Abstract
A novel SARS-like coronavirus (severe acute respiratory syndrome-related coronavirus-2, SARS-CoV-2) outbreak has recently become a worldwide pandemic. Researchers from various disciplinary backgrounds (social to natural science, health and medicine, etc.) have studied different aspects of the pandemic. The current situation has revealed how the ongoing development of nanotechnology and nanomedicine can accelerate the fight against the novel viruses. A comprehensive solution to this and future pandemic outbreaks includes preventing the spread of the virus through anti-viral personal protective equipment (PPE) and anti-viral surfaces, plus efforts to encourage behavior to minimize risks. Studies of previously introduced anti-viral biomaterials and their optimization to fight against SARS-CoV-2 is the foundation of most of the recent progress. The identification of non-symptomatic patients and symptomatic patients is vital. Reviewing published research highlights the pivotal roles of nanotechnology and biomaterials in the development and efficiency of detection techniques, e.g., by applying nanotechnology and nanomedicine as part of the road map in the treatment of coronavirus disease 2019 (COVID-19) patients. In this review, we discuss efforts to deploy nanotechnology, biomaterials, and stem cells in each step of the fight against SARS-CoV-2, which may provide a framework for future efforts in combating global pandemics.
Keywords: COVID-19, Coronavirus, SARS-COV-2, Biomaterials, Nanomaterials, Nanotechnology, Stem cells, Nanomedicine
Background and history
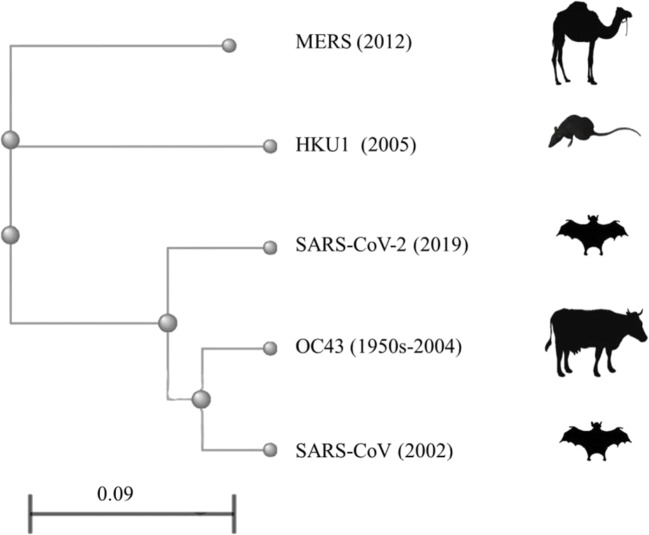
Coronaviruses are a group of related enveloped viruses with a large positive-sense single-stranded RNA genome. Betacoronaviruses (Beta-CoVs) is one of four genera (alpha, beta, gamma, and delta) of coronaviruses that cause respiratory tract infections in humans. Among Beta-CoVs, the utmost clinical concerns in humans include human CoV-OC43 and CoV-HKU1 (which can cause the common cold), SARS-CoV (Severe acute respiratory syndrome-related coronavirus, which causes the disease SARS), MERS-CoV (Middle East respiratory syndrome-related coronavirus, which causes the disease MERS), and SARS-CoV-2 (which causes the COVID-19). SARS and MERS are two examples of large-scale pandemics in the two decades before the 2019 novel coronavirus diseases (COVID-19) [1]. Since the outbreak, the genomic sequence and natural reservoirs of SARS-CoV-2 have been elucidated [2]. The full-length genome sequence study revealed that SARS-CoV-2 shares 79.6% and 96% sequence identity to SARS-CoV and bat coronavirus, respectively. The study indicated that the natural reservoir host for SARS-CoV-2 is bats (which is also the case for a large number of SARS-related coronavirus [3]) and currently available data does not recognize any animal species acted as an intermediate host [4]. To visualize the evolutionary relationship among the Beta-CoVs, their full-length genomes were mapped against the phylogenetic tree and their main host reservoir species were illustrated through phyloT website (https://phylot.biobyte.de/) based on the NCBI taxonomy (Fig. 1) [5]. Phylogenetic analysis of Beta-CoV whole-genome revealed similar evolutionary relationships described in several studies in detail [4]. SARS-CoV-2 is present in the respiratory tract in free, non-specific bound, and specific bound states. The contamination of respiratory epitheliums is a consequence of complex interactions at many lengths and time scales. Compared with the SARS-CoV and MERS-CoV, SARS-CoV-2 showed high human-to-human transmissibility that exacerbates the threat of a shocking pandemic [6]. The SARS-CoV-2 transmissibility and disease severity in humans compared with other coronaviruses are pieces of the puzzle that can be helpful to provide efficient solutions in the fight against the pandemic.
Fig. 1.
Phylogenetic analysis of full-length genomes of human CoV-OC43, HKU1, SARS-CoV, MERS-CoV, and SARS-CoV-2 and their main host reservoir species. The branches denote the relationship of genetic information between subsequent generations, and branch lengths represent genetic change or divergence. The scale bar represents the degree of divergence which generally estimate using the average number of nucleotide substitutions per site (0.09 means 9% differences between two sequences of species). To visualize the evolutionary relationship among the Beta-CoVs, their full-length genomes were mapped against the phylogenetic tree and their main host reservoir species were illustrated through phyloT website (https://phylot.biobyte.de/) based on the NCBI taxonomy
The outbreak of COVID-19 has emerged as a severe pandemic that has affected over eight million people (confirmed cases) and killed more than 450,000 people worldwide between December 2019 and Jun 2020 [7]. The strategic objectives for controlling the pandemic are to interrupt human-to-human transmission through awareness-raising in the population, rapid identification, early isolation and care for the patients, and acceleration of the development of diagnostics, therapeutics, and vaccines, so as to minimize the societal and economic impacts [8]. There are opportunities to take advantage of biomaterials, nanotechnology, and cellular biology to study COVID-19 and provide impactful public health interventions [9]. This review focuses on recent efforts and advancements in the use of biomaterials and nanotechnology to overcome the novel-virus outbreak.
An introduction to preventative strategies
The rapid spread of COVID-19 in China and the importation of cases to other countries posed a global public health emergency. Understanding the epidemiological parameters and transmission characteristics of COVID-19 is essential to break the chain of transmission. Epidemiological parameters like the interval between symptom onsets of successive cases in a transmission chain, and time between infection and onset of symptoms, directly affect transmission probability that should be considered for effective control of the pandemic. The WHO has developed interim guidance and updated it according to scientific evidence. According to guidance published on the 5th of June 2020, “COVID-19 virus is primarily transmitted between people via respiratory droplets and contact routes. Therefore, the transmission of the COVID-19 virus can occur directly by contact with infected people, or indirectly by contact with surfaces in the immediate environment or with objects used on or by the infected person” [10]. Physical distancing, hand hygiene maintenance, wearing gloves, and masks could reduce potential exposure risk from infected people or contaminated surfaces. In this regard, new protective materials and equipment are in high demand since preventing the transfer of COVID-19 viruses into the host is a more effective and cost-saving approach than fighting against the virus after infection. Since the onset of COVID-19, a broad spectrum of antiviral materials in the form of coatings, thin-films, fabrics, etc. have been studied. In this section of the review, ideas and studies about producing effective self-protection tools to stop the spread of the COVID-19 will be discussed.
Personal protective equipment
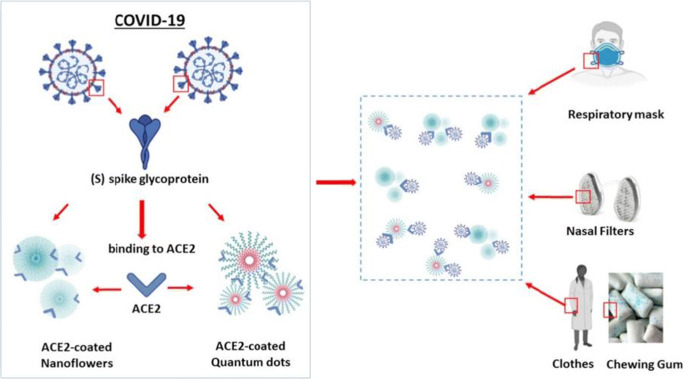
According to the WHO interim guidance, the virus is primarily transmitted between people via respiratory droplets when coughing, sneezing, or in very close personal contact [11]. In this way, personal protective equipment (PPE) like gloves, eye protection, gowns, and masks provide a barrier to prevent potential exposure to the virus. Fluid-resistant surgical filtering facemasks are designed to protect patients and healthcare workers from the spread of infectious diseases. Using facemasks and other PPE with anti-viral effects could offer a more efficient alternative. Adding anti-viral filters to the common non-invasive ventilation masks showed effective filtration of respirable particles relative to FFP3 and N95 respirators. The suggested system is reusable and could solve the shortage of masks and respirators for the protection of healthcare workers during the coronavirus pandemic [12]. Angiotensin-converting enzyme 2 (ACE2), a membrane protein exposed on the surface of the host cell, facilitated coronaviruses entry into host cells. Therefore, catching and holding coronaviruses before entering host cells is a step in the fight against COVID-19. Aydemir et al. [13] have suggested synthesizing of ACE2 coated/embedded nanoflowers or quantum dots to produce chewing gums, nose filters, and self-protective tools like masks, gloves, and clothes (Fig. 2). This concept can be used to produce long-lasting protective tools to minimize infections. Since antibodies can neutralize viral antigens, immobilizing specific antibodies on air filters represents a potentially effective way to preventing SARS-CoV-2 transmission.
Fig. 2.
Schematic representation of possible blocking of COVID-19 entering into the host at first step by ACE-2 coated nanoflowers and quantum dots. Respiratory masks, nasal filters, clothes, and chewing gums can be impregnated with functional ACE2-coated nanoflowers or quantum dots. Reprinted with permission from [13]
Surface protective coatings can destabilize coronaviruses on diverse surfaces and provide long-lasting protective tools. The stability of SARS-CoV-2 in aerosols and on different surfaces was studied resulting in the WHO recommendations to appropriately/consistently use disinfection products. According to one of these studies, SARS-CoV-2 is fairly stable on plastic and stainless steel, remaining viable up to 72 h after application to these surfaces [14]. One of the criteria to fight the spread of COVID-19 is to reduce transmission via standard public health interventions based on surface disinfection in commercial, healthcare facilities, nosocomial and residential environments. Liquid, gas, and light disinfectants are not permanent and recontamination is easy, so the process of decontamination must be repeated frequently. Self-disinfecting surfaces are continuously active coatings that are capable of inactivating deposited pathogens, and antiviral coatings offer a barrier to reduce human exposure to infectious viruses from fomites without the need for regular cleaning and disinfecting. Several effective coating strategies like hybrid coating, tin oxide nanowires, polysaccharide-coated NPs, zinc oxide tetrapod NPs, etc. have been studied to control the infection of envelope viruses [15]. For instance, polymers displaying quaternary ammoniums coated on stainless steel showed more than 90% reduction of the coronavirus 229E within 10 min and by greater than 99.9% after 2 h of contact. [16]. In SARS-CoV-2 research, most of the studies are theoretical studies, and experimental studies are currently somewhat limited. In Table 1, some of the theoretical and experimental studies were listed.
Table 1.
Selected studies on anti-SARS-CoV-2 PPE and surface coating
| Composition | Application | Fabrication method | Results | Ref |
|---|---|---|---|---|
| Ag nanocluster/silica composite | Facial FFP3 mask | Radio frequency co-sputtering | 100% inhibition | [17] |
| Ag NPs | Polycotton fabrics | Pad-dry-cure | 99.99% inhibition | [18] |
| SiO2-Ag nanoparticles | Air filter | Aerosolized coating | 92% inhibition | [19] |
| Ag | Surfaces | N/A | Inadequate in a naturalistic medical environment | [20] |
| Iron oxides | Fabric | N/A | Ideation | [21] |
| NPs combined with standard polylactic acid | Powered air-purifying respirators | Fused deposition modeling (FDM) | N/A | [22] |
| Graphene and its derivatives | Filters | N/A | Ideation | [23] |
Early detection and diagnostic approaches
The general clinical symptoms of COVID-19 include fever, dry cough, headache, and dyspnea that may progress to pneumonia and death. Some infected people have non-respiratory symptoms, and some report no symptoms at all. Diagnosis based on clinical symptoms is extremely difficult since there are no specific signs and symptoms of COVID-19 especially in the early stages of this disease. Accurate diagnosis of COVID-19 is crucial to identify infected people, especially asymptomatic carriers, to break the transmission chain. These investigations have been conducted to fulfill the vital necessity for easily operated, rapid, and uncomplicated detection techniques for the diagnosis of COVID-19. Other essential features for an ideal detection device include high sensitivity, high selectivity, multiplexing capabilities, multiple sensing modes, long shelf-life, mass manufacturing, and autonomous use [24]. Due to this urgent and demand, SARS-CoV-2 detection assays have been rapidly developed [25]. The detection strategies of viruses can be categorized into four main methods: Viral RNA/DNA detection (genetic tests), viral protein detections (antigenic recognition), antibody detection (serology tests), and direct detection of the virus. Real-time reverse-transcription polymerase chain reaction (RT-PCR) is an RNA/DNA detection test that is a gold standard for SARS-CoV-2 detection. However, this method’s accuracy and sensitivity depend on viral replication, viral titer, and sample collection. The positive rate of the first RT-PCR was around 70% [26]. Therefore, the false-negative results of RT-PCR raised clinical concerns since the prevention of cross-infection is very crucial in outbreak control. Moreover, genome sequencing is not applicable in rapid and mass diagnoses because of the time necessary for sequencing and the need for sophisticated equipment. Serological tests do not detect the virus itself but have been used to detect the viral protein or the antibodies that are produced in response to SARS-CoV-2. This test is not currently recommended for diagnosis. However, researchers have continued to work on serological tests with potential for rapid detection to be used in SARS-CoV-2 detection. With current advances in nanotechnology and nanofabrication, direct detection of the SARS-CoV-2 is a contemplative subject in several research groups [27]. Biosensors and nanoscale visualization tools like x-ray diffraction (XRD), electron microscopes, and atomic force microscopy (AFM) are commonly used in the direct detection of viruses. In this section, recent advances according to the role of biomaterials and nanotechnology in SARS-CoV-2 detection in each category will be discussed.
Biosensors
There is a global demand for rapid, mass-produced, and cost-effective methods of diagnosis of SARS-CoV-2 infections that needs to be met. Biosensors are analytical devices used to detect analytes (e.g., biomolecules, species produced by microorganisms, etc.). Biosensors typically consist of three parts: a bio-receptor (nucleic acids, antibody, enzyme, etc.), transducer (magnetic resonance, electrochemical, optical, electrical, thermal), and electronic system/signal processing. Biosensors have been developed to detect nucleic acids, enzymes, antibodies, cells, bacteria, and viruses in samples taken from the human body (e.g., blood, saliva, urine, etc.). In comparison with conventional virus detection methods, biosensors should be rapid, inexpensive, and sensitive [28], potentially incorporating nanomaterials that result in increasing sensitivity, ease of processing, and higher signal/noise ratio; some examples of such SARS-CoV-2 sensors are discussed below (examples highlighted in Table 2).
Table 2.
Recently developed detection methods and their parameters in SARS-CoV-2 detection
| Type | Target | Biomaterials | Advantages | Ref |
|---|---|---|---|---|
| Plasmonic fiber optic absorbance biosensor | N protein | Gold nanoparticles | Label-free | [29] |
| Smartphone-based microfluidic | Nucleic acid | Complementary metal oxide semiconductor | Fast | [30] |
| Electrowetting-on-Dielectric | Nucleic acid | Indium tin oxide | Small testing volume, fast, safeguard against contamination | [31] |
| Microfluidic ELISA | Monoclonal anti-S1 antibodies | Glass capillary | Small testing volume, fast, point-of-care | [32] |
| Lateral flow immunoassay | IgM/IgG antibody | Selenium nanoparticle | Sensitivity of the kit is 94.74% and the specificity is 95.12%, portable, fast | [33] |
| Lateral flow immunoassay | IgG antibody | Colloidal gold nanoparticles | Sensitivity of the kit is 69.1% and the specificity is 100%, portable, fast | [34] |
| Lateral flow immunoassay | IgM antibody | Colloidal gold nanoparticles | Sensitivity of the kit is 100% and the specificity is 93.3%, portable, fast | [35] |
| Lateral flow immunoassay | IgM/IgG antibody | Colloidal gold nanoparticles | The overall testing sensitivity is 88.66% and specificity is 90.63 | [36] |
| chemiluminescent immunoassays | IgM/IgG antibody | Magnetic microbeads | 100% sensitivity for IgG and 88% sensitivity for IgM | [37] |
| Immunochromatography assay (GICA) and enzyme-linked immunosorbent assay (ELISA) | IgM antibody | Colloidal gold | Reducing false-positive results | [38] |
| Colorimetric assay | Nucleic acid | Gold nanoparticles | Naked-eye detection | [39] |
| Flow-virometry | Virus particles | Magnetic nano-particles | Large-scale detection | [40] |
| Immunochromatographic assay | Nucleoprotein antigen | Colloidal gold nanoparticles | Sensitivity of the kit is 30.2% and the specificity is 100%, fast | [41] |
| Surface-enhanced Raman scattering (SERS) | Virus particles | Silver-nanorod array | Rapid and on-site diagnostic tool | [42] |
Loop-mediated isothermal amplification (LAMP) is a highly specific isothermal amplification assay that has been developed for the detection of multiple respiratory RNA viruses. The development of a reverse-transcription LAMP assay (RT-LAMP) coupled with biotin and streptavidin-conjugated nanoparticles yielded biosensors capable of detection of COVID-19 within an hour with 100% sensitivity and specificity in a total of 129 respiratory samples [43].
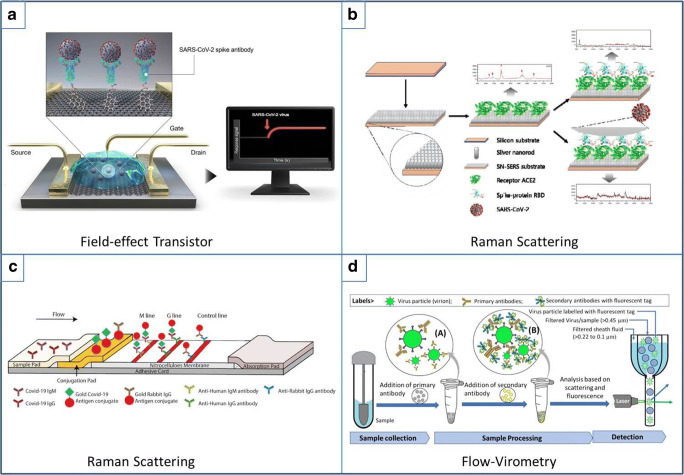
Electrochemical biosensors can also offer rapid, sensitive, and selective detection of viruses, and are consequently receiving increasing attention. The electrode materials have a crucial role in the signal/noise ratio, limit of detection, response time, and sensitivity; and nanomaterials with high surface area, electrical conductivity, electron-transfer-reaction, and chemical stability can be used to produce high-quality electrochemical biosensors, because the efficiency of these biosensors depends on the active area of the electrode [44]. A field-effect transistor (FET)-based biosensor is one of the suggested biosensors for instantaneous and accurate diagnosis of COVID-19 using small amounts of analyte. Recently, Seo et al. developed a graphene-based FET biosensor functionalized with the SARS-CoV-2 spike antibody for use as a SARS-CoV-2 detection platform, where the positive charge of the antibody exerted an n-doping effect on graphene after they were immobilized on the graphene surface (Fig. 3a), enabling the detection of SARS-CoV-2 from clinical samples with a detection limit of about 50-100 copies (although improvements might be needed for more accurate detection) [45].
Fig. 3.
Schematic diagram of some innovation in SARS-COV-2 detection process. a Real-time graphene-based FET in which SARS-CoV-2 spike antibody is conjugated onto the graphene sheet via 1-pyrenebutyric acid N-hydroxysuccinimide ester. Adapted with permission from ref [45]. b Functionalized silver-nanorod substrate used in surface-enhanced Raman scatting to detect binding of RBD on ACE2. Adapted with permission from ref [42]. c Using of colloidal gold in the conjugation pad in Lateral-flow assay schematic to detect IgM and IgG antibodies [36]. d Using primary and secondary antibodies to detect SARS-CoV-2 via flow-virometry process. Adapted with permission from ref [40]
Qiu et al. developed a plasmonic biosensor for the clinical COVID-19 diagnosis [46]. The plasmonic chip with gold nanoislands functionalized with complementary DNA receptor was capable of generating local plasmonic photothermal heat and transduces in situ hybridization for highly sensitive and accurate SARS-CoV-2 detection (future iterations of such sensors could enable real-time and label-free detection of viral sequences for application in other pandemics).
Microfluidic opportunity
Microfluidic analytical devices offer opportunities for rapid, sensitive, specific, instrument-free, user-friendly, point-of-care, and cost-effective detection of analytes with 3D printed and paper-based microfluidic analytical devices becoming increasingly popular. Temperature-dependent liquefied polymers like acrylonitrile-butadiene-styrene (ABS), nitrocellulose, wax, polystyrene, cellulose fiber, poly(dimethylsiloxane) (PDMS), and PDMS resin are common materials to construct 3D shapes [47], typically incorporating recognition elements like DNA, RNA, and proteins, and potentially integrating other detection methods like LAMP [48], ELISA [49], or CRISPR/Cas9 [50]. Microfluidic devices have been developed for the identification of pathogenic microorganisms like bacteria, fungi, viruses, and parasites [51]. For COVID-19 diagnosis researchers have detected biomarkers showing elevated expression in patients infected with COVID-19 relative to healthy patients (such biomarkers include serum ferritin, C-reactive protein, interleukin-2R, IL-6, D-dimer, and serum amyloid A) [52]. Lin et al. [53] designed a portable microfluidic immunoassay system for detecting IgG/IgM/Antigen of SARS-CoV-2 in clinical human serum. They integrated the microfluidic platform with a fluorescence detection analyzer. Their method revealed comparable results with the gold-immunochromatographic assay for SARS-CoV-2 detection.
Rapid testing
The COVID-19 outbreak has been a challenge for laboratories worldwide because of the huge number of samples and time-consuming diagnostic methods. Immunoassays may help to study immune responses, determine the precise rate of infection, and in the identification of donors for plasma therapy. Lateral flow immunoassays (LFIAs) are low-cost, simple, accurate, rapid, and portable platforms for the detection and quantification of specific antigens, antibodies, and products of gene amplification [54]. Chen et al. studied replacing lanthanide-doped polystyrene nanoparticles (LNPs) with conventional fluorescent dyes for detecting anti-SARS-CoV-2 IgG in human serum. The antibody-modified LNPs were used to fabricate the LFIA strips, and they claimed that their validation experiments met the requirements for clinical diagnosis of anti-SARS-CoV-2 IgG [55]. Li et al. developed an LFIA that can detect SARS-CoV-2 antibodies (both IgM and IgG) in human blood within 15 min, employing a surface antigen from SARS-CoV-2 conjugated to colloidal gold nanoparticles resulting in a method with an overall testing sensitivity of 88.66% and specificity of 90.63% [36].
Isolation and detection of viral RNA (which is inherently unstable) has been used to detect SARS-CoV-2. The silica-based spin-column RNA extraction method (spin-column traditional method) is laborious, time-consuming, and vulnerable to contamination. To address this issue, Zhao et al. have developed a polymer-coated magnetic nanoparticle viral RNA extraction method for SARS-CoV-2 detection that functions because of the fast and effective absorption of RNA molecules [56]. The extraction time for multiple samples was about 30 min which is significantly faster than 2 h for the traditional spin-column method. Somvanshi et al. used the surface-functionalized magnetic nanoparticles to extract viral RNA from several specimens via an automated process employing PCR for the diagnosis of COVID-19 [57].
The hybridization chain reaction (HCR) is a new method for nucleic acid detection through a hybridization cascade without the need for enzymes; this new method needs less material, less equipment and can be carried out at room temperature. Wu et al. employed in silico designed HCR reactions for SARS-CoV-2 detection, using cDNA as the target instead of RNA. The algorithm helped to analyze the target sequence and estimate the HCR efficiency and ultimately calculation of the mean unpaired probability of the target sequence [58].
Treatment solutions
Currently, there are no specific antiviral drugs or vaccines for COVID-19, and most treatments are supportive of cardiovascular, hemodynamic, and respiratory systems that do not efficiently kill the virus. To develop a successful treatment, understanding of a virus’s entry into the cell and the following events are beneficial. Generally, the SARS-CoV-2 life cycle includes virus-host cell receptor binding, proteolytic cleavage of the virus envelope followed by virus fusion into the host cell, viral RNA release and nucleoprotein uncoating, translation and replication, transcription, RNA replication and packaging, translation, assembly and budding, vesicle formation and exocytosis, and virus release. [59]. To clarify the coronavirus entry procedure, researchers tried to highlight the major process essential for interacting coronavirus with the ACE2 receptor. Previous studies emphasized the role of RBD (receptor-binding domain ) region interactions while a study of SARS-CoV S proteins suggested that host cell surface proteases cause refolding and energy release required to create stable virus-cell binding [60]. Host proteases belong to the serine protease family that cleave peptide bonds in S proteins. By designing a consensus Bat-SCoV genome and replacing the Bat-SCoV spike RBD with the SARS-CoV RBD, Becker et al. showed despite replacing the RBD of the lineage B bat virus Rp3 allowed the virus to enter cells expressing human ACE2; they concluded that coordinated interactions between the S1 RBD and select S2 domains might be important in epitope presentation and S protein function [61]. Letko et al. indicated that in cells with low expression of ACE2 adding protease during the course of SARS-CoV infection facilitated the virus entry [62].
To elucidate the potentially increased transmissibility of SARS-CoV-2 relative to SARS-CoV, the role of cell proteases in S protein priming was studied by two groups. The Hoffmann group has studied the role of cellular serine protease TMPRSS2 for S protein priming in SARS-CoV-2 and SARS-CoV. They showed that priming of S protein by TMPRSS2 in SARS-CoV-2 is essential for viral entry like SARS-CoV. Although, the presence of several arginine residues at the S1/S2 cleavage site in SARS-CoV-2 and lack of them at SARS-CoV have been shown in this study [63]. In other attempts, Walls et al.’s studies showed the unexpected furin-like proteases (PCSK3) cleavage site located at the S1/S2 boundary of SARS-CoV-2 comparative to SARS-CoV altering pathogenicity and increasing transmissibility of SARS-CoV-2. Furin-like proteases mediate pre-cleavage at the S1/S2 boundary in target cells might stimulate subsequent TMPRSS2-dependent viral entry [64, 65]. By comparing SARS-CoV-2 and SARS-CoV S-protein sequences and extracting pro-protein convertases cleavage amino acid motifs, Coutard et al. indicated that S1/S2 boundary and S2′ are proteolytic sites activated by furin-like protease. With different basic residues at S1/S2 boundary and S2′ in SARS-CoV-2 relative to SARS-CoV, suggesting a less efficient cleavage in SARS-CoV S-protein leading to less viral spread and pathogenesis [66]. These revelations on the structural characteristics of SARS-CoV-2 and comparing it with other coronaviruses are crucial to clarify the pathogenic mechanisms. Based on recognized pathogenic mechanisms several attempts are ongoing for possible treatment strategies. Using blocking monoclonal antibodies (mAbs) from recently recovered COVID-19 patients was suggested by Chen et al. for neutralizing virus infection. mAbs can specifically bind to the SARS-CoV-2 RBD region and effectively block the viral entry to host cells [67]. Drug design and development is a complex, expensive, and time-consuming process. Polypharmacology is a major challenge in drug design due to unintended drug-target interactions that causes side effects or toxicities. On the other hand, discovering the unknown targets for the existing drugs would help to identify potential drugs for other diseases [68]. Repurposing existing drugs on the market is an active area of intense research and clinical trials. The mechanism of action of these repurposed drugs, listed in Table 3, are variable and include blocking the virus entry inside the host cells, stopping virus replication, inhibiting protease activity, suppressing viral RNA synthesis, reducing the production of cytokines, and activating the T cell. The administration route of these conventional treatments is intravenous, and the delivery of their therapeutic agents to specific sites is limited. Nanomedicine and nanotechnology have promise for efficiently and selectively delivering such therapeutic agents into target sites (Fig. 4).
Table 3.
Underinvestigating repurposing drugs in COVID-19
| Drug | Primary indication | Mechanism of action | Ref |
|---|---|---|---|
| Methylprednisolone (Medrol) | Anti-inflammation | Suppression of exuberant and dysfunctional systematic inflammation | [69] |
| Tocilizumab (Actemra) | Rheumatoid arthritis | Interleukin-6 inhibitor | [70] |
| Sarilumab (Kevzara) | Rheumatoid arthritis | Interleukin-6 inhibitor | [71] |
| Baricitinib (Olumiant) | Rheumatoid arthritis | Inhibit endocytosis | [72] |
| Chloroquine | Malarial | Inhibition of pH-dependent viral fusion/replication | [73] |
| Hydroxychloroquine | Malarial | Inhibition of pH-dependent viral fusion/replication | [74] |
| Teicoplanin | Antibiotic | Inhibiting the low pH cleavage of the viral spike protein by cathepsin L | [75] |
| Azithromycin | Antibiotic | Reduced viral proliferation | [76] |
| Type 1 interferon | Cancer and autoimmune diseases | Inhibit viral replication | [77] |
| Heparin | Anticoagulant | Bind to RBD and induce conformational changes in S-protein | [78] |
| Enoxaparin | Anticoagulant | Supportive | [79] |
| Losartan (Cozaar) | Hypertension and kidney disorders | Angiotensin receptor 1 (AT1R) blockers | |
| Lopinavir | HIV | Inhibits the protease activity of coronavirus | [80] |
| Lopinavir/ritonavir | HIV | Inhibits the protease activity of HIV | [67] |
| Umifenovir (Arbidol) | Influenza | Inhibit endocytosis | [81] |
| Oseltamivir (Tamiflu) | Influenza A | Neuraminidase inhibitor | [82] |
| Remdesivir (Veklury) | Ebola virus | RNA polymerase (RdRp) inhibitor | [83] |
| Favipiravir (Avigan) | Ebola virus | RNA polymerase (RdRp) inhibitor | [84] |
| Lianhuaqingwen | Influenza | Regulation of cytokines | [85] |
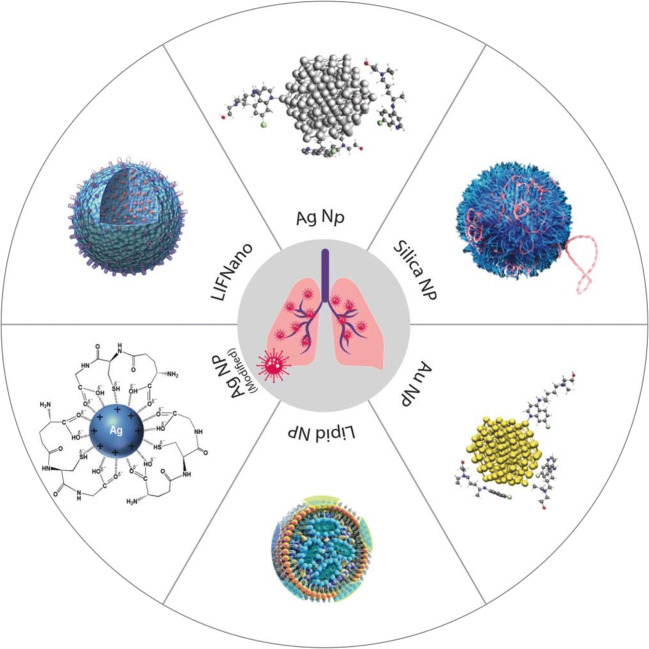
Fig. 4.
Innovative nanomedicine and carriers have been designed for SARS-CoV-2 treatment. Ag and Au NPs used as carriers for hydroxychloroquine/chloroquine molecules. Silica NP use suggested as a non-viral delivery vehicle of vaccine. Lipid NP used to encapsulate self-amplifying RNA encoding the SARS-CoV-2 S-proteins as a vaccine. LIFNano is a synthetic stem cell NP suggested for use to treat patients with pneumonia
Nanomedicines against COVID-19
Metal and metal oxide nanoparticles
Metal nanoparticles are used in the diagnosis and treatment of conditions because of their interesting properties including plasmonic resonance, fluorescence enhancement, photoluminescence, superparamagnetism, catalytic activity enhancement, cytotoxicity, antiviral, production of reactive oxygen species, biocompatibility, and ease of elimination from the body [86, 87]. Metallic NPs can form strong interactions with various species, may cause viral denaturation (and reduced virulence in the long term), and provide a convenient way to isolate the bound particles (e.g., with magnetic separation). Elucidation of specific mechanisms of action will aid in the design of improved NPs for viral eradication. The antiviral effect of metal nanoparticles is related to either inhibiting viral replication inside the host cells or binding of metal nanoparticles to surface glycoproteins of viruses thereby preventing the fusion of the virus into host cells. The antiviral activity of silver nanoparticles against different viral families, like HIV-1, hepatitis B, respiratory syncytial virus, herpes simplex virus, monkeypox virus, and H1N1 influenza, have been studied [88]. A nano-silver inhalation delivery formulation (optimal nanoparticle sizes of 3–7 nm) was reported to be useful at an early stage of respiratory infections in COVID-19 [89]. The mechanism of silver NP action has not been clarified completely; however, inactivation of virus particles prior to entry, interference with viral attachment, and interaction with viral RNA were shown in some studies [90].
A gold-based compound like auranofin (a gold-containing triethyl phosphine) is an FDA-approved medicine for the treatment of rheumatoid arthritis and in phase II clinical trials for cancer therapy. Inhibition of redox enzymes which results in cellular oxidative stress and intrinsic apoptosis is assumed to be its mechanism of action. Rothan et al. investigated the effect of auranofin on SARS-CoV-2, finding that auranofin inhibits 50% replication of SARS-CoV-2 in Huh7 cells at low micro-molar concentrations, and dramatically reduced the expression of SARS-CoV-2 induced cytokines in Huh7 cells, suggesting the drug could be useful in restricting SARS-CoV-2 infection and associated lung injury [91].
According to a docking study of Abo-zeid et al., Fe2O3 and Fe3O4 interacted efficiently with the spike protein receptor-binding domain (S1-RBD). Both Fe2O3 and Fe3O4 previously showed similar performance with hepatitis C virus glycoproteins E1 and E2. The binding of iron oxide nanoparticles (IONPs) with S1-RBD forms the most stable complex that is expected to be associated with viral protein conformational changes and subsequently inhibit virus entry into host cells. This binding could also initiate virus destruction through the generation of reactive oxygen species (ROS), and a clinical trial for FDA-approved IONPs for COVID-19 treatment has been endorsed [21].
Drug carriers
To achieve desired therapeutic effects, drug carriers are often employed to modify drug absorption and distribution. Various drug delivery systems (including nanostructures, nanofibers, dendrimers, liposomes, microspheres, micelles, protein-DNA complexes, protein-drug conjugates, virosomes, etc.) have been studied and developed [92]; in the ongoing pandemic, most studies focus on repurposing drugs and developing carriers for local and effective drug delivery. Rezaee et al. studied the affinity of hydroxychloroquine/chloroquine molecules towards silver and gold nanoparticles with the help of molecular dynamics simulations, and the calculated charge-transfer interactions suggest that these nanoparticles can be used as a drug delivery system for hydroxychloroquine/chloroquine with decreased drug side effects [93].
Lipid-based formulations are promising carriers for targeted delivery of therapeutic agents. Nanostructured lipid carriers derived from natural or synthetic lipids can be used for the delivery of hydrophobic/lipophilic drugs with high bioavailability [94]. Pindiprolu et al. suggested lipid carriers for intra-pulmonary delivery of salinomycin (a coccidiostat ionophore drug with a broad spectrum of antibacterial, anti-parasitic, antifungal, and antiviral effects). The antiviral effect of salinomycin is related to inhibition of the replication of viral RNA in the cytoplasm by altering the pH, and encapsulation of salinomycin in lipid nanocarriers enables aerosol-based pulmonary delivery providing sustained therapeutic effects [95].
Graphene and its derivatives have been investigated for use in protective materials, biosensors, antiviral drugs, and drug delivery owing to their high viral capture capacity, electronic properties for signal amplification, electrostatic interactions with the proteins of the virus, etc. [23, 96]; however, their in vivo cytotoxicity represents a challenge in their use in treatments.
Vaccines
A vaccine provides acquired immunity to a particular transmissible disease. Vaccines are typically composed of antigens (made from a weakened or killed form of microorganisms), toxins, or surface proteins, that are recognized by the immune system and induce a strong immune response. Recent innovative vaccines that are in development/use include dendritic cells, DNA, recombinant vectors, RNA, and T-cell receptor peptides. Major platform types of SARS-CoV-2 vaccine that have been studied include whole-cell killed or live-attenuated vaccines, recombinant proteins, nucleic acid-based DNA and mRNA, and replicating and non-replicating viral vectors [97]. The challenges faced in developing effective vaccines include the selection of a potent antigen, efficient adjuvant (immunological agents that activate the antigen), and delivery vehicles. In the past decade, nanomaterials have gained significant attention as potential adjuvant and carriers. Several nanoparticle-based vaccine adjuvant and delivery systems have been studied [98, 99]. According to the WHO, there have been 89 vaccine candidates in preclinical and clinical stages until April 2020. Seven of those in the phase 1 clinical stage are nucleic acid vaccines using non-replicating viral vectors for vaccine delivery, other candidates in the phase I clinical stage include recombinant proteins, DNA, and RNA [100]. In the following section, the latest progress and ideas on deploying biomaterials and nanotechnology in developing SARS-CoV-2 vaccines will be discussed.
Lipid nanoparticles
LNPs are a unique class of lipids considered the most clinically advanced non-viral DNA/RNA and drug delivery systems. They offer high encapsulation efficiency, improved penetration into cells, and low cytotoxicity. The first LNP-formulated RNA-based drug was approved in 2018 by the FDA [101]. McKay et al. studied a self-amplifying RNA encoding the SARS-CoV-2 S-protein encapsulated with an LNP as a vaccine. LNP used in this study contained ionizable cationic lipid/phosphatidylcholine/cholesterol/PEG-lipid with a mean hydrodynamic diameter of ca. 75 nm. Their immunogenicity results showed the LNP vaccine-elicited robust SARS-CoV-2 IgG antibody and cellular responses in mice. They claimed that their primary results would enable the rapid translation of the designed SARS-CoV-2 vaccine to the clinical trial [102].
Silica nanoparticles
Silica nanoparticles have shown great potential in drug and protein delivery because of their chemical stability, biocompatibility, low toxicity, and the ability to be synthesized in various sizes, shapes, and pore diameters. These characteristics besides the ability of silica nanoparticles to induce both humoral and cell-mediated immune responses led to the study of their potential to be used as antigen carriers and immunological adjuvant in vaccine delivery [103, 104]. N4 Pharma has developed Nuvec® silica nanoparticles coupled with polyethyleneimine that traps, protects and delivers DNA/RNA antigen into cells. Some key features of these silica nanoparticles include adjuvant effect, generating Th1 response, high loading capacity, strong bonding, and high cellular uptake [105]. Theobald suggested Nuvec® as a non-viral delivery vehicle of vaccine can be a safe and effective alternative to lipid nanoparticle system and non-replicating viral vectors that have been studied in many companies in developing SARS-CoV-2 vaccine [106].
Innovative strategies: hopes and promises
In response to the COVID-19 outbreak, pharmaceutical companies and researchers have stepped forward with plans to develop innovative strategies to fight the outbreak. Beyond the vaccines, for example, the siRNA-based RNA interference (RNAi) mechanism has been explored to eradicate viral genome from the host [107]. An additional promising strategy is to deploy theranostic agents. Multidisciplinary nanomedicine and nanotechnology have a pivotal role in changing conventional sight in disease diagnosis and therapy. Theranostic approaches benefit from combining therapeutics and diagnostics strategies. During the last few years, there has been ongoing progress in the field of theranostic approaches in oncology and recently infectious diseases. Nanomaterials and nanostructures like graphene, metal oxide, layered double hydroxides, metals, black phosphorus, transition metal dichalcogenides, etc. made this possible [108].
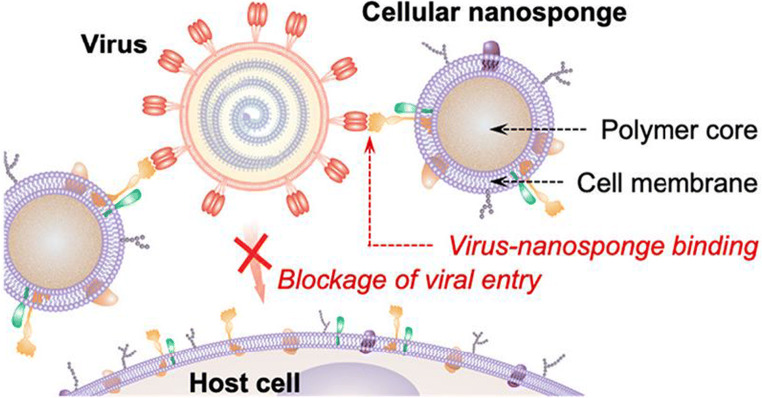
Cellular nanosponge
Zhang et al. investigated a novel approach mimicking the molecular mechanisms of viral infection. As mentioned above, SARS-CoV-2 uses ACE2 and CD147 receptors on the host cell surface in cellular entry. Covering polymer nanoparticles with membranes from human lung epithelial cells and macrophages creates a cellular nanosponge that can act as a decoy for SARS-CoV-2 (Fig. 5). In their study, a poly(lactic-co-glycolic acid) (PLGA) nanoparticle covered with cell membranes of human lung epithelial cells and macrophages that inherit the viral receptors (ACE2 and CD147) related to SARS-CoV-2 entry into host cells. The designed cellular nanosponges could neutralize the viral activity in a dose-dependent manner [109].
Fig. 5.
Schematic mechanism of cellular nanosponges inhibiting SARS-CoV-2 infectivity. The polymeric NP cores with natural cell membranes from target cells inherit the surface antigen profiles of the source cells and serve as decoys to bind with SARS-CoV-2 that blocks viral entry and inhibits viral infectivity [109]
Stem cell therapy
Reducing the infection rate besides treating patients with pneumonia are key requirements to reduce the mortality rate in the COVID-19. The currently available therapies in the COVID-19 mostly fail in the acute inflammatory pneumonia stage. One of the novel therapeutic strategies is using mesenchymal stem cells (MSCs). MSCs can provide a therapeutic environment in the lung via secretion of various cytokines, tissue mediators, and growth factors [110]. In one of the first attempts, a severely ill COVID-19 patient with ground-glass opacity (GGO) on CT scan and liver injury were treated with allogeneic human umbilical cord mesenchymal stem cells. After three intravenous infusions of stem cells, the patient was able to start spontaneous breathing and walking [111]. Currently, several clinical trials on using stem cells especially mesenchymal stem cells (MSCs) in COVID-19 treatment have been registered in Clinicaltrials.gov. Studies have shown MSCs have immunomodulatory and anti-inflammatory properties [112]. Metcalfe and his colleague from the University of Cambridge have developed a synthetic stem cells nanoparticles “LIFNano” to treat multiple sclerosis (MS). LIF (Leukaemia Inhibitory Factor) is a small blood-borne protein functioning to repair damaged tissues throughout the body. They suggested the nanotechnology-based LIFNano has the potential to rejuvenate damaged tissues and suppress cytokine storm in COVID-19 patients with pneumonia [113]. Other manufacturers of regenerative products like Exoflo™ and NestaCell® have started their clinical trials as a treatment of severe COVID-19. Exoflo™ is an exosome formulation derived from allogeneic bone marrow MSCs. In the clinical study, 24 patients with moderate to severe COVID-19 were administered a single 15 mL of Exoflo™ through intravenous infusion without any reaction. Their results indicated that patients’ clinical status and oxygenation improved after one treatment [114]. NestCell® is a MSC therapy produced by Cellavita Company. This product is under clinical trial to treat patients with severe COVID-19 pneumonia. In the clinical trials, patients will receive 2 x 107 cells on days 1, 3, 5, and 7 [115]. According to extraordinary opportunity of tissue engineering and biomaterials for long regeneration, bioengineering lung tissue might be an advanced strategy in patients suffering from lung injury [116].
In silico studies
Beside accelerating in vitro and in vivo studies in discovering vaccines and new therapies and diagnosing methods in COVID-19, artificial intelligence (AI)-inspired studies have demonstrated great success in diagnosing and treatment methods. One of the first applications of AI referred to COVID-19 was in medical imaging to detect and differentiate bacterial and viral pneumonia in chest computed tomography (CT) images [117]. The second use of AI is to help in understanding the virus-host cell interactions during the course of infection is key to developing new therapeutic strategies and repurposing existing drugs. In this regard, Gordon et al [118] cloned, tagged, and expressed 26 of the 29 proteins in human cells to identified high confidence SARS-CoV-2/human protein/protein interactions. And, through chemoinformatic databases and analyses of the above results, 67 druggable human protein or host factors were targeted by 69 existing FDA-approved or in clinical trial drugs. They claimed that they have started testing these compounds for the antiviral activity to developing therapeutics agents against SARS-CoV-2. In another attempt, molecular docking calculation showed hydroxychloroquine and azithromycin did not interact with receptors. It assumed that these drugs act in different steps in the viral cycle. The calculations indicated that metaquine (antimalarial substance) and saquinavir (anti-HIV antiretroviral) were potential candidates for multi-target drugs for COVID-19 [119].
Conclusion
The sudden appearance and rapid spread of COVID-19 have promoted an urgent need for mobilizing knowledge and facilities across the world to restrict the progressive socially and economically destructive effects of the pandemic. Much unknown information about the origin of SARS-CoV-2, the molecular events that led to human transmission from the main source, high human-human transmissibility, and the virus-cell interactions are part of the complexity to fight against the COVID-19. There has not been any clinically approved drug or vaccine that specifically target SARS-CoV-2 but rapid progress is underway. Repurposing drugs and upgrading present detection methods are part of the fighting strategies until supplying effective treatments or providing the vaccine. In the meantime, nanotechnology and nanomaterials are playing key roles either in slowing down the adverse effects or proposing new therapeutic solutions. For instance, silica nanoparticles, which had been developed as a vaccine carrier, are hopeful for developing the SARS-CoV-2 vaccine. It is clear that a key to tackling this pandemic is to cover all aspects of the fighting like protective equipment, detection technologies, and treatment solutions. The first step is to break the transmission chain through personal protective equipment and disinfected surfaces. Previously introduced anti-viral biomaterials accelerate research about fighting against SARS-CoV-2. In the next step, using nanotechnology and nanomaterials develop detection techniques rapidly. In the last step, nanomedicine and stem cells are part of the road map in the treatment of ill COVID-19 patients. Through this review, we highlight the recent advances in nanotechnology, biomaterials, and cellular biology that provide opportunities to fight the SARS-CoV-2 more efficiently.
Compliance with ethical standards
Conflict of interest
The authors declare that there are no conflicts of interest.
References
- 1.Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, Hu Y, Tao ZW, Tian JH, Pei YY, Yuan ML, Zhang YL, Dai FH, Liu Y, Wang QM, Zheng JJ, Xu L, Holmes EC, Zhang YZ. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yuen K-S, Ye Z-W, Fung S-Y, et al. SARS-CoV-2 and COVID-19: the most important research questions. Cell Biosci. 2020;10:40. doi: 10.1186/s13578-020-00404-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou P, Lou YX, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sayers EW, Cavanaugh M, Clark K, Ostell J, Pruitt KD, Karsch-Mizrachi I. GenBank. Nucleic Acids Res. 2019;47:D94–D99. doi: 10.1093/nar/gky989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Walls AC, Park Y, Tortorici MA, et al. Structure, Function , and Antigenicity of the SARS- Structure , Function , and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell. 2020;181:1–12. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization (2020) Coronavirus disease (COVID-19) pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed 21 Nov 2020
- 8.Culp WC. Coronavirus disease 2019. A A Pract. 2020;14:e01218. doi: 10.1213/xaa.0000000000001218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mozafari M, Tariverdian T, Beynaghi A. Trends in biotechnology at the turn of the millennium. Recent Pat Biotechnol. 2020;14:78–82. doi: 10.2174/1872208313666190924162831. [DOI] [PubMed] [Google Scholar]
- 10.Organización Mundial de la Salud, Advice on the use of masks in the context of COVID-19: interim guidance-2. Guía Interna la OMS, 1–5 (2020). 10.1093/jiaa077
- 11.World Health Organization, Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19): interim guidance, (World Health Organization, 2020) https://apps.who.int/iris/handle/10665/331498 (accessed Nov 21, 2020)
- 12.D. Dellweg, D. Koehler, F. Kloster, G. Gmbh Noninvasive ventilation masks with viral filters to protect health care workers from SARS-CoV-2 / Coronavirus infections. 1–18 (2020) 10.21203/RS.3.RS-21269/V1
- 13.Aydemir D, Ulusu NN. Angiotensin-converting enzyme 2 coated nanoparticles containing respiratory masks, chewing gums and nasal filters may be used for protection against COVID-19 infection. Travel Med. Infect. Dis. 2020;37:101697. doi: 10.1016/j.tmaid.2020.101697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.N. van Doremalen, T. Bushmaker, D.H. Morris, M.G. Holbrook, A. Gamble, B.N. Williamson, A. Tamin, J.L. Harcourt, N.J. Thornburg, S.I. Gerber, J.O. Lloyd-Smith, Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 382, 1564-1567 (2020) DOI: 10.1056/NEJMc2004973 [DOI] [PMC free article] [PubMed]
- 15.Kumar P, Usmani Z, Kumar V, Kumar V. Tackling COVID-19 pandemic through nanocoatings : confront and exactitude. Curr Res Green Sustain Chem. 2020;3:100011. doi: 10.1016/j.crgsc.2020.100011. [DOI] [Google Scholar]
- 16.L.A. Ikner, J.R. Torrey, P.M. Gundy, C.P. Gerba A continuously active antimicrobial coating effective against human coronavirus 229E. medRxiv 2020.05.10.20097329. (2020) 10.1101/2020.05.10.20097329
- 17.C. Balagna, S. Perero, E. Percivalle, EV. Nepita, M. Ferraris, Virucidal effect against Coronavirus SARS-CoV-2 of a silver nanocluster/silica composite sputtered coating. Open Ceramics 6, 100006 (2020). 10.1016/j.oceram.2020.100006
- 18.G.C. Tremiliosi, L.G. Simoes, D.T. Minozzi, R.I. Santos, D.B. Vilela, D.B. Durigon, R.R. Machado, D.S. Medina, L.K. Ribeiro, I.L. Rosa, M. Assis, Ag nanoparticles-based antimicrobial polycotton fabarics to prevent the transmission and spread of SARS-CoV-2. BioRxiv (2020). 10.1101/2020.06.26.152520
- 19.Park DH, Joe YH, Hwang J. Dry aerosol coating of anti-viral particles on commercial air filters using a high-volume flow atomizer. Aerosol Air Qual Res. 2019;19:1636–1644. doi: 10.4209/aaqr.2019.04.0212. [DOI] [Google Scholar]
- 20.B.O. Iddins, M.H. Waugh, T. Robbins, J. Cunningham III, D.E. Graham, M.T. Finn, Antimicrobial silver touch surfaces in an occupational medicine clinic. J. Occup. Environ. Med. (2020). 10.1097/JOM.0000000000001883 [DOI] [PMC free article] [PubMed]
- 21.Abo-zeid Y, Ismail NS, McLean GR, Hamdy NM. A molecular docking study repurposes FDA approved iron oxide nanoparticles to treat and control COVID-19 infection. Eur J Pharm Sci. 2020;153:105465. doi: 10.1016/j.ejps.2020.105465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.J. Cote, J. Haggstrom, R. Vivkanandan, et al., COVID-19 and a novel initiative to improve safety by 3D printing personal protective equipment parts from computed tomography. Res Sq, 1–26 (2020). 10.21203/rs.3.rs-31671/v1 [DOI] [PMC free article] [PubMed]
- 23.Palmieri V, Papi M. Can graphene take part in the fight against COVID-19? Nano Today. 2020;33:100883. doi: 10.1016/j.nantod.2020.100883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.N. Bhalla, Y. Pan, Z. Yang, A.F. Payam, Opportunities and challenges for biosensors and nanoscale analytical tools for pandemics : COVID-19. (2020). 10.1021/acsnano.0c04421 [DOI] [PMC free article] [PubMed]
- 25.Udugama B, Kadhiresan P, Kozlowski HN, Malekjahani A, Osborne M, Li VYC, Chen H, Mubareka S, Gubbay JB, Chan WCW. Diagnosing COVID-19: the disease and tools for detection. ACS Nano. 2020;14:3822–3835. doi: 10.1021/acsnano.0c02624. [DOI] [PubMed] [Google Scholar]
- 26.J.W. Ai, H.C. Zhang, T. Xu, J. Wu, M. Zhu, Y.Q. Yu, H.Y. Zhang, Z. Shen, Y. Li, X. Zhou, G.Q. Zang, Optimizing diagnostic strategy for novel coronavirus pneumonia, a multi-center study in Eastern China. MedRxiv (2020). 10.1101/2020.02.13.20022673
- 27.Pokhrel P, Hu C, Mao H. Detecting the coronavirus (COVID-19) ACS sensors. 2020;5:2283–2296. doi: 10.1021/acssensors.0c01153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Metkar SK, Girigoswami K. Diagnostic biosensors in medicine–a review. Biocatal Agric Biotechnol. 2019;17:271–283. doi: 10.1016/j.bcab.2018.11.029. [DOI] [Google Scholar]
- 29.Murugan D, Bhatia H, Sai VVR, Satija J. P-FAB: a fiber-optic biosensor device for rapid detection of COVID-19. Trans Indian Natl Acad Eng. 2020;5:1–5. doi: 10.1007/s41403-020-00122-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.N. Farshidfar, S. Hamedani, The potential role of smartphone-based microfluidic systems for rapid detection of COVID-19 using saliva specimen. Mol Diagnosis, Ther, 20–22 (2020). 10.1007/s40291-020-00477-4 [DOI] [PMC free article] [PubMed]
- 31.Muralidhar VJK. Electrowetting-on-dielectric system for COVID-19 testing. Trans Indian Natl Acad Eng. 2020;5:251–254. doi: 10.1007/s41403-020-00113-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.X. Tan, C. Lin, J. Zhang, et al., Rapid and quantitative detection of COVID-19 markers in micro-liter sized samples. bioRxiv 2020.04.20.052233. (2020). 10.1101/2020.04.20.052233
- 33.Z.Z. Wang, Z. Zheng, X.C. Wang, P.M. Zheng, F.C. Cui, Q.W. Zhou, H.Z. Hu, X.Q. Li, H.L. Zhang, Y.X. Wei, G. Li, Rapid detection of Anti-SARS-CoV-2 IgM and IgG using a selenium nanoparticle-based lateral flow immunoassay. (2020). 10.21203/rs.3.rs-34278/v1
- 34.Wen T, Huang C, Shi F-J, Zeng XY, Lu T, Ding SN, Jiao YJ. Development of a lateral flow immunoassay strip for rapid detection of IgG antibody against SARS-CoV-2 virus. Analyst. 2020;145:5345–5352. doi: 10.1039/D0AN00629G. [DOI] [PubMed] [Google Scholar]
- 35.Huang C, Wen T, Shi F-J, et al. Rapid detection of IgM antibodies against the SARS-CoV-2 virus via colloidal gold nanoparticle-based lateral-flow assay. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li Z, Yi Y, Luo X, Xiong N, Liu Y, Li S, Sun R, Wang Y, Hu B, Chen W, Zhang Y, Wang J, Huang B, Lin Y, Yang J, Cai W, Wang X, Cheng J, Chen Z, Sun K, Pan W, Zhan Z, Chen L, Ye F. Development and clinical application of a rapid IgM-IgG combined antibody test for SARS-CoV-2 infection diagnosis. J Med Virol. 2020;92:1518–1524. doi: 10.1002/jmv.25727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.A. Padoan, C. Cosma, L. Sciacovelli, D. Faggian, M. Plebani, Analytical performances of a chemiluminescence immunoassay for SARS-CoV-2 IgM/IgG and antibody kinetics. Clin. Chem. Lab. Med. 16(1) (2020). 10.1515/cclm-2020-0443 [DOI] [PubMed]
- 38.Wang Q, Du Q, Guo B, Mu D, Lu X, Ma Q, Guo Y, Fang L, Zhang B, Zhang G, Guo X. A method to prevent SARS-CoV-2 IgM false positives in gold immunochromatography and enzyme-linked immunosorbent assays. J. Clin. Microbiol. 2020;6:26–58. doi: 10.1128/JCM.00375-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moitra P, Alafeef M, Dighe K, Frieman MB, Pan D. Selective naked-eye detection of SARS-CoV-2 mediated by N gene targeted antisense oligonucleotide capped plasmonic nanoparticles. ACS Nano. 2020;14:7617–7627. doi: 10.1021/acsnano.0c03822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.N. Soni, P. Pai, V. Prasad, S. Dasgupta, B. Bhadra. Application of flow-virometry for large-scale screening of Covid 19 cases. (2020).
- 41.Scohy A, Anantharajah A, Bodéus M, Kabamba-Mukadi B, Verroken A, Rodriguez-Villalobos H. Low performance of rapid antigen detection test as frontline testing for COVID-19 diagnosis. J Clin Virol. 2020;129:104455. doi: 10.1016/j.jcv.2020.104455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.D. Zhang, X. Zhang, R. Ma, S. Deng, X. Wang, X. Zhang, X. Huang, Y. Liu, G. Li, J. Qu, Y. Zhu, Ultra-fast and onsite interrogation of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) in environmental specimens via surface enhanced Raman scattering (SERS). medRxiv (2020). 10.1101/2020.05.02.20086876 [DOI] [PMC free article] [PubMed]
- 43.Zhu X, Wang X, Han L, et al (2020) Reverse transcription loop-mediated isothermal amplification combined with nanoparticles-based biosensor for diagnosis of COVID-19. medRxiv 2020.03.17.20037796. 10.1101/2020.03.17.20037796 [DOI] [PMC free article] [PubMed]
- 44.Ran G, Wu F, Ni X, Li X, Li X, Liu D, Sun J, Xie C, Yao D, Bai W. A novel label-free electrochemical aptasensor with one-step assembly process for rapid detection of lead (II) ions. Sensors Actuators, B Chem. 2020;320:128326. doi: 10.1016/j.snb.2020.128326. [DOI] [Google Scholar]
- 45.Seo G, Lee G, Kim MJ, Baek SH, Choi M, Ku KB, Lee CS, Jun S, Park D, Kim HG, Kim SJ, Lee JO, Kim BT, Park EC, Kim SI. Rapid detection of COVID-19 causative virus (SARS-CoV-2) in human nasopharyngeal swab specimens using field-effect transistor-based biosensor. ACS Nano. 2020;14:5135–5142. doi: 10.1021/acsnano.0c02823. [DOI] [PubMed] [Google Scholar]
- 46.Qiu G, Gai Z, Tao Y, Schmitt J, Kullak-Ublick GA, Wang J. Dual-functional plasmonic photothermal biosensors for highly accurate severe acute respiratory syndrome coronavirus 2 detection. ACS Nano. 2020;14:5268–5277. doi: 10.1021/acsnano.0c02439. [DOI] [PubMed] [Google Scholar]
- 47.Loo JFC, Ho AHP, Turner APF, Mak WC. Integrated printed microfluidic biosensors. Trends Biotechnol. 2019;37:1104–1120. doi: 10.1016/j.tibtech.2019.03.009. [DOI] [PubMed] [Google Scholar]
- 48.Dou M, Sanchez J, Tavakoli H, Gonzalez JE, Sun J, Dien Bard J, Li XJ. A low-cost microfluidic platform for rapid and instrument-free detection of whooping cough. Anal Chim Acta. 2019;1065:71–78. doi: 10.1016/j.aca.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ng AHC, Fobel R, Fobel C, Lamanna J, Rackus DG, Summers A, Dixon C, Dryden MDM, Lam C, Ho M, Mufti NS, Lee V, Asri MAM, Sykes EA, Chamberlain MD, Joseph R, Ope M, Scobie HM, Knipes A, Rota PA, Marano N, Chege PM, Njuguna M, Nzunza R, Kisangau N, Kiogora J, Karuingi M, Burton JW, Borus P, Lam E, Wheeler AR. A digital microfluidic system for serological immunoassays in remote settings. Sci Transl Med. 2018;10:eaar6076. doi: 10.1126/scitranslmed.aar6076. [DOI] [PubMed] [Google Scholar]
- 50.Liu M, Hui CY, Zhang Q, Gu J, Kannan B, Jahanshahi-Anbuhi S, Filipe CDM, Brennan JD, Li Y. Target-induced and equipment-free DNA amplification with a simple paper device. Angew Chemie. 2016;128:2759–2763. doi: 10.1002/ange.201509389. [DOI] [PubMed] [Google Scholar]
- 51.Nasseri B, Soleimani N, Rabiee N, Kalbasi A, Karimi M, Hamblin MR. Point-of-care microfluidic devices for pathogen detection. Biosens Bioelectron. 2018;117:112–128. doi: 10.1016/j.bios.2018.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.R. Jain, M. Kaur, Protein based biomarkers for non-invasive Covid-19 detection. 10.31219/osf.io/qn256 [DOI] [PMC free article] [PubMed]
- 53.Lin Q, Wen D, Wu J, Liu L, Wu W, Fang X, Kong J. Microfluidic immunoassays for sensitive and simultaneous detection of IgG/IgM/Antigen of SARS-CoV-2 within 15 min. Anal Chem. 2020;92:9454–9458. doi: 10.1021/acs.analchem.0c01635. [DOI] [PubMed] [Google Scholar]
- 54.M. Infantino, V. Grossi, B. Lari, et al., Diagnostic accuracy of an automated chemiluminescent immunoassay for anti-SARS-CoV-2 IgM and IgG antibodies: an Italian experience. J Med Virol, 1–5 (2020). 10.1002/jmv.25932 [DOI] [PMC free article] [PubMed]
- 55.Chen Z, Zhang Z, Zhai X, Li Y, Lin L, Zhao H, Bian L, Li P, Yu L, Wu Y, Lin G. Rapid and sensitive detection of anti-SARS-CoV-2 IgG, using lanthanide-doped nanoparticles-based lateral flow immunoassay. Anal Chem. 2020;92:7226–7231. doi: 10.1021/acs.analchem.0c00784. [DOI] [PubMed] [Google Scholar]
- 56.Z. Zhao, H. Cui, W. Song, et al A simple magnetic nanoparticles-based viral RNA extraction method for efficient detection of SARS-CoV-2. bioRxiv 518055:2020.02.22.961268. (2020) 10.1101/2020.02.22.961268
- 57.Somvanshi SB, Kharat PB, Saraf TS, et al. Multifunctional nano-magnetic particles assisted viral RNA-extraction protocol for potential detection of COVID-19. Mater Res Innov. 2020;00:1–6. doi: 10.1080/14328917.2020.1769350. [DOI] [Google Scholar]
- 58.T.H. Wu, C.C. Chang, C.H. Yang, W.Y. Lin, T.J. Ee, C.W. Lin, Hybridization chain reactions targeting the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Int J Mol Sci 21 (2020). 10.3390/ijms21093216 [DOI] [PMC free article] [PubMed]
- 59.Chauhan G, Madou MJ, Kalra S, Chopra V, Ghosh D, Martinez-Chapa SO. Nanotechnology for COVID-19: therapeutics and vaccine research. ACS Nano. 2020;14:7760–7782. doi: 10.1021/acsnano.0c04006. [DOI] [PubMed] [Google Scholar]
- 60.Shulla A, Heald-Sargent T, Subramanya G, Zhao J, Perlman S, Gallagher T. A transmembrane serine protease is linked to the severe acute respiratory syndrome coronavirus receptor and activates virus entry. J Virol. 2011;85:873–882. doi: 10.1128/JVI.02062-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Becker MM, Graham RL, Donaldson EF, Rockx B, Sims AC, Sheahan T, Pickles RJ, Corti D, Johnston RE, Baric RS, Denison MR. Synthetic recombinant bat SARS-like coronavirus is infectious in cultured cells and in mice. Proc Natl Acad Sci. 2008;105:19944–19949. doi: 10.1073/pnas.0808116105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Letko M, Marzi A, Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat Microbiol. 2020;5:562–569. doi: 10.1038/s41564-020-0688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.M. Hoffmann, H. Kleine-Weber, S. Schroeder, et al., SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell, 1–10 (2020). 10.1016/j.cell.2020.02.052 [DOI] [PMC free article] [PubMed]
- 64.A.C. Walls, X. Xiong, A. Rey, et al., Activation of coronavirus fusion unexpected receptor functional mimicry elucidates activation of coronavirus fusion, 1026–1039 (2019). 10.1016/j.cell.2018.12.028 [DOI] [PMC free article] [PubMed]
- 65.Glycoprotein C-S, Walls AC, Park Y, et al. Structure , Function , and antigenicity of the SARS-Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181:281–292.e6. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Coutard B, Valle C, de Lamballerie X, Canard B, Seidah NG, Decroly E. The spike glycoprotein of the new coronavirus 2019-nCoV contains a furin-like cleavage site absent in CoV of the same clade. Antiviral Res. 2020;176:104742. doi: 10.1016/j.antiviral.2020.104742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, Ruan L, Song B, Cai Y, Wei M, Li X, Xia J, Chen N, Xiang J, Yu T, Bai T, Xie X, Zhang L, Li C, Yuan Y, Chen H, Li H, Huang H, Tu S, Gong F, Liu Y, Wei Y, Dong C, Zhou F, Gu X, Xu J, Liu Z, Zhang Y, Li H, Shang L, Wang K, Li K, Zhou X, Dong X, Qu Z, Lu S, Hu X, Ruan S, Luo S, Wu J, Peng L, Cheng F, Pan L, Zou J, Jia C, Wang J, Liu X, Wang S, Wu X, Ge Q, He J, Zhan H, Qiu F, Guo L, Huang C, Jaki T, Hayden FG, Horby PW, Zhang D, Wang C. A trial of lopinavir–ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020;382:1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.AH. Bahmanpour, T. Navaei, F. Ahadi, M. Mozafari, Pulmonary system responses to biomaterials. In: handbook of biomaterials biocompatibility. Elsevier 653–662 (2020)
- 69.Zhou W, Liu Y, Tian D, et al. Potential benefits of precise corticosteroids therapy for severe 2019-nCoV pneumonia. Signal Transduct Target Ther. 2020;5:1–3. doi: 10.1038/s41392-019-0089-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Xu X, Han M, Li T, Sun W, Wang D, Fu B, Zhou Y, Zheng X, Yang Y, Li X, Zhang X, Pan A, Wei H. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci. 2020;117:10970–10975. doi: 10.1073/pnas.2005615117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.C. Gov, Evaluation of the efficacy and safety of sarilumab in hospitalized patients with COVID-19. Regeneron Pharmaceuticals (2020)
- 72.Richardson P, Griffin I, Tucker C, et al. Baricitinib as potential treatment for 2019-nCoV acute respiratory disease. Lancet (London, England) 2020;395:e30. doi: 10.1016/S0140-6736(20)30304-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.F. Touret, X. de Lamballerie, Of chloroquine and COVID-19. Antiviral Res. 5, 104762 (2020). 10.1016/j.antiviral.2020.104762 [DOI] [PMC free article] [PubMed]
- 74.Chen J, Liu D, Liu L, Liu P, Xu Q, Xia L, Ling Y, Huang D, Song S, Zhang D, Qian Z. A pilot study of hydroxychloroquine in treatment of patients with common coronavirus disease-19 (COVID-19) J Zhejiang Univ. 2020;1(6):49. doi: 10.3785/j.issn.1008-9292.2020.03.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Baron SA, Devaux C, Colson P, Raoult D, Rolain JM. Teicoplanin: an alternative drug for the treatment of coronavirus COVID-19. Int J Antimicrob Agents. 2020;13;55(4):105944. doi: 10.1016/j.ijantimicag.2020.105944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gautret P, Lagier J-C, Parola P, Meddeb L, Mailhe M, Doudier B, Courjon J, Giordanengo V, Vieira VE, Dupont HT, Honoré S. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020;20:105949. doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 77.E. Sallard, F.-X. Lescure, Y. Yazdanpanah, F. Mentre, N. Peiffer-Smadja. Type 1 interferons as a potential treatment against COVID-19. Antiviral Res, 7:104791 (2020). 10.1016/j.antiviral.2020.104791 [DOI] [PMC free article] [PubMed]
- 78.C.J. Mycroft-West, D. Su, S. Elli, Y. Li, S.E. Guimond, G.J. Miller, J.E. Turnbull, E.A. Yates, M. Guerrini, D.G. Fernig, M.A. de Lima, The 2019 coronavirus (SARS-CoV-2) surface protein (Spike) S1 Receptor Binding Domain undergoes conformational change upon heparin binding. BioRxiv (2020). 10.1101/2020.02.29.971093
- 79.A. Kollias, K.G. Kyriakoulis, E. Dimakakos, G. Poulakou, G.S. Stergiou, K. Syrigos, Thromboembolic risk and anticoagulant therapy in COVID-19 patients: emerging evidence and call for action. Br J Haematol 189, 846–847 (2020). 10.1111/bjh.16727 [DOI] [PMC free article] [PubMed]
- 80.J. Chen, D. Liu, L. Liu, P. Liu, Q. Xu, L. Xia, Y. Ling, D. Huang, S. Song, D. Zhang, Z. Qian, A pilot study of hydroxychloroquine in treatment of patients with moderate COVID-19. Zhejiang da xue xue bao Yi xue ban = J Zhejiang Univ Med Sci 49, 215-219 (2020) DOI: 10.3785/j.issn.1008-9292.2020.03.03 [DOI] [PMC free article] [PubMed]
- 81.M. Costanzo, M.A.R. De Giglio, G.N. Roviello, SARS CoV-2: recent reports on antiviral therapies based on lopinavir/ritonavir, darunavir/umifenovir, hydroxychloroquine, remdesivir, favipiravir and other drugs for the treatment of the new coronavirus. Curr Med Chem 27 (2020). 10.2174/0929867327666200416131117 [DOI] [PubMed]
- 82.Q. Tan, Y. Jin, Ostavimir is ineffective against COVID-19: in silico assessment, in vitro and retrospective study. medRxiv (2020). 10.1101/2020.05.15.20102392
- 83.Wang Y, Zhang D, Du G, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020;395:1569–1578. doi: 10.1016/S0140-6736(20)31022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Q. Cai, M. Yang, D. Liu, J. Chen, D. Shu, J. Xia, X. Liao, Y. Gu, Q. Cai, Y. Yang, C. Shen, X. Li, L. Peng, D. Huang, J. Zhang, S. Zhang, F. Wang, J. Liu, L. Chen, S. Chen, Z. Wang, Z. Zhang, R. Cao, W. Zhong, Y. Liu, L. Liu, Experimental treatment with favipiravir for COVID-19: an open-label control study. Engineering. (2020). 10.1016/j.eng.2020.03.007 [DOI] [PMC free article] [PubMed]
- 85.Runfeng L, Yunlong H, Jicheng H, Weiqi P, Qinhai M, Yongxia S, Chufang L, Jin Z, Zhenhua J, Haiming J, Kui Z. Lianhuaqingwen exerts antiviral and anti-inflammatory activity against novel coronavirus (SARS-CoV-2) Pharmacol. Res. 2020;20:104761. doi: 10.1016/j.phrs.2020.104761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.M. Mozafari, Editor. Handbook of Biomaterials Biocompatibility. Woodhead Publishing, 2020.
- 87.Sharma H, Mishra PK, Talegaonkar S, Vaidya B. Metal nanoparticles: a theranostic nanotool against cancer. Drug Discov Today. 2015;20:1143–1151. doi: 10.1016/j.drudis.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 88.S.K. Kailasa, T.-J. Park, J.V. Rohit, J.R. Koduru, in Nanoparticles in Pharmacotherapy, William Andrew Publishing. Antimicrobial activity of silver nanoparticles (2019), pp. 461–484. 10.1016/B978-0-12-816504-1.00009-0
- 89.O. Zachar, Formulations for COVID-19 Treatment via silver nanoparticles inhalation delivery. OSF Prepr, 1–19 (2020). 10.31219/osf.io/adnyb
- 90.Rai M, Deshmukh SD, Ingle AP, Gupta IR, Galdiero M, Galdiero S. Metal nanoparticles: the protective nanoshield against virus infection. Crit Rev Microbiol. 2016;42:46–56. doi: 10.3109/1040841X.2013.879849. [DOI] [PubMed] [Google Scholar]
- 91.Rothan HA, Stone S, Natekar J, Kumari P, Arora K, Kumar M. The FDA-approved gold drug auranofin inhibits novel coronavirus (SARS-COV-2) replication and attenuates inflammation in human cells. Virology. 2020;547:7–11. doi: 10.1016/j.virol.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.M. Mozafari, J. Rajadas, D.L. Kaplan, An introduction to nanoengineered biomaterials. Nanoengineered Biomaterials for Regenerative Medicine, 1–11 (2019). 10.1016/B978-0-12-813355-2.00001-6
- 93.P. Rezaee, M. Akbari, R. Morad, A. Koochaki, M. Maaz, Z. Jamshidi, First principle simulation of coated hydroxychloroquine on Ag, Au and Pt nanoparticle as a potential candidate for treatment of SARS-CoV-2 (COVID-19). arXiv preprint arXiv, 2006. 02343 (2020) [DOI] [PMC free article] [PubMed]
- 94.Salvi VR, Pawar P. Nanostructured lipid carriers (NLC) system: a novel drug targeting carrier. J Drug Deliv Sci Technol. 2019;51:255–267. doi: 10.1016/j.jddst.2019.02.017. [DOI] [Google Scholar]
- 95.Pindiprolu SKSS, Kumar CSP, Kumar Golla VS, P. L, K. SC, S.K. EB, R.K. R. Pulmonary delivery of nanostructured lipid carriers for effective repurposing of salinomycin as an antiviral agent. Med Hypotheses. 2020;143:109858. doi: 10.1016/j.mehy.2020.109858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.P.K. Raghav, S. Mohanty, Are graphene and graphene-derived products capable of preventing COVID-19 infection? Med Hypotheses, 110031 (2020) [DOI] [PMC free article] [PubMed]
- 97.Zhang J, Zeng H, Gu J, Li H, Zheng L, Zou Q. Progress and prospects on vaccine development against sars-cov-2. Vaccines. 2020;8:1–12. doi: 10.3390/vaccines8020153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kargozar S, Ramakrishna S, Mozafari M. Chemistry of biomaterials: future prospects. Curr Opin Biomed Eng. 2019;10:181–190. doi: 10.1016/j.cobme.2019.07.003. [DOI] [Google Scholar]
- 99.Kazemzadeh H, Mozafari M. Fullerene-based delivery systems. Drug Discov Today. 2019;24:898–905. doi: 10.1016/j.drudis.2019.01.013. [DOI] [PubMed] [Google Scholar]
- 100.Thanh Le T, Andreadakis Z, Kumar A, et al. The COVID-19 vaccine development landscape. Nat Rev Drug Discov. 2020;19:305–306. doi: 10.1038/d41573-020-00073-5. [DOI] [PubMed] [Google Scholar]
- 101.Garber K. Alnylam launches era of RNAi drugs. Nat Biotechnol. 2018;36:777–778. doi: 10.1038/nbt0918-777. [DOI] [PubMed] [Google Scholar]
- 102.P.F. McKay, K. Hu, A.K. Blakney, et al Self-amplifying RNA SARS-CoV-2 lipid nanoparticle vaccine induces equivalent preclinical antibody titers and viral neutralization to recovered COVID-19 patients. bioRxiv 2020.04.22.055608. (2020) 10.1101/2020.04.22.055608
- 103.Mody KT, Popat A, Mahony D, Cavallaro AS, Yu C, Mitter N. Mesoporous silica nanoparticles as antigen carriers and adjuvants for vaccine delivery. Nanoscale. 2013;5:5167–5179. doi: 10.1039/c3nr00357d. [DOI] [PubMed] [Google Scholar]
- 104.Kargozar S, Baino F, Hamzehlou S, Hill RG, Mozafari M. Bioactive glasses entering the mainstream. Drug Discov Today. 2018;23:1700–1704. doi: 10.1016/j.drudis.2018.05.027. [DOI] [PubMed] [Google Scholar]
- 105.N4 Pharma. https://www.n4pharma.com/nuvec/. Accessed 21 Nov 2020
- 106.N. Theobald, Emerging vaccine delivery systems for COVID-19: Functionalised silica nanoparticles offer a potentially safe and effective alternative delivery system for DNA/RNA vaccines and may be useful in the hunt for a COVID-19 vaccine. Drug Discov. Today (2020). 10.1016/j.drudis.2020.06.020 [DOI] [PMC free article] [PubMed]
- 107.Uludağ H, Parent K, Aliabadi HM, Haddadi A. Prospects for RNAi therapy of COVID-19. Front Bioeng Biotechnol. 2020;8:916. doi: 10.3389/fbioe.2020.00916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Santiago I. Trends and innovations in biosensors for COVID-19 mass testing. ChemBioChem. 2020;21:2880–2889. doi: 10.1002/cbic.202000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Q. Zhang, A. Honko, J. Zhou, et al Cellular nanosponges inhibit SARS-CoV-2 infectivity. Nano Lett acs.nanolett.0c02278. (2020) 10.1021/acs.nanolett.0c02278 [DOI] [PMC free article] [PubMed]
- 110.A. Can, H. Coskun, The rationale of using mesenchymal stem cells in patients with COVID-19-related acute respiratory distress syndrome: what to expect. Stem Cells Transl Med, 1–16 (2020). 10.1002/sctm.20-0164 [DOI] [PMC free article] [PubMed]
- 111.Orleans LA, is Vice H, Manchikanti L (2020) Expanded umbilical cord mesenchymal stem cells (UC-MSCs) as a therapeutic strategy in managing critically ill COVID-19 patients: the case for compassionate use. Pain Physician 23:E71–E83 [PubMed]
- 112.Golchin A, Seyedjafari E, Ardeshirylajimi A. Mesenchymal stem cell therapy for COVID-19: present or future. Stem Cell Rev Reports. 2020;16:427–433. doi: 10.1007/s12015-020-09973-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Metcalfe SM. Mesenchymal stem cells and management of COVID-19 pneumonia. Med Drug Discov. 2020;5:100019. doi: 10.1016/j.medidd.2020.100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sengupta V, Sengupta S, Lazo A, Woods P, Nolan A, Bremer N. Exosomes derived from bone marrow mesenchymal stem cells as treatment for severe COVID-19. Stem Cells Dev. 2020;29:747–754. doi: 10.1089/scd.2020.0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Rajarshi K, Chatterjee A, Ray S. Combating COVID-19 with mesenchymal stem cell therapy. Biotechnol Reports. 2020;26:e00467. doi: 10.1016/j.btre.2020.e00467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.S. Moztarzadeh, K. Mottaghy, F. Sefat, A. Samadikuchaksaraei, M. Mozafari. Nanoengineered biomaterials for lung regeneration. Nanoengineered Biomaterials for Regenerative Medicine, 305-323 (2019). 10.1016/B978-0-12-813355-2.00013-2
- 117.L. Li, L. Qin, Z. Xu, Y. Yin, X. Wang, B. Kong, J. Bai, Y. Lu, Z. Fang, Q. Song, K. Cao, Artificial intelligence distinguishes COVID-19 from community acquired pneumonia on chest CT. Radiology (2020). 10.1148/radiol.2020200905 [DOI] [PMC free article] [PubMed]
- 118.D. Gordon, G. Jang, M. Bouhaddou, et al., A SARS-CoV-2-Human protein-protein interaction map reveals drug targets and potential drug-repurposing. bioRxiv Prepr Serv Biol 03 (2020). 10.1101/2020.03.22.002386
- 119.O.B. Romulo, L.C.C.J. Fabio, S.P. Wildrimak, et al., Interaction of drugs candidates with various SARS-CoV-2 receptors: an in silico study to combat COVID-19. chemRxiv, 1–15 (2020). 10.26434/chemrxiv.12100968.v1 [DOI] [PubMed]