Abstract
Only a few studies investigated the impact of quarantine on anxiety of general population during a second wave of COVID-19 breakout. We aimed to compare anxiety levels of quarantined and non-quarantined people and investigate factors affecting anxiety during the second COVID-19 pandemic. A total of 1837 participants were included in this cross-sectional study. Anxiety was measured by the State-Trait Anxiety Inventory (STAI). Participants were divided into the quarantined group (QG) and non-quarantined group (Non-QG). The mean STAI-S score in the QG was significantly higher than Non-QG (41.8 ± 11.2 vs 40.01 ± 9.9), so was the proportion of severe state anxiety (11.6% vs 5.5%). Males in the QG were significantly more anxious than females evaluated by both STAI-S and STAI-T. High income was independent protective factors while moderate or bad health status and high trait anxiety level were independent risk factors for severe state anxiety. In conclusion, the COVID-19 confinement could significantly increase anxiety of quarantined people. Males were more vulnerable to the quarantine of COVID-19 with significantly increased anxiety level than females. The results suggest that attention should be paid to anxiety during a second round of quarantine due to COVID-19 and are of help in planning psychological interventions.
Keywords: Anxiety, COVID‐19, Mental health, Quarantine
Author statement
Thank you for your letter and for the reviewers’ comments concerning our manuscript entitled “Anxiety levels during a second local COVID-19 pandemic breakout among quarantined people: A cross sectional survey in China”. Those comments are all valuable and very helpful for revising and improving our paper, as well as the important guiding significance to our research studies. We have studied the comments carefully and have made corrections which we hope will meet with approval.
All authors have seen and approved the final version of the manuscript being submitted and have no conflict of interest.
1. Introduction
The COVID-19 which was first announced by the World Health Organization (WHO) on December 31, 2019, is now world spreading. Until September 4th, 2020, the total number of international reported cases surged to more than 26.7 million (WHO). Psychological problems associated with the COVID-19 pandemic are attracting increasing attention from psychologists, such as anxiety and depression symptoms in individuals caused by COVID-19 itself and forced quarantine measurements (Dubey et al., 2020). A large cross-sectional study conducted from February 2 to 7, 2020 in China reported that the prevalence of anxiety was 3.4% among workers in a factory and psychological interventions were required (X.-R. Zhang et al., 2020).
Quarantine has been used in many countries to combat COVID-19. During quarantine, people who have the possibility or have potentially been exposed to COVID-19 will be separated so as to reduce the risk of infecting others or being infected. One recent review reported negative psychological effects and longer quarantine time was a stressor (Brooks et al., 2020). There are a growing number of studies about the impact of social quarantine on anxiety on the general population of different countries (Campos JADB et al., 2020; Pieh C et al., 2020; Rossi R et al., 2020). A recent meta-analysis showed compelling evidence for adverse mental health effects of isolation and quarantine, in particular depression, anxiety, stress-related disorders (Jonathan H et al., 2020). This issue is becoming a matter of concern to psychologists.
The first round of COVID-19 outbreak had forced entire cities in China take mass quarantine. People had experienced social isolation during the first pandemic in the spring including Urumqi, capital city of Xinjiang Uygur Autonomous Region. However, from July 15th, Urumqi has experienced a second round of COVD-19 outbreak. The government immediately hit the “pause button” and took a series of lockdown measures including closing communities. After the quarantine was lifted three weeks, the epidemic had been averted. People in Urumqi and some other areas have been isolated at home or working place for more than 40 days again. Will this secondary quarantine affect people's anxiety level? Also, at present, the European countries are experiencing a second wave of outbreaks of COVID-19 (WHO). This subject becomes even more important. Enrico Rubaltelli reported two cross-sectional waves: at the beginning of the outbreak and once the national lockdown was imposed. But it was not about the second wave of COVID-19 pandemic (Enrico et al., 2020).
Till now, there are currently almost no studies focusing on the effect of COVID-19 pandemic on the mental state and anxiety levels of individuals during a second time of quarantine. The main objective of the study was to evaluate the factors affecting the people's psychology especially anxiety and to compare this with those of non-quarantined people who may have experienced only one time home confinement during the first nationwide pandemic. Although not as compelling as it should be because of the limitations of case studies, our study provided a detailed analysis and would help to identify people at high risk of anxiety during a second quarantine and provide issues of concern for counseling psychologists.
2. Methods
Study Design.
The cross-sectional study was carried out in the format of a ‘Questionnaire Star’ electronic questionnaire system (Changsha Haoxing Information Technology Co., Ltd., China) during 20–23, August 2020. ‘Questionnaire Star’ is an application dedicated to send electronic questionnaires through Wechat or web page (scanning the special two-dimensional code). The study protocol was conducted in accordance with the Helsinki Declaration as revised 1989 and was approved by the Ethics Committee of the Eighth People's Hospital of Xinjiang Uygur Autonomous Region. Informed consent was shown on the first page of the questionnaire and people in China who could see the questionnaire chose to participate in the study voluntarily. All surveys were anonymous. Each subject filled out the same set of questionnaires.
Some items (e.g. age, marriage, job) were also used to check for invalidity and ensure data quality. The inclusion criteria were being a Chinese citizen living in Mainland China and responding correctly. The exclusion criteria were: ①invalid responses; ②age≤18 years; ③ with a known psychiatric illness. The participants were divided into two groups: the quarantined group (QG) and non-quarantined group (Non-QG) according to their responses to the questionnaire: What kind of situation are you in now? Participants who answered ‘being quarantined’ were assigned to the QG group and those who responded ‘being non-quarantined’ were allocated to the Non-QG group.
2.1. Questionnaire design
This questionnaire included the following parts: ①Aim and informed consent; ②General information questionnaire; ③State-Trait Anxiety Inventory (STAI); ④COVID-19 impact questionnaire. The general information questionnaire included the sociodemographic and descriptive data about the participants: age, gender, ethnicity, marriage, education, occupation, income status and health status. The answers were presented as ordered or unordered categorical variables. In China, with the exception of the main ethnic Han nationality, the remaining ethnic groups are defined as ethnic minorities.
The State-Trait Anxiety Inventory questionnaire has two subscales: state (STAI-S) and trait (STAI-T) (Spielberger et al., 1970). STAI-S has 20 items and determines how the individual feels at a certain moment and under certain conditions. STAI-T has 20 items and generally determines how the participant feels regardless of the situation and circumstances. The scale was introduced and adapted China in 1988. In our study, we defined a STAI-S score above 53 or a STAI-T score above 55 as having severe anxiety (Wang et al., 1999).
The COVID-19 impact questionnaire consisted of questions about attitude and feelings on COVID-19 pandemic. The ten items of the questionnaire include: ①what is your attitude toward this round of COVID-19 pandemic; ②how much time each day is devoted to focusing on COVID-19; ③are you scared or confused about COVID-19 news; ④does your sleep quality become poorer; are your mood getting worse and irascible; ⑤do you feel lonely and depressed because lack of social activities; ⑥do you feel relaxed after the pandemic alleviated; ⑦how about your family relations during the outbreak; ⑧what is the main sources of your psychological stress. Items one–six were assessed on three levels from ‘low’ to ‘strong’ or ‘not accordant’ to ‘accordant’ or ‘usual’, ‘moderate’ or “never’. Item seven-nine had multiple choices. Some content of this questionnaire was not analyzed in this manuscript.
2.2. Statistical analysis
The data were analyzed with SPSS 20 program (Statistical Packagefor Social Sciences, IBM Inc., Chicago, IL, USA) and RStudio Desktop-1.3.1073 (Open source, 250 Northern Ave, Boston, MA, USA). Quantitative variables were expressed as the mean ± standard deviation (SD). Qualitative variables were expressed as numbers and percentages. Histogram and Kolmogorov-Smirnov test were used for normality distribution of the STAI scores. Independent Samples T-Test or One-way ANOVA was used to compare the averages of independent groups with normal distribution. Statistical significance was further subjected to post hoc analysis by Bonferroni's correction. Chi-square or Fisher's exact tests was used to compare categorical variables. Multivariate regression analyses were performed to determine the association between quarantine state and incidence of severe anxiety, excluding the interference of confounding factors arising from statistically significant differences in the incidence of severe anxiety between the two groups. Adjustments included age, gender, marital status, income, education, occupation and health status. The results are presented as adjusted odds ratio (aOR), and confidence intervals (95% CI). A p-value < 0.05 was used for statistical significance. All tests were two-tailed.
3. Results
A total of 1843 participants from 27 provinces of China completed the questionnaire and six were excluded because of matching our exclusion criteria. So the final sample size was 1837 including 869 in non-QG and 968 in QG. The questionnaire was conducted under the circumstance of that there had been more than four consecutive days without newly confirmed COVID-19 cases in Urumqi.
3.1. Demographic characteristics
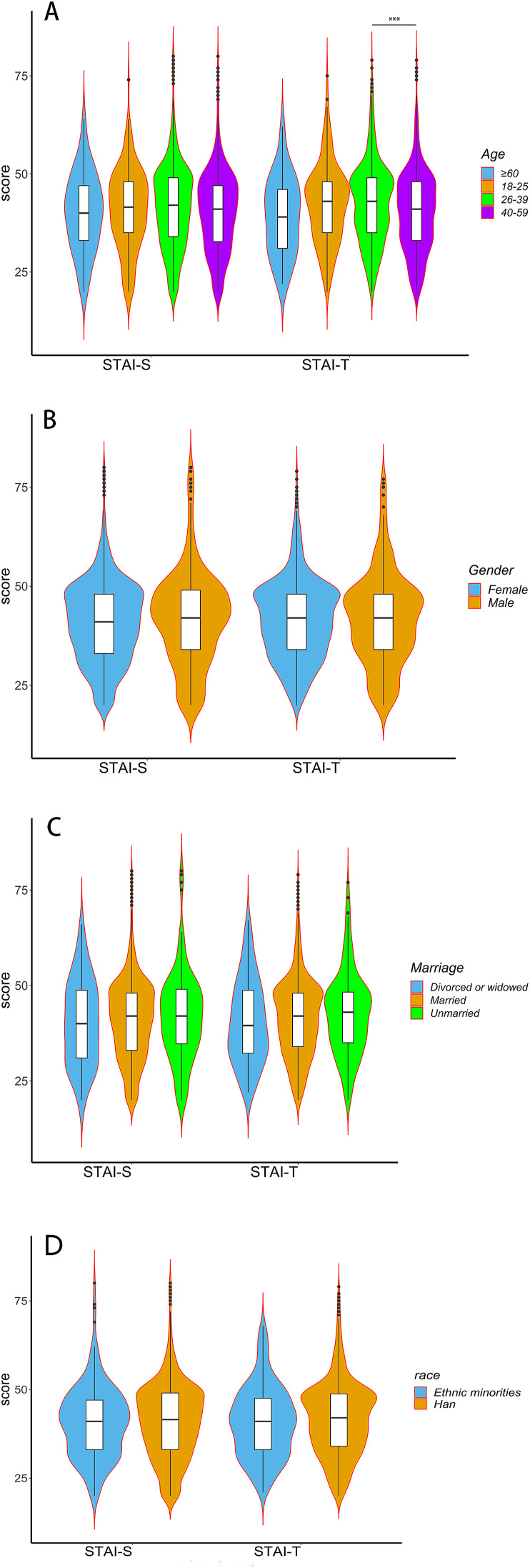
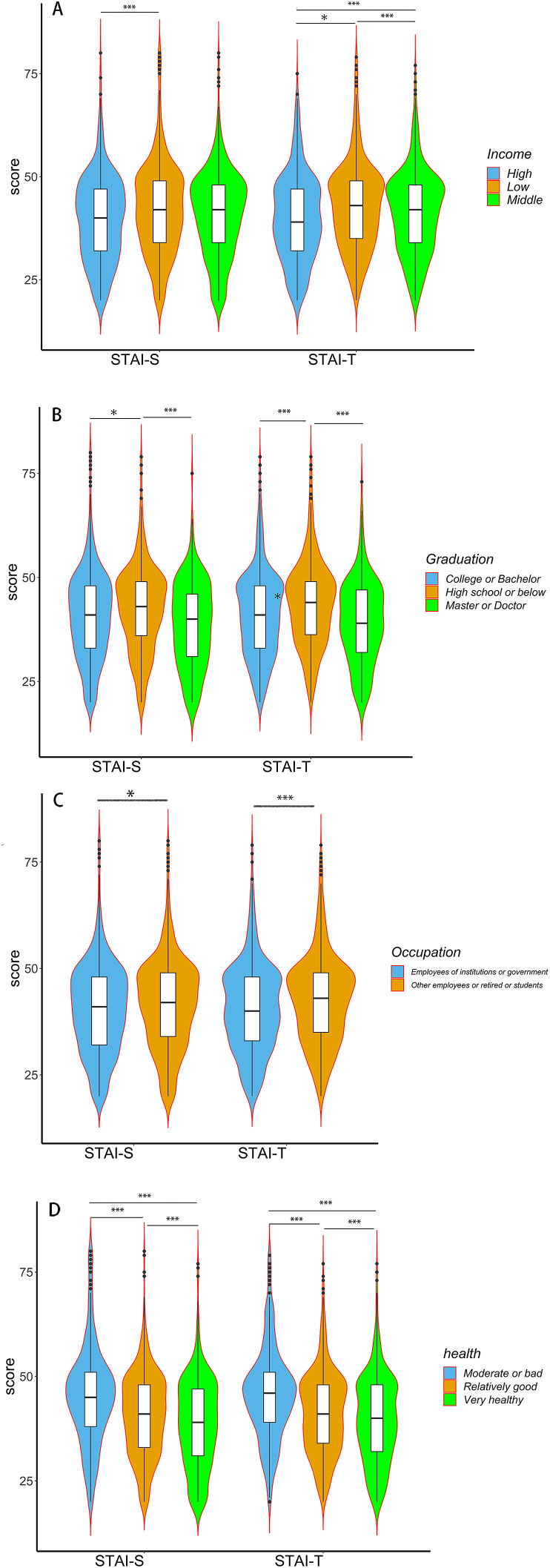
Fig. 1, Fig. 2 and Supplemental Table 1 summarized the demographic characteristics and anxiety levels of the total participants. The mean STAI-S score was 41.0 ± 10.7 and STAI-T score was 41.5 ± 10.4. The mean STAI-T score of the participants aged between 26 and 39 years was significantly higher than between 40 and 59 years (P < 0.001, Bonferroni analysis). There was no significant difference in STAI scores among different age, marital status and race. The mean STAI score of participants with higher income was significantly lower than with low income. 26.2% of the participants with a high school or lower education had significantly higher anxiety scores than people with college education or above (P = 0.001 for SATI-S and P < 0.001 for STAI-T). Employees of public institutions or government departments had significantly lower STAI scores than the other employees (P = 0.017 for SATI-S and P < 0.001 for STAI-T). Participants who felt they were generally in good health had significantly lower anxiety scores than participants who felt they were in poor health (P < 0.001 for both STAI scores).
Fig. 1.
Comparison of STAI scores of different age, gender, marital status and race. STAI-S, State-Trait Anxiety Inventory-State; STAI-T, State-Trait Anxiety Inventory-Trait. ***, P ≤ 0.001. No other significant differences were found between subgroups.
Fig. 2.
Comparison of STAI scores of different income, graduation, occupation and health status. STAI-S, State-Trait Anxiety Inventory-State; STAI-T, State-Trait Anxiety Inventory-Trait. *,0.01 < P < 0.05; ***, P ≦ 0.001.
3.2. Comparison of anxiety levels between the Non-QG and QG
Supplemental Table 1 displayed the group comparison of QG vs. non-QG including all characteristics variables. The distribution of ethnic minorities and Han Chinese between QG and non-QG groups (125/843 in QG and 90/779 in Non-QG, P = 0.089). Although there were significantly differences in the distribution of variables (P < 0.05) except ethnicity between the two groups, Table 1 showed the anxiety scores of the participants according to being quarantined or not, independent of the distribution. The mean STAI-S of all participants in the QG was significantly higher than those in the Non-QG (41.8 ± 11.2 vs 40.01 ± 9.9, P < 0.001), but not the STAI-T score. There were also no statistical differences in the STAI-T scores of participants having different age, income levels, education levels or health status. Unmarried participants showed significantly higher STAI-S and STAI-T scores in the QG than Non-QG. Participants, who were between 18 and 39 years of age, or with low income or education level above high school, or married, or very healthy, or were employees of institutions or government, had a significant higher STAI-S score in the QG than Non-QG. Both the STAI-S and STAI-T scores were significantly higher in the QG than Non-QG in male participants but not females (P < 0.001).
Table 1.
Comparison of STAI scores between the quarantined and non-quarantined groups.
| Characteristics | STAI-S Non QG (Mean ± SD) |
STAI-S QG (Mean ± SD) |
F | P | STAI-T Non-QG (Mean ± SD) | STAI-T QG (Mean ± SD) |
F | P |
|---|---|---|---|---|---|---|---|---|
| Total | 40.01 ± 9.9 | 41.8 ± 11.2 | 6.305 | <0.001 | 41.3 ± 9.9 | 41.7 ± 10.9 | 4.167 | 0.406 |
| Age(Y) | ||||||||
| 18–25 | 39.4 ± 9.7 | 43.1 ± 10.7 | 0.237 | 0.030 | 41.1 ± 9.7 | 44.3 ± 10.6 | 0.139 | 0.061 |
| 26–39 | 40.5 ± 10.1 | 43.1 ± 11.8 | 4.651 | <0.001 | 42.5 ± 10.5 | 43.2 ± 11.1 | 3.402 | 0.091 |
| 40–59 | 39.1 ± 9.4 | 40.8 ± 10.8 | 3.746 | 0.053 | 39.7 ± 9.7 | 40.5 ± 10.6 | 1.294 | 0.394 |
| ≥60 | 37.2 ± 8.4 | 41.4 ± 10.3 | 0.387 | 0.170 | 36.8 ± 7.9 | 40.3 ± 10.6 | 1.302 | 0.258 |
| Gender | ||||||||
| Female | 40.4 ± 9.9 | 41.2 ± 10.7 | 4.533 | 0.125 | 41.7 ± 9.9 | 41.2 ± 10.4 | 1.779 | 0.325 |
| Male | 37.9 ± 10.0 | 44.4 ± 12.7 | 1.049 | <0.001 | 38.9 ± 9.9 | 43.7 ± 12.4 | 2.38 | <0.001 |
| Marital status | ||||||||
| Unmarried | 39.4 ± 10.0 | 44.2 ± 12.6 | 1.254 | 0.002 | 41.0 ± 9.9 | 44.3 ± 11.8 | 0.906 | 0.022 |
| Married | 40.2 ± 9.9 | 41.5 ± 11.0 | 4.386 | 0.011 | 41.54 ± 9.9 | 41.4 ± 10.7 | 3.163 | 0.864 |
| Divorced or widowed | 35.7 ± 11.1 | 41.3 ± 11.0 | 0.008 | 0.072 | 36.2 ± 11.1 | 41.4 ± 10.7 | 0.009 | 0.083 |
| Income | ||||||||
| Low | 40.8 ± 10.1 | 42.7 ± 10.0 | 5.808 | 0.004 | 43.3 ± 11.9 | 43.1 ± 11.1 | 3.271 | 0.598 |
| Middle | 40.0 ± 9.5 | 41.0 ± 9.2 | 3.59 | 0.107 | 41.4 ± 10.8 | 41.4 ± 10.6 | 2.994 | 0.581 |
| High | 38.8 ± 10.0 | 39.7 ± 10.1 | 0.129 | 0.080 | 40.5 ± 10.9 | 40.2 ± 10.9 | 0.266 | 0.658 |
| Education | ||||||||
| High school or below | 41.9 ± 9.9 | 43.1 ± 10.7 | 1.086 | 0.212 | 43.7 ± 10.0 | 43.7 ± 10.4 | 0.063 | 0.982 |
| College or Bachelor | 39.7 ± 9.8 | 41.6 ± 11.4 | 6.647 | 0.003 | 40.8 ± 9.8 | 41.3 ± 10.9 | 4.451 | 0.427 |
| Master or Doctor | 37.6 ± 9.8 | 40.7 ± 10.6 | 0.015 | 0.036 | 38.7 ± 9.4 | 40.4 ± 10.9 | 0.604 | 0.259 |
| Occupation | ||||||||
| Employees of institutions or government | 39.0 ± 9.5 | 41.2 ± 11.2 | 6.560 | 0.002 | 40.0 ± 9.7 | 40.9 ± 10.8 | 3.165 | 0.211 |
| Other employees or retired or students | 40.7 ± 10.1 | 42.8 ± 11.1 | 0.997 | 0.003 | 42.2 ± 10.0 | 43.0 ± 10.8 | 1.388 | 0.231 |
| Health status | ||||||||
| Very healthy | 37.9 ± 10.1 | 39.8 ± 11.0 | 0.580 | 0.037 | 39.3 ± 9.9 | 39.9 ± 11.1 | 1.571 | 0.470 |
| Relatively good | 40.4 ± 9.4 | 40.9 ± 10.3 | 2.052 | 0.516 | 41.6 ± 9.7 | 40.7 ± 9.9 | 0.058 | 0.180 |
| Moderate or bad | 43.6 ± 9.9 | 46.2 ± 12.6 | 6.463 | 0.031 | 45.1 ± 9.4 | 45.9 ± 11.8 | 7.029 | 0.479 |
Notes. STAI-S, State-Trait Anxiety Inventory-State; STAI-T, State-Trait Anxiety Inventory-Trait; QG, quarantined group; Non-QG, non-quarantined group; Y, year. P values < 0.05 are in bold typeface.
The severe anxiety rate of the total participants was 8.7% (n:1837, STAI-S) and 7.6% (n:1837, STAI-T). To further compare the severity of anxiety between the two groups, we analyzed its incidence according to different factors (Table 2 ). Similarly, the proportion of severe anxiety measured by STAI-S was also significantly higher in the QG than Non-QG (11.6% vs 5.5%, P < 0.001), but not by STAI-T. Detailed analysis of the subgroups showed that only participants between the ages of 26 and 39 or male participants showed significant increases in the incidence of severe trait anxiety, but with no significant differences in the rest comparisons. However, the rates of severe state anxiety were significantly higher in the following subgroups: participants who were between 26 and 39 years of age, or with low income, or education level below bachelor, or married and unmarried. The total severe state anxiety rate of participants with college education or above was 4.5% (n: 62/1383).
Table 2.
Comparison of rates of severe anxiety between the quarantined and non-quarantined groups.
| Characteristics | Rate in Non-QG (STAI-S, %) | Rate in QG (STAI-S, %) | χ2 | P | OR(95%CI) | Rate in Non-QG (STAI-T, %) | Rate in QG (STAI-T,%) | χ2 | P | OR(95%CI) |
|---|---|---|---|---|---|---|---|---|---|---|
| Total | 5.5(48/869) | 11.6(112/968) | 21.119 | <0.001 | 0.446(0.314–0.634) | 6.7(59/869) | 8.3(80/968) | 1.425 | 0.233 | 0.809(0.570–1.147) |
| Sum | 8.7(160/1837) † | 7.6(139/1837) † | ||||||||
| Age(Y) | ||||||||||
| 18–25 | 5.6(5/89) | 10.5(6/57) | 0.273 | 0.506(0.147–1.743) | 7.9(7/89) | 12.3(7/57) | 0.377 | 0.610(0.202–1.841) | ||
| 26–39 | 5.7(32/561) | 10.3(58/361) | <0.001 | 0.316,(0.201–0.498) | 7.3(41/561) | 11.9(43/361) | 0.018 | 0.583(0.372–0.914) | ||
| 40–59 | 5.4(11/204) | 8.5(44/516) | 0.154 | 0.611(0.309–1.209) | 5.4(11/204) | 5.4(28/516) | 0.264 | 1.545(0.717–3.332) | ||
| ≥60 | 0(0/15) | 11.8(4/34) | 0.412 | NA | 0(0/15) | 5.9(2/34) | 0.860 | NA | ||
| Gender | ||||||||||
| Female | 5.9(43/734) | 10.2(79/778) | <0.001 | 0.472(0.320–0.695) | 7.1(52/734) | 6.6(51/778) | 0.683 | 1.087(0.728–1.622) | ||
| Male | 3.7(5/135) | 17.4(33/190) | <0.001 | 0.183(0.069–0.482) | 5.2(7/135) | 15.3(29/190) | 0.004 | 0.304(0.129–0.716) | ||
| Marital status | ||||||||||
| Unmarried | 4.3(5/115) | 17.4(19/109) | 0.002 | 0.215(0.077–0.599) | 8.6(10/115) | 13.8(15/109) | 0.229 | 0.597(0.256–1.392) | ||
| Married | 5.6(41/738) | 10.6(83/785) | <0.001 | 0.498(0.337–0.734) | 6.5(48/738) | 7.4(58/785) | 0.498 | 0.872(0.587–1.296) | ||
| Divorced or widowed | 12.5(2/16) | 13.5(10/74) | 1.000 | 0.914(0.180–4.641) | 6.3(1/16) | 9.5(7/74) | 1.000 | 0.638(0.073–5.582) | ||
| Income | ||||||||||
| Low | 6.3(23/363) | 14.8(49/322) | <0.001 | 0.377(0.224–0.634) | 8.0(29/363) | 9.3(30/322) | 0.536 | 0.845(0.495–1.442) | ||
| Middle | 5.4(13/241) | 9.9(43/434) | 0.042 | 0.518(0.273–0.985) | 4.6(11/241) | 5.1(22/434) | 0.125 | 0.581(0.288–1.172) | ||
| High | 4.5(12/264) | 9.4(20/212) | 0.034 | 0.457(0.218–0.958) | 7.2(19/264) | 8(17/212) | 0.736 | 0.890(0.450–1.757) | ||
| Education | ||||||||||
| High school or below | 6.5(17/262) | 12.0(23/192) | 0.018 | 0.464(0.243–0.885) | 9.5(25/262) | 12.0(23/192) | 0.264 | 0.707(0.384–1.302) | ||
| College or Bachelor | 5.9(27/455) | 4.4(31/711) | 0.001 | 0.477(0.304–0.750) | 18.2(83/455) | 7.5(53/711) | 0.680 | 0.908(0.573–1.437) | ||
| Master or Doctor | 2.6(4/152) | 0(0/65) | 0.442 | NA | 3.3(5/152) | 0(0/65) | 0.324 | NA | ||
| Occupation | ||||||||||
| Employees of institutions or government | 4.2(15/354) | 3.5(21/599) | 0.567 | 1.218(0.619–2.394) | 18(64/354) | 7.2(43/599) | 0.458 | 0.815(0.476–1.398) | ||
| Other employees or retired or students | 6.4(33/515) | 10.3(38/369) | 0.001 | 0.458(0.288–0.729) | 9.3(48/515) | 10.0(37/369) | 0.163 | 0.715(0.445–1.148) | ||
| Health status | ||||||||||
| Very healthy | 0.6(2/327) | 1.4(3/211) | 0.386 | 0.429,(0.071–2.587) | 1.2(4/327) | 1.9(4/211) | 0.718 | 0.644(0.159–2.603) | ||
| Relatively good | 2/398 | 7/541 | 4/398 | 11/541 | ||||||
| Moderate or bad | 144 | 216 | 144 | 216 | ||||||
Notes. STAI-S, State-Trait Anxiety Inventory-State; STAI-T, State-Trait Anxiety Inventory-Trait; QG, quarantined group; Non-QG, non-quarantined group; Y, year; NA, not applicable; CI, confidence interval; OR, odds ratio. P values < 0.05 are in bold typeface. † Sum of the two groups.
The score of anxiety in Non-QG was significantly lower in males than in females (P = 0.008 for STAI-S, P = 0.002 for STAI-T), but there was no significant difference in the proportion of severe anxiety (P = 0.314 for STAI-S, P = 0.420 for STAI-T). Males in the QG were significantly more anxious than females evaluated by both STAI-S and STAI-T. Male participants showed more susceptible to the quarantine of the COVID-19 (Table 3, Table 4 ).
Table 3.
Comparison of rates of severe anxiety evaluated by STAI-S between females and males.
| SATI-S | F | P | SATI-S | X2 | OR(95%CI) | P | |
|---|---|---|---|---|---|---|---|
| Non-QG | 1.196 | 0.008 | |||||
| Female | 40.4 ± 9.9 | 5.9(43/734) | 1.014 | 1.618(0.629–4.162) | 0.314 | ||
| Male | 37.9 ± 10.0 | 3.7(5/135) | |||||
| QG | 1.913 | <0.001 | 7.768 | 0.538(0.346–0.836) | 0.005 | ||
| Female | 41.2 ± 10.7 | 10.2(79/778) | |||||
| Male | 44.4 ± 12.7 | 17.4(33/190) |
Notes. STAI-S, State-Trait Anxiety Inventory-State; STAI-T, State-Trait Anxiety Inventory-Trait; QG, quarantined group; Non-QG, non-quarantined group; CI, confidence interval; OR, odds ratio. P values < 0.05 are in bold typeface.
Table 4.
Comparison of rates of severe anxiety evaluated by STAI-T between females and males.
| SATI-T | F | P | SATI-T | X2 | OR(95%CI) | P | |
|---|---|---|---|---|---|---|---|
| Non-QG | 0.613 | 0.002 | 0.650 | 1.94(0.619–3.138) | 0.420 | ||
| Female | 41.7 ± 9.9 | 7.1(52/734) | |||||
| Male | 38.9 ± 9.9 | 5.2(7/135) | |||||
| QG | 5.172 | 0.013 | 15.273 | 0.389(0.239–0.634) | <0.001 | ||
| Female | 41.2 ± 10.4 | 6.6(51/778) | |||||
| Male | 43.7 ± 12.4 | 15.3(29/190) |
Notes. STAI-S, State-Trait Anxiety Inventory-State; STAI-T, State-Trait Anxiety Inventory-Trait; QG, quarantined group; Non-QG, non-quarantined group; CI, confidence interval; OR, odds ratio. P values < 0.05 are in bold typeface.
After adjusting for age, gender, marital status, income, education, occupation and health status, quarantine was still statistically significantly associated with the incidence of severe anxiety based on STAI-S. Compared with the participants in Non-QG group, the participants in the QG had an aOR of 3.005 (95% CI, 1.773–5.093, P < 0.001) as shown in Table 5 . Moreover, high income was independent protective factors (P = 0.027) while moderate or bad health status was an independent risk factor for severe anxiety diagnosed by STAI-S and STAI-T (P < 0.001). A moderate or bad feeling of health increased the state anxiety 3.7 times and trait anxiety 4 times. Severe trait anxiety was also a risk factor for severe state anxiety (P < 0.001).
Table 5.
Adjusted odds ratios of severe anxiety by multivariate analysis (after modification).
| Variable | aOR of STAI-S (95%CI) | P | aOR of STAI-T (95%CI) | P |
|---|---|---|---|---|
| Group | ||||
| Non-QG | 1 | 1 | ||
| QG | 3.005 (1.773–5.093) | <0.001 | 1.453(0.977–2.161) | 0.065 |
| Age(Y) | ||||
| 40–59 | 1 | 1 | ||
| 18–25 | 0.679 (0.216–2.136) | 0.508 | 2.660(1.135–6.237) | 0.024 |
| 26–39 | 1.540 (0.899–2.640) | 0.116 | 2.754(1.743–4.351) | <0.001 |
| ≥60 | 1.624 (0.459–5.741) | 0.452 | 0.634(0.144–2.788) | 0.547 |
| Gender | ||||
| Female | 1 | 1 | ||
| Male | 1.271 (0.698–2.314) | 0.433 | 2.125(1.362–3.315) | 0.001 |
| Marital status | ||||
| Unmarried | 1 | 1 | ||
| Married | 0.797 (0.351–1.811) | 0.588 | 0.631(0.345–1.155) | 0.135 |
| Divorced or widowed | 1.229 (0.369–4.086) | 0.737 | 0.965(0.363–2.561) | 0.943 |
| Income | ||||
| Low | 1 | 1 | ||
| Middle | 0.629 (0.372–1.066) | 0.085 | 0.870(0.558–1.356) | 0.539 |
| High | 0.480 (0.251–0.919) | 0.027 | 1.267(0.768–2.092) | 0.354 |
| Education | ||||
| High school or below | 1 | 1 | ||
| College or Bachelor | 1.974 (1.073–3.631) | 0.029 | 0.718(0.450–1.147) | 0.166 |
| Master or Doctor | 0.990 (0.321–3.049) | 0.986 | 0.320(0.139–0.733) | 0.007 |
| Occupation | ||||
| Employees of institutions or government | 1 | 1 | ||
| Other employees or retired or students | 1.295 (0.776–2.162) | 0.323 | 1.010(0.657–1.553) | 0.965 |
| Health status | ||||
| Very healthy | 1 | 1 | ||
| Relatively good | 1.589 (0.869–2.908) | 0.133 | 1.333(0.830–2.143) | 0.234 |
| Moderate or bad | 3.726 (1.908–7.275) | <0.001 | 4.042(2.428–6.729) | <0.001 |
| STAI-T | ||||
| No | 1 | |||
| Yes | 82.752(48.636–140.800) | <0.001 | ||
Notes. STAI-S, State-Trait Anxiety Inventory-State; STAI-T, State-Trait Anxiety Inventory-Trait; QG, quarantined group; Non-QG, non-quarantined group; Y, year; CI, confidence interval; OR, odds ratio. P values < 0.05 are in bold typeface.
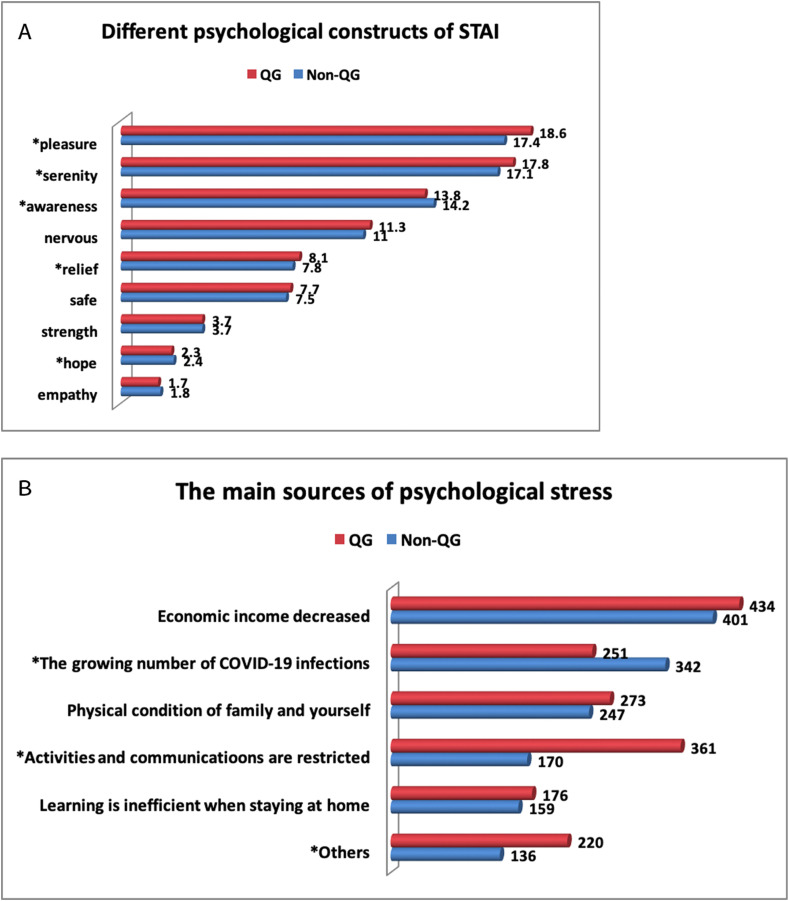
The different psychological components of STAI were shown in Fig. 3 A. The proportions of feeling pleasure, serenity and relief were significantly larger in the Non-QG than QG. The proportions of feeling awareness and hope were significantly larger in the QG than Non-QG.
Fig. 3.
STAI components and respond to questions about COVID-19 pandemic. QG, quarantined group; Non-QG, non-quarantined group; STAI-S, State-Trait Anxiety Inventory-State; STAI-T, State-Trait Anxiety Inventory-Trait. *P < 0.05. A) The bar numbers were the average STAI scores. B) The bar numbers were the number of people who chose this option.
3.3. Other psychological effects of the second COVID-19 confinement
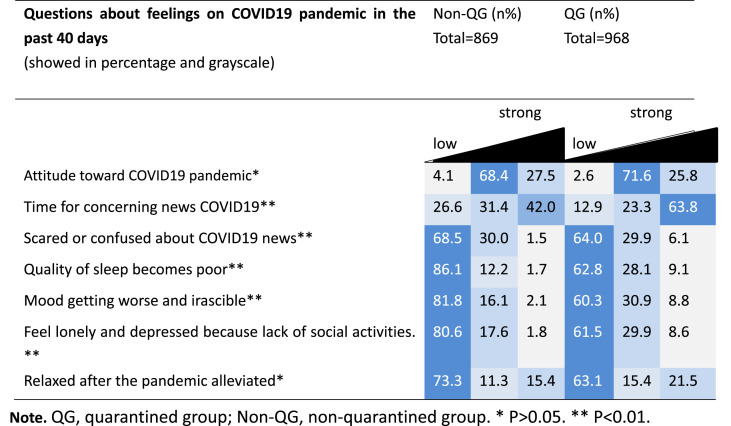
Table 6 summarized the other psychological findings of the study participants related to COVID-19 pandemic. There was a similar trend in the percentage of responses between the two groups. There were no significant difference in the attitude toward COVID-19 pandemic and the extent to feel relaxed after the pandemic alleviated between the two groups. However, participants in the QG paid significantly more time for concerning news COVID-19 (P < 0.001), and were more scared or confused about COVID-19 news (P = 0.001), and also had a mood toward getting worse and irascible (P < 0.001). Quality of sleep became significantly poorer in the QG (P < 0.001). The proportion of participants feeling lonely and depressed in the QG was significantly different than Non-QG (P < 0.001). Fig. 3B showed that the main source of psychological stress was from decreased income and the increased number of COVID-19 infections in the Non-QG (85.5%) and decreased income and significantly restricted communications and activities in the QG (82.1%).
Table 6.
Summary of the responses on the emotional and somatic state.
Note. QG, quarantined group; Non-QG, non-quarantined group. *P > 0.05. **P < 0.01.
4. Discussion
The present study found that the COVID-19 confinement during the second breakout in Urumqi could significantly increase anxiety of quarantined people. The anxiety level of women in the Non-QG was higher than that of men, but males were more vulnerable and susceptible to the quarantine of the COVID-19 with significantly increased anxiety. Bad health status was another risk factor for increased severe anxiety during isolation. Quarantine also cause sleep problems and depression. Reduced income, increased COVID-19 infections and severe restrictions were the main causes of stress.
The COVID-19 epidemic is accelerating rapidly in multiple countries. We should beware of the second wave of COVID-19 (Xu et al., 2020). One study predicted that the second wave of would be most severe than the first one (Behzad G., 2020). Now, a second wave is creeping back in Europe. In China, the first wave of COVID-19 was nationwide, while the second wave was restricted to local regions like Urumqi with extremely decreased infected patients. But the severity of the quarantine measures was similar during the two outbreaks in Urumqi.
To our knowledge, this is the first study designed to investigate the psychological impact by a second wave of social isolation in a local breakout region with sporadic cases reported in other provinces in China. The results suggest that attention should be paid to anxiety symptoms during quarantine. The results shared in this article may be useful for other countries that may encounter second wave of COVID-19.
Quarantine was associated with anxiety and COVID-19 related stressful life event in the Italian general population three to four weeks into the COVID-19 pandemic and lockdown measures (Rossi et al., 2020). Our survey was conducted during the late stage of city lockdown when there were no newly occurred COVID-19 infected cases reported in Xinjiang. Despite that, our results showed that quarantined participants still reported high levels of anxiety, and were in line with recently published reports on mental health outcomes during the COVID-19 pandemic (Lai et al., 2020; Mosheva et al., 2020). The distribution and anxiety levels of different ethnic groups were similar in the QG and Non-QG groups. STAI-S scores are closely related to stressful events and COVID-19 pandemic may increase state anxiety and hopelessness. The severe anxiety incidence (8.7% assessed as STAI-S>53) was similar with Zhao's report from China, that people living in high epidemic area presented significantly higher incidence of severe anxiety compared to those in low epidemic area (9.49% vs 3.21%) (Zhao et al., 2020).
Our study found that the trait anxiety level at the age of 26–39 was significantly higher than that of 40–59 years old. Also the state anxiety level of participants between 26 and 39 years of age was significantly higher in the QG than Non-QG. This may be because people aged 26–39 years usually have much heavier burden in life and work, while those in the 40–59 years of age tend to be successful or in a more stable work-life situation. One study also reported that during COVID-19 pandemic in China people aged between 21 and 40 years old are in a more vulnerable position regarding their mental health status than other age groups (Ahmed MZ et al., 2020).
One of our novel findings was that male participants were more vulnerable and susceptible to the quarantine measurement while female participants were more resistant to quarantine, although the in the Non-QG the anxiety level of men was significantly lower than that of women. Given the proposal of gender schema theory and social role theory, men and women are predisposed to experience social anxiety during quarantine differently. However, the conclusions of gender differences about anxiety to COVID-19 pandemic remain controversial. Hacimusalar reported that having a female gender increased the anxiety 1.81 times (Hacimusalar et al., 2020). Michael L Tee also reported that female gender was associated with high level of stress and anxiety (Tee et al., 2020). But Zhao reported that there was no significant difference of anxiety in participated males and females (Zhao et al., 2020). The above studies did not distinguish between quarantined and non-quarantined states and were at different phases of the COVID-19 epidemic in different countries. It has been reported that anxiety is one emotion that men and women experience differently. Gender differences are partially determined by social roles and gender roles. Different attributes are attached to femininity and masculinity in the culture. Our findings showed that in China, women had a higher anxiety level at a non-quarantine state than mem while men were particularly at risk to experience anxiety disorders at a quarantine state. This may be because usually men's income is the main source of household income in China, so they are more likely to worry about the dangers of falling incomes from segregation. Women's levels of anxiety also increased in the QG, but were not so much as men's. This was perhaps because men could share some of the responsibility for caring for the family during home confinement. The social and gender roles had changed due to quarantine in China. However, men were more anxious in the QG group than the Non-QG group showed by both STAI-S and STAI-T scores in Table 1. Because there were no significant difference in the trait anxiety scores in the QG and Non-QG totally, we think that our results in Table 1 could also demonstrate that quarantine situation might influence both state and trait anxiety levels in males.
Our findings on marital status showed that divorced and widowed individuals presented similar levels of anxiety in the QG and Non-QG. But unmarried and married people showed significantly increased severe anxiety level in the QG than in the Non-QG. This could be related to age or pressure from a family's lower income. We also found that the incidence of severe anxiety and STAI scores in low-income group were significantly increased in the QG. From Fig. 1, Fig. 2 we could see a trend of negative correlation of income level and STAI scores. In China, low-income people usually have unstable jobs and are vulnerable to COVID-19. For example, if they were farmers, crops affected by traffic would not easy be sold, which could increase their anxiety. Our result presented that the incidence of severe anxiety of participants with college education or above was 4.5%, which was higher than reported rates of 0.9% (Cao et al., 2020). This inconsistence could be due to the particular population investigated.
Financial loss can be a problem during quarantine related cessation of work and appear to be a risk factor for symptoms of psychological disorders like anxiety several months after quarantine (Samantha et al., 2020). As shown in Fig. 3B, income reduction was the biggest source of stress for both groups. The significantly increased rate of severe state anxiety in the employees of non-government in the QG may also be due to change of financial problems. However, in STAI-T, we found no significant differences in characteristic anxiety between the QG and non-QG subgroups across different marital status, education, income, occupational and health subgroups, considering that STAI-T reflects ordinary emotional experience. We suggested that efforts to increase the economic income of the isolated population, or to provide financial compensation, can help to alleviate their anxiety.
Many studies have analyzed the multiple risk factors for anxiety caused by COVID-19 breakout. Hyland P reported that anxiety or depression was associated with younger age, female sex, loss of income due to COVID-19, COVID-19 infection and higher perceived risk of COVID-19 infection (Hyland et al., 2020). Another study found that was no significant association between occupation, income and anxiety among population during the outbreak of COVID-19 in Kurdistan Region of Iraq(Blbas et al., 2020). However, there were few studies focusing on the factors that may affect anxiety of quarantined people. In our study, we found that after the multivariate regression analysis, quarantine was still statistically significantly associated with the incidence of severe state anxiety. The other risk factors include high trait anxiety level and bad health status. So the observed state anxiety effects are resulting not only from trait differences. Bad health status was a very strong risk factor for state anxiety. It is known that people who are in poor health tend to be more concerned about their health and have higher levels of anxiety. A lack of well-being contributes significantly to the high score on the STAI (Kvaal K et al., 2001).
Although pandemic diseases were found to be associated with high-level anxiety in many studies, the mechanism underlying certain processes is still unclear. Psychological distance may serve as a mediator to explain the relationship between pandemic severity and social anxiety in pandemic regions base on a Stimulus-Organism-Response model (Lei Z et al., 2020). This is in line with the construal level theory. If participants of Non-QG perceived the COVID-19 at a remote distance, they tend to construe the virus at a high level with less emotional responses, thus exhibiting lower levels of anxiety (Blbas et al., 2020). Behaviors like sleep became significantly poorer in the QG, consistent with Casagrande's study (Casagrande et al., 2020).
To help people at high risk of anxiety to relax, we psychological expert should give proper and timely guidance. Building awareness and telling people that what makes stressful is not the stressful event itself but how we perceive it. To cultivate positive emotions, adjust lifestyle, like through exercise and meditation, will help the quarantined people better perceive their thoughts and emotions, connect with their bodies, and release anxiety.
Through the analysis of different psychological states, we found that after being isolated not only uneasy emotions, but hope and subjective awareness of the rise. According to Schacht-Singh's theory, emotional state is the result of the joint action of cognitive process, physiological state and environmental factors. This isolation, with the active response of the government, synchronous support of the society and full cooperation of the residents, is extremely effective for the prevention and control of bad emotions. That may explain why the proportions of the responses toward COVID-19 pandemic showed similar patterns in the grayscale diagram in Table 6.
On the other hand, there is the positive impact of containment measures on the COVID-19 epidemic. A more stringent confinement of people in high risk areas seem to have a potential to slow down the spread of COVID-19 (Lau H et al., 2020). Lockdown could buffer social anxiety caused by COVID-19 (Lei Z et al., 2020). As most QG participants experienced isolation for the second time, the basic needs of residents were guaranteed, the group effect was fully exerted, and the intervention was relatively successful, which alleviated anxiety to some extent.
Our research has some limitations. First, this study employed a cross-sectional design. Follow-up data was not included. Although the sample size is relatively large, it may have sampling bias due to internet access issues. One of them was that most of the variables between the two groups were unevenly distributed. Second, although these inventories are widely used in previous studies, self-reported measurements may run the risk of responses being influenced by participants’ moods and also cause could introduce a systematic bias. Third, we did not do the survey during the first breakout period, and could not compare the differences of mental status and risk factors of anxiety between the two periods of quarantine to help counseling psychologists to make adjustments. However, since many countries are experiencing the second wave of COVID-19 pandemic, we suggested psychologists to conduct comparative studies about this issue. Future research should investigate whether prolonged quarantine will have long-term impact on mental and psychological health (Pera A. 2020).
Our research may serve as a reminder to other countries that mental health issues still need to be addressed after the first and second outbreaks are contained. These data help to develop psychological intervention plans for different subgroups of the general public during and after COVID-19 outbreaks. From a clinical perspective, this means that counseling psychologists should pay more attention to vulnerable groups, especially those with high levels of state anxiety. Individual counseling or group counseling can be used.
Conclusion
The COVID-19 confinement could significantly increase anxiety of quarantined people. Males were more vulnerable to the quarantine of COVID-19 with significantly increased anxiety level than females. Health status was a very strong influencing factor on state anxiety. Participants with bad health or reduced income should be taken care of. The results suggest that attention should be paid to anxiety during a second round of quarantine due to COVID-19 and are of help in planning psychological interventions.
Declaration of competing interest
None.
Acknowledgments
This study was supported by the National Key Research and Development Program of China (2018YFC1004800) and the National Natural Science Foundation of China (82071617). The authors thank Dr. Lin Zhang from Maternal and Child Health Care Hospital of Shandong Province, Shandong University for help in statistics.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2020.12.067.
Credit author statements
All authors contributed, reviewed, and approved the final manuscript.
Lei Yan: Conceptualization, Methodology, Software, Review & Editing.
Lili Chen, Hua Zhao, Delnur.Razin, Tingting Song, Yan Wu, Xiaopei-Ma, Huerxida.Aji and Gang Wang: Investigation, Data curation.
Manli Wang: Supervision.
Lili Chen: Original draft preparation, Writing- Reviewing and Editing.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Ahmed M.Z., Ahmed O., Aibao Z., Hanbin S., Siyu L., Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J Psychiatr. 2020;51:102092. doi: 10.1016/j.ajp.2020.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behzad G. On forecasting the spread of the COVID-19 in Iran: the second wave. Chaos, Solit. Fractals. 2020;140:110176. doi: 10.1016/j.chaos.2020.110176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blbas H.T.A., Aziz K.F., Nejad S.H., Barzinjy A.A. Phenomenon of depression and anxiety related to precautions for prevention among population during the outbreak of COVID-19 in Kurdistan Region of Iraq: based on questionnaire survey. Z Gesundh Wiss. 2020:1–5. doi: 10.1007/s10389-020-01325-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/s0140-6736(20)30460-8. 10227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatr. Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos J.A.D.B., Martins B.G., Campos L.A., Marôco J., Saadiq R.A., Ruano R. Early psychological impact of the COVID-19 pandemic in Brazil: a national survey. J. Clin. Med. 2020;9(9):E2976. doi: 10.3390/jcm9092976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casagrande M., Favieri F., Tambelli R., Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubey S., Biswas P., Ghosh R., Chatterjee S., Dubey M.J., Chatterjee S., Lahiri D., Lavie C.J. Psychosocial impact of COVID-19. Diabetes Metab Syndr. 2020;14(5):779–788. doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enrico Rubaltelli, Elisa Tedaldi, Noemi Orabona, Sara ScriminBr. Environmental and psychological variables influencing reactions to the COVID-19 outbreak. J Health Psychol Sep. 2020;19 doi: 10.1111/bjhp.12473. 10.1111/bjhp.12473. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacimusalar Y., Kahve A.C., Yasar A.B., Aydin M.S. Anxiety and hopelessness levels in COVID-19 pandemic: a comparative study of healthcare professionals and other community sample in Turkey. J. Psychiatr. Res. 2020;129:181–188. doi: 10.1016/j.jpsychires.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland P., Shevlin M., McBride O., Murphy J., Karatzias T., Bentall R.P., Martinez A., Vallières F. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta Psychiatr. Scand. 2020 doi: 10.1111/acps.13219. 2020 Jul 27. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- Jonathan Henssler, Friederike Stock, Joris van Bohemen, Henrik Walter, Andreas Heinz, Lasse Brandt. Mental health effects of infection containment strategies: quarantine and isolation-a systematic review and meta-analysis. Eur. Arch. Psychiatr. Clin. Neurosci. 2020 doi: 10.1007/s00406-020-01196-x. Oct 6;1-12.Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kvaal K., Laake K., Engedal K. Psychometric properties of the state part of the Spielberger State-Trait Anxiety Inventory (STAI) in geriatric patients. Int. J. Geriatr. Psychiatr. 2001;16(10):980–986. doi: 10.1002/gps.458. [DOI] [PubMed] [Google Scholar]
- Lau H., Khosrawipour V., Kocbach P., Mikolajczyk A., Schubert J., Bania J., Khosrawipour T. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J. Trav. Med. 2020;27(3) doi: 10.1093/jtm/taaa037. taaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease. JAMA Netw Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei Z., Miao M., JiYoon L., Maorui L., Shu N., Xiaojun Z. International journal of environmental research and public health is lockdown bad for social anxiety in COVID-19 regions?: a national study in the SOR perspective. Int. J. Environ. Res. Publ. Health. 2020;17(12):4561. doi: 10.3390/ijerph17124561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosheva M., Hertz-Palmor N., Dorman Ilan S., Matalon N., Pessach I.M., Afek A., Ziv A., Kreiss Y., Gross R., Gothelf D. Anxiety, pandemic-related stress and resilience among physicians during the COVID-19 pandemic. Depress. Anxiety. 2020 doi: 10.1002/da.23085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pera Aurel. Cognitive, behavioral, and emotional disorders in populations affected by the COVID-19 outbreak. Front. Psychol. 2020;11:2263. doi: 10.3389/fpsyg.2020.02263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieh C., O Rourke T., Budimir S., Probst T. Relationship quality and mental health during COVID-19 lockdown. PloS One. 2020;15(9) doi: 10.1371/journal.pone.0238906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F., Di Marco A., Rossi A., Siracusano A., Di Lorenzo G. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psychiatr. 2020;11:790. doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger C.D., Gorsuch R., Lushene R. Consulting Psychologists Press; Palo Alto, CA: 1970. STAI Manual for the State-Trait Anxiety Inventory. [Google Scholar]
- Tee M.L., Tee C.A., Anlacan J.P., Aligam K.J.G., Reyes P.W.C., Kuruchittham V., Ho R.C. Psychological impact of COVID-19 pandemic in the Philippines. J. Affect. Disord. 2020;277:379–391. doi: 10.1016/j.jad.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Wang X., Ma H. Supplemental Edition. Chinese Journal of Mental Health; Beijing: 1999. Handbook of Mental Health Rating Scale (Revised Edition) pp. 205–209. [Google Scholar]
- Xu S., Li Y. Beware of the second wave of COVID-19. Lancet. 2020;395:1321–1322. doi: 10.1016/S0140-6736(20)30845-X. 10233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Huang Q., Wang X., Cheng X., Li Z., Wang Z., Zhong W., Liu D., Shen D., Chen P., Song W., Wu X., Yang X., Mao C. Prevalence of anxiety and depression symptoms, and association with epidemic-related factors during the epidemic period of COVID-19 among 123,768 workers in China: a large cross-sectional study. J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao H., He X., Fan G., Li L., Huang Q., Qiu Q., Kang Z., Du T., Han L., Ding L., Xu H. COVID-19 infection outbreak increases anxiety level of general public in China: involved mechanisms and influencing factors. J. Affect. Disord. 2020;276:446–452. doi: 10.1016/j.jad.2020.07.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.