Abstract
Objective
The study aims to determine the association of diabetes-related emotional distress with reported diabetes self-care, and glycemic control of adult Filipinos with type 2 diabetes mellitus at The Medical City using 2 psychometric tests.
Methodology
This is a cross-sectional study conducted among 94 Filipinos diagnosed with type 2 diabetes mellitus, who answered 2 validated English questionnaires: Problem areas in diabetes (PAID-20) and Diabetes self-management questionnaire (DSMQ) that screen for diabetes-related emotional distress and diabetes reported self-care, respectively. Data were encoded and analyzed using Stata SE v.13.
Results
42.6% of Filipinos with type 2 diabetes mellitus had emotional distress showing moderate to severe distress in factor 1 (diabetes-related emotional distress) and factor 3 (food related problems). 51.1% had suboptimal self-care, poorly scoring in areas of health-care use and dietary control. Majority of those who had diabetes-related distress and poor self-care where young, pre-obese and had diabetes duration of ±5 years. There was no significant association between diabetes-related emotional distress with diabetes self-care and emotional distress with glycated hemoglobin, but majority of those who had diabetes distress had higher glycated hemoglobin. There was significant association between diabetes self-care and glycemic outcomes (p=0.006) with relative risk of 1.51 (95% CI 1.10-2.07). There was linear inverse weak correlation between all subdomains of DSMQ with glycated hemoglobin except Dietary Control.
Conclusion
Diabetes-related emotional distress and sub-optimal self-care are prevalent among Filipinos with type 2 diabetes mellitus. Those who had poor self-care were 1.5 times more likely to have poor glycemic outcomes.
Keywords: emotional distress, Filipino, self-care, diabetes self-management questionnaire
INTRODUCTION
The global burden of diabetes mellitus is looming. It is estimated by the World Health Organization in 2016 that 422 million adults are living with the disease.1 Locally, according to the National Nutrition and Health Survey of 2008, one out of every 5 adult Filipinos could potentially have diabetes mellitus or prediabetes.2 The care of persons with diabetes is lifelong owing to the chronicity of the disease. It involves more than simple adherence to pharmacotherapy but should be patient-centered care, defined as respectful of, and responsive to individual patient preferences, needs and values. It ensures that patient values guide all clinical decisions.3
A person with diabetes will require integration of the long-term treatment regimen as well as coping with the fear of the occurrence of diabetic complications. This psychological burden can have a significant impact on many aspects of the quality of life-affecting work, interpersonal relationships, social functioning, physical and emotional well-being.4 It is well studied that psychological burden can lead to emotional distress and negatively impact a person’s motivational behavior over the course of the illness. The psychological aspect of diabetes mellitus however, is often a neglected component in the diabetes care despite the fact that having the disease itself is a risk factor for developing decreased psychological well-being.5
Diabetes-related emotional distress or diabetes distress is a unique entity arising from the disease manifesting as a hidden emotional burden or worry. It is often significantly associated with low diabetes self-efficacy and poor quality of life even after management for clinical depression.6 A number of studies have also shown that patients with diabetes who have high levels of depressive affects do not necessarily fulfill the criteria for clinical depression. Moreover, there is a significant association between diabetes-related emotional distress with diabetes-related behavior and biologic variables than major depressive disorder or depressive state.7
In 2015, the Diabetes Center of The Medical City in its aim to provide a more patient-centered care launched the Lifestyle Assessment and Management Program (LAMP) in partnership with the Psychiatry Department. This program screens for diabetes-related emotional distress, depression, anxiety, as well as diabetes self-management of patients using validated self-administered English questionnaires. The results of the psychometric tests are interpreted and a session with a psychiatrist for life coaching is made. Screening for diabetes-related distress and self-reported diabetes care are crucial not only for assessment of psychological issues but because they may have an impact on clinical parameters such as glycemic control and disease-related complications. Numerous studies have looked into the significant association of diabetes-related emotional distress and self-care with glycemic control, but none were done locally using the aforementioned questionnaires.
The general objective of this study is to determine the association between diabetes-related emotional distress with overall quality of diabetes self-care and glycemic control of adult Filipinos with Type 2 Diabetes Mellitus at The Medical City. The specific objectives are: (1) to determine the prevalence of diabetes-related emotional distress using the Problem Areas in Diabetes Questionnaires-20 and the prevalence of self-reported overall quality of diabetes reported self-care using Diabetes Self-Management Questionnaires (DSMQ); (2) to determine the association between diabetes-related emotional distress with diabetes reported overall quality of self-care; (3) to determine association between diabetes-related emotional distress and glycemic control; and (4) to determine the association between diabetes reported overall quality of self-care and glycemic control.
METHODOLOGY
The Instruments: PAID-20 and DSMQ
Various questionnaires have been developed and validated to aid clinicians in identifying patients who may be experiencing diabetes-related emotional distress and for assessing diabetes self-management care including Problem Areas in Diabetes-20 (PAID) which is the most widely used, and Diabetes Self-Management Questionnaire (DSMQ) which is the preferred.
The PAID scale is an English self-report 20-item measure of emotional adjustment to life with diabetes developed by Polonsky et al., in 1995.8 Each item represents a unique area of diabetes-related psychosocial distress, and the degree is reported using a six-point Likert scale. It could be used for insulin dependent and non-insulin dependent diabetes mellitus patients.4 In comparing various diabetes-related emotional distress instruments, one meta-analysis has shown that the Problem Areas in Diabetes-20 (PAID) is the best validated, widely used and recommended among the other instruments.9 Furthermore, PAID-20 was also the same questionnaire utilized in the DAWN study to screen for diabetes-related emotional distress.10
The self-management of diabetes involves multiple domains of care including compliance to pharmacotherapy, health care visits and lifestyle modifications. The DSMQ was introduced by Schmitt et al., in 2013.11 This an English self-report scale comprising of 16 items which focuses on four domain, namely (1) glucose management; (2) dietary control; (3) physical activity; and (4) health-care use. It recalls the previous 8 weeks of self-care and includes both positively and negatively formulated questions structured in alternating manner, and a four-point Likert scale was used to report the magnitude. The instrument was useful for evaluating problematic behaviors of patients with both type 1 and type 2 diabetes and has been shown to have very good psychometric properties in terms of item characteristics, reliability and validity.11 In addition, this scale has been evaluated to be the preferred tool when analyzing self-reported behavioral problems in relation to control of blood sugar of patients with diabetes in Caucasian populations.12
Questionnaire interpretation
PAID: Each item has 5 possible answers using the Likert scale with values from 0 to 4 with 0 representing “no problem” and 4 representing “a serious problem.” The scores were added up and multiplied by 1.25, generating a total score between 0-100. Patients scoring 40 or higher may be at the level of “emotional burnout” and warrant special attention. An extremely low PAID-20 score (0-10) combined with poor glycemic control may be indicative of denial.4 In the original study on the utilization of PAID- 20, the multiple subdomains of the questionnaire was not explored and was only interpreted as one factor,8 however on multiple studies using the questionnaire in different races, some investigators proposed either a 1-to-4 factor domain in the analysis of PAID-20 with Snoek et al.,13 proposing a four-factor subscale (Table 1) that includes: (1) diabetes-related emotional problems; (2) treatmentrelated problems; (3) food-related problems; and (4) social support-related problems.14 To date however, no consensus has yet been formulated regarding which factor tool structure should be uniformly used in its interpretation.15 Nevertheless, in the clinical interpretation of the PAID-20, it is recommended that clinicians aside from computing the raw score, should take note of the specific areas where the patients scored 3 to 4 in the Likert scale corresponding to having moderate to severe distress, and using these items as a take-off point in the discussion during consultation.16
Table 1.
Scoring and subset scales of PAID*
| Sub scales | |
|---|---|
| Diabetes-related Emotional Distress (Items 3, 6, 7, 8,9, 10, 12, 13, 14, 16, 19, 20) | |
| Treatment-related Problems (Items 1, 2,15) | |
| Food-related Problems (Items 4, 5,11) | |
| Social support-related Problems (Items 17,18) | |
| Sum scale | (Raw score x 1.25) |
| Score (Highest score: 100) | |
Proposed by Snoek et al.13
DSMQ: Each item has 4 possible answers using the Likert scale with value from 0 to 3 with 0 representing “does not apply to me” and 3 representing “applies to me very much”. Seven of 16 items were formulated positively and 9 were inversely stated with regard to what is considered effective self-care. Scoring of the questionnaires involved reversing the negatively structured questions such that the higher values are indicative of more effective self-care and they include items 5, 7, 10, 11, 12, 13, 14, and 15. Scale scores were calculated as sums of item scores and then transformed to a scale ranging from 0 to 10 [(raw score/theoretical maximum score) x 10] (Table 2). A transformed score of 10 thus represented the highest self-rating of the assessed behavior. If “not required as part of my treatment” had been marked in an item, it means that it was not used and the scale score computation should be adapted accordingly by reducing the theoretical maximum score by 3 points.17
Table 2.
Scoring and subset scales of DSMQ
| Sub scales | |
|---|---|
| Glucose Management (Sum of items 1, 4, 6, 10 and 12) | (Raw score /15) x 10 |
| Dietary Control (Sum of items 2, 5, 9 and 13) | (Raw score/ 12) x 10 |
| Physical Activity (Sum of items 8, 11, and 15) | (Raw score/ 9) x 10 |
| Health-Care use (Sum of items 3, 7, and 14) | (Raw score /9) x 10 |
| Sum scale | (Raw score/ 48) x 10 |
| Score (Highest score: 10) | |
A cut off score of ≤6.0 is indicative of suboptimal selfcare as proposed by Schmitt using German populations while no cut off score was suggested on the individual subscale domains.17
Study design
This is a cross-sectional study done at The Medical City approved by Institutional Review Board and participated by adult Filipinos with Type 2 diabetes mellitus from June 2017 to November 2017. The original authors of PAID-20 and DSMQ expressed their consent to the use of their questionnaires and gave recommendations as to its proper interpretation. Consent forms were first handed and thoroughly explained to each participant including data privacy and the limitation of the study not to include psychiatric consultations. Once they agreed, they were given 2 sets of English validated questionnaires of PAID-20 and DSMQ and they were asked to answer it in 5-15 minutes. Questionnaires were tabulated and interpreted on the same day and patients who had emotional distress or suboptimal self-care, were individually contacted and advised to return to the Diabetes Center for scheduling of initial life coaching with a psychiatrist of choice and to continue consult as advised. Their attending endocrinologists were likewise notified of the results for proper coordination and follow-up.
Glycated hemoglobin was done at The Medical City using high performance liquid chromatography (HPLC) using Bio-RAD D-10 HbA1c with NGSP certification until January 1, 2019. Results were viewed and collected using the Laboratory Information System (LIS) of the Hospital. The Average time lapse from the actual administration of the questionnaires and glycated hemoglobin was 6.6±11 days.
Sample population
A total of 94 health-care diagnosed adult Filipinos with type 2 diabetes mellitus were enrolled in the study. They were either seen at the Diabetes Center, at the clinic of endocrinologists or admitted in the hospital.
Sample size
Using NCSS-PASS 2013, the minimum sample size requirement is at least 84 patients based on the correlation between emotional distress and glycemic control =0.30>6 with alpha level =5% and power =80%. Inclusion criteria: (1) 18 years old and above, (2) type 2 diabetes mellitus diagnosed by health care provider, (3) with HbA1C done within 3 months at The Medical City. Exclusion criteria: (1) the participant was unable to read or understand English, (2) no HbA1C results or results done outside The Medical City, and (3) recent history of blood loss, or blood transfusion.
Analysis
Descriptive statistics were used to summarize the characteristics of the population. Frequency and proportion were used for nominal variables, mean and standard deviation were used for quantitative variables.
Independent T-test was used to compare the means for age, body mass index, diabetes duration, subset scores in PAID-20 and DSMQ and glycated hemoglobin, while Pearson’s Chi-square was used to compare gender, and type of anti-diabetes medications as well as the association between diabetes related emotional distress with glycated hemoglobin; self-care with glycated hemoglobin and emotional distress with self-care while relative risk was used to ascertain the likelihood of the association. Pearson’s correlation coefficient was used to determine the linear correlation of the subset domains of DSMQ and glycated hemoglobin. All tests were performed using Stata SE version 13 and set at 0.5% level of significance.
RESULTS
General characteristics
A total of 94 adult Filipinos with type 2 diabetes mellitus were analyzed in the study. The overall demographic profile was summarized in Table 3. The mean age was 54.03±11.45 years with majority belonging to the pre-obese category using the Asia-Pacific cut-off. Most of these patients were married and finished college and were currently employed. They had diabetes for 5.6±4.9 years, mostly maintained on oral anti-diabetic medications and had a mean glycated hemoglobin of 8.37±2.16% with 66% uncontrolled.
Table 3.
Sociodemographic and clinical characteristics of the study population
| Characteristics (N=94) | Mean±SD or n (%) |
|---|---|
| Age (years) | 54.0±11.5 |
|
Gender Male Female |
45 (47.9) 49 (52.1) |
| BMI (kg/m2) | 28.1±5.3 |
|
Marital Status Single Married Separated/Divorced Widowed |
20 (21.3) 66 (70.2) 3 (3.2) 5 (5.3) |
|
Educational Attainment Elementary High school College Post Graduate Vocational |
4 (4.3) 8 (8.5) 68 (72.3) 12 (12.8) 2 (2.1) |
|
Employment Employed Self-employed Unemployed Retired |
43 (45.7) 18 (19.2) 13 (13.8) 20 (21.3) |
| Diabetes Duration (years) | 5.6±4.9 |
|
Anti-diabetic Medications Oral only Insulin only Combination of both |
64 (68.1) 8 (8.5) 22 (23.4) |
|
PAID Scores Without Distress (<40) With Distress (≥40) In denial (<10 with HbA1c ≥7%) |
32.2±20.6 40 (42.6) 47 (50) 7 (7.5) |
|
DSMQ Scores Suboptimal self-care (<6) Optimal self-care (≥6) |
6.5±1.4 48 (51.1) 46 (48.9) |
|
HbA1C (%) Good glycemic control (<7%) Poor glycemic control (≥7%) |
8.4±2.2 32 (34) 62 (66) |
Diabetes-related emotional distress
The mean PAID score of 94 adult Filipinos with diabetes was 32.18±20.51(Table 3). The prevalence of diabetes-related emotional distress was 42.6% with PAID-20 mean scores of 52.75±10.26 (cut-off of >40) (Table 5). Only 7 patients were classified under “in denial” category (e.g. PAID-20 <10 with glycated hemoglobin ≥7%), with majority of them males (71.4%), had a mean BMI of 31.7±7.7 kg/m2 with diabetes duration of 4±4.8 years. 62.5% of them were treated with oral anti-diabetic medications with an average glycated hemoglobin of 9.2±2.2%.
Table 5.
Summary of PAID scores and HbA1C results
| With Emotional Distress+ n=40 | Without Emotional Distress+ n=47 | p value | |
|---|---|---|---|
| Age | 49.6±10.0 | 57.8±11.2 | <0.001* |
|
Gender Male Female |
18 (45%) 22 (55%) |
22 (46.8%) 25 (53.2%) |
0.866 |
| BMI | 27.9±4.8 | 27.8±5.2 | 0.922 |
| Diabetes Duration (years) | 5.6±5.2 | 5.9±4.7 | 0.815 |
|
Anti-diabetic medications Oral Insulin Combination |
26 (29.9%) 3 (3.5%) 11 (12.6%) |
33 (37.9%) 5 (5.7%) 9 (10.3%) |
0.615 |
|
PAID Scores Sum Score Factor 1 (Diabetes-related emotional distress)‡ Factor 2 (Treatment related problems)‡ Factor 3 (Food related problems)‡ Factor 4 (Social support related problems)‡ |
52.8±10.3 2.4±1.0 1.7 ±1.3 2.5 ±0.8 1.2 ±0.8 |
18.8±9.6 0.8±0.8 0.5±0.9 0.9±0.8 0.3±0.3 |
<0.001* <0.001* <0.001* <0.001* <0.001* |
| HbA1C (%) | 9.0±2.5 | 7.7±1.7 | 0.004* |
|
Glycemic Control Good Glycemic Control (<7%) Poor Glycemic Control (≥7%) |
12 (13.8%) 28 (32.2%) |
20 (23%) 27 (31%) |
0.226 |
Data presented in Mean±SD or n (%)
proposed by Snoek et al.13
Statistically significant at 5% level
Patients who had emotional distress had a cut-off score of ≥40 and showed moderate to severe distress (Likert scale of 3-4) in 16 out of the 20 specific item questions (Table 4). On the other hand, patients who had no emotional distress or who were in denial did not show any moderate or severe distress in any specific item in the questionnaire. Using the 4 subscale factors proposed by Snoek at el13, all four factors were significantly different between those with emotional distress and those without. Moreover, in those that had emotional distress, the factors that scored the highest were in factor 1, diabetes-related emotional distress and factor 3, food-related problems (Table 5).
Table 4.
Specific items in the PAID-20 questionnaire and their mean scores
| Item No. | Abbreviated item content | Percentage ofMissing Values | With Emotional Distress+ (n=40) | Without Emotional Distress+ (n=47) | In Denial+ (n=7) |
|---|---|---|---|---|---|
| 1 | Concrete goals | 1.1 | 2.3±1.1* | 0.9±1.1 | 0.3±0.5 |
| 2 | Discouraged | 0 | 2.1±0.9* | 0.6±0.9 | 0 |
| 3 | Scared | 0 | 3.0±0.8* | 0.8±0.9 | 0.7±1.5 |
| 4 | Social Situations | 0 | 2.5±0.9* | 1.0±0.9 | 0.1±0.4 |
| 5 | Deprivation | 0 | 2.6±0.8* | 0.7±0.7 | 0 |
| 6 | Depressed | 0 | 2.6±0.8* | 1.0±0.8 | 0 |
| 7 | Indistinguishable mood | 0 | 2.6±0.8* | 0.9±1.0 | 0.4±0.5 |
| 8 | Overwhelmed | 0 | 2.1±0.9* | 0.9±1.0 | 0 |
| 9 | Reactions | 0 | 2.5±0.9* | 0.9±0.8 | 0.1±0.4 |
| 10 | Angry | 0 | 2.2±0.8* | 0.4±0.6 | 0.3±0.5 |
| 11 | Concerned | 0 | 2.5±0.9* | 1.0±0.9 | 0.1±0.4 |
| 12 | Worry about the future | 0 | 3.3±0.6* | 1.5±1.2 | 0.4±0.5 |
| 13 | Guilty | 0 | 2.4±1.1* | 1.3±0.8 | 0 |
| 14 | Accepting | 0 | 2.0±1.4* | 0.6±0.9 | 0 |
| 15 | Unsatisfied | 1.1 | 0.7±0.7 | 0.2±0.5 | 0 |
| 16 | Energy | 0 | 2.2±0.8* | 0.4±0.6 | 0 |
| 17 | Alone | 0 | 1.4±0.9 | 0.2±0.5 | 0 |
| 18 | Supportive | 0 | 0.9±0.8 | 0.4±0.7 | 0 |
| 19 | Coping | 0 | 1.8±1.0 | 0.9±1.0 | 0 |
| 20 | Burned out | 0 | 2.1±1.0* | 0.7±0.7 | 0 |
Data presented in Mean±SD
Mean Scores ≥3
When gender, body mass index, diabetes duration and type of anti-diabetic medications were compared between those with emotional distress and those without, no significant differences were seen (Table 5). In terms of age however, majority of those who had emotional distress were younger (p=<0.001) with a mean age of 49.6±10.0 years and their glycated hemoglobin was significantly lower (p=0.004) although still above the <7% cut-off for optimal control. No statistically significant association was noted between the presence of emotional distress and glycemic control (Table 5).
Diabetes reported self-care
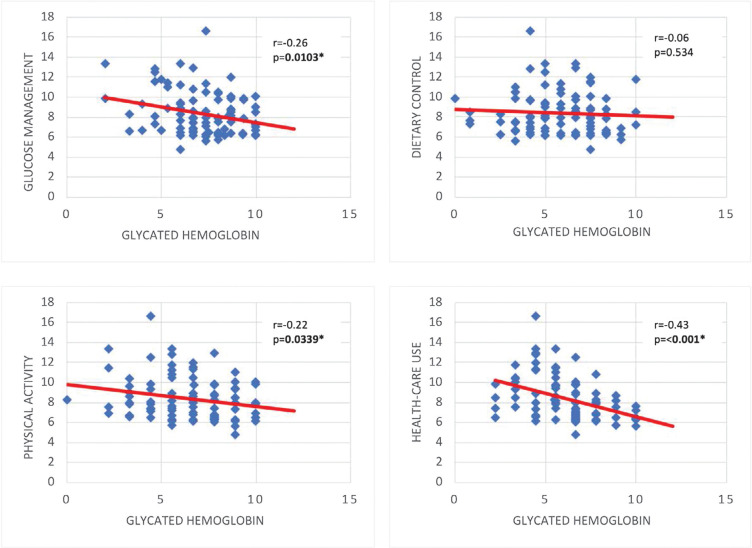
The mean DSMQ scores of the sample was 6.46±1.44 (Table 3). The prevalence of suboptimal reported self-care (cut-off score of ≤6) was noted at 51.1% (Table 6) and these patients had a mean age of 50.1±10.86 years and were younger compared to those who had good self-care (p=<0.001). Body Mass Index, duration of diabetes and types of anti-diabetic medications were comparable between the two groups and did not show any statistical difference (Table 6). Comparing the glycated hemoglobin between the two groups, there was a significant difference (p=0.001) between those in the suboptimal and optimal self-care with the latter having lower glycated hemoglobin albeit still not within the ideal glycemic target of <7%. All the scores in the subset domains were statistically different from the two groups (Table 6) with majority of patients in the suboptimal group scoring poorly in Dietary Control followed by Health-Care Use. In comparison, those who had optimal self-care scored highest in areas of Glucose Management followed by Dietary Control (Table 4). Furthermore, there was a statistically significant association between the quality of self-care and glycemic outcomes (p=0.006) (Table 6) with a relative risk of 1.51 (95% CI 1.10-2.07). In terms of the subdomains of DSMQ, only Dietary Control showed no significant linear correlation with glycated hemoglobin, while others showed a weak, inverse linear correlation (Figure 1).
Table 6.
Summary of DSMQ scores and HbA1C results
| Sub-optimal self-care+ n=48 | Optimal self-care+ n=46 | p value | |
|---|---|---|---|
| Age | 50.1±11.3 | 58.1±10.1 | <0.001* |
|
Gender Male Female |
19 (39.6%) 26 (54.2%) |
29 (63%) 20 (43.5) |
0.1507 |
| BMI | 28.1±4.3 | 28.2±6.2 | 0.921 |
| Diabetes Duration (years) | 6.2±5.3 | 5.1±4.5 | 0.310 |
|
Anti-diabetic medications Oral Insulin Combination |
33 (68.8%) 3 (6.3%) 12 (25%) |
31 (67.4%) 5 (10.9%) 10 (21.7%) |
0.704 |
|
DSMQ scores Sum Score Sub-scale scores Glucose Management Dietary Control Physical Activity Health Care Use |
5.31±0.9 6.2±1.7 4.5±1.8 5.5±2.1 5.3±1.6 |
7.80±1.8 8.2±1.3 7.6±1.8 7.5±1.8 7.1±1.9 |
<0.001* <0.001* <0.001* <0.001* <0.001* |
| HbA1C (%) | 9.1±2.3 | 7.6±1.7 | 0.001* |
|
Glycemic Control Good Glycemic Control (<7%) Poor Glycemic Control (≥7%) |
10 (10.6%) 38 (40.4%) |
22 (23.4%) 24 (25.5%) |
0.006* |
Data presented in Mean±SD or n (%)
Statistically significant at 5% level
Figure 1.
Linear correlation of DSMQ subdomains with glycated hemoglobin.
Diabetes-related emotional distress and diabetes reported self-care
The presence of emotional distress did not show significant association with the quality of reported diabetes self-care (Table 7).
Table 7.
Cross tabulation (PAID and DSMQ)
| PAID outcomes | DSMQ outcomes | p value | |
|---|---|---|---|
| Sub-optimal Self Care+ | Optimal Self-Care+ | ||
| Without Emotional Distress With Emotional Distress |
31% 32.2% |
23% 13.8% |
|
| 0.226 | |||
+ Data presented in n (%)
Emotional distress as measured by the PAID questionnaire was not significantly associated with the quality of reported diabetes self-care.
DISCUSSION
More than a quarter of patients in this study reported diabetes-related emotional distress. This high prevalence of diabetes-emotional distress (42.6%) was similar to that seen in the DAWN2 study (44.6%), which included 17 countries with China and Japan as the only two Asian countries.18 Compared to the DAWN1 study, the prevalence of diabetes-related emotional distress in the DAWN2 study doubled. Interestingly, the DAWN1 study also reported a high prevalence of emotional distress (85.2%), but this was commonly observed in newly diagnosed patients with diabetes.19
In the PAID-20 subscale domains proposed by Snoek et al.,13 Filipinos with type 2 diabetes mellitus seem to manifest a great deal of distress in factor 1 that is specific to diabetes-related emotional distress and comprised of 12 items, followed by factor 3 that deals with food-related problems and has 3 items. In fact, in the individual questions, the items that scored the highest were those that tackled the feeling of being scared about living with the disease and worrying about its possible complications. Taking into account that majority of the persons enrolled in this study have diabetes in a 5-year period, it is understandable that many show distress in terms of how such a condition will affect their lives. This finding is also similar to the study involving Koreans with type 2 diabetes where majority had a mean age of 58.02±10.88 years old, diabetes duration of 10 years and on combination regimen with insulin. The study reported moderate to severe distress in the item concerning diabetic complications.15
In the study done by Lee et al.,15 as described above, and the original study of Snoek et al.,13 that looked into Dutch and Americans aged 51±16 years with diabetes duration of 16±12 years, a high incidence of insulin use, whether alone or in combination with an oral anti-diabetic medication was found. In our study however, only 32% of the subjects were on insulin, the rest were solely on oral anti-diabetic medications (68%). This mirrors the findings of Jimeno et al.,20 in their survey about the glycemic control and status of diabetes care and complications of Filipinos with type 2 diabetes mellitus, where 78.5% of the population were treated exclusively with oral anti-diabetic medications. It may be speculated that unlike those seen in other countries, the distress brought about by using insulin may not be the sole reason why it is infrequently used in the local setting considering that while most of the subjects reported distress, majority of them did not use insulin at all. On the other hand, the possible distress brought about by insulin use cannot be eliminated especially for those participants who reported distress. However, since no focus group discussion was done, the matter was not investigated thoroughly.
As noted earlier, the results of this study share the same moderate to severe distress in factors 1 and 3 of the sub-analysis proposed by Snoek et al.13 One key difference in this study however is that the items for factor 3 individually scored moderate to severe distress. This may support the colloquial knowledge that Filipinos are passionate eaters and being diagnosed with diabetes where the cornerstone of management entails careful selection and proper control of food intake, will presumably cause distress. The results of these studies support the conclusion that having diabetes may lead to significant physical and psychological burden. However, cultural background continues to influence certain aspects of diabetes distress.
This study did not show significant association between the presence of diabetes-related emotional distress and poor glycemic outcomes. This finding is contrary to the first study conducted at Joslin Diabetes Center Clinic on the assessment of PAID-20 where greater distress was significantly associated with poorer glycemic outcomes with PAID-20 having a predictive glycemic outcome control of up to 12 months.8 The results of the study done by Stranderg et al., in 201421 on Norwegians with type 1 diabetes mellitus similarly showed no significant linear relationship between diabetes-related emotional distress and glycated hemoglobin but after 1 year of follow-up, showed significant correlation.22 In the meta-analysis on several instruments for assessment of diabetes-related emotional distress by Lee et al.,9 the generalized conclusion was a positive but weak pooled correlation between emotional distress and glycated hemoglobin. Although this study failed to show any significant association between the presence of diabetes-related emotional and poor glycemic outcomes, it is still noteworthy to point out that the average glycated hemoglobin of those with emotional distress and without, were statistically significant (p=0.004) with those with emotional distress having higher glycated hemoglobin. This difference in glycated hemoglobin although not reaching the optimal target of <7%, may still be clinically relevant because as pointed out in the landmark results of UKPDS, every percentage point decrease in glycated hemoglobin will have a 35% decrease in the overall risk of developing diabetes complications.23
There was no significant association between the presence of diabetes-related emotional distress and quality of diabetes reported self-care. This was in contrast to the study done by Ogbera and Adeyemi-doro24 on Nigerians with type 2 diabetes mellitus, where PAID-20 had a very weak correlation (r=0.21) with self-care using Self-Care inventory. The suggested reason is that diabetes distress impacts self-care in various levels, affecting multiple domains that ultimately results to poor selfcare in general.24 Patients who have emotional distress may feel powerless over their disease, and this feeling of powerlessness can significantly impact self-care behaviors.24 In this study, the effect of diabetes-related emotional distress on self-care may have been too weak to show any statistical significance.
Diabetes self-care or self-management includes activities like glucose monitoring, compliance to medications and diet prescription, regular health-care follow up and adherence to physical activities. All of these require adequate knowledge and motivation from the patient. In this study, 52.1% of Filipinos with type 2 diabetes who were young, pre-obese, and had diabetes duration of ±5 years, reported suboptimal self-care, scoring poorly in subset domains for Dietary Control and Health Care Use. These findings were similar to the self-care management behaviors reported in the DAWN1 study were patients who had poor self-care scored lower in area of diet.19 The probable reasons why younger Filipinos in this study reported poor self-care may be related to their lack of proper education with regards to the disease and their limited experience in their active role in its management. Moreover, there was a significant difference in the glycated hemoglobin of those who reported optimal self-care from those who did not (p=0.001). In the group that reported optimal self-care, it was observed that their mean glycated hemoglobin level was not the targeted optimal level of <7%, reaching an average of 7.63±1.70%. This discrepancy between the patient’s perceived and reported self-care behavior and unmet glycemic outcomes should alert physicians to be more vigilant with their advice to patient’s self-care behavior; scrutinize health-care practices in order to address deep-seated knowledge gaps and more importantly, provide motivation in the management of their illness. Factors such as coping behaviors to chronic illness that is influenced by ethnic and sociocultural variations should likewise be explored to explain the possible reasons behind this discrepancy. To date however, limited data have been published on the way Filipinos cope with debilitating diseases.
Optimal glycemic control requires an interplay of several factors including adherence to medications, dietary counseling, self-monitoring of blood glucose and education on diabetes.24 These factors were the very same domains that were evaluated using structured questions in the Diabetes Self-Management Questionnaires (DSMQ). In the initial correlation study done by the author of the DSMQ on both German patients with type 1 and type 2 diabetes, there was an inverse nearly moderate correlation between the two (p=<0.001; r=-0.46) and DSMQ was the better self-management questionnaire compared to others10. In another study that looked into the association of DSMQ with the presence of diabetes-related microvascular complications among Iranian patients with diabetes, DSMQ sum scale had a statistically significant association with neuropathy and a weak association with nephropathy.25 The results of our study showed significant association between diabetes reported selfcare and glycemic outcomes (p=0.006) with patients who have poor self-care 1.5 times likely to be uncontrolled. Although a self-care assessment questionnaire does not need to always correlate with glycemic outcome for it to be considered a valid psychometric instrument,11 DSMQ stands apart because it has consistently proven in various studies, including ours, to correlate with clinically measured endpoints like glycated hemoglobin.
In the individual subset domains of DSMQ, dietary control was one of the subset domains that scored poorly in persons that had suboptimal self-care and was the second highest for those who had good self-care (Table 6). It was however the sole factor that did not show linear relationship when correlated with glycated hemoglobin. Glucose management, physical activity and health-care used, all showed a negative inverse although weak correlation that reached statistical significance (Figure 1). In a study involving Pakistanis with type 2 diabetes mellitus, glucose management and dietary control subscales were the only factors that had linear correlation.26 This variation may be because of cultural differences.26
CONCLUSIONS AND RECOMMENDATIONS
The study found that for Filipinos with type 2 diabetes mellitus at The Medical City, 42.6% had emotional distress showing moderate to severe distress in factor 1 (diabetes-related emotional distress) and factor 3 (food related problems) while 51.1% had suboptimal self-care, poorly scoring in areas of health-care use and dietary control. Majority of patients who had emotional distress and poor self-care were young, pre-obese and had diabetes duration of ±5 years. No significant association was seen between emotional distress and diabetes reported selfcare, together with diabetes related emotional distress and glycated hemoglobin. However, majority of those with emotional distress had higher glycated hemoglobin compared to those without. Moreover, those with poor self-care were 1.5 times more likely to have uncontrolled glycemic outcomes.
Further study is recommended to ascertain other cultural factors that influence diabetes-related emotional distress and diabetes reported self-care as well as other compounding variables that can influence glycemic outcomes.
Limitations of the study
Multivariate analysis on other confounding factors that influence glycated hemoglobin was not done because of the small sample size. Moreover, although participants who had emotional distress or poor self-care were encouraged to attend the life coach sessions in order to discuss the results of their test, the scope of the study did not include triangulation using focus group discussion to provide further information on the exact reason for such distress as well as identify other variables that may influence diabetes distress and reported self-care.
Statement of Authorship
All authors certified fulfillment of ICMJE authorship criteria.
Author Disclosure
The authors declared no conflict of interest.
Funding Source
None.
Authors are required to accomplish, sign and submit scanned copies of the JAFES Author Form consisting of: (1) Authorship Certification, that authors contributed substantially to the work, that the manuscript has been read and approved by all authors, and that the requirements for authorship have been met by each author; (2) the Author Declaration, that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere, that the article does not infringe or violate any copyrights or intellectual property rights, and that no references have been made to predatory/suspected predatory journals; (3) the Author Contribution Disclosure, which lists the specific contributions of authors; and (4) the Author Publishing Agreement which retains author copyright, grants publishing and distribution rights to JAFES, and allows JAFES to apply and enforce an Attribution-Non-Commercial Creative Commons user license. Authors are also required to accomplish, sign, and submit the signed ICMJE form for Disclosure of Potential Conflicts of Interest. For original articles, authors are required to submit a scanned copy of the Ethics Review Approval of their research as well as registration in trial registries as appropriate. For manuscripts reporting data from studies involving animals, authors are required to submit a scanned copy of the Institutional Animal Care and Use Committee approval. For Case Reports or Series, and Images in Endocrinology, consent forms, are required for the publication of information about patients; otherwise, appropriate ethical clearance has been obtained from the institutional review board. Articles and any other material published in the JAFES represent the work of the author(s) and should not be construed to reflect the opinions of the Editors or the Publisher.
REFERENCES
- 1.World Health Organization Global report on diabetes, 2016. https://www.who.int/diabetes/global-report/en/.
- 2.UNITE for Diabetes Philippines Compendium of Philippine Medicine, 2013. http://endo-society.org.ph/wp-content/uploads/2013/06/Diabetes-United-for-Diabetes-Phil.pdf.
- 3.American Diabetes Association Standards of medical care in diabetes 2017;40(Suppl 1):s48-s56; s57-s8. https://professional.diabetes.org/files/media/dc_40_s1_final.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Welch GW, Johnson AM, Polonsky WH. The problem areas in Diabetes Scale: An evaluation of its clinical utility. Diabetes Care. 1997;20(5):760-6. PMID: 10.2337/diacare.20.5.760. [DOI] [PubMed] [Google Scholar]
- 5.Chew BH, Shariff-Ghazali S, Fernandez A. Psychological aspect of diabetes care: Effecting behavioral change in patients. World J Diabetes. 2014;5(1);796-808. PMID: PMCID: 10.4239/wjd.v5.i6.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fisher L, Hessler DM, Polonsky WH, Mullan J. When is diabetes distress clinically meaningful? Establishing cut points for the Diabetes Distress Scale. Diabetes Care. 2012;35(2):259-64. PMID: PMCID: 10.2337/dc11-1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fisher L, Mullan J, Skaff MM, Glasgow RE, Arean P, Hessler D. Predicting diabetes distress in patients with type 2 diabetes: A longitudinal study. Diabet Med. 2009;26(6):622-7. PMID: PMCID: 10.1111/j.1464-5491.2009.02730.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Polonsky WH, Anderson BJ, Loher PA, et al. . Assessment of diabetes-related distress. Diabetes Care. 1995;18(6);754-60. PMID: 10.2337/diacare.18.6.754. [DOI] [PubMed] [Google Scholar]
- 9.Lee J, Lee EH, Kim CJ, Moon SH. Diabetes-related emotional distress instruments: A systemic review of measurement properties. International journal of nursing studies. 2015;52(12); 1868-78. PMID: 10.1016/j.ijnurstu.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 10.Alberti G. The DAWN (diabetes, attitudes, wishes and needs) study. Pract Diabetes Int. 2002;19(1); 22-4. [Google Scholar]
- 11.Schmitt A, Gahr A, Hermanns N, Kulzer B, Huber J, Haak T. The Diabetes Self-Management Questionnaire (DSMQ): Development and evaluation of an instrument to assess diabetes self-care activities associated with glycemic control. Health Qual Life Outcomes. 2013;11:138. PMID: PMCID: 10.1186/1477-7525-11-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schmitt A, Reimer A, Hermanns N, et al. . Assessing diabetes self-management with the Diabetes Self-Management Questionnaire (DSMQ) can help analyze behavioural problems related to reduced glycemic controls. PloS One. 2016;11(3):e0150774. PMID: PMCID: 10.1371/journal.pone.0150774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Snoek FJ, Pouwer F, Welch GW, Polonsky WH. Diabetes-related emotional distress in Dutch and U.S. diabetic patients: Cross-cultural validity of the problem areas in diabetes scale. Diabetes Care. 2000;23(9):1305-9. PMID: 10.2337/diacare.23.9.1305. [DOI] [PubMed] [Google Scholar]
- 14.Miller ST, Elasy TA. Psychosomatic evaluation of the Problem Areas in Diabetes (PAID) survey in Southern, rural African American women with Type 2 diabetes. BMC Public Health. 2008;8:70. PMID: PMCID: 10.1186/1471-2458-8-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee EH, Lee YW, Lee KW, Kim YS, Nam MS. Measurement of diabetes-related distress using the Problem Areas in Diabetes scale: Psychometric evaluations show that the short form is better than the full form. Health Qual Life Outcomes. 2014;12:142. PMID: PMCID: 10.1186/s12955-014-0142-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Snoek FJ, Kersch NYA, Eldrup E, et al. . Monitoring of Individual Needs in Diabetes (MIND)-2. Diabetes Care. 2012;35(11):2128-32. PMID: PMCID: 10.2337/dc11-1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schmitt A. Diabetes Self-Management Questionnaire (DSMQ), 2013. https://eprovide.mapi-trust.org/instruments/diabetes-self-management-questionnaire.
- 18.Nicolucci A, Kovacs Burns K, et al. . Diabetes attitudes, wishes and needs second study (DAWN2TM): Cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes. Diabet Med. 2013;30(7):767-77. PMID: 10.1111/dme.12245. [DOI] [PubMed] [Google Scholar]
- 19.Skovlund S, Peyrot M. The diabetes attitudes, wishes and needs (DAWN) program: A new approach to improving outcomes of diabetes care. Diabetes Spectrum. 2005;18(3):136-42. 10.2337/diaspect.18.3.136. [DOI] [Google Scholar]
- 20.Jimeno CA, Sobrepeña LM, Mirasol RC. DiabCare 2008: A survey on glycemic control and the status of diabetes care and complications among patients with type 2 diabetes mellitus in the Philippines. Philipp J Int Med. 2012;50(1):15-22. [Google Scholar]
- 21.Stranderg RB, Graue M, Wentzel-Larsen T, Peyrot M, Rokne B. Relationship of diabetes-specific emotional distress, anxiety, and overall well-being with HbA1C in adult with type 1 diabetes. J Psychosom Res. 2014;77(3):174-9. PMID: 10.1016/j.jpsychores.2014.06.015. [DOI] [PubMed] [Google Scholar]
- 22.Strandberg RB, Graue M, Wentzel-Larsen T, Peyrot M, Thordarson HB, Rokne B. Longitudinal relationship between diabetes-specific emotional distress and follow-up HbA1c in adults with type 1 diabetes mellitus. Diabet Med. 2015;32(10):1304-10. PMID: PMCID: 10.1111/dme.12781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study Group (UKPDS) Group. Lancet. 1998;352(9131):837-53. PMID: . [PubMed] [Google Scholar]
- 24.Ogbera A, Adeyemi-Doro A. Emotional distress is associated with poor self care in type 2 diabetes mellitus. J Diabetes. 2011;3(4):348-52. PMID: 10.1111/j.1753-0407.2011.00156.x [DOI] [PubMed] [Google Scholar]
- 25.Mehravar F, Mansournia MA, Holakouie-Naieni K, Nasli-Esfahani E, Mansournia N, Almasi-Hashiani A. Associations between diabetes self-management and microvascular complications in patients with type 2 diabetes. Epidemiol Health. 2016;38:e2016004. PMID: PMCID: 10.4178/epih/e2016004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bukhsh A, Lee SWH, Pusparajah P, Schmitt A, Khan TM. Psychometric properties of the Diabetes Self-Management Questionnaire (DMSQ) in Urdu. Health Qual Life Outcomes. 2017;15(1):200. PMID: PMCID: 10.1186/s12955-017-0776-8. [DOI] [PMC free article] [PubMed] [Google Scholar]