Abstract
India's cervical cancer screening program was launched in 2016. We evaluated baseline facility readiness using nationally representative data from the 2012–13 District Level Household and Facility Survey on 4 tiers of the public health care system - 18,367 sub-health centres (SHCs), 8540 primary health centres (PHCs), 4810 community health centres and 1540 district/sub-divisional hospitals. To evaluate facility readiness we used the Improving Data for Decision Making in Global Cervical Cancer Programmes toolkit on six domains - potential staffing, infrastructure, equipment and supplies, infection prevention, medicines and laboratory testing, and data management. Composite scores were created by summing responses within domains, standardizing scores across domains at each facility level, and averaging across districts/states.
Overall, readiness scores were low for cervical cancer screening. At SHCs, the lowest scores were observed in ‘infrastructure’ (0.55) and ‘infection prevention’ (0.44), while PHCs had low ‘potential staffing’ scores (0.50) due to limited manpower to diagnose and treat (cryotherapy) potential cases. Scores were higher for tiers conducting diagnostic work-up and treatment/referral. The highest scores were in ‘potential staffing’ except for PHCs, while the lowest scores were in ‘infection & prevention’ and ‘medicines and laboratory’. Goa and Maharashtra were consistently among the top 5 ranking states for readiness.
Substantial heterogeneity in facility readiness for cervical cancer screening spans states and tiers of India's public healthcare system. Infrastructure and staffing are large barriers to screening at PHCs, which are crucial for referral of high-risk patients. Our results suggest focus areas in cervical cancer screening at the district level for policy makers.
Keywords: Cervical Cancer, India, Screening
1. Introduction
In India, over 410,000 new cervical cancer cases and 228,000 deaths occur every year (GLOBOCAN 2018). Though low-cost, feasible, early detection methods are available, most cervical cancer cases are diagnosed at advanced stages (Krishnan et al., 2015). Aligned with WHO recommendations for a screen-and-treat approach in low-resource settings (World Health Organization, 2013; Bagcchi, 2016; Shastri et al., 2014; Sankaranarayanan et al., 2007), India implemented universal cervical cancer screening by visual inspection with acetic acid (VIA) at primary health care facilities, as part of the Comprehensive Primary Health Care Programme of Ayushman Bharat and National Programme for Prevention and Control of Cardiovascular Disease, Diabetes, Cancer and Stroke (NPCDCS) (Ministry of Health and Family Welfare GoI, 2016; Ministry of Health and Family Welfare GoI, n.d.). The guidelines recommend nationwide cervical cancer screening for women aged 30–65 years once every 5 years with reliance primarily on the VIA (Government of India, 2016).
India's primary health care system - traditionally focused on reproductive and child health needs - consists of a four-tier facility hierarchy starting from the sub-health centre (SHC), which is largely focused on health promotion, nutrition, and immunization, as a first point of contact with the community (Table 1). Second tier facilities are Primary Health Centres (PHC), which provide preventive and curative services and are staffed with a medical officer. Community Health Centres (CHC) are third tier facilities, which provide PHC services as well as emergency and lab services; and CHC's implement national health programmes such as those focused on non-communicable diseases (NCDs). The fourth and final tier includes the district hospital/sub divisional hospital (DH), with stronger staffing, specialist services, resources and 24-h emergency care. According to the operational guidelines, breast, cervical and oral cancer screening should occur primarily at the SHC and PHC levels, and all four levels are engaged for referral of suspicious lesions and diagnostic follow-up.
Table 1.
Health facilities in India's 4-tier public health care system.a
| Health facility type/ tier of facility |
Number of people/villages catering to | Activities/Responsibilities | Staffing requirements (minimum) | Other resources required |
|---|---|---|---|---|
| Sub-health Centre (SHC) | 5000 person or 4–5 villages 5000 people in plain areas and 3000 people in hilly/tribal/desert areas |
Health promotion, nutrition, immunization Essential services include: Maternal and child health (MCH, deliveries for Type B SHC's only), family planning, Medical Termination of Pregnancy (MTP), curative services for minor ailments, adolescent and school health services, control of local endemic diseases, field services for monitoring and health promotion |
Female/male health worker, auxiliary nurse cum-mid-wife Support cleaning staff (Desirable: + 1 Staff Nurse if > 20 deliveries in a month) |
An individual building or adequate rented space with easy access, adequate infrastructure, drugs and support services |
| Primary Health Centre (PHC) | 30,000 persons or 27 villages 30,000 people in plain areas and 20,000 people in hilly/tribal/desert areas 6 SHC's under each PHC |
Health promotion, prevention, curative care Essential services include: Medical care services (outpatient (OPD), emergency), MCH, family planning, MTP, nutrition services, adolescent & school health services, STI management, promotion of safe drinking water, sanitation, prevention and control of locally endemic diseases Data collection and management, education and behavior change communication |
Female/male health assistant, lab technician, multi-skilled worker Medical officer, pharmacist, staff nurses Accountant, lab technician, support cleaning staff |
6 indoor beds for patients, lab, recording and reporting facilities, disaster prevention measures, waiting area, outpatient department, labor room, residential accommodation |
| Community Health Centre (CHC) | 120,000 persons or 133 villages 1,20,000 people in plain areas and 80,000 people in hilly/tribal/desert areas 4 PHC's under each CHC |
Health promotion & prevention, Curative care, Emergency services, Lab services, National Health Programmes Essential services include: OPD and inpatient (IPD) services (general medicine, surgery, obstetrics & gynecology, pediatrics, dental and AYUSH services), eye specialist services (1 in 5) |
Female/male health assistant, lab technician, multi-skilled worker Medical specialists & block medical officer, Public health specialist, Public health nurse, nurses/paramedical |
30 in-patient beds, operation theatre (OT), lab, labor room, x-ray 30 indoor beds for patients, 1OT, labor room, X-ray, ECG, blood storage, and lab facilities |
| District Hospital (DH) | 1 DH in every district that caters to the population of that district (this varies from 32,000 to 30 lakhs) | Curative care, Emergency services, Lab services, National Health Programmes, Specialty services Essential services include: OPD, IPD & emergency services (gen'l specialty services, diagnostic and para-clinical services, lab services, ancillary and support services, admin services, services under National Health and Family Welfare Programmes, epidemic control, capacity building, monitoring and data management) |
Admin and support cleaning staff Medical specialists & block medical officer, Public health specialist, Public health nurse, nurses/paramedical Admin and support cleaning staff |
24-h obstetric care, continuous blood 100–500 beds Facilities include: quality assurance in clinics, labs, blood bank, ward unit, pharmacies, and accident & emergency, OTs, imaging, cardio-pulmonary equipment, labor wards, and other medical service equipment depending on grade. |
Selected data as it pertains to women's health.
For the present study, we assessed facility readiness for cervical cancer screening at all four levels of the health care system prior to the initiation of universal screening of common NCDs in 2016 utilizing data from the nationally representative District Level Health and Facility Survey-4 (DLHS-4) conducted during 2012–2013 (Ministry of Health and Family Welfare GoI, 2016; National Health System Resource Centre, n.d.).
2. Data and methods
2.1. Data source
The District Level Household and Facility Survey (DLHS-4, 2012–13) is the fourth government-conducted nationwide health survey on the utilization and quality of maternal and child healthcare services in India at the district level (http://www.rchiips.org/DLHS-4.html). Four questionnaires were administered to survey each of the four facility levels. Information at each health facility was collected by surveying relevant personnel, physical inspections, and assessing registers.
The DLHS-4 data includes health care facilities from 26 states and 3 union territories including all 1540 DHs and 4810 CHCs, and a representative sample of 8540 PHCs, and 18,367 SHCs. Data from two states (Gujarat, Jammu and Kashmir) and four union territories (Dadra and Nagar Haveli, Daman and Diu, Delhi, and Lakshadweep) were not available for analysis.
2.2. Assessing health facility readiness to implement cervical cancer screening
To assess health facility readiness for cervical cancer screening, we utilized the Improving Data for Decision Making in Global Cervical Cancer Programmes (IDCCP) Toolkit which provides a framework of indicators to assess facility readiness to implement cervical cancer screening programmes in low-and middle-income country settings (Drummond et al., 2017; Senkomago et al., 2017; World Health Organization, 2018). The IDCCP toolkit contains 13 categories and 83 questions, ranging from 2 to 14 questions per category, and 0–2 points per question (Drummond et al., 2017; Senkomago et al., 2017; World Health Organization, 2018).
For this analysis, we used the IDCCP toolkit developed by the Centers for Disease Control and Prevention, and the George W. Bush Institute and the World Health Organization to find exact/comparable matches from the health facility questionnaires at each of the 4 health care levels, and found 6 out of 13 categories met these criteria in DLHS-4: potential staffing, infrastructure, equipment and supplies, infection prevention, medicines and laboratory testing, and data management (see Appendix 1-4). In brief, the potential staffing category assesses if the health facility has staff capable for training in 10 different cervical cancer-screening methodologies. The infrastructure category assesses if the health facility has the proper infrastructure (e.g. running water, examination room, electricity, etc.) to carry out cervical cancer screening. The equipment and supplies category is focused on the necessary equipment to conduct different cervical cancer screening methodologies included in the IDCCP toolkit. The infection prevention category measures if the health facility has the proper sterilization equipment and disposes of biomedical waste appropriately. Medicines and laboratory testing ensures that essential items such as pain medication, reproductive tract infection (RTI)/ sexually transmitted infections (STI) medication, and pregnancy tests are available. Finally, the data management category ensures that appropriate staff and materials are in place to allow for adequate recordkeeping. The DH questionnaire included two additional categories - services, which measured if the health facility was currently performing cervical cancer screening services, and procurement and supply chain, which assessed if the DH regularly assessed, monitored, and ensured a reliable stock of their equipment and supply levels.
The IDCCP toolkit along with the Indian Public Health Standards (IPHS) (Nicholson et al., 2018) were used to determine best practices standards for each indicator, and the scoring for each question.
2.3. Statistical analysis
We used a binary system of scoring (0,1 for absent & present) since we were relying on secondary data collected for other purposes. For each question, the health facility received 1 point if they responded with an answer that met the identified standard and 0 points for any alternative response. For questions in which the IDCCP toolkit and IPHS were discordant on the appropriate response, the IPHS prevailed. The IDCCP questions for the six analyzed categories (and seven for DH), the corresponding questions from the DLHS-4, and the selected responses for the SHC, PHC, CHC, and DH can be found in Appendix 1-4, respectively. The assigned scores represent whether the measured resources are absent (0) or fully available (1) based on in-person visits of health facilities. Raw scores were calculated for each of the categories by summing all selected questions (classified as 1 for present, 0 for absent) in that category. To allow for comparability between categories, standardized scores were generated by dividing the raw scores by the number of selected questions included in each respective category. An overall score was calculated by taking an average of the standardized scores in each category, ensuring that each category received equal weight. Average category/overall scores were then stratified by health facility level and state. Maps were created at the district level using the overall score category for each health facility level. As scores across health facility levels are not comparable, quintile categories were calculated for each health facility level.
Prior to calculating PHC and SHC scores at the state level, districts were weighted based on the number of PHCs or SHCs they contained relative to those in the state. The distribution of health facilities by state and district was obtained from Rural Health Statistics for 2011–2012 (Government of India, 2013). No weighting was conducted at the CHC or DH level, as every health facility in sampled states and territories was selected. Maps were created at the district level, stratified by health facility level and score category. A sensitivity analysis was conducted to reflect changes of health personnel training from the initial roll-out, which was modified based on low SHC preparedness; instead, VIA training was taking place at the PHC level only instead of SHCs, and loop electrosurgical excision procedure (LEEP) or colposcopy procedures were conducted by obstetrician/gynecologists instead of other health providers/personnel.
All data analyses were conducted in SAS v9.4 (SAS Institute; Cary, NC).
3. Ethical considerations
This study is a secondary analysis of de-identified publicly available national databases. All participants provided written informed consent to participate in the survey. The DLHS-4 received ethics approval from the International Institute for Population Science's Ethical Review Board and the Ministry of Health and Family Welfare, Government of India.
4. Results
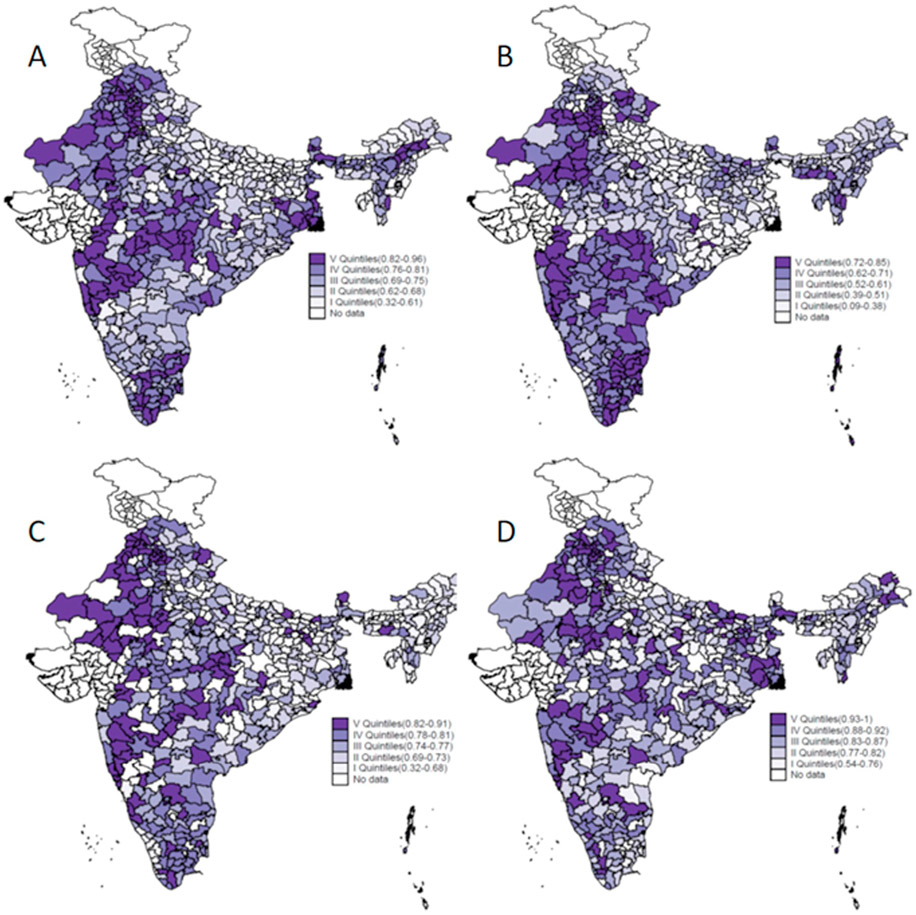
Overall, two adjacent states in western India - Goa and Maharashtra - ranked in the top 5 in three out of four health facility levels; no state ranked in the top 5 for all 4 levels of India's public healthcare system (Tables 2-5). For union territories - smaller administrative and geographical units - Chandigarh (north), Puducherry (south) and Andaman and Nicobar Islands ranked in the top 5 for three out of four health care levels. Maharashtra, despite being populous and large, also performed more consistently at the district-level (e.g., limited variation across the districts) – the overall composite score varied from 0.76 to 0.91, 0.62 to 0.78, 0.76 to 0.90 and 0.76 to 0.99 at the four levels of health facilities (Fig. 1). Scores closer to 1.0 indicate better preparedness in reaching a maximum score. Further explanation of how to interpret these scores are listed below, which presents findings for each facility level and category score, across the states and union territories of India.
Table 2.
Facility readiness for cervical cancer screening in Indian states and union territories at the sub health centre level.
| State | Composite Score |
Potential Staffing |
Infrastructure | Equipment & Supplies |
Infection & Prevention |
Medicines & Laboratory |
Data Management |
|---|---|---|---|---|---|---|---|
| India | 0.695 | 0.936 | 0.552 | 0.639 | 0.437 | 0.736 | 0.872 |
| Haryana | 0.843 | 0.993 | 0.777 | 0.955 | 0.622 | 0.864 | 0.847 |
| Maharashtra | 0.839 | 0.978 | 0.76 | 0.814 | 0.581 | 0.919 | 0.983 |
| Sikkim | 0.823 | 1 | 0.797 | 0.969 | 0.471 | 0.829 | 0.876 |
| Chandigarh | 0.811 | 0.913 | 0.745 | 0.892 | 0.71 | 0.826 | 0.783 |
| West Bengal | 0.811 | 0.997 | 0.619 | 0.904 | 0.505 | 0.882 | 0.96 |
| Punjab | 0.791 | 0.988 | 0.812 | 0.885 | 0.485 | 0.827 | 0.751 |
| Himachal Pradesh | 0.786 | 0.933 | 0.758 | 0.841 | 0.598 | 0.687 | 0.904 |
| Assam | 0.783 | 0.999 | 0.656 | 0.827 | 0.452 | 0.777 | 0.991 |
| Madhya Pradesh | 0.776 | 0.964 | 0.591 | 0.716 | 0.548 | 0.906 | 0.93 |
| Rajasthan | 0.742 | 0.946 | 0.579 | 0.694 | 0.445 | 0.863 | 0.929 |
| Andaman & Nicobar Island | 0.714 | 0.972 | 0.576 | 0.717 | 0.335 | 0.824 | 0.859 |
| Puducherry | 0.71 | 0.719 | 0.818 | 0.903 | 0.305 | 0.578 | 0.935 |
| Andhra Pradesh | 0.701 | 0.993 | 0.436 | 0.623 | 0.3 | 0.957 | 0.898 |
| Odisha | 0.699 | 0.982 | 0.494 | 0.618 | 0.345 | 0.799 | 0.954 |
| Mizoram | 0.696 | 0.958 | 0.612 | 0.726 | 0.356 | 0.798 | 0.726 |
| Goa | 0.692 | 0.941 | 0.601 | 0.489 | 0.397 | 0.747 | 0.975 |
| Tamil Nadu | 0.692 | 0.332 | 0.756 | 0.772 | 0.523 | 0.862 | 0.905 |
| Kerala | 0.67 | 0.929 | 0.583 | 0.525 | 0.347 | 0.797 | 0.838 |
| Karnataka | 0.663 | 0.932 | 0.587 | 0.549 | 0.351 | 0.778 | 0.784 |
| Nagaland | 0.655 | 1 | 0.545 | 0.535 | 0.319 | 0.604 | 0.926 |
| Uttarakhand | 0.653 | 0.997 | 0.635 | 0.687 | 0.27 | 0.487 | 0.839 |
| Meghalaya | 0.65 | 0.999 | 0.493 | 0.598 | 0.536 | 0.828 | 0.45 |
| Chhattisgarh | 0.648 | 0.886 | 0.509 | 0.65 | 0.328 | 0.76 | 0.752 |
| Jharkhand | 0.648 | 0.986 | 0.397 | 0.597 | 0.328 | 0.764 | 0.817 |
| Uttar Pradesh | 0.61 | 0.988 | 0.457 | 0.467 | 0.423 | 0.425 | 0.902 |
| Bihar | 0.571 | 0.988 | 0.259 | 0.282 | 0.477 | 0.615 | 0.805 |
| Manipur | 0.558 | 0.976 | 0.344 | 0.63 | 0.198 | 0.472 | 0.725 |
| Arunachal Pradesh | 0.534 | 0.821 | 0.464 | 0.399 | 0.168 | 0.593 | 0.76 |
| Tripura | 0.475 | 0.613 | 0.444 | 0.305 | 0.213 | 0.522 | 0.756 |
Scores are shaded from red to green to help the viewer read and interpret a range of numbers, with red indicating the lowest and green the highest scores; States/UTs are ranked according to the Composite score.
Table 5.
Facility readiness scores for cervical cancer screening in India/states and union territories at the district and sub divisional hospital level.
| India and States/UT’s | Composite Score |
Services | Potential Staffing |
Infrastructure | Procurement & Supply Chain |
Infection & Prevention |
Medicines & Laboratory |
Data Management |
|---|---|---|---|---|---|---|---|---|
| India | 0.843 | 0.690 | 0.975 | 0.905 | 0.964 | 0.725 | 0.814 | 0.825 |
| Goa | 0.968 | 1.000 | 1.000 | 0.889 | 1.000 | 0.889 | 1.000 | 1.000 |
| Puducherry | 0.960 | 1.000 | 1.000 | 0.944 | 1.000 | 1.000 | 0.778 | 1.000 |
| Chandigarh | 0.952 | 1.000 | 1.000 | 1.000 | 1.000 | 0.667 | 1.000 | 1.000 |
| Punjab | 0.939 | 0.966 | 0.997 | 0.937 | 1.000 | 0.805 | 0.902 | 0.966 |
| West Bengal | 0.917 | 0.742 | 1.000 | 0.968 | 1.000 | 0.860 | 0.866 | 0.984 |
| Maharashtra | 0.915 | 0.840 | 0.987 | 0.947 | 0.983 | 0.840 | 0.938 | 0.870 |
| Rajasthan | 0.910 | 0.698 | 1.000 | 0.956 | 0.981 | 0.811 | 0.931 | 0.991 |
| Himachal Pradesh | 0.887 | 0.917 | 1.000 | 0.889 | 0.917 | 0.639 | 0.889 | 0.958 |
| Haryana | 0.881 | 0.762 | 0.962 | 0.972 | 0.976 | 0.675 | 0.881 | 0.940 |
| Kerala | 0.879 | 0.900 | 1.000 | 0.917 | 1.000 | 0.548 | 0.790 | 1.000 |
| Chhattisgarh | 0.865 | 0.750 | 1.000 | 0.917 | 0.950 | 0.667 | 0.900 | 0.875 |
| Mizoram | 0.862 | 0.900 | 1.000 | 0.867 | 1.000 | 0.533 | 0.933 | 0.800 |
| Bihar | 0.861 | 0.632 | 0.974 | 0.922 | 0.971 | 0.858 | 0.745 | 0.926 |
| Andaman & Nicobar Island | 0.849 | 1.000 | 1.000 | 1.000 | 1.000 | 0.222 | 0.889 | 0.833 |
| Karnataka | 0.839 | 0.689 | 0.964 | 0.939 | 0.960 | 0.733 | 0.834 | 0.751 |
| Andhra Pradesh | 0.833 | 0.598 | 0.984 | 0.919 | 0.979 | 0.670 | 0.863 | 0.820 |
| Uttarakhand | 0.832 | 0.615 | 0.979 | 0.923 | 0.949 | 0.709 | 0.709 | 0.936 |
| Odisha | 0.827 | 0.655 | 1.000 | 0.930 | 0.982 | 0.606 | 0.836 | 0.782 |
| Madhya Pradesh-E | 0.827 | 0.573 | 0.984 | 0.896 | 0.942 | 0.693 | 0.841 | 0.859 |
| Nagaland | 0.816 | 0.636 | 1.000 | 0.712 | 1.000 | 0.697 | 0.848 | 0.818 |
| Meghalaya | 0.814 | 1.000 | 1.000 | 0.700 | 1.000 | 0.600 | 0.600 | 0.800 |
| Tamil Nadu | 0.812 | 0.773 | 0.929 | 0.846 | 0.989 | 0.772 | 0.728 | 0.644 |
| Arunachal Pradesh | 0.803 | 0.643 | 1.000 | 0.833 | 0.857 | 0.452 | 0.905 | 0.929 |
| Assam | 0.791 | 0.694 | 0.956 | 0.889 | 0.917 | 0.620 | 0.824 | 0.639 |
| Jharkhand | 0.791 | 0.774 | 1.000 | 0.806 | 0.935 | 0.613 | 0.828 | 0.581 |
| Uttar Pradesh | 0.773 | 0.268 | 0.989 | 0.907 | 0.894 | 0.739 | 0.714 | 0.901 |
| Tripura | 0.769 | 0.688 | 1.000 | 0.823 | 0.938 | 0.313 | 0.688 | 0.938 |
| Manipur | 0.744 | 0.625 | 1.000 | 0.625 | 0.875 | 0.333 | 0.875 | 0.875 |
| Sikkim | 0.732 | 0.750 | 1.000 | 1.000 | 0.250 | 0.750 | 0.750 | 0.625 |
Scores are shaded from red to green to help the viewer read and interpret a range numbers, with red indicating the lowest and green the highest scores; States/UTs are ranked according to the composite score.
Fig. 1.
Composite scores for each of the 4 health facility levels in India by district - DLHS-4 (2012 – 2013). (A) Sub Health Centres, (B) Primary Health Centres, (C) Community Health Centres, (D) District Hospitals (separate TIF file).
4.1. Facility readiness at the Sub-Health Centre (SHC) level
For SHCs, the mean overall composite score was 0.70 (min, max: 0.48, 0.84, Table 2). The lowest and highest scores were observed in the north-east (e.g., Manipur and Sikkim, respectively). ‘Potential staffing’ had the highest scores; 93.6% of SHCs had an auxiliary nurse midwife (ANM) and/or female health worker available to perform VIA (Appendix 1) - although there was wide variation by state (Table 2) and district (Fig. 1). Two small states in the north-east achieved perfect scores for potential staffing – Nagaland and Sikkim – indicating that an ANM, female health worker, or contractual additional ANM were staffed at all sub-centres in the sampled districts. Another category with overall high scores for the nation (0.87) was ‘Data Management’ where most of the facilities had available registers (95%), supplied their data in Health management information system (HMIS) format (92%), and had an ANM performing data entry (75%, Appendix 1). The lowest category scores (0.44) were observed in ‘Infection Prevention’, which was driven by the low proportion of SHCs with an available and functional autoclave for sterilizing equipment (27%) and only 39% properly disposed of hazardous/infectious waste. This category also had considerable variation with a > 3-fold difference across states (e.g., Arunachal Pradesh, 0.17, Haryana 0.62). There was also substantial SHC score variation at the district-level; in Kerala, composite scores varied from 0.44 in Kasaragod district to 0.90 in Idukki district.
4.2. Facility readiness at the Primary Health Centre (PHC) level
The mean overall composite PHC score was 0.56 (min, max – 0.31, 0.78) with the highest scores in smaller (Goa, 0.74), and larger states (Haryana, 0.74, Table 3). The lowest scoring states were low income states that lag behind in demographic, epidemiological transitions (Dandona et al., 2017) and infant mortality rate reductions (Uttar Pradesh, 0.33). The highest performing PHC categories were ‘Equipment and Supplies’ (mean score-0.78) and ‘Infrastructure’ (mean score – 0.64) with top-ranking states in the west, south and north (Maharashtra, 0.97 and 0.87, Tamil Nadu, 0.97 and 0.87, and Haryana, 0.96 and 0.88, respectively). The lowest scoring category was ‘Medicines and Laboratory’ with an overall score of 0.30 and a 48-fold level of variation across states. Only 14.1% of PHCs had all 4 antibiotics recommended by the IPHS for treatment of cervicitis and sexually transmitted infections per national guidelines (Appendix 2). Less than a quarter of PHCs (23.4%) had a ‘medical officer’ (classified as ‘lady medical officers’ on the questionnaire), which contributed to the lower scores for ‘Potential Staffing’ at this health facility level (Appendix 2). One-third of PHCs met IPHS standards for communication equipment – having a functioning telephone, computer and internet.
Table 3.
Facility readiness scores for cervical cancer screening in India/states and union territories at the primary health centre level*.
| India and States/UT’s | Composite Score |
Potential Staffing |
Infrastructure | Equipment & Supplies |
Infection & Prevention |
Medicines & Laboratory |
Data Management |
|---|---|---|---|---|---|---|---|
| India | 0.559 | 0.461 | 0.637 | 0.783 | 0.677 | 0.297 | 0.499 |
| Andaman & Nicobar Island | 0.776 | 0.9 | 0.677 | 0.949 | 0.728 | 0.864 | 0.54 |
| Goa | 0.738 | 0.854 | 0.739 | 0.791 | 0.667 | 0.529 | 0.851 |
| Haryana | 0.738 | 0.624 | 0.876 | 0.961 | 0.838 | 0.292 | 0.835 |
| Maharashtra | 0.724 | 0.534 | 0.871 | 0.972 | 0.856 | 0.586 | 0.525 |
| Tamil Nadu | 0.72 | 0.74 | 0.867 | 0.97 | 0.842 | 0.401 | 0.503 |
| Sikkim | 0.71 | 0.755 | 0.747 | 0.957 | 0.648 | 0.482 | 0.672 |
| Meghalaya | 0.694 | 0.766 | 0.746 | 0.968 | 0.667 | 0.431 | 0.584 |
| Rajasthan | 0.689 | 0.505 | 0.753 | 0.88 | 0.781 | 0.405 | 0.81 |
| Andhra Pradesh | 0.685 | 0.707 | 0.718 | 0.925 | 0.649 | 0.479 | 0.63 |
| Mizoram | 0.649 | 0.587 | 0.694 | 0.896 | 0.666 | 0.367 | 0.684 |
| Punjab | 0.642 | 0.662 | 0.734 | 0.849 | 0.776 | 0.256 | 0.575 |
| Karnataka | 0.636 | 0.482 | 0.747 | 0.9 | 0.847 | 0.439 | 0.4 |
| Uttarakhand | 0.619 | 0.458 | 0.738 | 0.864 | 0.75 | 0.253 | 0.65 |
| Puducherry | 0.589 | 0.657 | 0.684 | 0.768 | 0.81 | 0.345 | 0.274 |
| Bihar | 0.571 | 0.484 | 0.61 | 0.691 | 0.736 | 0.169 | 0.736 |
| Manipur | 0.566 | 0.79 | 0.479 | 0.839 | 0.529 | 0.343 | 0.417 |
| Tripura | 0.556 | 0.732 | 0.56 | 0.702 | 0.652 | 0.104 | 0.587 |
| Nagaland | 0.55 | 0.511 | 0.588 | 0.854 | 0.566 | 0.342 | 0.437 |
| Chhattisgarh | 0.54 | 0.338 | 0.595 | 0.828 | 0.543 | 0.284 | 0.651 |
| Assam | 0.51 | 0.513 | 0.655 | 0.842 | 0.693 | 0.203 | 0.152 |
| Madhya Pradesh | 0.501 | 0.273 | 0.562 | 0.739 | 0.699 | 0.296 | 0.439 |
| Jharkhand | 0.485 | 0.442 | 0.449 | 0.818 | 0.491 | 0.307 | 0.404 |
| Arunachal Pradesh | 0.473 | 0.465 | 0.502 | 0.711 | 0.466 | 0.28 | 0.413 |
| Kerala | 0.473 | 0.587 | 0.587 | 0.574 | 0.547 | 0.318 | 0.226 |
| Himachal Pradesh | 0.463 | 0.313 | 0.512 | 0.592 | 0.743 | 0.235 | 0.385 |
| West Bengal | 0.362 | 0.52 | 0.434 | 0.38 | 0.515 | 0.135 | 0.189 |
| Uttar Pradesh | 0.33 | 0.183 | 0.359 | 0.517 | 0.419 | 0.064 | 0.441 |
| Odisha | 0.314 | 0.238 | 0.399 | 0.613 | 0.499 | 0.018 | 0.117 |
Scores are shaded from red to green to help the viewer read and interpret a range numbers, with red indicating the lowest and green the highest scores; States/UTs are ranked according to the Composite score; No Primary Health Centres in Chandigarh were sampled as part of the DLHS-4.
4.3. Facility readiness at the Community Health Centre (CHC) level
Nationwide, CHCs had an overall composite score of 0.76, with higher scores in general than SHCs and PHCs (Table 4). The highest scoring states catered to smaller geographic areas and populations eg, (Sikkim, 0.87). ‘Potential Staffing’ scored the highest (mean = 0.96) with nearly one third of states (n = 9) reaching a perfect score of 1.0; these 9 states included 4 with smaller populations (eg, Chandigarh), 4 in the north-east (eg, Meghalaya) and 1 in the west (West Bengal). The lowest scoring category for CHC's was ‘Medicines and Laboratory’ (mean = 0.52) with less than a quarter (23.6%) stocked with the reproductive tract infection/sexually transmitted drugs under the Reproductive and Child Health Programme (Appendix 3).
Table 4.
Facility readiness scores for cervical cancer screening in India/states and union territories at the community health centre level.
| India and States/UT’s | Composite Score |
Potential Staffing |
Infrastructure | Equipment & Supplies |
Infection & Prevention |
Medicines & Laboratory |
Data Management |
|---|---|---|---|---|---|---|---|
| India | 0.760 | 0.956 | 0.803 | 0.820 | 0.719 | 0.520 | 0.743 |
| Goa | 0.884 | 1.000 | 0.929 | 0.958 | 0.750 | 0.667 | 1.000 |
| Sikkim | 0.869 | 1.000 | 0.714 | 0.833 | 1.000 | 0.667 | 1.000 |
| Rajasthan | 0.855 | 0.969 | 0.884 | 0.845 | 0.756 | 0.747 | 0.930 |
| Punjab | 0.851 | 0.948 | 0.863 | 0.910 | 0.867 | 0.656 | 0.863 |
| Maharashtra | 0.836 | 0.995 | 0.919 | 0.899 | 0.838 | 0.798 | 0.568 |
| Andaman & Nicobar Island | 0.836 | 1.000 | 0.893 | 0.833 | 0.750 | 0.917 | 0.625 |
| Haryana | 0.809 | 0.877 | 0.902 | 0.847 | 0.771 | 0.557 | 0.901 |
| Puducherry | 0.800 | 0.886 | 0.939 | 0.952 | 0.857 | 0.667 | 0.500 |
| Tamil Nadu | 0.799 | 0.926 | 0.893 | 0.934 | 0.835 | 0.660 | 0.542 |
| Madhya Pradesh | 0.795 | 0.950 | 0.810 | 0.810 | 0.720 | 0.720 | 0.762 |
| Karnataka | 0.784 | 0.889 | 0.879 | 0.855 | 0.743 | 0.771 | 0.570 |
| Chandigarh | 0.772 | 1.000 | 0.714 | 1.000 | 0.750 | 0.667 | 0.500 |
| Andhra Pradesh | 0.768 | 0.977 | 0.771 | 0.850 | 0.688 | 0.669 | 0.650 |
| Uttarakhand | 0.767 | 0.978 | 0.821 | 0.839 | 0.738 | 0.467 | 0.758 |
| Himachal Pradesh | 0.757 | 0.948 | 0.759 | 0.859 | 0.688 | 0.545 | 0.740 |
| West Bengal | 0.754 | 1.000 | 0.813 | 0.797 | 0.740 | 0.298 | 0.878 |
| Chhattisgarh | 0.751 | 0.954 | 0.735 | 0.754 | 0.698 | 0.514 | 0.849 |
| Meghalaya | 0.748 | 1.000 | 0.673 | 0.857 | 0.696 | 0.548 | 0.714 |
| Mizoram | 0.739 | 1.000 | 0.727 | 0.833 | 0.659 | 0.576 | 0.636 |
| Uttar Pradesh | 0.725 | 0.986 | 0.741 | 0.776 | 0.662 | 0.293 | 0.889 |
| Bihar | 0.706 | 0.894 | 0.779 | 0.672 | 0.761 | 0.324 | 0.809 |
| Odisha | 0.702 | 0.927 | 0.772 | 0.792 | 0.709 | 0.288 | 0.726 |
| Jharkhand | 0.697 | 0.983 | 0.683 | 0.733 | 0.706 | 0.522 | 0.553 |
| Nagaland | 0.695 | 0.900 | 0.626 | 0.810 | 0.429 | 0.762 | 0.643 |
| Kerala | 0.677 | 0.757 | 0.802 | 0.790 | 0.609 | 0.676 | 0.427 |
| Arunachal Pradesh | 0.670 | 1.000 | 0.625 | 0.808 | 0.429 | 0.384 | 0.774 |
| Manipur | 0.662 | 0.950 | 0.545 | 0.760 | 0.469 | 0.563 | 0.688 |
| Assam | 0.660 | 0.984 | 0.767 | 0.794 | 0.619 | 0.329 | 0.467 |
| Tripura | 0.645 | 1.000 | 0.584 | 0.712 | 0.500 | 0.303 | 0.773 |
Scores are shaded from red to green to help the viewer read and interpret a range numbers, with red indicating the lowest and green the highest scores; States/UTs are ranked according to the composite score.
4.4. Facility readiness at the district/sub-divisional hospital (SDH) level
DH/SDH category scores, which included 2 new domains – ‘Services’ and ‘Procurement and Supply chain’, were on average, higher than those of CHCs, and the highest scoring states were smaller in size and population (eg, Puducherry, 0.96, Table 5). Sixty-nine percent of DHs conducted Pap smear testing (‘Services’) and 96% of hospitals maintained stock registers for equipment and supplies yielding perfect scores for a majority of states in ‘Procurement and Supply Chain. Categories with the highest overall scores included ‘Potential Staffing’ (mean =0.98) and ‘Procurement and Supply Chain’ (mean = 0.96) with perfect scores for 18 states in staffing and for 9 states in procurement/supply chain. On average, 97% of DH's had staff that could be trained to perform all of the methodologies with a maximum score observed across high-income states such as Goa and Chandigarh, as well as low-income states such as Odisha and Jharkhand. Of the nation's DH's, 89% could provide STI treatment, 90% had pregnancy and 65% had human immunodeficiency virus (HIV) tests available. A close examination of the district-level composite scores (Fig. 1) reveals that several of the bigger states such as – Uttar Pradesh, Madhya Pradesh and Odisha - have a wide range of performance at the district level, with districts belonging to both the bottom as well as top 20 ranking districts. This suggests substantial heterogeneity within a state that should also be considered.
5. Sensitivity analyses
5.1. Health personnel changes who conduct VIA screening, LEEP and colposcopy procedures
Sensitivity analyses were conducted to capture deviations from the guidelines, whereby designated centres and personnel for screening were changed due to limitations in infrastructure and resources. Certain centres (SHCs) and providers (accredited social health activists (ASHAs), ANMs) were not equipped to roll out cervical cancer screening, and only certain health providers (e.g., Ob/Gyn and medical officers) were designated to conduct the LEEP and colposcopy procedures, which changed ‘Potential Staffing’ scores. When we conducted a sensitivity analysis to reflect this scenario, the overall average facility readiness scores at the PHC level stayed the same (0.56) and slightly reduced at the CHC (0.75 to 0.72), and SDH (0.84 to 0.83) levels. The relative ranking of most states did not substantially change either.
6. Discussion
An evaluation of DLHS-4 data on facility readiness for cervical cancer screening shows wide variation across states, domains and 4-tiers of India's public health care system. Goa and Maharashtra were in the top 5 composite score rankings for 3 out of 4 facility levels. Goa was an early state to undergo the epidemiological transition towards a dominant NCD burden, and as a smaller state, may be better equipped to carry out early detection programmes for NCDs more effectively. Maharashtra hosts the country's leading comprehensive cancer centre, some of the oldest urban and rural population-based cancer registries (Shastri et al., n.d.; Kaur and Suresh, 2013; The burden of cancers and their variations across the states of India: the Global Burden of Disease Study 1990-2016, 2018), and sites of randomized trials in cervical cancer screening. While a few smaller states/union territories (<1.5 million population size as of Census 2011) tended to have higher composite scores (for eg. Sikkim, Chandigarh), medium-size (25–30 million population size) and larger states (90 million or greater) states such as Punjab, and West Bengal respectively also fared well. Composite scores tended to increase for higher facility levels of care though the scores are not directly comparable since criteria for developing these scores differed at each level (Appendix Tables 1-4).
Our analysis suggests that the biggest challenges to overcome in India's public health facilities include gaps in ‘Infection Prevention’ and ‘Infrastructure’ at SHCs, and ‘Medicine and Laboratory Testing’ and ‘Potential staffing’ at PHCs. Specifically, autoclave availability was low (27%) at SHCs, where most did not have an adequate mode of disposal of infectious/biological waste (39% following ICMR guidelines). At CHCs, only one fourth (24%) had the required antibiotics for treating sexually transmitted infections (STI's). A potentially important barrier for community uptake is a satisfactory, clean layout and space to conduct private cervical examinations, which was present in less than half (45%) of SHCs. At PHCs, a major gap was lack of antibiotics for STIs (14%) and only 23% had a ‘medical officer’ for referrals, management and treatment of positive cases. Our assessment also suggests challenges in effective linkages and referral pathways and monitoring and evaluation at PHCs; a telephone, computer and internet were only available for a third (34%) and a smaller proportion for data entry staff (27%).
Lower scores at SHCs and PHCs - where the majority of cancer screening at the population level is to be implemented - suggests a need to focus on gaps at these facility levels for successful implementation of the guidelines on oral, breast and cervical cancers. This was recognized by the government's nodal training agency for cancer screening, the National Institute for Cancer Prevention Research (NICPR), during implementation; in recognition of these gaps, there was a reliance on PHCs instead of SHCs for cervical cancer screening. Our sensitivity analysis however, suggests similar results; there was a slight decrease in scores for CHCs and SDHs when limiting the diagnostic and treatment follow-up to specialists. In an effort to improve and learn as the programme is rolled out, there are efforts to identify the performance of health centres in rolling out screening for common NCDs using mobile-based applications and research on dashboards to identify problem hotspots (Pati et al., 2013). Since the time of the DLHS-4 survey, there has been a nationwide increase to address the shortfall of health care workers at the SHC and PHC levels in rural areas; from 2012 to 2018, there was a 12.8% increase in female health workers and ANMs at the SHC/PHC level, and a 2.8% increase in doctors at PHCs. This reduced the shortfall from 10.3% in 2012 (Rural Health Statistics 2012, 2012) to 6.0% in 2018 (Rural Health Statistics 2018, 2018); other changes in health infrastructure may have also improved over time, though data are not yet available to analyze.
According to the operational guidelines of cancer screening released by the Government of India (Government of India, 2016) women aged 30 years and older should undergo cervical cancer screening by VIA at least once every 5 years by trained female health workers and auxiliary nurse midwives at SHC's, and by trained staff nurses at PHC's, with positive tests referred to the PHC/CHC/DH for further evaluation and management by a trained ‘medical officer’ or gynecologist (Bagcchi, 2016; Government of India, 2016). We observed lower staffing scores at PHCs than at SHCs, which is largely due to a low proportion with ‘medical officers’ (23%) and staff nurses, which are required for confirmation of positive VIA and to perform cryotherapy in eligible cases. Screening implementation is further challenged by a decentralized healthcare system with limited resources, state-driven health agendas and inadequate financial coverage/protection (Chalkidou et al., 2014). While health spending (Kaur and Suresh, 2013) may positively correlate with facility readiness scores in some states (e.g., Goa), the same was not observed in others (e.g., Bihar which has higher spending but lower scores), highlighting the challenges in pinpointing factors that are driving the facility readiness scores.
There are important aspects of a successful screening programme for cancer that are not captured in our findings. For example, ASHAs play a crucial role in motivating eligible women in the community to come to their screening site (SHCs), which is not captured by the DLHS-4. Future surveys could capture these and other referral and diagnostic pathway points and processes, which are necessary links and common problems (Nicholson et al., 2018).
To ensure better uptake of screening at the SHC and PHC levels, additional strategies could include raising public awareness on cancer prevention and early detection, addressing fear and stigma and monitoring knowledge levels – “pull”-related factors to increase demand for services (Krishnan et al., 2015; Nyblade et al., 2017). The IDCCP toolkit contains 13 categories for addressing facility readiness, of which we evaluated 8 (6 for all levels and 2 additional categories for DHs) based on available DLHS-4 data; other categories such as service utilization, referral mechanisms and community sensitization, can address important gaps and be considered for inclusion in future DLHS surveys. Moreover, the toolkit encompasses a broad range of cervical cancer screening and control strategies, including the Pap smear, HPV testing and vaccination, so it can be applied as cancer screening strategies and recommendations evolve for the country (Kaur et al., 2017; Sankaranarayanan et al., 2018). As India launches cervical, breast and oral screening, this analysis can highlight gaps for states to focus their efforts for successful implementation of cancer screening, and to set performance standards going forward. Our study of the assessment of quality of screening delivery provides critical information regarding the facilitators and barriers to implement cancer screening; this information is essential for strengthening cancer programs. Other aspects of successfully launching a screening programme, such as monitoring and evaluation (Sivaram et al., 2018) to measure aspects such as trained personnel, meeting targets for screening and follow-up, supportive infrastructure as well as quality standards (Sivaram et al., 2018) can be integrated into DLHS surveys.
7. Conclusion
Our findings suggest wide variation in facility readiness across the country for cervical cancer screening as India prepares to implement screening programme. In particularly, deficits in infrastructure and staffing at the PHC-level may pose major barriers to the cervical cancer screening flow as envisioned by the current guidelines. The top 5 states/territories for each facility level included 2–3 smaller states or union territories, as well the second most populous state, Maharashtra. The IDCCP toolkit provides a method and measurement for assessing standards and performance across India's health care system as cervical cancer screening is rolled out across the country, and over time for adapting and improving screening implementation.
Supplementary Material
Acknowledgements
The study was supported by the U.S. Centers for Disease Control and Prevention (CDC) through its cooperative agreement (5NU380T000203-04) with the National Network of Public Health Institutes (NNPHI) and sub-award to the Public Health Institute (PHI).”
Footnotes
Declaration of competing interest
The authors have no conflicts of interest to disclose
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ypmed.2020.106147.
References
- Bagcchi S, 2016. India Launches Plan for National Cancer Screening Programme. British Medical Journal Publishing Group, In. [DOI] [PubMed] [Google Scholar]
- Chalkidou K, Marquez P, Dhillon PK, et al. , 2014. Evidence-informed frameworks for cost-effective cancer care and prevention in low, middle, and high-income countries. The lancet oncology 15 (3), e119–e131. [DOI] [PubMed] [Google Scholar]
- Dandona L, Dandona R, Kumar GA, et al. , 2017. Nations within a nation: variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease Study. Lancet 390 (10111), 2437–2460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond JL, Were MC, Arrossi S, Wools-Kaloustian K, 2017. Cervical cancer data and data systems in limited-resource settings: challenges and opportunities. Int. J. Gynecol. Obstet 138, 33–40. [DOI] [PubMed] [Google Scholar]
- Government of India. Ministry of Health and Family Welfare. Statistics Division. Rural Health Statistics in India 2012. 2013; Available from https://nrhm-mis.nic.in/SitePages/HMIS-Publications.aspx?RootFolder=%2FPubStatistical_Publications%2FRural%20Health%20Statistics&FolderCTID=0x012000AC878C9A74E6DC46A4B9220C1AAC27300098F49E13CE4ED442AB009F0A97E0CFFA&View=%7b963874F4-C1DD-4335-9EEB-C1FC961508FB%7d [Accessed 15 October 2017]. [Google Scholar]
- Government of India. Ministry of Health and Family Welfare. Operational Framework Management of Common Cancers. 2016; Available from http://nicpr.res.in/images/pdf/Operational_Framework_Management_of_Common_Cancers.pdf [Accessed 15 October 2017]. [Google Scholar]
- Kaur B M S, Suresh AK. Cyclicality of Social Sector Expenditures: Evidence from Indian States. Reserve Bank of India;2013. [Google Scholar]
- Kaur P, Mehrotra R, Rengaswamy S, et al. , 2017. Human papillomavirus vaccine for cancer cervix prevention: Rationale & recommendations for implementation in India. Indian J. Med. Res 146 (2), 153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan S, Sivaram S, Anderson BO, et al. , 2015. Using implementation science to advance cancer prevention in India. Asian Pacific journal of cancer prevention: APJCP 16 (9), 3639–3644. [DOI] [PubMed] [Google Scholar]
- Ministry of Health and Family Welfare GoI. Operational framework. Management of common cancers. In: 2016. [Google Scholar]
- Ministry of Health and Family Welfare GoI. National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular disease & Stroke National Health Mission. [Google Scholar]
- National Health System Resource Centre. Ministry of Health & family Welfare. Ayushman Bharat Comprehensive Primary Health Care through Health & Wellness Centres. Operational Guidelines. In. [Google Scholar]
- Nicholson BD, Oke J, Smith CF, et al. , 2018. The Suspected CANcer (SCAN) pathway: protocol for evaluating a new standard of care for patients with non-specific symptoms of cancer. 8 (1), e018168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyblade L, Stockton M, Travasso S, Krishnan S, 2017. A qualitative exploration of cervical and breast cancer stigma in Karnataka, India. BMC Womens Health 17 (1), 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pati S, Hussain MA, Chauhan AS, Mallick D, Nayak S, 2013. Patient navigation pathway and barriers to treatment seeking in cancer in India: a qualitative inquiry. Cancer Epidemiol. Biomark. Prev 37 (6), 973–978. [DOI] [PubMed] [Google Scholar]
- Rural Health Statistics 2012 New Delhi, India: Ministry of Health and Family Welfare, Government of India;2012. [Google Scholar]
- Rural Health Statistics 2018 New Delhi, India: Ministry of Health and Family Welfare, Government of India;2018. [Google Scholar]
- Sankaranarayanan R, Esmy PO, Rajkumar R, et al. , 2007. Effect of visual screening on cervical cancer incidence and mortality in Tamil Nadu. India: a cluster-randomised trial 370 (9585), 398–406. [DOI] [PubMed] [Google Scholar]
- Sankaranarayanan R, Joshi S, Muwonge R, et al. , 2018. Can a single dose of human papillomavirus (HPV) vaccine prevent cervical cancer? Early findings from an Indian study. Vaccine. 36 (32), 4783–4791. [DOI] [PubMed] [Google Scholar]
- Senkomago V, Duran D, Loharikar A, et al. , 2017. CDC activities for improving implementation of human papillomavirus vaccination, cervical cancer screening, and surveillance worldwide. Emerg. Infect. Dis 23 (Suppl. 1), S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shastri SS, Mittra I, Mishra GA, et al. Effect of VIA screening by primary health workers: randomized controlled study in Mumbai, India. Journal of the National Cancer Institute. 2014;106(3):dju009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shastri SS, Mittra I Fau - Mishra GA, Mishra Ga Fau - Gupta S, et al. n.d. Effect of VIA screening by primary health workers: randomized controlled study in Mumbai, India. (1460–2105 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivaram S, Majumdar G, Perin D, et al. , 2018. Population-based cancer screening programmes in low-income and middle-income countries: regional consultation of the International Cancer Screening Network in India. The Lancet Oncology 19 (2), e113–e122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The burden of cancers and their variations across the states of India: the Global Burden of Disease Study 1990–2016. Lancet Oncol. 2018;19(10):1289–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. WHO guidelines: WHO guidelines for screening and treatment of precancerous lesions for cervical cancer prevention. 2013; Available from https://apps.who.int/iris/bitstream/handle/10665/94830/9789241548694_eng.pdf;jsessionid=1403DC3001F7F14FD5906FA2BB0CBB56?sequence=1 [Accessed on 15 October 2017]. [PubMed]
- World Health Organization, 2018. Licence: CC BY-NC-SA 3.0 IGO. and add link, https://www.who.int/ncds/surveillance/data-toolkit-for-cervical-cancer-prevention-control/en/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.