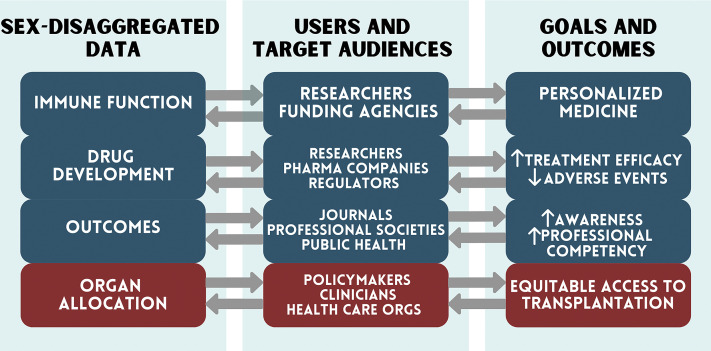
No less important is evaluation of the role gender may play in outcomes relating to SARS-CoV-2 infection. Transplant patients represent a vulnerable population experiencing a high comorbidity burden, warranting more rigorous social distancing than the general population, which also impacts access of these patients to services and limits their return to work. This might affect individuals identifying as women and men differently. COVID-19 introduces a novel stressor to the health care system, which may lead to delays in the provision of routine or scheduled care related to recipient and/or living-donor assessment and transplantation surgery. Operations may be delayed, potentially impacting the prospects of survival and/or morbidity on the waiting list, which can also differ by sex. There is a need for tailored preventive strategies that are sex and gender sensitive. Globally, women make up >70% of health and social frontline workers, such as nurses, midwives, social workers, cleaners, and laundry workers. We need equitable strategies that specifically address the social and economic impact of COVID-19 and support women within the health sector to build resilience and independence in managing their own health during this pandemic. Policymakers also need to take this gender divide into account to guarantee the safety, recognition, and support of essential health care workers involved in the care of patients with kidney disease and transplantation. This includes ensuring adequate access to personal protective equipment that accommodates both male and female anatomical differences and user preference. Finally, testing for COVID-19 and sex-stratified evidence-based treatments must be offered equally to men and women. A selection of policy considerations, targeted stakeholders, and the potential benefits to kidney transplant patients is shown in Figure 2 .
Figure 2.
Summary of proposed policy changes, targeted stakeholders, and benefits to the individual patient.
In conclusion, differences in sex- and COVID-19–related mortality between kidney transplant recipients and the general population may enhance our evolving understanding of COVID-19 pathophysiology and disease management. Biological sex differences impact the incidence of infection, disease course, and treatment; these may be further modulated by gendered factors, affecting exposure and participation in care. The health crisis precipitated by COVID-19 forces us to consider the impact of sex and gender in our transplant patients. Even when COVID-19 is brought under control, stepping up to the challenge of providing tailored care for individual kidney transplant patients requires continued consideration of sex and gender in study design, conduct, analysis, and reporting of fundamental as well as observational and interventional clinical research.
Disclosure
All the authors declared no competing interests.
Acknowledgements
This article is a product of initiatives by Women in Transplantation, The Transplantation Society. RS-P is supported by a Fonds de recherche du Quebec—Santé chercheur boursier clinician award (grant no. 254386) and CIHR grant FRN-156730.
References
- 1.Elias M., Pievani D., Randoux C., et al. COVID-19 infection in kidney transplant recipients: disease incidence and clinical outcomes. J Am Soc Nephrol. 2020;31:2413–2423. doi: 10.1681/ASN.2020050639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jager K.J., Kramer A., Chesnaye N.C., et al. Results from the ERA-EDTA Registry indicate a high mortality due to COVID-19 in dialysis patients and kidney transplant recipients across Europe. Kidney Int. 2020;98:1540–1548. doi: 10.1016/j.kint.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marquez E.J., Trowbridge J., Kuchel G.A., et al. The lethal sex gap: COVID-19. Immun Ageing. 2020;17:13. doi: 10.1186/s12979-020-00183-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klein S.L., Dhakal S., Ursin R.L., et al. Biological sex impacts COVID-19 outcomes. PLoS Pathog. 2020;16 doi: 10.1371/journal.ppat.1008570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bastard P., Rosen L.B., Zhang Q., et al. Autoantibodies against type I IFNs in patients with life-threatening COVID-19. Science. 2020;370 doi: 10.1126/science.abd4585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Group RC, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with Covid-19: preliminary report [epub ahead of print]. N Engl J Med. https://doi.org/10.1056/NEJMoa2021436. Accessed September 30, 2020.
- 7.Gebhard C., Regitz-Zagrosek V., Neuhauser H.K., et al. Impact of sex and gender on COVID-19 outcomes in Europe. Biol Sex Differ. 2020;11:29. doi: 10.1186/s13293-020-00304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tadiri C.P., Gisinger T., Kautzy-Willer A., et al. The influence of sex and gender domains on COVID-19 cases and mortality. CMAJ. 2020;192:E1041–E1045. doi: 10.1503/cmaj.200971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klein S.L. Sex influences immune responses to viruses, and efficacy of prophylaxis and treatments for viral diseases. Bioessays. 2012;34:1050–1059. doi: 10.1002/bies.201200099. [DOI] [PMC free article] [PubMed] [Google Scholar]