Abstract
Background and Objective The Health Information Technology for Economic and Clinical Health (HITECH) Act has distributed billions of dollars to physicians as incentives for adopting certified electronic health records (EHRs) through the meaningful use (MU) program ultimately aimed at improving healthcare outcomes. The authors examine the extent to which the MU program impacted the EHR adoption curve that existed prior to the Act.
Methods Bass and Gamma Shifted Gompertz (G/SG) diffusion models of the adoption of “Any” and “Basic” EHR systems in physicians’ offices using consistent data series covering 2001–2013 and 2006–2013, respectively, are estimated to determine if adoption was stimulated during either a PrePay (2009–2010) period of subsidy anticipation or a PostPay (2011–2013) period when payments were actually made.
Results Adoption of Any EHR system may have increased by as much as 7 percentage points above the level predicted in the absence of the MU subsidies. This estimate, however, lacks statistical significance and becomes smaller or negative under alternative model specifications. No substantial effects are found for Basic systems. The models suggest that adoption was largely driven by “imitation” effects ( q -coefficient) as physicians mimic their peers’ technology use or respond to mandates. Small and often insignificant “innovation” effects (p-coefficient) are found suggesting little enthusiasm by physicians who are leaders in technology adoption.
Conclusion The authors find weak evidence of the impact of the MU program on EHR uptake. This is consistent with reports that many current EHR systems reduce physician productivity, lack data sharing capabilities, and need to incorporate other key interoperability features (e.g., application program interfaces).
Keywords: American recovery and reinvestment act, health information technology, electronic health records, bass model, technology adoption
BACKGROUND AND SIGNIFICANCE
The 2009 Health Information Technology for Economic and Clinical Health (HITECH) Act was signed into law with the explicit intention of accelerating the adoption and promoting the “meaningful use (MU)” of electronic health records (EHRs) by US physicians. 1 The Act appropriated billions of dollars to create financial incentives for eligible providers who implement EHRs and can demonstrate that their systems and utilization patterns meet certain criteria designed to have a meaningful impact on care and costs. 2 By the end of 2014, the federal government had distributed $28.1 billion to eligible physicians and other professionals through the Medicare and Medicaid EHR MU programs. 3 This includes $406 million paid to Medicare Advantage Organizations for eligible providers. 4 For individual physicians who used “certified EHRs” beginning in 2011, the subsidy payments could be either $63 750 over 6 years or $44 000 over 5 years, depending on whether the physician participates in the Medicare or Medicaid program, respectively. Providers must attest to MU Stage Two program eligibility by 2016 to qualify and participate in the reward payments schema. Additionally, physicians eligible for the Medicare incentive program, who do not adopt a certified EHR by 2015 will be penalized 1% of Medicare payments, increasing to 3% over the following 3 years and reaching 5% in later years. The penalties will be in effect at the 5% level thereafter barring a change in the underlying legislation. The logic motivating the legislation was that a pay-for-performance approach, combining rewards early on followed by penalties later, would transform the overall healthcare system by accelerating EHR adoption rates. 5
Evaluating the impact of the HITECH Act is important so that policymakers can assess the extent to which their intended EHR adoption goals are being realized in a cost-effective manner. 6 To date, most physician-focused research on the HITECH Act has described the proportion of physicians eligible for incentives, 7 measured the intention of physicians to apply for incentive payments, and/or assessed their anticipated barriers. 8 Prior to the HITECH Act, Ford et al. 9 utilized simulation methods to project future EHR adoption curves based on observed utilization rates. Using Bass diffusion models, they found that full EHR adoption was unlikely to occur by 2014 as originally planned for by policymakers. Ford et al. 10 later updated their projections to reflect EHR adoption patterns that anticipated the HITECH Act’s imminent passage. Their updated analysis suggested that EHR adoption was increasing, but at a decreasing rate. The earlier projections are over 5 years old, and more importantly, do not encompass the initial MU reward payments period—when the rewards phase took effect. Since then, one forecast using an expert Delphi panel convened in 2010 predicted that 65% of primary care physicians in large group practices, 45% of primary care physicians in small group practices, and 44% of all other specialists could achieve MU by 2015 with these same groups achieving 80%, 65%, and 66% MU in 2019. 11 A weighted average based on the number of practices represented by these groups would predict 46.3% in 2015 and 66.7% in 2019. Therefore, the overall effects of the MU program on physicians’ EHR uptake is unclear compared to normal adoption rate that would have occurred absent the intervention.
The uptake of EHRs may have also been slowed by disappointment with their performance at exchanging data among providers. Data exchange difficulties may arise from a lack of clear standards for information exchange and proprietary innovations by different vendors who may simply be trying to improve certain technical features of their product. More disturbing, however, may be efforts by vendors to gain advantages by not cooperating in data exchange in order to lock in their own customers. The Office of the National Coordinator has recently issued a report on “information blocking” which is defined to occur “when persons or entities knowingly and unreasonably interfere with the exchange or use of electronic health information.” The report states “… there is little doubt that information blocking is occurring and that it is interfering with the exchange of electronic health information.” 12
The purpose of the current study is to utilize Bass diffusion models, 13,14 and federal EHR adoption data that encompasses the MU period to assess the program’s impact on EHR uptake. As such, the study assesses the HITECH Act’s realized impact on the physician EHR diffusion curve. Specifically, the diffusion of “Any” EHR, vs meeting the “Basic” MU requirements, among office-based physicians between 2001 and 2013 is examined. The analysis distinguishes between a PrePay period (2009–2010) after the act was passed but before eligible systems were defined or subsidies were being paid, and a PostPay period (2010–2013) during which subsidies were paid for attesting to the adoption of certified EHR systems.
The study’s results will be of interest to policymakers and stakeholders concerned with promoting improved healthcare delivery through better information management. Moreover, our study will be of interest to researchers interested in understanding the regulatory effects of the HITECH Act on the EHR adoption market. Lastly, those audiences concerned with patient safety and healthcare cost control will find the results informative.
METHODS
To examine the adoption of EHRs and the effects of the HITECH Act, we estimated a Gamma Shifted Gompertz (G/SG) diffusion model as well as the Bass model embedded in it. Rogers is credited with creating a theory of technology diffusion that describes innovators (i.e., first adopters), early adopters, early majority, late majority, and laggard’s adoption pattern. 15 Numerous studies of the diffusion of new products have examined the shape of the diffusion curve which may plot total product sales or the share of a potential market that has been captured over time. Many of these studies have found an S-shaped curve which depicts an initially slow start followed by a period of rapid adoption and then a leveling off as a market approaches maturation. 16,17 Bass is credited with developing a simple functional form involving two key coefficients that could be fit to a small number of early market data points so that the estimated curve could be used to predict the future path of adoption in the market. 18 In Bass’s scheme the adoption path was governed by innovation factors (coefficient p ) representing enthusiasm by early adopters who were alert to the potential uses of the new product and by imitation factors (coefficient q ) where later adopters join the crowd to embrace the demonstrated benefits of the product. The relative sizes of p and q determine the elongation or compression of the S-shape. In a later generalization of the model, Bass added coefficients for variables such as price and advertising which he found to be empirically important when these variables did not change smoothly over time. 19 Later extensions by others placed the Bass function within a family of G/SG functions distinguished by the degree of heterogeneity (coefficient α) among the adopters where the Bass model represented (α = 1) a homogeneous population. 20 The G/SG model also reduces to the familiar exponential model when α = 0.
The basic formula in the G/SG family for calculating the cumulative percentage of adopters at any point, using discrete time notation, can be written as
| (1) |
where
F ( t ) = the cumulative fraction of adopters at time t ,
p = coefficient of innovation, sometimes called the advertising effect, capturing the intrinsic tendency to adopt, and the effect of time invariant external influences,
q = coefficient of imitation or social contagion, sometimes called the word-of-mouth effect, capturing the extent to which the probability that one adopts (given that one has not yet done so) increases with the proportion of eventual adopters who have already opted in and
t = period of measurement (0, 1, 2, 3,…)
α = coefficient of heterogeneity; if α = 1 the model is the Bass form, if α = 0 the model is an exponential,
β = vector of other coefficients, and
X = vector of other variables
This class of models has several attractive features for assessing an intervention’s impact on adopters’ behaviors. When fit with a few early data points for p and q , it can be used to forecast a technology’s future uptake path, over time, in a specific market. When fit with a longer series of historical observations, it can be used to test hypothesis about the time path of diffusion of one technology or product compared to another. For either purpose, the coefficients p and q describe the innovation versus imitation factors driving the diffusion rate, respectively. A high value for q indicates that the diffusion has a quick start but also tapers off quickly. A high value of p indicates that the diffusion starts slowly but later accelerates as the product’s utility is more broadly accepted by later adopters. Typical values in the Bass diffusion literature for p range from below 0.01 to around 0.03; typical values for q range from 0.3 to 0.5. 16 When q is larger than p , the cumulative number of adopters F ( t ) + F ( t − 1) has the graph of an S-shaped curve often seen for high risk, innovative products that take extended time to become widely used. When q is smaller than p , the cumulative number of adopters rises quickly and then flattens (an inverse J -shaped curve) in a pattern typical of less risky innovations, such as the adoption of new consumer durables (e.g., washers and dryers). Once p and q are known, the time ( t *) at which the peak adoption rate occurs (i.e., the period when the largest number of individuals adopts) can be calculated as 21 :
| (2) |
where t * is often referred to as the inflection or “tipping point” when the diffusion paradigm becomes self-sustaining.
The G/SG model and its embedded Bass form have several limitations. First, coefficient estimates may be unstable depending on the point in time that is assumed to be the start of sales ( t = 0). 20 For some products one may have to make an assumption about the starting date because data on sales during the early startup period may not be available or the date on which the product was first available may be uncertain. Second, forecasting accuracy varies by functional form. One study found that for one, two and three step-ahead forecasts, the G/SG model gave more accurate predictions than the Bass when using simulated data but the Bass was more accurate in two and three step-ahead forecasts using real data. 22 Third, estimates of diffusion models often vary systematically as more data points become available. For the Bass model in particular, estimates of q tend to decrease and estimates of p increase as data points are added. 20,22 Estimating the more flexible G/SG lessens the risk of systematic error and misinterpretation of the coefficients. 22
DATA
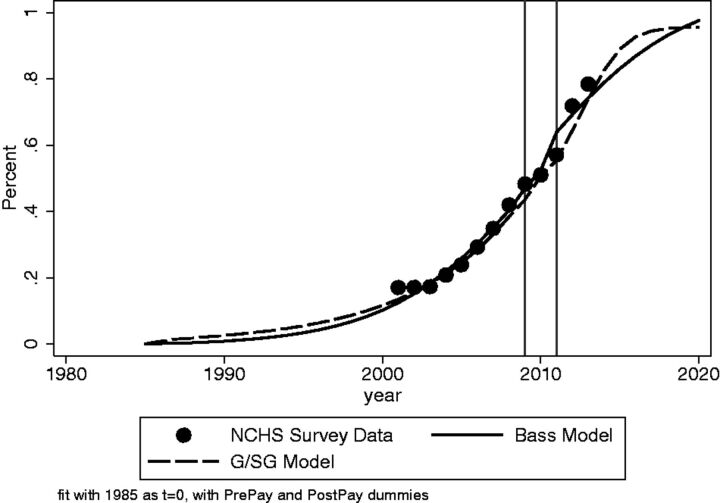
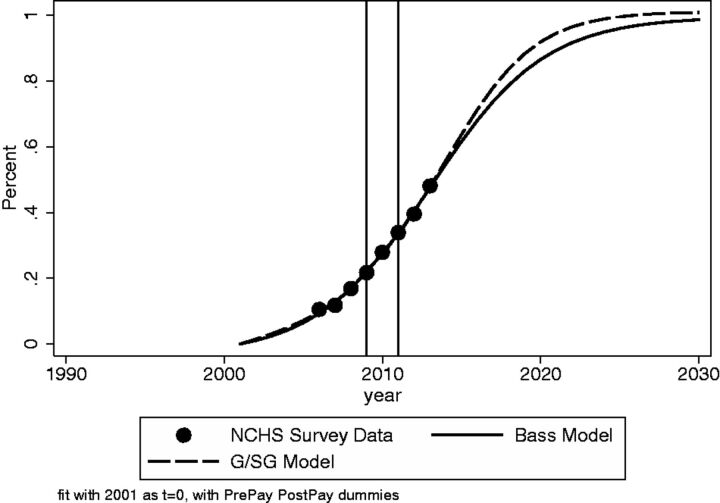
We examine two series on the adoption of EHRs by nonfederal office based physicians excluding radiologists, anesthesiologists, and pathologists. These national aggregate survey estimates come from various waves and modalities of the National Ambulatory Medical Care Survey (NAMCS) collected via in-person interviews and mail surveys by the Centers for Disease Control and Prevention (CDC) and the National Center for Health Statistics. 23 The “Any EHR System” series spanning 2001–2013 applies to physicians who responded “yes” to the question “does this practice use electronic medical records or electronic health records (not including billing records)?.” Figure 1 plots the data points from various years of the survey for the percent of physicians in the survey reporting Any EHR. The figure also shows G/SG and Bass models curves which are discussed later. Figure 2 plots the data points for the percent of physicians responding during survey years 2006–2013 that they had a “Basic” system (perhaps better named as a Robust System) defined as having all of the following functionalities: “… patient history and demographics, patient problem lists, physician clinical notes, comprehensive list of patients’ medications and allergies, computerized orders for prescriptions, and ability to view laboratory and imaging results electronically.” The figure also shows G/SG and Bass model curves, which are discussed later.
Figure 1:
Bass and G/SG models of Any EHR Adoption.
Figure 2:
Bass and G/SG models of Basic EHR Adoption.
Estimation
We estimated the G/SG and Bass models in equation (1) to include in the X vector two dummy variables to account for shifts in the adoption process due to the passage of the HITECH Act and the subsequent payment of subsidies. The dummy PrePay equals 1 for the years 2009 and 2010 and otherwise equals zero. This dummy variable will capture changes in adoption that occurred after the passage of the HITECH legislation in 2009 but before any subsidy payments were made in 2011. This was a period of uncertainty when the federal government was developing EHR system specifications that it would subsequently certify as being eligible for subsidy payments. Similar to other new technologies, it was expected that physicians were likely to be cautious about adopting EHRs until they could be sure that the system they invested in would qualify for a subsidy. 24 The dummy PostPay equals 1 for 2011 through the end of the data series in 2013 and otherwise equals zero. The PostPay dummy variable captures physicians’ responses to subsidy payments that began in 2011. It was widely expected that physicians EHR adoption rate would jump beginning in 2011 because of the financial support. 25 For the Basic System, a similar model is estimated except that the observed data series begins in 2006.
The Bass model assumes new adoptions grow without decline. The NAMCS reports a slight decline in the cumulative percent of “Any EHR system” adoption over the period from 2001 to 2003. One explanation is that the EHR use differences are due to population-sampling differences over the periods studied. Given the number of physicians practicing in small groups is declining, sampling drift may explain the decline as doctors migrate to larger practices that have an EHR. Therefore, the estimation is adjusted for the percent of adopters of “Any EHR system” to be 17.0 (from 18.4) and 17.1 (from 17.3) in 2001 and 2002.
We have not been able to find data series on either the prices of EHR software or expenditures on advertising and marketing. One appealing feature of our models is that they can be estimated without price or advertising information and yield coefficients that are informative about the diffusion process. 19,26
The time at which EHR systems became available for purchase or were actually bought by physician office practices is not well documented. A report by the Institute of Medicine in 1991 calling for the widespread use of “computerized patient records” is often considered to be the starting point for today’s EHR industry. 27 It is not clear from the report how many vendors may have been selling EHR systems for office based physicians at that time. Because the G/SG and Bass models are known to be sensitive to the starting date, we estimated the sensitivity of these models using the available data with various years specified as t = 0. For the Any EHR models, we experimented with annual starting points from 1985 to 1995; for Basic systems we used starting points of 1995 to 2005. We estimated these models with nonlinear regression using Stata version 14. 28
Our sensitivity estimates were concerned with the following issues. First, is the G/SG α coefficient equal to 1.0, confirming the appropriateness of estimating a Bass model? Second, are the sign, size, and significance of the p and q coefficients sensitive to the choice of the starting year? Third, how large and statistically significant are the PrePay and PostPay variables that would indicate the effect of the MU subsidies?
RESULTS
The fit of the G/SG and Bass models for Any EHR system is shown in Figure 1 which draws the graph lines based upon the estimated coefficients. Both models track the available data points reasonably well assuming that 1985 is the starting point for the system. For the years 2014 to 2020 beyond the observed data, the G/SG model predicts a more rapid adoption of EHRs. All of the models are characterized by small values of the innovation coefficient p, much larger values of the imitation coefficient q. The α coefficient for the G/SG model is usually small (around 0.15) and sometimes statistically significant suggesting that the data have in them some heterogeneity or “extra bass skew” that might make them better described by the G/SG model. For the 1985 starting point, the PrePay and PostPay coefficients are statistically indistinguishable from zero in both models and in the G/SG model the coefficients have an unexpected negative sign suggesting that the subsidies actually decreased adoption. In the Bass model, the PrePay and PostPay coefficients suggest that the MU subsidies are associated with an increase in adoption of EHRs of 1 and 7 percentage points, respectively, during these periods. If we re-draw the graphs for annual starting points between 1986 and 1995, the Bass model graph remains virtually unchanged but the G/SG model has erratic kinks for starting years after 1991 and it improbably attributes around half of cumulative adoption to the PostPay subsidy (These additional graph results are not shown but are available from the authors.)
Figure 2 shows the data and estimated graphs for the Basic EHR system using 2001 as the starting date for the product. The G/SG and Bass models both fit the data reasonably well with the G/SG again predicting more rapid adoption in the future. When different starting times are selected, the Bass model preserves its shape and fit but the G/SG model again has erratic kinks in some years. Both models find small and statistically insignificant effects for both the PrePay and PostPay dummies. In the Appendix we present tables with the regression results and a discussion of some further sensitivity tests.
DISCUSSION
Using 13 years of data consistently collected by the NAMCS on the adoption of “Any EHR system” in physicians’ offices, a Bass diffusion model predicts that the adoption rate in 2017 (the year following the deadline for subsidy eligibility) will be around 90% (with standard error 2.0%) compared to the 83% (standard error = 5.0%) that would be predicted in the absence of the HITECH subsidies. This change is consistent with the presumed effects of the HITECH subsidy payments and the reimbursement penalties that Medicare will impose on physicians who do not have certified EHR systems. The model estimates that anticipated subsidies during the PrePay period contributed slightly more than a one percentage point increase in the adoption of “AnyEHR system.” During the PostPay period with subsidy payments, EHR adoption increased by seven percentage points. However, these estimates of the HITECH Act’s effects lack statistical significance. A similar story emerges when the models are fit on NAMCS data for 2006–2013 applying to the adoption of EHR “Basic” systems with more extensive capabilities. The model finds that the passage of the HITECH Act and the subsequent subsidy payments contributed statistically insignificant nudges to the EHR diffusion curve of less than one percentage point and a half percentage point, respectively.
We conducted extensive sensitivity tests of these findings by estimating the Bass model with alternative years at which the marketing of software may have begun. We also estimated a G/GS model which embeds both the Bass model and a simple exponential model as special cases. We found that the Bass model was not seriously affected by the presumed starting point year for the beginning of the market but the G/SG was sensitive so that its estimates of subsidy effects varied over improbable ranges depending on which starting year was chosen.
The analyses support the speculation that the adoption of “Any EHR system” was largely driven by what the Bass model designates as “imitation” effects ( q -coefficient). The “innovation” coefficients ( p -coefficient) in the various models are well below the ranges for other technologies (the average p = 0.03 found in 213 similar analyses). 29 The standard interpretation of q and p coefficients in this arrangement is that physicians are striving to keep up with their peers in EHR use rather than adopting due to an external influence such as advertising. 5
The relatively large coefficient of contagion ( q- coefficient) can be interpreted in 2 ways. On the one hand, mimetic forces may induce physicians to adopt in areas where other physicians have already adopted and where they are using EHRs as a networking tool for Health Information Exchange. 30 On the other hand, physicians may merely have a strong desire to keep up with technical changes in the field without any information sharing intention or external stimulus. Both scenarios are desirable. The former scenario in particular (e.g., the desire to share patient information) is desirable because data sharing is at the core of the value that electronic records provide. However, the empirical evidence-to-date shows that most physicians have not connected their EHRs to other provider organizations due in part to lack of connectivity in their software. 31–33 The latter scenario suggests that the adoption of EHRs is being driven by expected gains in convenience and productivity much like the decades-earlier adoption of the personal computers into the workplace. A potentially worse scenario is that the MU program promoted the adoption of inferior technologies that had already been rejected by physicians. 32
Collectively, the analyses suggest that the external stimulus on physicians of the MU Program had ambiguous effects on the overall adoption rates. Somewhat like the “cash for clunkers” subsidies in the automobile industry, the HITECH subsidies may have only contributed to inevitable adoptions. 34 However, the new regulation may have had unintended, negative consequences. One explanation is that the MU requirement for a “certified” EHR may have slowed technological advancements in the field as system vendors invested in compliance rather than research and development. 32 More work is needed to better understand the dynamics of physician adoption patterns. 35 Our results for physicians are, however, consistent with an evaluation of the effect of subsidies on the adoption of electronic medical records in hospitals, which found that “in the absence of HITECH incentives, the 77 percent adoption rate would have been realized by 2013, just 2 years after the date achieved due to HITECH.” 36
This paper has the limitation that we have looked only at aggregate national data over relatively short periods of 2001–2013 and 2006–2013. This may explain the lack of statistical significance for the estimated effects of the subsidies. More can be learned from studies of EHR adoption over time across geographic regions and in specific healthcare providers. The current paper also does not comment on the comparative costs and benefits of accelerating market adoption via subsidies and reimbursement penalties. Did forcing the adoption of EHRs save lives, improve the quality of care, or favorably reduce inflation in medical spending? Evaluations of the effects of EHRs to date have found weak and inconsistent effects. 37 Absent evidence of significant gains in either care quality or cost savings, the federal government’s near-term return on investment may be negligible or negative. Additionally, little generalizable evidence currently exists to show that the electronic exchange of health information among providers boots efficiency, reduces healthcare costs and improves outcomes for patients. 38 Future studies should therefore seek to examine the impact of the HITECH Act on subsequent quality and cost outcomes.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
COMPETING INTERESTS
The authors have no competing interests to declare.
CONTRIBUTORS
S.T.M. wrote the initial draft and final version of manuscript and estimated the nonlinear Bass models. N.M. wrote the detailed discussion of issues related to EHRs, health information technology, manuscript revisions, and previous analyses of Bass Models in prior papers. S.R. is responsible for literature review, identification of relevant data, and revision of draft text.
E.W.F. wrote the detailed discussion of health information technology policy, manuscript revisions and previous analyses of Bass Models in prior papers.
REFERENCES
- 1. Maxson E Jain S Kendall M Mostashari F Blumenthal D . The regional extension center program: helping physicians meaningfully use health information technology . Ann Intern Med. 2010. ; 153 ( 10 ): 666 – 670 . [DOI] [PubMed] [Google Scholar]
- 2. Buntin MB Burke MF Hoaglin MC Blumenthal D . The benefits of health information technology: a review of the recent literature shows predominantly positive results . Health Aff. 2011. ; 30 ( 3 ): 464 – 471 . [DOI] [PubMed] [Google Scholar]
- 3. Centers for Medicare and Medicaid Services . Medicare and Medicaid EHR Incentive Program Basics 2015 [cited February 17, 2015] . http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Basics.html . Accessed February 29, 2015 . [Google Scholar]
- 4. Wright A Feblowitz J Samal L McCoy AB Sittig DF . The medicare electronic health record incentive program: provider performance on core and menu measures . Health Serv Res. 2014. ; 49 ( 1pt2 ): 325 – 346 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Samuel CA . Area-level factors associated with electronic health record adoption and meaningful use in the Regional Extension Center Program . JAMIA. 2014. ; 21 ( 6 ): 976 – 983 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Millenson ML . The long wait for medical excellence . Health Aff. 2013. ; 32 ( 10 ): 1757 – 1760 . [DOI] [PubMed] [Google Scholar]
- 7. Bruen BK Ku L Burke MF Buntin MB . More than four in five office-based physicians could qualify for federal electronic health record incentives . Health Aff. 2011. ; 30 ( 3 ): 472 – 480 . [DOI] [PubMed] [Google Scholar]
- 8. Menachemi N Yeager VA Bilello L Harle CA Sullivan CB Siler-Marsiglio KI . Florida doctors seeing Medicaid patients show broad interest in federal incentives for adopting electronic health records . Health Aff. 2011. ; 30 ( 8 ): 1461 – 1470 . [DOI] [PubMed] [Google Scholar]
- 9. Ford EW Menachemi N Phillips MT . Predicting the adoption of electronic health records by physicians: When will health care be paperless? JAMIA . 2006. ; 13 ( 1 ): 106 – 112 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ford EW Menachemi N Peterson LT Huerta TR . Resistance is futile: but it is slowing the pace of EHR adoption nonetheless . JAMIA. 2009. ; 16 ( 3 ): 274 – 281 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Blavin FE Buntin MB . Forecasting the use of electronic health records: an expert opinion approach . Medicare Medicaid Res Rev. 2013. ; 3 ( 2 ): E1 – E16 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. The Office of the National Coordinator for Health Information Technology (ONC) . Report to Congress: Report on Health Information Blocking . In: Department of Health and Human Services, ed. Washington, DC; 2015 . [Google Scholar]
- 13. Bass FM . A new product growth model for consumer durables . Manag Sci. 1969. ; 15 : 215–227 . [Google Scholar]
- 14. Lilien GL Van de Bulte C . Diffusion Models: Managerial Application and Software . University Park: , PA: The Pennsylvania State University; ; 1999. . [Google Scholar]
- 15. Rogers EM . Diffusion of Innovations . New York: : Free Press of Glencoe; ; 1962. . [Google Scholar]
- 16. Mahajan V Muller E Bass FM . Diffusion of new products: empirical generalizations and managerial uses . Marketing Sci. 1995. ; 14 ( 3 ): G79 – G88 . [Google Scholar]
- 17. Mahajan V Muller E Wind Y . New product diffusion models: from theory to practice . In: Mahajan V, Muller E, Wind Y , eds. New Product Diffusion Models . Boston: : Kluwer Academic; ; 2000. : 3 – 24 . [Google Scholar]
- 18. Bass FM . A new product growth for model consumer durables . Manag Sci. 1969. ; 15 ( 5 ): 215 – 227 . [Google Scholar]
- 19. Bass FM Krishnan TV Jain DC . Why the Bass model fits without decision variables . Marketing Sci. 1994. ; 13 ( 3 ): 203 – 223 . [Google Scholar]
- 20. Bulte Cvd Lilien GL . Bias and systematic change in the parameter estimates of macro-level diffusion models . Marketing Sci. 1997. ; 16 ( 4 ): 338 – 353 . [Google Scholar]
- 21. Van den Bulte C . Want to know how diffusion speed varies across countries and products? Try using a Bass model PDMA Visions. PDMA Visions Magazine. 2002;XXVI(4):12–15 . [Google Scholar]
- 22. Bemmaor AC Lee J . The impact of heterogeneity and Ill-conditioning on diffusion model parameter estimates . Marketing Sci. 2002. ; 21 ( 2 ): 209 – 220 . [Google Scholar]
- 23. Hsiao C-J Hing E . Use and characteristics of electronic health record systems among office-based physician practices: United States, 2001–2013 . NCHS data brief Hyattsville, MD: National Center for Health Statistics. http://wwwcdcgov/nchs/data/databriefs/db143htm . 2014; No. 143 . [PubMed] [Google Scholar]
- 24. Spooner SA . We are still waiting for fully supportive electronic health records in pediatrics . Pediatrics. 2012. ; 130 ( 6 ): e1674 – e1676 . [DOI] [PubMed] [Google Scholar]
- 25. Joseph SB Sow MJ Furukawa MF Posnack S Daniel JG . E-prescribing adoption and use increased substantially following the start of a federal incentive program . Health Aff. 2013. ; 32 ( 7 ): 1221 – 1227 . [DOI] [PubMed] [Google Scholar]
- 26. Deepa C Gerard JT . A Critical Review of Marketing Research on Diffusion of New Products . In: Naresh K Malhotra , ed. Review of Marketing Research (Review of Marketing Research, Volume 3) Emerald Group Publishing Limited; , 2007. : 39 – 80 . [Google Scholar]
- 27. Dick RS Steen EB Detmer DE , eds. The Computer-Based Patient Record: An Essential Technology for Health Care . Revised Edition. Washington, D.C.: Institute of Medicine; 1997 . [PubMed] [Google Scholar]
- 28. StataCorp . Stata Statistical Software: Release 14 . College Station, TX: StataCorp LP; 2015 . [Google Scholar]
- 29. Sultan F Farley JU Lehmann DR . A meta-analysis of applications of diffusion models . J Market Res. 1990. ; 27 ( 1 ): 70 . [Google Scholar]
- 30. Yaraghi N Du AY Sharman R et al. . Professional and geographical network effects on healthcare information exchange growth: does proximity really matter? JAMIA . 2014. ; 21 ( 4 ): 671 – 678 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rittenhouse DR Casalino LP Shortell SM et al. . Small and medium-size physician practices use few patient-centered medical home processes . Health Aff. 2011. ; 30 ( 8 ): 1575 – 1584 . [DOI] [PubMed] [Google Scholar]
- 32. Whitney E . Sharing patient records is still a digital dilemma for doctors . http://www.npr.org/blogs/health/2015/03/06/388999602/sharing-patient-records-is-still-a-digital-dilemma-for-doctors . Morning Edition. 2015 . [Google Scholar]
- 33. Alexander L Burr R Coburn T Enzi M Roberts P Thune J . Reboot: Re-examining the Strategies Needed to Successfully Adopt Health IT . In: Senate US , ed. Washington D.C; ., 2013. . [Google Scholar]
- 34. Mian A Sufi A . The Effects of Fiscal Stimulus: Evidence from the 2009 ‘Cash for clunkers’ Program . National Bureau of Economic Research; , Cambridge MA: ; 2010. . [Google Scholar]
- 35. Decker SL Jamoom EW Sisk JE . Physicians in nonprimary care and small practices and those age 55 and older lag in adopting electronic health record systems . Health Aff. 2012. ; 31 ( 5 ): 1108 – 1114 . [DOI] [PubMed] [Google Scholar]
- 36. Dranove D Garthwaite C Li B Ody C . Investment Subsidies and the Adoption of Electronic Medical Records in Hospitals . National Bureau of Economic Research; , Evanston, IL: ; 2014. . [DOI] [PubMed] [Google Scholar]
- 37. Ancker JS Kern LM Edwards A et al. . How is the electronic health record being used? Use of EHR data to assess physician-level variability in technology use . JAMIA. 2014. ; 21 ( 6 ): 1001 – 1008 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Rahurkar S Vest JR Menachemi N . Despite the spread of health information exchange, there is little evidence of its impact on cost, use, and quality of care . Health Aff. 2015. ; 34 ( 3 ): 477 – 483 . [DOI] [PubMed] [Google Scholar]