To the Editor:
The COVID-19 pandemic has impacted cancer screening,1, 2, 3 with multistate data reporting reductions in breast, colon, and cervical cancer screenings but not reporting on lung cancer screening (LCS).4 In late April 2020, the Radiological Society of North America COVID-19 Task Force suggested postponing nonurgent outpatient imaging, including LCS.3 Also in April 2020, an expert panel of 24 physicians provided guidance for LCS during the pandemic, stating it was appropriate to defer enrollment in LCS for new patients and to delay annual screening but that patient preferences should also be considered.1 Patients eligible for LCS have significant smoking exposure and underlying comorbidities,5 putting this group at increased risk for infection and severe complications from COVID-19. Although two studies reported reductions in LCS at the start of the pandemic,6,7 differences in screening volumes based on patient characteristics and COVID-19 risk factors were not reported. We sought to compare LCS volumes from multiple screening centers before and during the pandemic to determine whether patients who underwent LCS differ based on sociodemographic and COVID-19 risk factors. If certain subgroups of the population are less likely to undergo LCS or delay LCS during the ongoing COVID-19 pandemic, this may impact downstream lung cancer disparities.
Materials and Methods
This analysis included all low-dose CT (LDCT) lung screening examinations that occurred among adults ≥18 years old (98.7% aged 55-80 years) at two academic and two community imaging sites affiliated with the University of North Carolina Healthcare System from January 1, 2019, to September 30, 2020. Patient characteristics included age, sex, race, smoking status, BMI, hypertension, COPD, and patient residence. We classified screening examinations as initial LDCT vs returning for annual screening examinations as part of routine care. This study was approved by the Institutional Review Board of the University of North Carolina at Chapel Hill.
We conducted two analyses. First, to compare LCS volumes before and during the pandemic, we used an interrupted time series analysis and assigned the date of the first COVID-19 diagnosis in North Carolina as the intervention date (March 3, 2020). We calculated the predicted mean number of examinations per month in the pre-COVID-19 time period (January 1, 2019, to March 2, 2020) and each subsequent month. For each time period (pre-COVID-19 and subsequent months), this involved computing two predicted means: one accounting for COVID-19 and one assuming an absence of COVID-19. We then calculated differences between these two predicted means for each post-COVID-19 month, along with 95% CIs. Finally, for the first analysis, we calculated the percentage difference in the predicted monthly means, given the onset of the COVID-19 pandemic, compared with the predicted monthly means in the absence of the COVID-19 pandemic. The overall effect of COVID-19 on screening volume was tested using the likelihood ratio test.
In our second analysis, we investigated whether changes in receipt of LCS disproportionately affected patient subgroups, by comparing patient characteristics during four time periods: (1) before COVID-19: January 1, 2019, to March 2, 2020; (2) beginning of pandemic: March 3, 2020, to March 29, 2020; (3) shut down: March 30, 2020, to May 21, 2020, when North Carolina state-wide “Stay-At-Home” order was in place and the health-care system recommended closing LCS initial enrollment and annual follow up; and (4) ramp-up: May 22, 2020, through September 30, 2020, when North Carolina “Stay-At-Home Order” was lifted, but other restrictions remained, and the health-care system began scheduling initial and follow-up LCS examinations. Random-effects models were used to generate predicted probabilities of outcomes by time period. Pairwise differences in predicted probabilities by time period were computed, with probability values adjusted with the use of the false discovery rate to control for type 1 error.8 All statistical analysis was conducted with SAS software (version 9.4; SAS Institute Inc, Cary, NC). Two-sided probability values <.05 were considered statistically significant.
Results
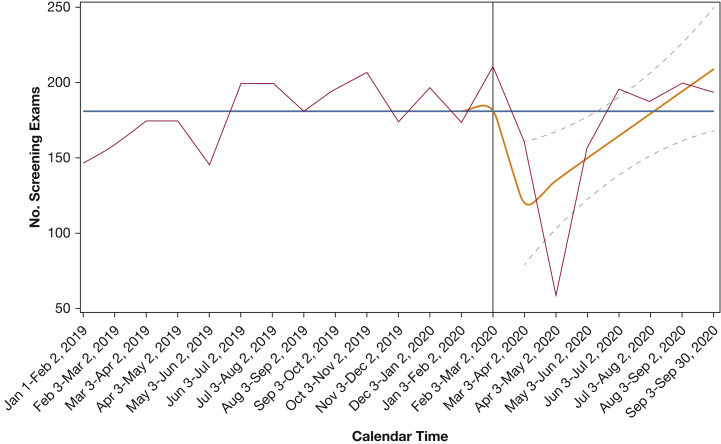
We included 3,688 LCS examinations: 1,930 (52.3%) were initial LDCT scans, and 1,758 (47.7%) were returns for annual LCS. From January 1, 2019, to March 2, 2020, LCS volumes steadily increased over time with a notable decrease in early March 2020 with the interrupted time series analysis demonstrating a significant effect of COVID-19 on reducing screening volumes (likelihood ratio test: P = .0068) (Fig 1). The largest reductions in predicted LCS volumes were seen in March 2020 (percentage change: -33.6% [95% CI, -55.3% to -11.9%]) that coincided with the beginning of the COVID-19 pandemic. By June 2020, predicted LCS volumes had returned to expected pre-COVID-19 levels based on trends before March 3, 2020 (percentage change: -9.1% (95% CI, -23.0%-4.7%]). LCS volumes from June to September 2020 remained similar to pre-COVID-19 levels (percentage change: 15.3% (95% CI, -7.8%-38.4%]).
Figure 1.
Trend in lung cancer screening across four screening sites, January 2019 to September 2020. The time series plots show actual low-dose CT lung cancer screening examinations performed between January 1, 2019, and September 30, 2020 (solid red line), smoothed predicted examinations in the absence of COVID-19 (solid blue line), and smoothed predicted examinations accounting for COVID-19 (solid orange line). The number of lung cancer screening examinations is shown on the Y-axis; the calendar time is shown on the X-axis. The expected number of examinations was modeled based on the preintervention trend (before March 3, 2020; vertical line). The dotted gray lines around the observed number of examinations indicate 95% CI bands estimated with the use of interrupted time series models. Although the interrupted time series procedure itself does not use smoothing, we used smoothing to ensure that the vertices were connected by a differentiable line.
Comparison of patient characteristics during the pre-COVID-19 time period to each of the three time periods during the pandemic found no significant differences for age, sex, race, smoking status, BMI, COPD, hypertension, or patient residence (P > .05 for all) (Table 1). The proportion of initial LDCT LCS examinations was highest in the pre-COVID-19 time period (53.8%) and decreased in all three subsequent time periods: 50.7% during the beginning of pandemic, 49.7% during the shut down, and 48.6% during the ramp-up, with significant differences between the pre-COVID-19 and ramp-up time periods (P = .0072).
Table 1.
Comparison of Patient Characteristics of Those Who Underwent Lung Cancer Screening Before and During the COVID-19 Pandemic, January 2019 to September 2020
| Variable | Before Coronavirus (01/01/2019 – 03/02/2020) (n = 2,541) |
Beginning of Pandemic (03/02/2020 – 03/29/2020) (n = 152) |
Shut Down (03/30/2020 – 05/21/2020) (n = 151) |
Ramp-Up (05/22/2020 – 09/30/2020) (n = 844) |
|---|---|---|---|---|
| Mean monthly volumea | 181.1 | 171.4 | 86.7 | 194.6 |
| Screening examination type | ||||
| Initial | 1,368 (53.8) | 77 (50.7) | 75 (49.7) | 410 (48.6) |
| Returning | 1,173 (46.2) | 75 (49.3) | 76 (50.3) | 434 (51.4) |
| Age, No. (%) | ||||
| <65 y | 1,200 (47.2) | 75 (49.3) | 73 (48.3) | 360 (42.7) |
| ≥65 y | 1,341 (52.8) | 77 (50.7) | 78 (51.7) | 484 (57.4) |
| Sex, No. (%) | ||||
| Female | 1,225 (48.2) | 62 (40.8) | 82 (54.3) | 432 (51.2) |
| Male | 1,316 (51.8) | 90 (59.2) | 69 (45.7) | 412 (48.8) |
| Race, No. (%) | ||||
| White | 1,974 (77.7) | 110 (72.4) | 119 (78.8) | 637 (75.5) |
| Non-white | 567 (22.3) | 42 (27.6) | 32 (21.2) | 207 (24.5) |
| Smoking Status, No. (%) | ||||
| Current | 1,071 (42.2) | 76 (50.0) | 61 (40.4) | 351 (41.6) |
| Former | 1,470 (57.9) | 76 (50.0) | 90 (59.6) | 493 (58.4) |
| BMI | ||||
| Under/normal/overweight | 1,495 (61.1) | 88 (59.5) | 87 (60.8) | 490 (60.6) |
| Obese | 951 (38.9) | 60 (40.5) | 56 (39.2) | 319 (39.4) |
| Missingb | 95 | 4 | 8 | 35 |
| Hypertension, No. (%) | ||||
| Yes | 1,599 (62.9) | 87 (57.2) | 92 (60.9) | 514 (60.9) |
| No | 942 (37.1) | 65 (42.8) | 59 (39.1) | 330 (39.1) |
| COPD, No. (%) | ||||
| Yes | 1,064 (41.9) | 59 (38.8) | 69 (45.7) | 359 (42.5) |
| No | 1,477 (58.1) | 93 (61.2) | 82 (54.3) | 485 (57.5) |
| Patient residence, No. (%) | ||||
| Rural | 501 (19.7) | 29 (19.1) | 23 (15.2) | 187 (22.2) |
| Urban | 2,040 (80.3) | 123 (80.9) | 128 (84.8) | 657 (77.8) |
Mean monthly volumes were calculated by computing the volume in the given time period divided by a normalized denominator. The normalized denominator was calculated by computing the exact number of days in the time period and multiplying this by the inverse of the average number of days in a month (12/365.25).
Missing are excluded from column percentage.
Discussion
Despite sharp reductions in LCS volumes at the start of the pandemic, LCS volumes returned to pre-COVID-19 levels by June 2020 and remained at pre-COVID-19 volumes through September 2020. Our results are in line with the 62% reduction in LCS volume reported by the Population-based Research to Optimize the Screening Process consortium7 and with the 74% reported by Lang et al.6 We found that the proportion of initial LCS examinations decreased from 53.8% in the pre-COVID-19 time period to 48.6% in the ramp-up time period, with almost one-half of LCS occurring in new patients during the pandemic. This finding is counter to the CHEST expert panel’s suggestion that new patients forgo enrollment in LCS during the pandemic and may reflect local transmission rates or the availability of resources.1 Our results may be explained by differences in how the CHEST consensus statement regarding LCS during the pandemic was communicated within sites and to providers who refer patients for LCS. This is an area that warrants further investigation to understand best strategies for rapid dissemination of recommendations across screening programs.
Our results do not demonstrate differences in LCS volumes before vs during COVID-19 among non-white patients or rural patients, both of whom persistently have experienced disparities in lung cancer outcomes and other cancer screening modalities.9 Additionally, our results do not suggest that patients at high risk of COVID-19 complications (ie, patients who are obese, have COPD, or have hypertension) were less likely to undergo LCS. Our study is limited to four lung imaging sites in one state, and our findings should be confirmed in other geographic areas where pandemic responses may have differed. As the pandemic continues to surge, ongoing monitoring of cancer screening and downstream consequences on cancer diagnoses are needed to ensure that all patients receive the highest quality care.
Acknowledgments
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Footnotes
FINANCIAL/NONFINANCIAL DISCLOSURES: The authors have reported to CHEST the following: M. R. served as an Advisory Board Member for Biodesix and bioAffinities Tech, and served on an advisory research panel for Johnson and Johnson. None declared (L. H., T. B., T. B., J. L.).
FUNDING/SUPPORT: This study was funded by NIH/NCI [grants R01CA212014 and R01CA251686].
References
- 1.Mazzone P.J., Gould M.K., Arenberg D.A. Management of lung nodules and lung cancer screening during the COVID-19 pandemic: CHEST Expert Panel Report. Chest. 2020;158(1):406–415. doi: 10.1016/j.chest.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cancer Screening During the COVID-19 Pandemic American Cancer Society. https://www.cancer.org/healthy/find-cancer-early/cancer-screening-guidelines/cancer-screening-during-covid-19-pandemic.html
- 3.Mossa-Basha M., Azadi J., Ko J., Klein J.M.C. COVID-19 Task Force. RSNA COVID-19 Task Force: Best Practices for Radiology Departments during COVID-19. RSNA 2020 [updated 4/27/2020] https://www.rsna.org/-/media/Files/RSNA/Covid-19/RSNA-COVID-19-bestpractices
- 4.Epic Health Research Network Preventive cancer screenings during COVID-19 pandemic. Published 2020. https://ehrn.org/articles/delays-in-preventive-cancer-screenings-during-covid-19-pandemic
- 5.Howard D.H., Richards T.B., Bach P.B., Kegler M.C., Berg C.J. Comorbidities, smoking status, and life expectancy among individuals eligible for lung cancer screening. Cancer. 2015;121(24):4341–4347. doi: 10.1002/cncr.29677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lang M., Yeung T., Shepard J.O. Operational challenges of a low-dose CT lung cancer screening program during the Coronavirus Disease 2019 Pandemic. Chest. 2021;159(3):1288-1291. CHEST. 2020 doi: 10.1016/j.chest.2020.10.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Corley D.A., Sedki M., Ritzwoller D.P. Cancer screening during Coronavirus Disease-2019 pandemic: A perspective from the National Cancer Institute's PROSPR consortium. Gasteroenterology. 2021;160(4):999–1002. doi: 10.1053/j.gastro.2020.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benjamini Y., Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Statist Soc B Methodol. 1995;57(1):289–300. [Google Scholar]
- 9.Rivera M.P., Katki H.A., Tanner N.T. Addressing disparities in lung cancer screening eligibility and healthcare access. Am J Respir Crit Care Med. 2020;202(7):e97–e112. doi: 10.1164/rccm.202008-3053ST. [DOI] [PMC free article] [PubMed] [Google Scholar]