Abstract
Objective
The objective of this study is to measure the level of knowledge and practice of diabetic foot self-care and determine the factors that affect the level and knowledge and practice of diabetic foot self-care among among patients with diabetes..
Methodology
Three hundred thirty adult patients with diabetes at the outpatient clinics were given self-administered questionnaires on knowledge and practice of diabetic foot self-care. The scores were computed based on their answers. A score of >70% was gauged as good, 50 to 70% as satisfactory and <50% as poor.
Results
Of the subjects, 82.7% had good foot care knowledge, 22.4% had good foot self-care practice, and 71% had satisfactory practice score. Patients who received diabetes education were twice as likely to have a good knowledge score (OR 2.41, 95% CI, 1.09 to 5.32; p=0.03). Compared to patients who received diabetes care in private clinics, those who attended the charity outpatient clinic were nearly three times as likely to have a good knowledge score (OR 2.8, 95% CI, 1.32 to 5.96; p=0.007). Patients with known diabetes for more than ten years and those with a family history of diabetes were 50% less likely to have good practice scores (OR 0.50, 95% CI, 0.28 to 0.90; p=0.021 and OR 0.49, 95% CI, 0.29 to 0.83; p=0.008, respectively).
Conclusion
The current state of foot care knowledge in Filipino respondents with diabetes is good but the level of foot self-care practice is only satisfactory.
Keywords: diabetic foot, diabetes mellitus, knowledge, self-care
INTRODUCTION
Among the complications of diabetes, those that occur in the foot are considered the most preventable. The annual incidence of new foot ulcer in patients with diabetes is 2.2%, with incidence increasing to 5.8% in three years.1,2 The lifetime incidence of developing a foot ulcer is estimated to be as high as 25%.3,4 Poor knowledge and poor foot care practices were identified as important risk factors for foot problems in diabetes.5 Hence, in order to minimize, if not totally prevent, foot complications, it is important that appropriate and timely foot self-care be emphasized to patientsÊwith diabetes.6-8
A previous study showed that patients with diabetes often neglect foot self-care practices. The same study concluded that foot self-care practices appear underutilized as a primary complication prevention measure. Instead, patients only adopt foot care practices once complications have already occurred. Facilitators of foot self-care practices, such as patient education, appear to be reserved for individuals who have already developed foot complications.9
Prior to instructing proper self-care techniques to a patient, it is essential for the health care professional to understand the extent of the said patient’s knowledge and practice. The authors found, during the conduct of this study, that administration of standardized written questionnaires was helpful in establishing a patient’s baseline knowledge on self-care. By establishing the baseline knowledge level of the subject patients, healthcare providers may be able to determine the gaps in their knowledge and practice on foot self-care and provide feedback. Diabetes education will then be more effective in the prevention of foot complications through proper foot care.
Based on extensive literature search by the authors, there is no locally conducted study that has investigated the knowledge and foot self-care practices carried out by patients. This study aimed to determine the knowledge and practice of foot care among Filipinos with diabetes in our institution using knowledge questionnaires (Appendices 1 and 2).10,11 We also sought to identify factors that affect the level of knowledge and practice of foot selfcare. The results of this study can provide information to clinicians and healthcare providers on proper foot care.
Health care professionals and educators may use the results of this study in the formulation of modules for diabetes-related education.
METHODOLOGY
This cross-sectional analytical study was conducted for 3 months among patients with diabetes who consulted at the Outpatient Clinics of the Chinese General Hospital and Medical Center (CGHMC), a tertiary level hospital in Manila, Philippines. The study protocol and informed consent forms were submitted to and approved by the institutional Research Ethics Review Board.
The authors used the Knowledge questionnaire developed by Hasnain and colleagues and the Nottingham Assessment of Functional Foot Care (NAFFC) (Appendices 1 and 2).10,11 Both questionnaires were translated to the local vernacular to ensure that these would be fully understood by the patients (Appendices 3 and 4). Language experts in Filipino and English performed the forward and back translations, respectively. Ten respondents deemed eligible by the inclusion and exclusion criteria provided their opinion regarding the relevance and phrasing of the Filipino translated questions. Eight internal medicine specialists and subspecialists evaluated content validity of the final forward translated questionnaires, while 10 patients were asked to assess face validity. To determine if the Filipino version would elicit the same answers over time, it was administered twice to 10 respondents with an interval of three days in-between. Reliability of answers was analyzed using the test-retest method.12
Patients with type 1 or type 2 diabetes of any duration, age 18 years and older, were recruited for the actual survey. They must be able to read, comprehend and understand Filipino or English, and consent to participate in the study. The diagnosis of diabetes mellitus was based on the Unite for Diabetes Philippines Clinical Practice Guidelines: fasting plasma glucose ≥126 mg/dL (7.0 mmol/L) after an overnight fast, two-hour plasma glucose ≥200 mg/dL (11.1 mmol/L) during an oral glucose tolerance test, or random plasma glucose ≥200 mg/dL (11.1 mmol/L) in a patient with classic symptoms of hyperglycemia or with signs and symptoms of hyperglycemic crisis.13 Exclusion criteria were impaired fasting glucose, impaired glucose tolerance and gestational diabetes.
To ensure a high response rate, the principal investigator conducted a recruitment process and gave cover letters in English and Filipino to fully explain the purpose of the study, its significance, its risks and benefits and the personal information needed. It was emphasized that the results of this study will be used to improve how healthcare providers may improve diabetes education on proper foot self-care. Patients who qualified and gave consent were then recruited.
The respondents were encouraged to complete all the questionnaires. Pamphlets on proper foot care were given to the patients after participating in the study as a form of incentive. Patients were also advised on proper foot care after answering the questionnaire. As a matter of poststudy intervention and correction of incorrect answers in the Knowledge and Practice Questionnaire, the authors taught the respondents proper foot care practice after their participation in the study.
Information collected per respondent included age, gender, address, contact number, duration of diabetes, family history of diabetes, medications, educational attainment, smoking history, family monthly income bracket (to assess economic status based on the Philippine Statistics Authority income bracket),14 latest HbA1c when available, and where the patient received diabetes care and information on diabetes foot care. Patient history and present foot problems such as ulcers, blisters, calluses, wounds, non-healing wounds for more than two weeks, foot surgery (debridement or amputation) and paresthesia were likewise recorded.
The authors used a 15-item questionnaire answerable with “yes,” “no” and “I don’t know” on knowledge of diabetic foot care developed by Hasnain et al., and used by the groups of Muhammad-Lufti and Seid (Appendix 1).10,15,16 Knowledge score was determined based on the proportion of correct answers. The level of knowledge was assessed as good if the score was more than 70% (11 to 15 correct answers out of 15). Scores of 50 to 70% (8 to 10 correct answers) were categorized as satisfactory knowledge. Scores less than 50% (7 or below correct answers) were evaluated as poor knowledge.
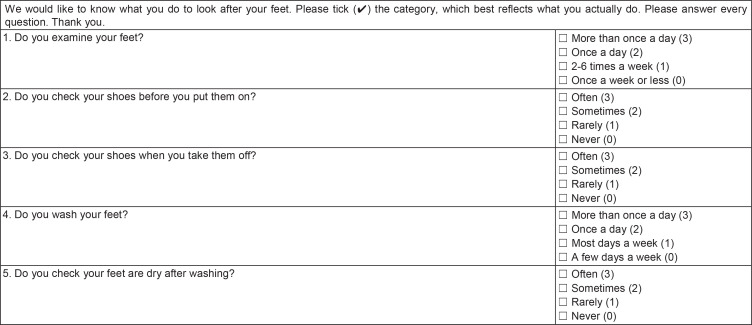
Responses to questions of the translated NAFFC were recorded on a categorical scale (scored 0 to 3) according to the frequency of occurrence of the behavior.11 The NAFFC consists of 29 independent questions (Appendix 2). Pictures of examples of footwear accompanied the questionnaires. Scoring on practice was arbitrarily gauged as good for scores more than 70% (61 and above). Scores of 50 to 70% (43 to 60) were considered satisfactory practice. Scores less than 50% (42 and below) were labeled as poor practice.
A minimum of 324 subjects was required for this study based on a level of significance of 5%, with a desired width of confidence interval of 10% and a prevalence of 30.1% of good knowledge of diabetic foot care among patients with diabetes mellitus noted in the reference article by Desalu et al.17,18
Descriptive statistics were used to summarize the clinical characteristics of the patients. Frequency and proportion were used for nominal variables, while mean and standard deviation (SD) were applied for interval/ratio variables. Wilcoxon signed rank test was used to determine the content validity of the translated questionnaire using ratings from the panel of experts. Odds ratios and corresponding 95% confidence intervals from binary logistic regression were computed to determine significant predictors for good knowledge and practice of diabetic patients. All valid data were included in the analysis. Missing variables were neither replaced nor estimated. Null hypothesis was rejected at 0.05 α-level of significance. STATA 12.0 was used for data analysis.19
RESULTS
We enrolled a total of 330 patients for this study, with a mean age (±SD) of 59.09 (±12.69) years. They were predominantly female (66%) and married (65%). Half of the patients were unemployed, and half were at least college graduates. Approximately 4 in 10 patients had a monthly family income of below PhP 15,000 (Table 1).
Table 1.
Socio-demographic and diabetes-related profile of the individuals with diabetes
| Characteristic | Frequency (%) |
|---|---|
| Mean age, yr | 59.09 ± 12.69 |
| Female gender | 218 (66.06) |
| Civil status | |
| Single | 38 (11.52) |
| Married/cohabiting | 223 (67.57) |
| Widowed/annulled/separated | 69 (20.91) |
| Occupation | |
| None | 166 (50.30) |
| Employed | 74 (22.42) |
| Self-employed | 67 (20.30) |
| Professional | 23 (6.97) |
| Educational attainment | |
| No formal training | 6 (1.82) |
| Elementary | 38 (11.52) |
| High school graduate | 94 (28.48) |
| Vocational | 8 (2.42) |
| College graduate | 161 (48.79) |
| Postgraduate | 23 (6.97) |
| Monthly family income, PhPa | |
| Below 15,000 | 143 (43.33) |
| 15,000 to 32,000 | 93 (28.18) |
| 32,000 to 80,000 | 45 (13.64) |
| 80,000 to 120,000 | 26 (7.88) |
| More than 120,000 | 23 (6.97) |
| Mean duration of diabetes | |
| Less than a year | 43 (13.03) |
| 1 to 5 years | 94 (28.48) |
| 5 to 10 years | 75 (22.73) |
| More than 10 years | 118 (35.76) |
| Medication | |
| None | 3 (0.91) |
| Oral | 198 (60) |
| Insulin-requiring | 129 (39.09) |
| Attended diabetes education | 85 (25.76) |
| Information source of diabetic foot care | |
| Diabetes Center | 61 (18.48) |
| Reading materials | 73 (22.12) |
| Doctor | 134 (40.61) |
| Relatives/neighbors | 33 (10) |
| Lay forum/lectures | 39 (11.82) |
| No information | 106 (32.12) |
| Receives diabetic care | |
| Private clinic | 227 (68.79) |
| Charity outpatient clinic | 103 (31.21) |
| Family history of diabetes | 221 (66.97) |
| Previous smoker/Smoker | 96 (29.09) |
| Mean HbA1cb | 7.57 ± 2.06 |
Table 1 provides the clinical profile of the patients. Of 330, there were 118 (36 %) with diabetes for more than 10 years, and 129 (39%) were insulin requiring. About a quarter (26%) of the patients had attended diabetes education. Only 18% of the subjects received proper foot self-care from the Diabetes Center.
The mean (±SD) knowledge and practice scores were 86.7% (± 16) or good and 63.2% (± 8.7) or satisfactory.
Among the 330 respondents, 82.7%, 13.3%, and 3.9% had good, satisfactory, and poor knowledge, respectively. Nearly one-third (31.5%) of respondents gave an incorrect answer or “I don’t know” when asked if lukewarm water should be used for washing the feet. More than half (53%) of the patients were not aware that lotion should not be applied in between toes, and that talcum powder be used to keep the areas between the toes dry.
Regarding the level of practice on foot self-care, only 22.4% had good practice while 71.2% and 6.4% had satisfactory and poor scores, respectively. Majority of the patients examined their feet daily (76%), washed their feet daily (97%), did not use nylon stockings (71%), never used pointed shoes (77%), did not place their feet near hot objects (83 to 96%) and did not use corn paints or plasters (72%). More than half checked their shoes before putting them on (57%), dried the areas between the toes (63%), did not put lotion in between toes (54%), often checked that their feet were dry after washing (60%) and cut their toenails weekly (61%).
Although 71% of patients had satisfactory practice scores, there were foot care practices that were not observed by patients. Majority of them did not use lotion on their feet (60%), did not regularly inspect their footwear after taking them off (69%), and did not wear slippers most of the time (77%). More than 30% of the patients never practiced breaking-in new shoes, never wore seamless socks, wore shoes without socks and never checked the temperature of the water they used for washing feet. More than 60% never used dressing when they had blisters or wounds on their feet. About 45% walked barefoot indoors and about 13% walked barefoot outdoors.
We conducted simple binary logistic regression to determine factors associated with knowledge scores (Table 2). Patients who received diabetes education were twice as likely to have a knowledge score above 70% (OR 2.41, 95%CI, 1.09 to 5.32; p=0.03). Similarly, compared to patients who received diabetic care in private clinics, patients who attended the charity outpatient clinic were nearly three times as likely to have a knowledge score above 70% (OR 2.8, 95% CI, 1.32 to 5.96; p=0.007).
Table 2.
Factors associated with knowledge scores of the individuals with diabetes
| Characteristic | Knowledge score >70% (n=273) | Knowledge score ≤70% (n=57) | Crude odds ratio (95% CI) | p-value |
|---|---|---|---|---|
| Socio-demographic factors | ||||
| Age 60 and above, yr | 138 (50.55) | 27 (47.37) | 1.14 (0.64-2.01) | 0.662 |
| Gender | ||||
| Male | 93 (34.07) | 19 (33.33) | (reference) | - |
| Female | 180 (65.93) | 38 (66.67) | 0.97 (0.53-1.77) | 0.915 |
| Civil status | ||||
| Single | 33 (12.09) | 5 (8.77) | (reference) | - |
| Married/cohabiting | 178 (65.2) | 45 (78.95) | 0.60 (0.22-1.62) | 0.314 |
| Widowed/annulled/separated | 62 (22.71) | 7 (12.28) | 1.34 (0.40-4.56) | 0.637 |
| Occupation | ||||
| None | 142 (52.01) | 24 (42.11) | (reference) | - |
| Employed | 59 (21.61) | 15 (26.32) | 0.66 (0.33-1.36) | 0.262 |
| Self-employed | 55 (20.15) | 12 (21.05) | 0.77 (0.36-1.66) | 0.51 |
| Professional | 17 (6.23) | 6 (10.53) | 0.48 (0.17-1.34) | 0.16 |
| With college degree | 25 (9.16) | 6 (10.53) | 0.86 (0.33-2.19) | 0.748 |
| Monthly family income 32,000 and above, PhPa | 79 (28.94) | 15 (26.32) | 1.14 (0.60-2.17) | 0.69 |
| Diabetes-related factors | ||||
| Duration more than 10 yr | 98 (35.90) | 20 (30.59) | 1.04 (0.57-1.88) | 0.908 |
| Insulin-requiring | 109 (39.93) | 20 (30.59) | 1.23 (0.68-2.23) | 0.496 |
| Attendance to Diabetes Center | 77 (28.21) | 8 (14.04) | 2.41 (1.09-5.32) | 0.03 |
| Diabetes Center as source of information on foot care | 55 (20.15) | 6 (10.53) | 2.14 (0.88-5.25) | 0.095 |
| Receives diabetic care | ||||
| Private clinic | 179 (65.57) | 48 (84.21) | (reference) | - |
| Charity outpatient clinic | 94 (34.43) | 9 (15.79) | 2.8 (1.32-5.96) | 0.007 |
| Family history of diabetes | 180 (65.93) | 41 (71.93) | 0.76 (0.40-1.42) | 0.382 |
| HbA1c 7 or greater, % | 129 (49.24) | 23 (42.59) | 1.31 (0.72-2.36) | 0.374 |
| No history of foot problem | 86 (31.62) | 19 (33.33) | 0.92 (0.50-1.70) | 0.801 |
| No current foot problem | 118 (43.22) | 24 (42.11) | 1.05 (0.59-1.86) | 0.877 |
PhP, Philippine Peso
bFor n=316
In the final model, however, there was insufficient evidence to establish an association between foot care/diabetes education (adjusted OR 1.63, 95% CI, 0.68 to 3.90) or receiving diabetes care in the OPD (adjusted OR 2.28, 95% CI, 1.00 to 5.22) with knowledge scores.
We conducted simple binary logistic regression to determine factors associated with practice scores (Table 3). Patients who were self-employed were twice as likely to have a practice score above 70% compared to unemployed patients (OR 2.22, 95% CI, 1.16 to 4.23; p=0.016). Patients who had diabetes for more than 10 years were only 50% less likely to have good practice scores (OR 0.50, 95% CI, 0.28 to 0.90; p=0.021). This was also observed in those with a family history of diabetes (OR 0.49, 95% CI, 0.29 to 0.83; p=0.008). Patients who do not have current foot problems were more likely to have good practice scores (OR 1.78, 95% CI, 1.05 to 2.99; p=0.031).
Table 3.
Factors associated with good practice scores of the individuals with diabetes
| Characteristic | Practice score >70% (n=74) | Practice score ≤70% (n=256) | Crude odds ratio (95% CI) | p-value |
|---|---|---|---|---|
| Socio-demographic factors | ||||
| Age 60 and above, yr | 38 (51.35) | 127 (49.61) | 1.07 (0.64-1.80) | 0.792 |
| Gender | ||||
| Male | 32 (43.24) | 80 (31.25) | (reference) | - |
| Female | 42 (56.76) | 176 (68.75) | 0.60 (0.35-1.01) | 0.056 |
| Civil status | ||||
| Single | 8 (10.81) | 30 (11.72) | (reference) | - |
| Married/cohabiting | 52 (70.27) | 171 (66.8) | 1.14 (0.49-2.64) | 0.759 |
| Widowed/annulled/separated | 14 (18.92) | 55 (21.48) | 0.95 (0.36-2.53) | 0.926 |
| Occupation | ||||
| None | 30 (40.54) | 136 (53.13) | (reference) | - |
| Employed | 16 (21.62) | 58 (22.66) | 1.25 (0.63-2.47) | 0.519 |
| Self-employed | 22 (29.73) | 45 (17.58) | 2.22 (1.16-4.23) | 0.016 |
| Professional | 6 (8.11) | 17 (6.64) | 1.6 (0.58-4.40) | 0.362 |
| With college degree | 9 (12.16) | 22 (8.59) | 1.47 (0.65-3.35) | 0.356 |
| Monthly family income 32,000 and above, PhPa | 21 (28.38) | 73 (28.52) | 0.99 (0.56-1.76) | 0.982 |
| Diabetes-related factors | ||||
| Duration more than 10 yr | 18 (24.32) | 100 (39.06) | 0.50 (0.28-0.90) | 0.021 |
| Insulin-requiring | 28 (37.84) | 101 (39.45) | 0.93 (0.55-1.59) | 0.802 |
| Attendance to Diabetes Center | 21 (28.38) | 64 (25) | 1.19 (0.67-2.12) | 0.559 |
| Diabetes Center as source of information on foot care | 17 (22.97) | 44 (17.19) | 1.44 (0.76-2.70) | 0.26 |
| Receives diabetic care | ||||
| Private clinic | 49 (66.22) | 178 (69.53) | (reference) | - |
| Charity outpatient clinic | 25 (33.78) | 78 (30.47) | 1.16 (0.67-2.02) | 0.588 |
| Family history of diabetes | 40 (54.05) | 181 (70.70) | 0.49 (0.29-0.83) | 0.008 |
| HbA1c 7 or greater, % | 37 (52.11) | 115 (46.94) | 1.23 (0.72-2.09) | 0.443 |
| No history of foot problem | 26 (35.62) | 79 (30.86) | 1.24 (0.72-2.14) | 0.442 |
| No current foot problem | 40 (54.05) | 102 (39.84) | 1.78 (1.05-2.99) | 0.031 |
PhP, Philippine Peso
In the final model, duration and family history of diabetes were found to be significant. Those with more than 10 years of diabetes (adjusted OR 0.54, 95% CI, 0.30 to 0.98) and with family history of diabetes (adjusted OR 0.52, 95% CI, 0.30 to 0.89) were 50% less likely to have good practice scores. This model was significant, but only explains 2.78% in the variation of good and poor practice scores.
DISCUSSION
The study results show that majority of patients (83%) had good knowledge and only a small proportion (22%) had a good score on practice on foot care.
About a third of the subjects were not knowledgeable that lukewarm water should be used for washing the feet and that the temperature of the water should be checked first before using it to wash the feet. More than half of the patients were not aware about the proper use of lotion and talcum powder on the feet. The above good practices were also not practiced by patients with diabetes in Pakistan and Malaysia.10,15 Owing to our country’s tropical climate and the general unavailability of water temperature control devices in many households, most Filipinos use water that comes out of the tap or shower without checking the temperature. Also, because the common footwear of many Filipinos are open-type sandals, the subjects may not have found it necessary to use talcum powder to keep the interdigital spaces on their feet dry. This finding indicates that healthcare providers may not have emphasized proper use of lotion and talcum powder in these patients.
Good scores on knowledge were comparable to findings in India, where 75% had good knowledge.20 This is in clear contrast to the findings in Nigeria, where 78% had poor knowledge. Poor knowledge was significantly associated with poor educational attainment and low socioeconomic status.17 However, our study did not show any correlation of knowledge scores with age, gender or educational attainment.
Our study showed that those who received diabetes education from the Diabetes Center were twice as likely to have good knowledge. Individuals with diabetes from the charity clinic were nearly three times as likely to have good knowledge. More patients from the charity clinic than from private practices were enrolled in diabetes education at the Diabetes Center, likely encouraged due to lower fees. Furthermore, more charity patients attended lay forums on diabetes compared to those from private clinics.
One study showed that foot care knowledge of patients who received education on complications was much better than those who did not. Patients aware of complications were willing to take action only when they learned that these were preventable.21 Willingness to receive education to prevent diabetes-related complications should encourage healthcare providers to offer diabetes education to all patients, and healthcare institutions to improve diabetes educational programs and provide better patient access to formal diabetes education.
On the are of foot care practices, a small proportion (22%) had good practice while majority (71%) had satisfactory scores. Practices in foot self-care that most respondents did not follow included daily use of moisturizing cream or lotion, inspection of feet and footwear after use, use of adequate footwear, breaking-in shoes, use of seamless socks, checking temperature of water when washing feet, and use of dressing for blisters and wounds on feet. The most remarkable findings were that 45% of the respondents walked barefoot indoors and about 13% walked barefoot outdoors.
The scores on practice may have been affected by the choice of footwear and poor foot-care practices. Majority of patients wore slippers and flip-flops. This result is consistent with the study among Filipinos with diabetes in the preferred primary choice of footwear.22 In India and Iran, 41% and 62% of individuals with diabetes walked barefoot indoors, respectively23,24 These findings in poor foot care practice may be due to the lack of perceived immediate effect of these poor practices.
Our study also found that those who were self-employed had good self-care practices. This complements a study conducted in the southeastern United States, which found that diabetes empowerment was related to better diabetes knowledge, medication adherence and improved self-care behaviors. Emphasis on empowerment and self-efficacy is relevant to improve outcomes in the management of diabetes.25 Both studies showed that self-empowerment brought about by employment has a positive effect on the management of diabetes.
Respondents who had diabetes for more than 10 years were only 50% less likely to have good practice scores. In contrast, a study done in China found that the state of practice was influenced by duration of diabetes mellitus and education about diabetic complications.21 Patients with longer duration of diabetes and follow-up regularly got a high score in foot self-care behavior, suggesting that these patients paid more attention to self-care. However, in our study, patients were apparently less keen in practicing proper foot care practice despite the chronic duration of their diabetes.
We found that respondents with a family history of diabetes were only 50% less likely to have good practice scores, in contrast to findings in studies in Asian populations. 26,27 A possible reason for this finding in our study is that the diabetic family members of our subjects may not have had foot complications, making our subjects less cautious about foot care practices. However, this reason was not verified in our study.
Respondents who did not have current foot problems also had higher foot self-care practice scores. This echoes the findings of Nongmaithem et al., which showed that those with diabetic foot ulcers had poor foot care practice, leading to diabetic foot ulcer.28
Our study found that while the respondents had a good knowledge of diabetic foot self-care, the scores for actual practice are only satisfactory. This implies that adequate knowledge by itself does not necessarily translate to action, as shown in the study by Li et al.21 Complications such as diabetic foot ulcers and lower extremity amputations are preventable with good knowledge and good practice of diabetic foot care. Foot care education is the most crucial tool in preventing lower leg amputations necessitated by complications.29 Simple patient evaluation, coupled with concomitant preventive measures, significantly reduce the rates of risk among individuals with diabetes.
The advantage of this study was the use of the Filipino language in our questionnaires. These questionnaires were tested and validated. Respondents were shown accompanying illustrations to help them understand the type of footwear being asked. The questions covered the recommended good foot-care practices in the areas of feet washing techniques, inspection of foot and footwear, skin and nail care, footwear use, and self-foot care management. The questionnaire can be used as an outcome measure after attending or administering diabetes education on foot care for patients with and without diabetic foot ulcers.
We recognized certain limitations in our study. The subjects consisted of patients attending the CGHMC outpatient clinics, with a small number of patients seeking treatment for diabetic foot ulcer. Some questions in the questionnaire may not be applicable in our local setting, such as the use of lukewarm water for washing feet, placing feet near fire or use of seamless socks, which are not usually available or in fashion here in our country. Our tropical weather is markedly different from area where the Nottingham foot care questionnaire was developed. Our respondents preferred the use of flip-flops and slippers and were unaccustomed to use of socks or tights. Appropriately revised knowledge and practice questionnaires should be developed to make these applicable to Filipino patients. The revised versions of the questionnaires may be used in future studies. We also did not document foot deformities, neuropathy and peripheral arterial disease. Information on current and past history of foot problems only came from questionnaires, unverified from patient records. For future studies, knowledge and practice scores in patients at highrisk for diabetic foot ulcers may also be compared.
CONCLUSION
The current state of foot care knowledge in Filipino diabetic respondents is good, but the level of foot self-care practice is only satisfactory. Healthcare providers should focus on addressing gaps in foot care knowledge, supporting proper foot care practices and encouraging patients to participate in educational activities on diabetes.
Acknowledgments
The authors thank the Section of Endocrinology, Diabetes, and Metabolism of the Chinese General Hospital and Medical Center for its continued support for this research.
Appendix 1. Questionnaire on Knowledge of Foot Care (English version)10
| Place a check (✓) in the appropriate column to indicate whether the statement is CORRECT or WRONG | Correct | Wrong | I do not know | |
|---|---|---|---|---|
| 1 | Anti-diabetic medications should be taken regularly to prevent complications. | |||
| 2 | Feet should be washed daily. | |||
| 3 | Lukewarm water should be used to wash feet. | |||
| 4 | The temperature of the water should be checked before washing feet. | |||
| 5 | Feet should be completely dried after washing. | |||
| 6 | Talcum powder should be used to keep the areas between the toes dry. | |||
| 7 | Lotion or moisturizing cream should be applied on the feet to prevent dryness of skin. | |||
| 8 | Lotion should not be applied between the toes. | |||
| 9 | Socks should be changed daily. | |||
| 10 | Toenails should be trimmed straight across. | |||
| 11 | Feet should be inspected at least once a day. | |||
| 12 | Diabetic patients should wear comfortable shoes. | |||
| 13 | The inside of the shoes should be inspected for before wearing them. | |||
| 14 | Diabetic patients should not walk barefoot. | |||
| 15 | Diabetic patients should consult a doctor if their feet have redness, blisters, cuts, or wound/s. | |||
Appendix 2. Nottingham Assessment of Functional Foot Care (English Version)11
Footnotes
*Presented during the PRIDE session of the 2017 Philippine Society of Endocrinology, Diabetes and Metabolism Annual Convention on March 23, 2017 at the EDSA Shangri-La Hotel, Mandaluyong, Philippines
Statement of Authorship
The authors certified fulfillment of ICMJE authorship criteria.
Author Disclosure
The authors declared no conflict of interest.
Funding Source
None.
Authors are required to accomplish, sign and submit scanned copies of the JAFES Author Form consisting of: (1) Authorship Certification, that all the requirements for authorship have been met by each author, and that the final version of the manuscript has been read and approved by all authors; (2) the Author Declaration, that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere; (3) the Statement of Copyright Transfer [accepted manuscripts become the permanent property of the JAFES and are licensed with an Attribution-Share Alike-Non-Commercial Creative Commons License. Articles may be shared and adapted for non-commercial purposes as long as they are properly cited]; and the ICMJE form for Disclosure of Potential Conflicts of Interest. For original articles, authors are required to submit a scanned copy of the Ethics Review Approval of their research as well as registration in trial registries as appropriate. For manuscripts reporting data from studies involving animals, authors are required to submit a scanned copy of the Institutional Animal Care and Use Committee approval. For Case Reports or Series, and Images in Endocrinology, consent forms, are required for the publication of information about patients; otherwise, authors declared that all means have been exhausted for securing such consent. Articles and any other material published in the JAFES represent the work of the author(s) and should not be construed to reflect the opinions of the Editors or the Publisher.
References
- 1.Abbott CA, Carrington AL, Ashe H, et al. The North-West Diabetes Foot Care Study: incidence of, and risk factors for, new diabetic foot ulceration in a community-based patient cohort. Diabetic Med. 2002;19(5):377-84. PMID: https://doi:10.1046/j.1464-5491.2002.00698.x [DOI] [PubMed] [Google Scholar]
- 2.Ramsey SD , Newton K, Blough D, et al. Incidence, outcomes, and cost of foot ulcers in patients with diabetes. Diabetes Care. 1999;22(3):382-7. PMID: 10.2337/diacare.22.3.382 [DOI] [PubMed] [Google Scholar]
- 3.Boulton AJ, Armstrong DG, Albert SF, et al. Comprehensive foot examination and risk assessment: A report of the task force of the foot care interest group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Diabetes Care. 2008;31(8):1679-85. PMID: PMCID: 10.2337/dc08-9021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with Diabetes. JAMA. 2005;293(2):217-28. PMID: 10.1001/jama.293.2.217 [DOI] [PubMed] [Google Scholar]
- 5.Chandalia HB, Singh D, Kapoor V, Chandalia SH, Lamba PS. Footwear and foot care knowledge as risk factors for foot problems in Indian diabetics. Int J Diabetes Dev Ctries. 2008;28(4):109-13. PMID: PMCID: 10.4103/0973-3930.45269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mayfield JA, Reiber GE, Sanders LJ, Janisse D, Poqach LM; AmericanDiabetes Association Preventive foot care in diabetes. Diabetes Care. 2004;27(Suppl 1):S63-4. PMID: . [DOI] [PubMed] [Google Scholar]
- 7.Pinzur MS, Slovenkai MP, Trepman E, Shields NN; Diabetes Committee of American Orthopaedic Foot and Ankle Society Guidelines for diabetic foot care: recommendations endorsed by the Diabetes Committee of the American Orthopaedic Foot and Ankle Society. Foot Ankle Int. 2005;26(1):113-9. PMID: 10.1177/107110070502600112. [DOI] [PubMed] [Google Scholar]
- 8.Bonner T, Foster M, Spears-Lanoix E. Type 2 diabetes-related foot care knowledge and foot self-care practice interventions in the United States: A systematic review of the literature. Diabet Foot Ankle. 2016;7:29758. PMID: PMCID: https://doi.org/10.3402/dfa.v7.29758.eCollection 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matricciani L, Jones S. Who cares about foot care? Barriers and enablers of foot self-care practices among non-institutionalized older adults diagnosed with diabetes: An integrative review. Diabetes Educ. 2015;41(1):106-17. PMID: 10.1177/0145721714560441. [DOI] [PubMed] [Google Scholar]
- 10.Hasnain S, Sheikh NH. Knowledge and practices regarding foot care in diabetic patients visiting diabetic clinic in Jinnah Hospital, Lahore. J Pak Med Assoc. 2009;59(10):687-90. PMID: . [PubMed] [Google Scholar]
- 11.Lincoln NB, Jeffcoate WJ, Ince P, Smith M, Radford K. Validation of a new measure of protective footcare behaviour: The Nottingham Assessment of Functional Footcare (NAFF). Pract Diab Int. 2007;24(4):207-11. 10.1002/pdi.1099. [DOI] [Google Scholar]
- 12.Polit DF, Yang FM. Measurement and the measurement of change. Philadelphia: Wolters Kluwer, 2016. [Google Scholar]
- 13.UNITE for Diabetes Philippines: Philippine Practice Guidelines on the Diagnosis and Management of Diabetes Mellitus. http://obesity.org.ph/v4/wp-content/uploads/2014/07/Diabetes-United-for-Diabetes-Phil.pdf. Accessed August 1, 2016. [Google Scholar]
- 14.Philippine Statistics Authority 2012 Family Income and Expenditure Survey Final Results: National Capital Region. Number: 2014-11. http://nso-ncr.ph/special%20release/fies/2012%20Fies.pdf. Accessed August 6, 2016. [Google Scholar]
- 15.Muhammad-Lutfi AR, Zaraihah MR, Anuar-Ramdhan IM. Knowledge and practice of diabetic foot care in an in-patient setting at a tertiary medical center. Malays Orthop J. 2014;8(3):22-6. PMCID: 10.5704/MOJ.1411.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seid A, Tsige Y. Knowledge, practice, and barriers of foot care among diabetic patients attending Felege Hiwot Referral Hospital, Bahir Dar, Northwest Ethiopia. Advances in Nursing. 2015;2015:Article ID 934623. 10.1155/2015/934623 [DOI] [Google Scholar]
- 17.Desalu OO, Salawu FK, Jimoh AK, Adekoya AO, Busari OA, Olokoba AB. Diabetic Foot Care: self-reported knowledge and practice among patients attending three tertiary hospital in Nigeria. Ghana Med J. 2011;45(2):60-5. PMID: PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mcmillan G, Hanson TE. Sample size requirements for establishing clinical test-retest standards. Ear Hear. 2014;35(2): 283-6. PMID: 10.1097/01.aud.0000438377.150036b. [DOI] [PubMed] [Google Scholar]
- 19.Peacock J, Peacock PJ. Oxford handbook of medical statistics. Oxford: Oxford University Press, 2011. [Google Scholar]
- 20.George H, Rakesh P, Krishna M, et al. Foot care knowledge and practices and the prevalence of peripheral neuropathy among people with diabetes attending a secondary care rural hospital in southern India. J Family Med Prim Care. 2013;2(1):27-32. PMID: PMCID: 10.4103/2249-4863.109938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li R, Yuan L, Guo KH, et al. The current status of foot self-care knowledge, behaviours, and analysis of influencing factors in patients with type 2 diabetes mellitus in China. International Journal of Nursing Sciences. 2014; 1(3):266-71. 10.1016/j.ijnss.2014.05.023. [DOI] [Google Scholar]
- 22.Isip J, de Guzman M, Ebison A Jr, Narvacan-Montano C. Footwear appropriateness, preferences and foot ulcer risk among adult diabetics at Makati Medical Center Outpatient Department. J ASEAN Fed Endocr Soc. 2016;31(1):37-43. 10.15605/jafes.031.01.07. [DOI] [Google Scholar]
- 23.Kumhar M, Dara N, Saini T. Foot wear and footcare knowledge—an independent risk factor for diabetic foot in Indian diabetics. Indian Medical Gazette. 2014;25-8. http://imsear.hellis.org/handle/123456789/157578. [Google Scholar]
- 24.Khamseh ME, Vatankhah N, Baradaran HR. Knowledge and practice of foot care in Iranian people with type 2 diabetes. Int Wound J. 2007;4(4):298-302. PMID: 10.1111/j.1742-481X.2007.00381.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hernandez-Tejada MA, Campbell JA, Walker RJ, Smalls BL, Davis KS, Egede LE. Diabetes empowerment, medication adherence and self-care behaviors in adults with type 2 diabetes. Diabetes Technol Ther. 2012;14(7):630-4. PMID: PMCID: 10.1089/dia.2011.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim SY, Hongsranagon P. Preventive behaviors regarding foot ulcers in diabetes type II patients at BMA Health Center No. 48, Bangkok, Thailand. J Health Res. 2008;22(Suppl):21-8. http://www.jhealthres.org/upload/journal/341/22(suppl)_p21-28_sonyongkim.pdf. [Google Scholar]
- 27.Malathy R, Narmadha M, Ramesh S, Alvin JM, Dinesh BN. Effect of a diabetes counseling programme on knowledge, attitude and practice among diabetic patients in Erode district of South India. J Young Pharm. 2011;3(1):65-72. PMID: PMCID: 10.4103/0975-1483.76422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nongmaithem M, Bawa AP, Pithwa AK, Bhatia SK, Singh G, Gooptu S. A study of risk factors and foot care behavior among diabetics. J Family Med Prim Care. 2016;5(2):399-403. PMID: . PMCID: 10.4103/2249-4863.192340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nagpal J, Bhartia A. Quality of diabetes care in the middle- and highincome group populace: The Delhi Diabetes Community (DEDICOM) Survey. Diabetes Care. 2006;29(11):2341-8. PMID: 10.2337/dc06-0783. [DOI] [PubMed] [Google Scholar]