Abstract
Context
The COVID-19 pandemic resulted in visitation restrictions across most health care settings, necessitating the use of remote communication to facilitate communication among families, patients and health care teams.
Objective
To examine the impact of remote communication on families’ evaluation of end-of-life care during the COVID-19 pandemic.
Methods
Retrospective, cross-sectional, mixed methods study using data from an after-death survey administered from March 17–June 30, 2020. The primary outcome was the next of kin's global assessment of care during the Veteran's last month of life.
Results
Data were obtained from the next-of-kin of 328 Veterans who died in an inpatient unit (i.e., acute care, intensive care, nursing home, hospice units) in one of 37 VA medical centers with the highest numbers of COVID-19 cases. The adjusted percentage of bereaved families reporting excellent overall end-of-life care was statistically significantly higher among those reporting Very Effective remote communication compared to those reporting that remote communication was Mostly, Somewhat, or Not at All Effective (69.5% vs. 35.7%). Similar differences were observed in evaluations of remote communication effectiveness with the health care team. Overall, 81.3% of family members who offered positive comments about communication with either the Veteran or the health care team reported excellent overall end-of-life care vs. 28.4% who made negative comments.
Conclusions
Effective remote communication with the patient and the health care team was associated with significantly better ratings of the overall experience of end-of-life care by bereaved family members. Our findings offer timely insights into the importance of remote communication strategies.
Key Words: Communication, end-of-life care, COVID-19, quality improvement
Background
The COVID-19 pandemic has radically altered the delivery of health care, especially care at the end-of-life (EOL). One critical change is around visitation policies. To minimize infection transmission, most health care facilities have greatly curtailed in-person visits from family, banning all visitation except for “compassionate care situations.”1 These restrictions increase a sense of isolation and distress for families, patients, and staff and can have significant consequences including complicated grief reactions for patients’ families.2 , 3
Open communication is a hallmark of high-quality palliative and EOL care. Current limitations on in-person interaction among patients, families, and health care providers necessitates increased use of alternative communication approaches. To implement these approaches, clinicians may turn to existing guidelines for enhancing remote communication in health care settings during natural disasters, including pandemics.4, 5, 6, 7, 8 However, little is known about their effectiveness in promoting positive patient and family outcomes.
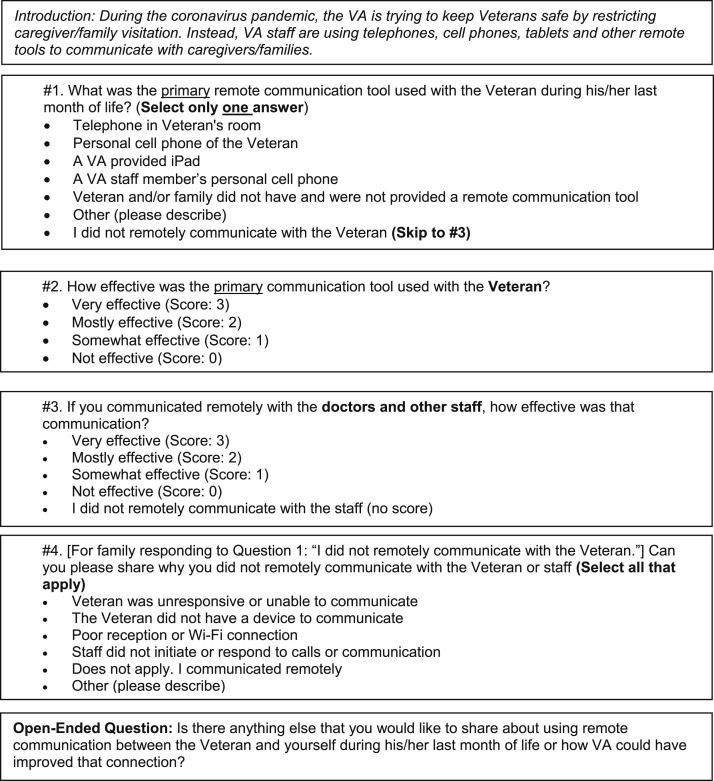
The COVID-19 pandemic provides an opportunity to examine the effects of remote health care communication. The Department of Veterans Affairs (VA), the largest integrated health care system in the United States, is an excellent setting for examining challenges created by COVID-19. On March 17, 2020, the VA implemented a “no visitation” policy for all VA medical centers to protect the most vulnerable Veterans from contracting COVID-19. Families were permitted in-person visitation whenever possible when the Veteran was identified as imminently dying. As the numbers of COVID-19-related hospitalizations and deaths grew, the national VA Palliative and Hospice Care program began an effort to understand the impact of the pandemic on bereaved families’ experiences and evaluations of EOL care. Starting with deaths occurring in March 2020, three temporary COVID-19-related items—two forced-choice and one open-ended question—were added to the Bereaved Family Survey (BFS), an after-death survey used to assess and improve the quality of care for all seriously ill Veterans across the VA with a focus on the last month of life. The questions focused on the use and effectiveness of remote communication tools during COVID-19. Beginning with May 2020 deaths, two additional questions related to remote communication were added to the survey. The first asked respondents about the effectiveness of communication between the family and the health care team and the second asked respondents who had no remote contact with the Veteran or health care team to state a reason for the lack of contact (Appendix Figure I).
Appendix Figure I.
COVID-19–specific questions about communication.
Applying a convergent parallel mixed methods design, we integrated quantitative and qualitative BFS data with clinical and administrative data to address the following question: What impact does remote communication have on families' evaluations of care in the last month of life for Veterans dying in inpatient settings during the COVID-19 visitation restrictions? Specifically, we examined the associations among bereaved families’ perceptions of the quality of remote communication with 1) the Veteran and 2) the health care team and their evaluations of the quality of end-of-life care.
Methods
Data Sources and Procedures
Data for this retrospective observational analysis were derived from two sources: 1) The VA Corporate Data Warehouse (CDW), which contains patient clinical and administrative information from a variety of sources, and 2) the BFS, a postdeath survey that is routinely administered to the next of kin of Veterans who die in VA inpatient settings, including acute care units, intensive care units, community living centers (i.e., VA nursing homes), and hospice units, most of which are located in a nursing home unit. Four to six weeks after the Veteran's death, next-of-kin are contacted and asked to complete the BFS by mail, telephone, or online. The BFS has demonstrated validity and reliability and is endorsed by the National Quality Forum.9, 10, 11, 12, 13, 14 There is also evidence of measurement invariance across all three administration modalities.10
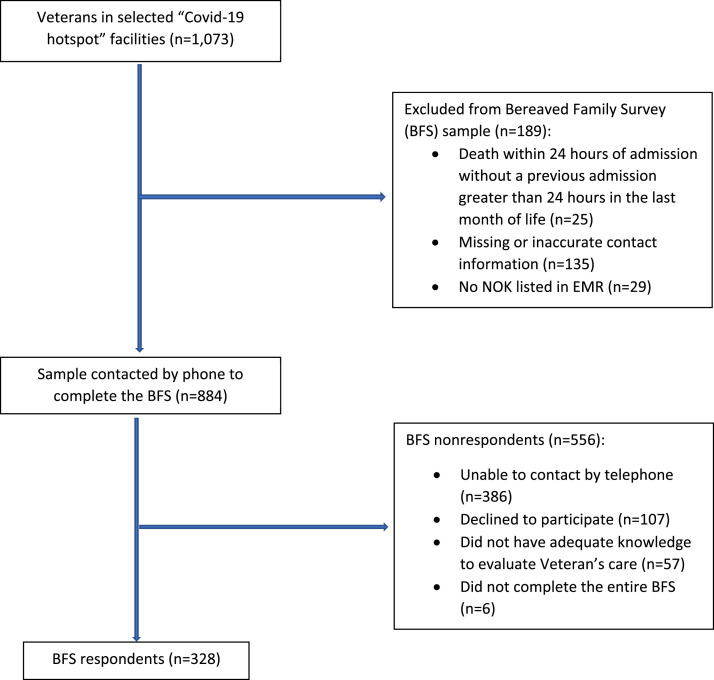
For this analysis, the next-of-kin of 1073 Veterans who died from March 17, 2020, to June 30, 2020 were selected from facilities with the highest numbers of COVID cases to receive the BFS with additional COVID-19–related questions. Specific COVID-19 “hotspot” facilities were identified through the VA COVID National Summary website, which reports the number of Veterans served by the facility who were diagnosed with COVID-19.15 Each month, this website was accessed to identify the VA medical centers with the highest numbers of COVID-19 cases. A programmer then identified deaths at each of the facilities, starting with the facility with the highest number of COVID-19 cases, and proceeding down the facility list until 400 deaths were identified. This number was chosen based on staff's capacity to contact next-of-kin by phone to complete the BFS. The facility list changed from month to month but included deaths from 12 to 14 facilities per month, for a total of 37 facilities over the study period. These facilities were located in 19 states and the District of Columbia. Consistent with patterns in COVID-19 prevalence during this period, some facilities (e.g., New York City) were included every month, whereas others (e.g., Houston, Las Vegas) were included only in the later months.
The COVID-19 sample received the BFS by phone to maximize timely data collection. The survey was administered by experienced, trained interviewers. Attempts to contact next-of-kin were made up to three times including at least one attempt after business hours. A total of 328 surveys were completed (37.1% response rate). Appendix Figure II depicts the recruitment flow diagram.
Appendix Figure II.
Recruitment flow diagram.
All data collection and analyses were conducted as part of ongoing quality improvement efforts at the Department of Veterans Affairs. As such, this analysis was reviewed and received approval as “exempt” by the Institutional Review Board at the Corporal Michael J. Crescenz VA Medical Center in Philadelphia, PA.
Study Variables
Dependent Variables: Bereaved families’ Evaluation of Care
Our primary outcome was the BFS Performance Measure (BFS-PM) which is the next-of-kin's global assessment of care during the Veteran's last month of life (ranging from 0 = “poor” to 4 = “excellent”).
Our secondary outcomes were two additional BFS items that reflect the family member's evaluation of specific aspects of communication: During his/her last month of life, 1) how much of the time were the staff who took care of him/her willing to take time to listen; and 2) how often did the staff who took care of him/her keep you or other family members informed about his/her condition and treatment? Possible responses to these items are: Always, Usually, Sometimes, Never, and I did not speak with the staff who took care of him/Unsure.
For all three dependent variables, we used a top-box scoring method, comparing the most favorable response (i.e., Excellent or Always) to all other responses. To reclaim cases with missing BFS item-level data, we used ICE imputation procedures in STATA because of the small sample size.16 Overall, 1% (n = 3) of responses were imputed.
Independent Variables: Measures of Remote Communication Effectiveness
Our key measures of remote communication effectiveness were derived from two forced-choice items (Appendix Figure I). Respondents were asked to report the effectiveness of the primary remote communication tool used with the Veteran (e.g., telephone in the Veteran's room, personal iPad/tablet, VA-provided iPad/tablet) and with the staff using four options: Very, Mostly, Somewhat, or Not at All Effective.
As an additional measure of communication effectiveness, we analyzed communication-specific responses from two standard, open-ended questions on the BFS: Is there anything else that you would like to share about the Veteran's care during his/her last month of life? and, Is there anything else that you would like to share about how the care could have been improved for the Veteran? The COVID-19 version included the additional question: Is there anything else that you would like to share about using remote communication between the Veteran and yourself during his/her last month of life or how VA could have improved that connection? Because all surveys for this study were completed by phone, interviewers asked each question in sequence, taking extensive notes while the family member answered. These notes were then read back to the respondent, who verified their accuracy or offered corrections or clarification.
To transform the qualitative responses into data for the quantitative analyses,17 we compiled all comments into a spreadsheet, with one row per respondent and three columns, each containing a response, if available, for each of the three questions. A detailed description of the comprehensive qualitative analysis is reported elsewhere.18 For this analysis, our goal was to examine the association between communication and perceptions of quality of end-of-life care. Directed content analysis with deductive open coding was used to identify conceptual categories along two matrices: focus and valence.19 , 20 Coders analyzed data from all three questions using a priori rules. Comments were coded according to focus, specifically, contextual (i.e., relating to any aspect of care that was not specific to the quality of communication) and communication-specific. The latter were identified using keywords such as “talked,” “informed/information,” “meeting/met,” as well as terms focused on remote communication (e.g., “iPad,” “phoned,” “video chat”). Then, we assigned a valence to each communication-specific coded comment: 1) positive; 2) negative; 3) both positive and negative (i.e., comments included both negative and positive elements); or 4) not applicable (no comments or comments were not explicitly positive or negative, e.g., “we were not allowed in”). This step allowed us to assign values to the qualitative data for purposes of our quantitative analysis.17 Two authors (M.E. and H.G.) independently coded all data, achieving 86% agreement on determination of codes. They then met to discuss all discrepancies and reach consensus on final coding. Table 1 provides examples of communication-specific coded statements according to assigned valences.
Table 1.
Examples of Communication-specific Comments Coded by Valance
| Positive |
|
| Negative |
|
| Neutral |
|
Covariates
We extracted Veterans’ clinical and demographic data including age, race/ethnicity and an indicator as to whether the Veteran had a diagnosis of COVID-19. We measured medical comorbidities using the Elixhauser method with a one-year look back period.21 , 22 We also collected data on site of death and four care process indicators that are associated with high-quality EOL care: 1) receipt of a comprehensive palliative care consult in the last 90 days of life;23 2) completion of a life-sustaining treatment note and orders;24 , 25 3) Veteran/family contact with a chaplain in the last month of life; and 4) presence of a “Do Not Resuscitate” order.26 , 27 All indicators were coded as dichotomous variables (yes/no).
Statistical Analysis
We calculated descriptive statistics to examine demographic and clinical characteristics of the sample. To examine the associations between remote communication effectiveness variables and BFS outcomes, we calculated adjusted proportions and odds ratios using robust logistic and linear regression models clustered by facility. Models were adjusted for age (continuous), COVID-19 diagnosis (yes/no), race (non-Hispanic white vs. other), next-of-kin relationship (spouse/partner; child; other), site of death (ICU, acute care, VA nursing home, hospice palliative care unit), palliative care consult (yes/no), and chaplain visit/contact (yes/no). We did not include life-sustaining treatment note and orders and the Do Not Resuscitate variables in the models because most decedents had both. Owing to known differences between BFS responders and nonresponders in factors such as age, race/ethnicity, venue of death, and receipt of EOL care processes, including a palliative care consult, we included inverse propensity weights in our adjusted models to statistically account for nonresponse (Table 2 ).13 We also calculated the percentage of “top box” responses for BFS outcomes according to valence of the coded qualitative comments: positive, negative, both positive and negative, no comment/neutral comment. We used STATA statistical software version 15.1 (StataCorp., College Station, TX) for all analyses. Statistical significance was set at P < 0.05 for all analyses.
Table 2.
Sample Demographic and Process Measures
| Patient Characteristic/Process Measure | Overall Sample, N = 328 |
BFS Responders, N = 328 |
BFS Nonresponders, N = 556 |
P value | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Age: mean years (SD) | 77 (11.4) | 77 (11.4) | 75 (11.5) | 0.104 | |||
| Male gender | 316 | 96.3 | 316 | 96.3 | 537 | 96.6 | 0.775 |
| Race/Ethnicity | 0.884 | ||||||
| Non-Hispanic White | 153 | 46.7 | 153 | 46.7 | 256 | 46.0 | |
| All other race/ethnicity | 167 | 50.9 | 167 | 50.9 | 293 | 52.7 | |
| Unknown | 8 | 2.4 | 8 | 2.4 | 7 | 1.3 | |
| Next of Kin Relationship | 0.001 | ||||||
| Spouse/partner | 113 | 34.5 | 113 | 34.5 | 173 | 31.1 | |
| Child | 116 | 35.4 | 116 | 35.4 | 171 | 30.8 | |
| All other | 99 | 30.0 | 99 | 30.0 | 209 | 37.6 | |
| COVID-19 diagnosis | 132 | 40.4 | 132 | 40.4 | 196 | 35.3 | 0.128 |
| Number of comorbid conditions: mean (SD) | 5.8 (2.9) | 5.8 (2.9) | 5.8 (3.0) | 0.832 | |||
| Venue of Death | 0.004 | ||||||
| ICU | 122 | 37.2 | 122 | 37.2 | 250 | 45.0 | |
| Acute | 93 | 28.4 | 93 | 28.4 | 158 | 28.4 | |
| CLC | 46 | 14.0 | 46 | 14.0 | 56 | 10.1 | |
| HPCU | 67 | 20.4 | 67 | 20.4 | 92 | 16.6 | |
| Completed LST Note/Order | 309 | 94.2 | 309 | 94.2 | 494 | 88.9 | 0.005 |
| DNR order completed (from LST Order) | 284 | 86.6 | 284 | 86.6 | 445 | 80.0 | 0.002 |
| Received Palliative Care Consult | 209 | 63.7 | 209 | 63.7 | 294 | 52.9 | <.001 |
| Received Chaplain Contact | 247 | 75.3 | 247 | 75.3 | 386 | 69.4 | 0.008 |
CLC = Community Living Center; DNR = Do Not Resuscitate; HPCU = Hospice/Palliative Care Unit; ICU = Intensive Care Unit; LST = Life Sustaining Treatment.
Results
The final sample included 328 decedents, with an average age of 76 years (standard deviation [SD]: 11.4); 96% were male, and 46.7% were white, non-Hispanic. Forty percent had a COVID-19 diagnosis, reflecting the focus on pandemic “hotspots.” Almost two-thirds (65.6%) of the sample died in an intensive care or other acute care unit, whereas the other third (34%) died in a VA nursing home or hospice-palliative care unit. The vast majority had a completed life-sustaining treatment note and orders (94.2%) in which 86.6% contained a Do Not Resuscitate order. Table 2 summarizes the sample characteristics.
While most (74%) respondents reported either in-person or remote communication with the Veteran in the last month of life, 86 family members (26%) stated they had no remote contact. Of the 40 respondents who were specifically asked to provide a reason for no contact, over half (n = 22) stated that they had no remote contact because they were able to see the Veteran in person (Per VA policy, family visitors were allowed visitation if death was expected.), and seven (17.5%) stated the Veteran did not want contact or was unable to communicate. Only 14 of the 195 (7%) family members who were asked about contact with the health care team stated that they had no contact with providers or staff.
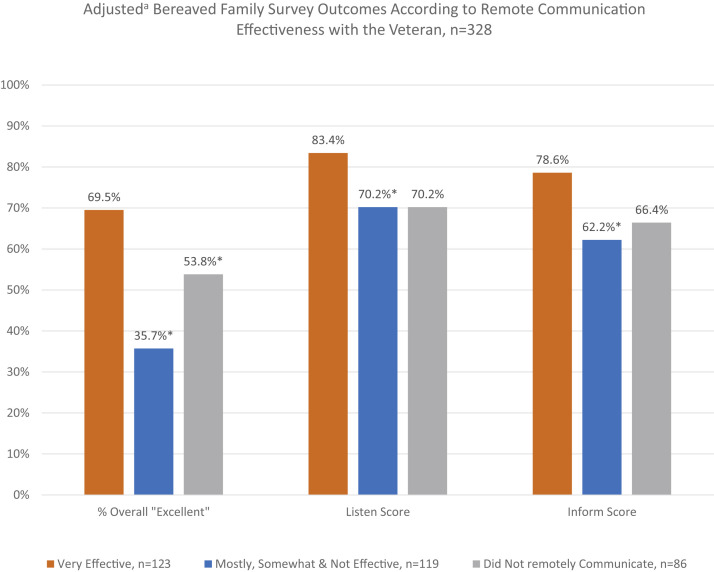
Figure 1 depicts the adjusted proportions of each BFS outcome by remote communication effectiveness with the Veteran. BFS-PM for respondents in each category were as follows: Very Effective was (69.5%); Mostly, Somewhat, or Not at All Effective (35.7%); and Did not Remotely Communicate with the Veteran (53.8%). The differences in BFS-PM between Very Effective and the other two categories were statistically significant. The difference between Mostly, Somewhat, or Not at All Effective and Did not Remotely Communicate with the Veteran also was significant (OR = 1.89; 95% confidence interval [CI] = 1.08–3.29; P = 0.011).
Fig. 1.
Bereaved Family Survey Outcomes Associated with Remote Communication Effectiveness with the Veteran, n = 328. aAll comparisons adjusted for patient age, patient race/ethnicity, Elixhauser comorbidity, COVID-19 Diagnosis, next-of-kin relationship, palliative care consult in the last 90 days of life, chaplain, contact with the family or Veteran during the last month of life, venue of inpatient death, nonresponse bias and clustered by facility. Overall “Excellent” Score = Proportion of family members that rated care at the EOL as “Excellent” vs."Very good”, “Good”, “Fair” or “Poor”. Listen Score: Proportion of family members who reported Staff “Always” listened to the Veteran and family vs.“Usually”, “Sometimes” or “Never” listened. Inform Score: Proportion of family members who reported Staff “Always” kept the Veteran and family informed about the Veteran's condition and treatment vs. “Usually”, “Sometimes” or “Never” kept the Veteran and family informed. ∗Difference with reference group (Very Effective) statistically significant at P < 0.05.
Similar patterns were seen for the BFS staff listened and Kept family informed outcomes. The adjusted odds ratio (AOR) for the BFS-PM, comparing families who rated the remote communication as Very Effective vs. Mostly/Somewhat/Not At All Effective was 4.68 (95% CI: 2.27–9.65) indicating that families who responded that communication with the Veteran was Very Effective were almost 4.7 times more likely to report that the quality of EOL care was Excellent than families who rated remote communication effectiveness less favorably. Families who reported that communication with the Veteran was Very Effective were almost twice as likely to report an excellent overall rating on the BFS-PM compared with family members who did not remotely communicate with the Veteran (AOR: 1.89; 95% CI: 1.08–3.29).
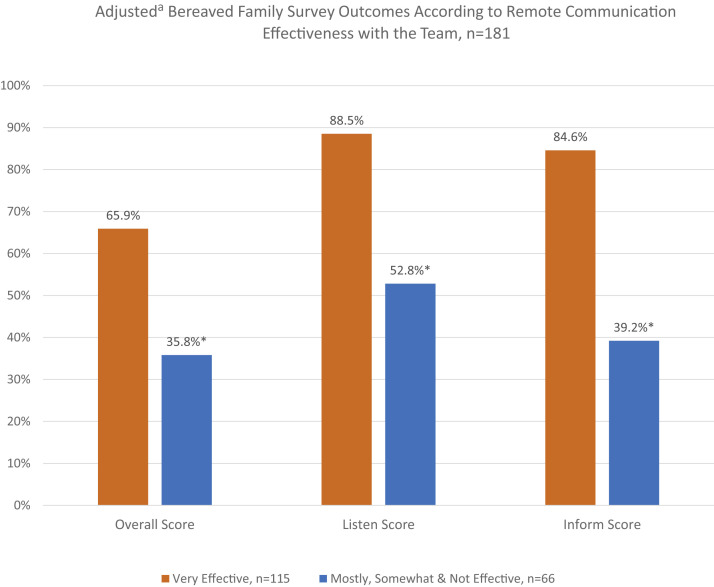
Figure 2 shows the adjusted proportions of each BFS outcome by remote communication effectiveness with the health care team. The likelihood of family members with the most favorable views of remote communication effectiveness (i.e., Very Effective) to report the overall care as Excellent was nearly four times higher than families with less favorable views of family/health care team remote communication (AOR: 3.74; 95% CI: 1.27–10.99). Statistically significant differences were also seen when comparing Very Effective vs. Mostly, Somewhat and Not Effective remote communication for the Staff Listens and Staff Kept Us Informed outcomes.
Fig. 2.
Bereaved Family Survey Outcomes Associated with Remote Communication Effectiveness with the Health care Team, n = 181. aAdjusted for patient age, patient race/ethnicity, Elixhauser comorbidity, COVID Diagnosis, next-of-kin relationship, palliative care consult in the last 90 days of life, chaplain contact with the family or Veteran during the last month of life, venue of inpatient death, nonresponse bias and clustered by facility. Overall Score: Proportion of family members that rated care at the EOL as “Excellent” vs. “Very good”, “Good”, “Fair” or “Poor”. Listen Score: Proportion of family members who reported Staff “Always” listened to the Veteran and family vs. “Usually”, “Sometimes” or “Never” listened. Inform Score: Proportion of family members who reported Staff “Always” kept the Veteran and family informed about the Veteran's condition and treatment vs. “Usually”, “Sometimes” or “Never” kept the Veteran and family informed. ∗Difference with reference group (Very Effective) statistically significant at P < 0.05.
Analysis of the qualitative data revealed that positive and negative reports about communication were highly associated with family ratings of care (Table 3 ). Overall, 81.3% of family members who offered positive comments about communication with either the Veteran or the health care team rated care at the EOL as Excellent vs. 28.4% who made negative comments and 50.0% of those who had mixed (negative and positive) reports about communication. Similar patterns were found for Staff listens and Staff kept family informed.
Table 3.
Association Among Negative and Positive Communication-specific Comments and Outcomes, N = 301
| Valence | N | % | Overall Quality of Care % Excellent | Staff Listened % Always | Staff Kept Family Informed % Always |
|---|---|---|---|---|---|
| Positive | 48 | 15.9 | 81.3 | 89.6 | 89.4 |
| Negative | 86 | 28.6 | 28.4 | 52.9 | 45.3 |
| Positive and Negative | 24 | 8.0 | 50.0 | 78.3 | 62.5 |
| No comment/Neutral comment | 143 | 47.5 | 57.8 | 79.7 | 71.1 |
Discussion
Results of this study support the importance of communication, particularly remote communication, among family, patients, and health care teams during periods of restricted visitation resulting from the COVID-19 pandemic. We found that family reports of effective remote communication with the patient and the health care team were associated with significantly better family experiences of EOL care. Overall evaluation of EOL care, as well as communication-specific aspects of care (health care team listens and kept family informed) were more highly rated when bereaved families reported that communication with the patient and/or the health care team was very effective. Findings were similar when family members offered positive open-ended responses to questions about their communication experiences at the patient's EOL. To our knowledge, this study is the first to examine the associations between bereaved families' experiences of communication—in particular, remote communication—and EOL care during the COVID-19 pandemic.
It is possible that families' general views of EOL care quality influenced their ratings of remote communication, rather than effective remote communication driving families' perception of overall care. However, numerous studies document the importance that patients and families place on communication at the EOL.10 , 28, 29, 30, 31 For this reason, the BFS and other measures of patients' and families' experience of EOL care include items that directly assess communication.28 , 32 , 33 Thus, we believe that families’ experience of remote communication at EOL influenced their rating of overall care, although we are unable to demonstrate this directionality empirically in our analyses.
Our findings lend empirical support for the guidance that the health care team optimize communication with families during COVID-19 and other times of restrictions on in-person visits.4 , 34, 35, 36 The effectiveness of specific recommendations, however, such as the use of video conferencing when possible, asynchronous communication, or providing families with information about low-cost internet options, remains unknown. Both quantitative and qualitative findings from our study suggest that families highly value regular communication about the patient's status, a priority that has been identified by other investigators.37 Nonetheless, the content and quality of the communication when families are physically distant is unclear. Is there information that is particularly important to convey under these circumstances? For example, a common comment among respondents was to express distress at the thought of the Veteran “dying alone” without family present. Given well-documented challenges in predicting mortality,38 it is likely that opportunities to facilitate in-person visits for patients who are identified as imminently dying will be missed. Thus, remote communication with all seriously ill patients is critical. Relatedly, a few families conveyed relief and appreciation when staff communicated that the patient was not alone. Future research should examine the preferences and effectiveness of specific strategies to promote remote communication among patients, families, and the health care team.
Qualitative comments reflected characteristics of less-than-ideal remote communication that have been found in other studies.39 , 40 For example, some family members expressed frustration when staff were unavailable to facilitate phone or video calls with patients who were too weak or confused to manage the technology independently. Others found the technology difficult to navigate or encountered connectivity and other problems.41 , 42 These challenges were likely more pronounced among families in rural areas, where broadband internet connection is sometimes unavailable,43 and for people with low literacy or digital literacy skills, and those with vision or hearing loss.44 Addressing these particular barriers is critical to achieving high quality care.
Interestingly, we found that families who reported having no remote contact with the Veteran rated the quality of EOL care significantly higher than those who described less than very effective remote communication. The explanation for this finding is not clear; however, over half of respondents (22/40) who were asked to provide a reason for not using remote communication reported that they were able to visit the patient, making remote communication options less necessary. Furthermore, many in the sample were not asked to state a reason for the lack of remote communication with the Veterans as this question was added later; thus, this number is likely an undercount of families who were permitted in-person visits, thereby eliminating the need for remote communication. Overall, this finding suggests that facilitating in-person visitation whenever possible is important. However, our findings also show that meaningful, comforting communication can occur without in-person contact. This observation is consistent with Otani et al., who found that the patient's inability to say goodbye before death was more highly associated with complicated grief than the family's inability to see the patient in person prior to death.2
There are several limitations to this study, including the response rate of 37%. Although lower than we expected, this rate is comparable to that of the Consumer Assessment of Healthcare Providers and Systems-Hospice survey.45 Furthermore, we adjusted our analyses for nonresponse bias.13 Veterans comprise a unique, mostly male population; on the other hand, we were able to survey a diverse group of families from geographic locations and care settings. Also, while the BFS is a validated measure, the questions that were added to understand remote communication were not formally tested or validated. In addition, the data were collected for quality improvement rather than research. Thus, we were unable to audio record the interviews and transcribe verbatim as would be the case in a research study. Trained experienced staff conducted all interviews, wrote down respondent's comments, and read them back to respondents to check for accuracy; however, there was no independent evaluation that written responses were accurate or complete. Furthermore, interviewers did not ask follow-up questions to probe into the strengths and challenges of specific modes of communication (e.g., video chat, phone).
Our findings offer timely and critical insights about attending to remote communication with patients, their families, and health care teams. There are opportunities to improve virtual communications and expand the use of health care system-provided communication devices. Additional research is needed to identify the most effective and preferred modalities, frequency, content and messaging to promote high-quality EOL care. Families are experiencing distress as a result of visitation policies, but it appears this stress can be mitigated to some degree by effective communication. What we observed offers important lessons for EOL communication during the current pandemic, future pandemics, and other disasters, as well as in situations when families lack the resources or ability to be physically present.
Disclosures and Acknowledgments
The authors would like to thank our three expert interviewers, Shirley Binner, Daisy Enck, and Charlotte Peffley, whose dedication to our nation's Veterans inspire us every day.
The analysis described here is based on work supported by the Department of Veterans Affairs, Veterans Health Administration, which had no role in the design, methods, participant recruitment, data collection, analysis, or preparation of this article or in the decision to submit this article for publication. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the U.S. Government.
Appendix
References
- 1.Centers for Medicare and Medicaid Services Frequently asked questions on nursing home visitation. 2020. https://www.cms.gov/files/document/covid-visitation-nursing-home-residents.pdf Available from.
- 2.Otani H., Yoshida S., Morita T. Meaningful communication before death, but not present at the time of death itself, is associated with better outcomes on measures of depression and complicated grief among bereaved family members of cancer patients. J Pain Symptom Manage. 2017;54:273–279. doi: 10.1016/j.jpainsymman.2017.07.010. [DOI] [PubMed] [Google Scholar]
- 3.Strang P., Bergstrom J., Martinsson L., Lundstrom S. Dying from COVID-19: Loneliness, end-of-life discussions, and support for patients and their families in nursing homes and hospitals. A national register study. J Pain Symptom Manage. 2020;60:e2–e13. doi: 10.1016/j.jpainsymman.2020.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davidson J.E., Aslakson R.A., Long A.C. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45:103–128. doi: 10.1097/CCM.0000000000002169. [DOI] [PubMed] [Google Scholar]
- 5.Thomas J.D., Leiter R.E., Abrahm J.L. Development of a palliative care Toolkit for the COVID-19 pandemic. J Pain Symptom Manage. 2020;60:e22–e25. doi: 10.1016/j.jpainsymman.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Janssen D.J.A., Ekstrom M., Currow D.C. COVID-19: guidance on palliative care from a European Respiratory Society international task force. Eur Respir J. 2020;56:2002583. doi: 10.1183/13993003.02583-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chua I.S., Jackson V., Kamdar M. Webside manner during the COVID-19 pandemic: Maintaining human connection during virtual Visits. J Palliat Med. 2020;23:1507–1509. doi: 10.1089/jpm.2020.0298. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Department of Health and Human Services Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency. 2020. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html Available from.
- 9.Smith D., Caragian N., Kazlo E. Can we make reports of end-of-life care quality more consumer-focused? results of a nationwide quality measurement program. J Palliat Med. 2011;14:301–307. doi: 10.1089/jpm.2010.0321. [DOI] [PubMed] [Google Scholar]
- 10.Thorpe J.M., Smith D., Kuzla N., Scott L., Ersek M. Does mode of survey administration matter? Using measurement invariance to validate the mail and telephone versions of the Bereaved Family Survey. J Pain Symptom Manage. 2016;51:546–556. doi: 10.1016/j.jpainsymman.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 11.National Quality Forum . NQF; Washington DC: 2012. Performance measurement coordination strategy for hospice and palliative care: Final report. [Google Scholar]
- 12.Kutney-Lee A., Carpenter J., Smith D. Case-mix adjustment of the bereaved family survey. Am J Hosp Palliat Care. 2018;35:1015–1022. doi: 10.1177/1049909117752669. [DOI] [PubMed] [Google Scholar]
- 13.Smith D., Kuzla N., Thorpe J., Scott L., Ersek M. Exploring nonresponse bias in the Department of veterans Affairs' bereaved family survey. J Palliat Med. 2015;18:858–864. doi: 10.1089/jpm.2015.0050. [DOI] [PubMed] [Google Scholar]
- 14.Veteran Experience Center Bereaved family survey: description and methods. https://www.cherp.research.va.gov/PROMISE/vecmethods.asp Available from.
- 15.Department of Veterans Affairs COVID-19 National Summary. 2020. https://www.accesstocare.va.gov/Healthcare/COVID19NationalSummary Available from.
- 16.Royston P. ICE: Stata module for multiple imputation of missing values," Statistical Software Components S446602, Boston Coll Department Econ. https://ideas.repec.org/c/boc/bocode/s446602.html originally published 2006, revised 25 Oct 2014. Available from.
- 17.Guest G., MacQueen K., Namey E. Applied Thematic Analysis. SAGE Publications, Inc.; Thousand Oaks: 2014. Data reduction techniques. [Google Scholar]
- 18.Feder S., Smith D., Griffin H. "Why couldn't I go in to see him?" Bereaved families' perceptions of end-of-life communication during COVID-19. J Am Geriatr Soc. 2020 doi: 10.1111/jgs.16993. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hsieh H.F., Shannon S.E. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 20.Elo S., Kyngas H. The qualitative content analysis process. J Adv Nurs. 2008;62:107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- 21.Elixhauser A., Steiner C., Harris D.R., Coffey R.M. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 22.van Walraven C., Austin P.C., Jennings A., Quan H., Forster A.J. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47:626–633. doi: 10.1097/MLR.0b013e31819432e5. [DOI] [PubMed] [Google Scholar]
- 23.Carpenter J.G., McDarby M., Smith D. Associations between timing of palliative care consults and family evaluation of care for veterans who die in a hospice/palliative care unit. J Palliat Med. 2017;20:745–751. doi: 10.1089/jpm.2016.0477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levy C., Ersek M., Scott W. Life-Sustaining Treatment Decisions Initiative: Early implementation results of a national Veterans Affairs program to honor veterans' care preferences. J Gen Intern Med. 2020;35:1803–1812. doi: 10.1007/s11606-020-05697-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Foglia M.B., Lowery J., Sharpe V.A., Tompkins P., Fox E. A comprehensive approach to eliciting, documenting, and honoring patient wishes for care near the end of life: the Veterans Health Administration's Life-Sustaining Treatment Decisions Initiative. Jt Comm J Qual Patient Saf. 2019;45:47–56. doi: 10.1016/j.jcjq.2018.04.007. [DOI] [PubMed] [Google Scholar]
- 26.Ersek M., Thorpe J., Kim H., Thomasson A., Smith D. Exploring end-of-life care in Veterans Affairs community living centers. J Am Geriatr Soc. 2015;63:644–650. doi: 10.1111/jgs.13348. [DOI] [PubMed] [Google Scholar]
- 27.Wachterman M.W., Pilver C., Smith D. Quality of end-of-life care provided to patients with different serious illnesses. JAMA Intern Med. 2016;176:1095–1102. doi: 10.1001/jamainternmed.2016.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anhang Price R., Stucky B., Parast L. Development of valid and reliable measures of patient and family experiences of hospice care for public reporting. J Palliat Med. 2018;21:924–932. doi: 10.1089/jpm.2017.0594. [DOI] [PubMed] [Google Scholar]
- 29.Virdun C., Luckett T., Davidson P.M., Phillips J. Dying in the hospital setting: a systematic review of quantitative studies identifying the elements of end-of-life care that patients and their families rank as being most important. Palliat Med. 2015;29:774–796. doi: 10.1177/0269216315583032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Teno J.M., Clarridge B.R., Casey V. Family perspectives on end-of-life care at the last place of care. JAMA. 2004;291:88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 31.Steinhauser K.E., Christakis N.A., Clipp E.C. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284:2476–2482. doi: 10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]
- 32.Casarett D., Shreve S., Luhrs C. Measuring families' perceptions of care across a health care system: preliminary experience with the Family Assessment of Treatment at End of Life Short form (FATE-S) J Pain Symptom Manage. 2010;40:801–809. doi: 10.1016/j.jpainsymman.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 33.Teno J.M., Clarridge B., Casey V., Edgman-Levitan S., Fowler J. Validation of Toolkit after-death bereaved family member interview. J Pain Symptom Manage. 2001;22:752–758. doi: 10.1016/s0885-3924(01)00331-1. [DOI] [PubMed] [Google Scholar]
- 34.Hart J.L., Turnbull A.E., Oppenheim I.M., Courtright K.R. Family-centered care during the COVID-19 era. J Pain Symptom Manage. 2020;60:e93–e97. doi: 10.1016/j.jpainsymman.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Akgun K.M., Shamas T.L., Feder S.L., Schulman-Green D. Communication strategies to mitigate fear and suffering among COVID-19 patients isolated in the ICU and their families. Heart Lung. 2020;49:344–345. doi: 10.1016/j.hrtlng.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Houchens N., Tipirneni R. Compassionate communication amid the COVID-19 pandemic. J Hosp Med. 2020;15:437–439. doi: 10.12788/jhm.3472. [DOI] [PubMed] [Google Scholar]
- 37.Rhodes R.L., Mitchell S.L., Miller S.C., Connor S.R., Teno J.M. Bereaved family members' evaluation of hospice care: what factors influence overall satisfaction with services? J Pain Symptom Manage. 2008;35:365–371. doi: 10.1016/j.jpainsymman.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 38.Chu C., White N., Stone P. Prognostication in palliative care. Clin Med (Lond) 2019;19:306–310. doi: 10.7861/clinmedicine.19-4-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lau J., Knudsen J., Jackson H. Staying connected in the COVID-19 pandemic: telehealth at the largest safety-net system in the United States. Health Aff (Millwood) 2020;39:1437–1442. doi: 10.1377/hlthaff.2020.00903. [DOI] [PubMed] [Google Scholar]
- 40.Steindal S.A., Nes A.A.G., Godskesen T.E. Patients' experiences of telehealth in palliative home care: Scoping review. J Med Internet Res. 2020;22:e16218. doi: 10.2196/16218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jess M., Timm H., Dieperink K.B. Video consultations in palliative care: a systematic integrative review. Palliat Med. 2019;33:942–958. doi: 10.1177/0269216319854938. [DOI] [PubMed] [Google Scholar]
- 42.Tieman J.J., Swetenham K., Morgan D.D., To T.H., Currow D.C. Using telehealth to support end of life care in the community: a feasibility study. BMC Palliat Care. 2016;15:94. doi: 10.1186/s12904-016-0167-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Perrin A. Digital gap between rural and nonrural America persists. 2019. https://www.pewresearch.org/fact-tank/2019/05/31/digi Available from.
- 44.World Health Organization WHO guideline recommendationson digital interventions for health system strengthening. 2019. https://apps.who.int/iris/handle/10665/311941 Available from. [PubMed]
- 45.Parast L., Elliott M.N., Hambarsoomian K., Teno J., Anhang Price R. Effects of survey mode on consumer assessment of healthcare providers and systems (CAHPS) hospice survey scores. J Am Geriatr Soc. 2018;66:546–552. doi: 10.1111/jgs.15265. [DOI] [PubMed] [Google Scholar]