Abstract
Objective:
Adult research supports the efficacy of targeting the malleable risk factor of anxiety sensitivity (AS) in preventing anxiety and related psychopathology. However, very little work has evaluated the impact of AS reduction among youth, which is unfortunate given adolescence is a “core risk” period in terms of disorder onset.
Method:
The primary project aim was to test the effects of an Anxiety Sensitivity Amelioration Program for Youth (ASAP-Y) among a sample of 88 youth aged 10-14 years with elevated AS. High AS youth and a parent were randomly assigned to either the ASAP-Y, which consisted of psychoeducation and experimenter-led and parent-led exposures, or a general health information control condition.
Results:
Youth AS levels in both conditions decreased from baseline to the one-month assessment, but this decrease was more pronounced at one-month for youth in the intervention condition. Further, significant indirect effects of condition on one-month anxiety and depression symptoms via reduced AS were detected. Homework compliance rates and self-report data support the acceptability of the ASAP-Y. Contrary to hypotheses, differences between conditions in emotional reactivity elicited using experimental psychopathology methods were not observed.
Conclusions:
The current findings offer preliminary support for the ASAP-Y as an acceptable selective preventive intervention for at-risk youth, with specific anxiety- and depression-related effects through reduced AS.
Keywords: anxiety sensitivity, anxiety, depression, preventive intervention, prevention, youth
Adolescence marks an important period in terms of psychological vulnerability (Dahl, 2004). Several disorders, such as anxiety and depression, emerge during the course of adolescence (Beardslee, Chien, & Bell, 2011; Kessler et al., 2012). These conditions negatively impact functioning and physical health, increase risk for other forms of psychopathology, and have a lasting impact for many youth into their adult lives (Ames & Leadbeater, 2018; Copeland, Angold, Shanahan, & Costello, 2014). These outcomes underscore the importance of developing evidence-based prevention strategies before and during the critical period of adolescence.
Anxiety sensitivity (AS) is a malleable cognitive risk factor that reflects beliefs pertaining to the harmful consequences of anxiety (Reiss & McNally, 1985). Although AS is a robust risk factor for panic, it can also be conceptualized as a transdiagnostic risk factor with relevance to other types of psychopathology, such as depression and other forms of anxiety (Naragon-Gainey, 2010; Noel & Francis, 2011; Olatunji & Wolitzky-Taylor, 2009), and a range of negative health behaviors (e.g., substance use; Otto et al., 2016). As such, AS modification may not only decrease panic vulnerability, but has the potential to attenuate the risk for development of other types of psychopathology.
A large body of work supports the malleability of AS (Naragon-Gainey, 2010; Olatunji & Wolitzky-Taylor, 2009). For example, Schmidt and colleagues (2007) found that a brief AS reduction training produced a 30% reduction in AS (compared to 17% in the control condition) and decreased likelihood of Axis I disorders at a two-year follow-up. In a follow-up study that included interoceptive exposure (IE) homework, Keough and Schmidt (2012) reported even larger reductions in AS at one and six-months post-intervention. Among the few preventive interventions that have targeted AS among youth (Conrod, Castellanos-Ryan, & Strang, 2010), Balle and Tortella-Feliu (2010) adapted the Australian FRIENDS anxiety prevention program to a six-session school-based program for high AS youth (11 to 17 years) and assessed AS, anxiety, and depression outcomes. Condition differences were only detected at the 6-month follow-up, in that participants in the prevention condition evidenced decreased AS compared to controls. Although promising, this intervention was resource intensive and condition differences were limited to AS. Nonetheless, evidence indicates AS is malleable via brief psychosocial interventions and that such reductions impact anxiety, depression, and other psychopathology (Schmidt et al., 2007).
Consistent with theoretical perspectives on the importance of including parents in youth prevention protocols (Beardslee et al., 2011), converging lines of empirical evidence underscore the benefit of parents in youth intervention efforts. Nonspecific anxiety and depression prevention programs that integrate parents evidence statistically and/or clinically significant anxiety reduction (Feldner, Zvolensky, & Schmidt, 2004), and “child plus parent” conditions outperform “child only” conditions (Pina, Zerr, Villalta, & Gonzales, 2012). Evidence from other prevention literatures suggest parent training can be an effective preventive intervention among youth (e.g., substance use; Mahabee-Gittens, Xiao, Gordon, & Khoury, 2013). Finally, parents are key agents in efforts to generalize exposure-related learning (Hirshfeld-Becker & Biederman, 2002), such as promoting learning experiences designed to reduce anxious responding to panic-relevant cues (e.g., IE exercises) in contexts outside the clinic/laboratory.
The current study evaluated the selective (i.e., specific to those at elevated risk) preventive intervention targeting the transdiagnostic risk factor of AS among at-risk youth. This brief intervention integrated experimenter- and family-directed IE exercises with the aim of decreasing vulnerability for anxiety and depression psychopathology through reducing AS. Vulnerability was indexed via anxiety and depression symptoms and emotional reactivity elicited using experimental psychopathology methods (Olatunji, Leen-Feldner, Feldner, & Forsyth, 2007). Proximal and short-term distal effects of the Anxiety Sensitivity Amelioration Program for Youth were evaluated by comparing it to a general health information control condition.
Method
Participants
Eighty-eight nonclinical youth (51.1% male) between 10 and 14 years (M = 12.52 years, SD = 1.41) and one of their parents were recruited from the local community. We chose the lower cutoff age of 10 years given the beginning of adolescence has been defined as the onset of puberty, which is underway by age 8 years for many American girls with outward signs appearing around age 10 years (Dahl, 2004; Susman & Rogol, 2004); we reasoned the upper cutoff of 14 years best captures the anxiety-related vulnerability of this period prior to disorder onset. Youth had a total CASI score ≥ 1 SD above the mean for males or females and the PI stratified by gender (Silverman, Fleisig, Rabian, & Peterson, 1991). Table 1 includes youth characteristics as a function of condition. Exclusionary criteria for youth were current or past cardiopulmonary or respiratory illness, possibility of being pregnant, current enrollment in mental health treatment, sibling enrollment in the current study, current psychotic disorder, current suicidal intent, and/or inability to give informed, written assent. Please see the CONSORT flow diagram in Figure 1 for more details on those excluded. Due to recommendations that prevention efforts should occur prior to disorder diagnosis (O’Connell et al., 2009), combined with evidence that suggests panic and generalized anxiety are two of the disorders most strongly associated with AS (Knapp, Blumenthal, Mischel, Badour, & Leen-Feldner, 2016; Naragon-Gainey, 2010), we also excluded for current or past PD, panic attacks, and GAD. All procedures were approved by the sponsoring university’s Institutional Review Board.
Table 1.
Correlations between Anxiety Sensitivity and Depression and Anxiety Symptoms at Baseline and Follow-up
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. BL CASI | -- | ||||||||||
| 2. Post CASI | .50* | -- | |||||||||
| 3. W2 CASI | .36* | .71* | -- | ||||||||
| 4. ML CASI | .29* | .55* | .58* | -- | |||||||
| 5. BL RCADS | .31* | .62* | .44* | .38* | -- | ||||||
| 6. BL Anx | .32* | .65* | .47* | .39* | .98* | -- | |||||
| 7. BL Dep | .17 | .36* | .25* | .21 | .82* | .71* | -- | ||||
| 8. M1 RCADS | .21 | .52* | .48* | .67* | .70* | .69* | .58* | -- | |||
| 9. M1 Anx | .20 | .56* | .50* | .70* | .70* | .70* | .53* | .99* | -- | ||
| 10. M1 Dep | .21 | .30* | .31* | .45* | .58* | .52* | .62* | .85* | .75* | -- | |
| 11. Age | −.01 | .05 | .07 | −.07 | .01 | .02 | .02 | −.03 | −.07 | .10 | -- |
Note. BL = Baseline. CASI = Childhood Anxiety Sensitivity Index. W2 = Week 2. M1 = Month 1. RCADS = Revised Child Anxiety and Depression Scale. Anx = Anxiety symptoms. Dep = Depression symptoms. n = 88.
p < .05.
Figure 1.
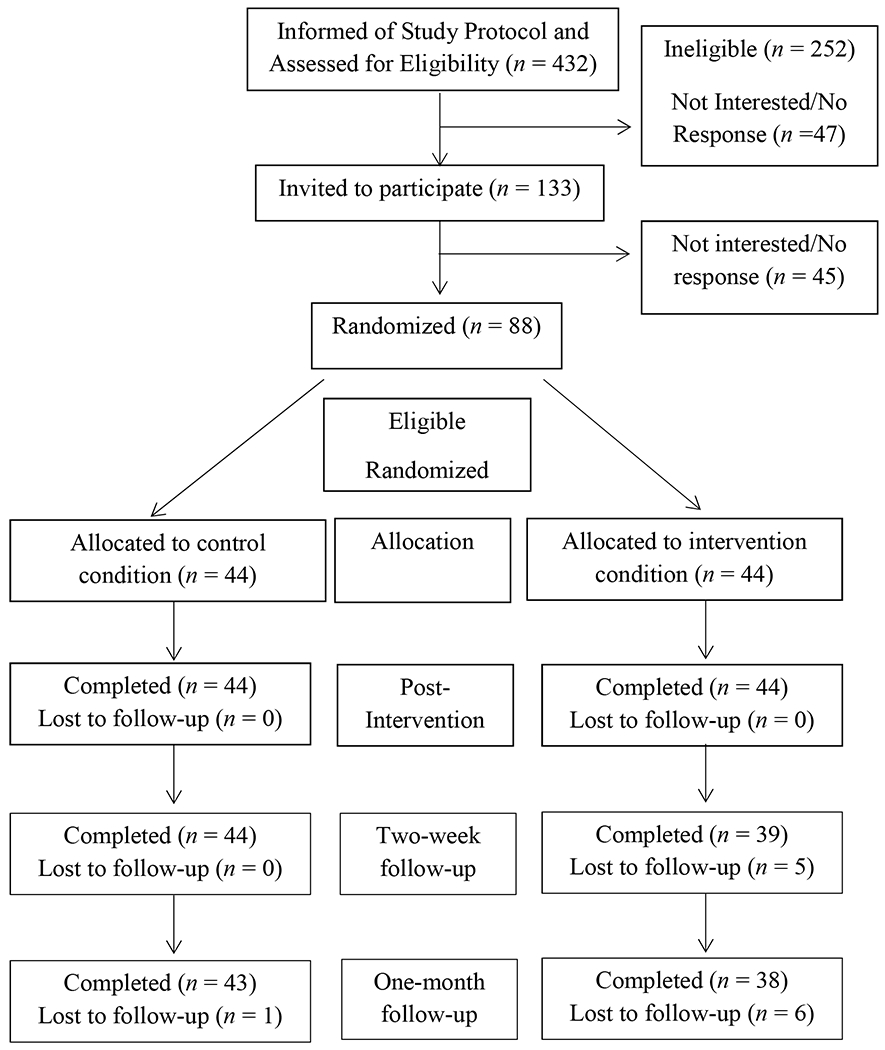
CONSORT Flow Diagram of the progress through the phases of a preventive intervention among two conditions (i.e., enrollment, intervention allocation, post-intervention, and two-week and one-month follow-up).
Measures
Youth assessment.
The Anxiety Disorders Interview Schedule-IV: Child version (ADISC; Silverman & Albano, 1996) and the Panic Attack Questionnaire (PAQ; Norton, Dorward, & Cox, 1986) were used to assess exclusionary criteria. The negative affect subscale of the Positive and Negative Affect Schedule for Children (PANAS; Joiner, Catanzaro, & Laurent, 1996) examined the effectiveness of random assignment to conditions. A manipulation check survey was used to ask youth about the topics (i.e., healthy foods, AS, bodily sensations, sleep, and/or none of the above) “talked about” in the presentation and related exercise.
Primary outcome variables.
The 18-item Childhood Anxiety Sensitivity Index (CASI; Silverman et al., 1991) was used to index global fear regarding the consequences of anxiety-related sensations. The 47-item Revised Child Anxiety and Depressive Scales (RCADS; Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000) was administered to assess how often youth experienced anxiety and depressive symptoms. Both the RCADS total score, anxiety symptom subscale, and depression symptom subscales were employed in analyses.
Experimental psychopathology variables.
A three-minute voluntary hyperventilation (VH) challenge, where the participant breathes at a rate of 30 respiratory cycles/min, was utilized to index real-time panic-relevant reactivity (Fried & Grimaldi, 1993). Participants provided pre-and post-challenge ratings of panic symptom intensity using the 23-item Acute Panic Inventory (API; Dillon, Gorman, Liebowitz, Fyer, & Klein, 1987). An ideographic worry induction procedure, where the participant is asked to engage in the cognitive process of worry for five-minutes, was used to index real-time emotional reactivity to worry (Frala, Mischel, Knapp, Autry, & Leen-Feldner, 2014). Participants reported current anxiety before and after the procedure using a 100-point Subjective Units of Distress Scale (SUDs; Wolpe, 1958).
Parent-youth dyad assessments.
Each week over the one-month intervention period, the parent and youth were asked to report homework completion. During the one-month debriefing, both the youth and parent in the ASAP-Y condition were separately asked to rate how reasonable or manageable the weekly homework was on a 11-point scale from 0 (not reasonable at all) to 10 (very reasonable) and to provide the completed weekly homework forms. Each youth-parent dyad was able to earn up to $75 for their participation in the study, and entered into a Mac-Apple gift-card raffle for each homework completed.
Procedure
Standardized Intervention and Control Programs
The Anxiety Sensitivity Amelioration Program for Youth, and associated administrator manual, were adapted from the standardized Anxiety Sensitivity Amelioration Training program and manual (ASAT; Schmidt et al., 2007) to make it developmentally appropriate for youth and consisted of two parts. Part I consisted of psychoeducation regarding the nature of anxiety/fear and AS, and an individual experimenter-directed exposure session of 10 repeated trials of straw breathing. Part II consisted of parent training in conducting at-home exposure exercises and training the dyad to monitor exposure practice once per week (four times total) during the follow-up period. The psychoeducation presentation was followed verbatim, and there was no deviation from the manual regarding the straw exercises. To control for general education effects and time spent with the researcher, the General Health Information Control Condition (GHI) also consisted of two parts (Schmidt et al., 2007). Part I included psychoeducation about the benefits of healthy dietary habits and practice using a “food tracker” to plan, record, and monitor nutritional information of meals (USDA; 2010). Part II consisted of parent training in using the food tracker and training the dyad in planning and tracking meals. The GHI control condition was adapted from the standardized Physical Health Education Training program and manual used in the ASAT and ASAT-Revised (Keough & Schmidt, 2012; Schmidt et al., 2007). Each program lasted approximately 50min.
Data Analytic Strategy
To test the equivalence of conditions on key baseline and demographic characteristics, t-tests and chi-square analyses were conducted to compare conditions regarding the variables of age, gender, PANAS, CASI, and RCADS (total, anxiety subscale, and depression subscale). Zero-order correlations were conducted between continuous variables to evaluate relations between demographic, baseline, and outcome characteristics. Chi-square tests were used to compare conditions on their knowledge of topics addressed during the programs.
Primary analyses.
Next, a latent difference score approach, using a latent growth curve framework (Mun, von Eye, & White, 2009) was used to model the effects of condition on changes in AS levels from baseline to post-intervention, post-intervention to two-weeks, and two-weeks to one-month. Models were fit in Mplus version 8 (Muthén & Muthén, 1998-2017) using full information maximum likelihood and the Yuan-Bentler scaled chi-square index (Y-B χ2) to adjust for nonnormality and missing data. A nonsignificant value indicated that the model provided good fit to the data (Kline, 2011). The comparative fit index (CFI), root mean square error of approximation (RMSEA), and RMSEA 90% confidence interval (CI) were also examined for model fit (Browne & Cudeck, 1993; Hu & Bentler, 1999). Modification indices and residual covariances were examined in the event of model misfit. Effect sizes (Cohen’s d) were calculated for the difference in change from baseline to the three separate outcome points over the pooled baseline standard deviation. Condition (0 = GHI, 1 = ASAP-Y) and age were included as predictors in this model.
Next, the direct effect of condition on one-month RCADS total score was examined, covarying for baseline RCADS total score. A separate model was conducted to examine the direct effects of condition on the RCADS anxiety and depression subscale scores. Following examination of the direct effects models, indirect effects models were examined to test whether condition led to reductions in RCADS total, RCADS anxiety, and RCADS depression scores through reductions in AS. Indirect effects models were conducted using maximum likelihood estimation and percentile-based CIs with 5,000 bootstrap resamples (Preacher & Hayes, 2008).
Random-intercept fixed effects MLMs were conducted to examine WIP Δ SUDs post-intervention and at one-month as well as VH Δ API post-intervention and at one-month. All models were initially centered at post-intervention. Time, condition, and time by condition interaction terms were included to examine the effects of condition on post-intervention and one-month challenge task outcomes.
Results
Preliminary Analyses
Missing data, skew, and kurtosis.
Five participants did not complete the two-week assessment and seven participants did not complete the one-month follow-up (four did not complete either session). Of these eight participants, seven were enrolled in ASAP-Y and one was enrolled in GHI. This difference in attrition was not significant (χ2 = 3.09, df = 1, p = .08). Comparison of demographics and baseline variables revealed no significant differences between those who attended all appointments and those who missed at least one appointment. No problematic levels of skew or kurtosis were detected (Curran, West, & Finch, 1996). The correlation matrix for all variables is provided in Table 1.
Covariates.
Preliminary analyses indicated that random assignment effectively equated conditions across key baseline and demographic variables. Conditions did not significantly differ as a function of youth age, gender, race, ethnicity, negative affect, baseline AS, baseline RCADS total, RCADS anxiety, or RCADS depression scores. Table 2 includes the means, standard deviations, and p-values of t-tests as a function of condition. Given the theoretical and empirical precedent of age in relation to anxiety and depression (Olatunji & Walistzky-Taylor, 2009), age and baseline symptom scores were included as covariates for relevant primary analyses.
Table 2.
Evaluation of the Efficacy of Random Assignment among Youth Demographic and Baseline Characteristics
| Total Samplea | GHI (Control)b | ASAP-Y (Intervention)b | pa | |
|---|---|---|---|---|
| M (SD) or % | M (SD) or % | M (SD) or % | ||
| Baseline Assessment | ||||
| Age | 12.5 (1.4) | 12.5 (1.4) | 12.6 (1.4) | ns |
| Gender (Males) | 51.1% | 50.0% | 52.3% | ns |
| Race (White) | 73.3% | 69.8% | 76.7% | ns |
| Ethnicity (Hispanic) | 10.2% | 15.9% | 4.5% | ns |
| Negative Affectb | 25.9 (8.3) | 25.9 (8.5) | 25.8 (8.2) | ns |
| Anxiety Sensitivityc | 32.9 (4.1) | 32.5 (4.1) | 33.3 (4.1) | ns |
| RCADS-Totald | 77.1 (18.2) | 77.8 (20.9) | 76.5 (15.4) | ns |
| Anxiety Symptomse | 60.7 (14.7) | 61..0 (16.3) | 60.5 (13.0) | ns |
| Depression Symptomsl | 16.4 (4.5) | 16.8 (5.1) | 15.9 (3.9) | ns |
| Post-Intervention Assessment | ||||
| Anxiety Sensitivitye | 27.8 (5.2) | 27.9 (5.7) | 27.7 (4.6) | |
| Two-Week Assessment | ||||
| Anxiety Sensitivitye | 27.2 (5.0) | 27.6 (5.5) | 26.7 (4.5) | |
| One-Month Follow-Up | ||||
| Anxiety Sensitivitye | 27.1 (5.6) | 28.6 (6.1) | 25.8 (4.3) | |
| RCADS-Totalf | 73.9 (18.4) | 75.9 (21.7) | 71.6 (13.8) | |
| Anxiety Symptomsg | 58.3 (14.7) | 60.1 (17.4) | 56.2 (10.8) | |
| Depression Symptomsl | 15.6 (4.6) | 15.8 (4.8) | 15.4 (4.5) | |
Note: a: n = 88 b: n = 44
A series of t-tests and chi square tests were utilized to examine condition differences between youth in the intervention condition and control condition.
Positive and Negative Affect Scale for Children
Childhood Anxiety Sensitivity Index
Revised Child Anxiety and Depressive Scales- Total Score
Revised Child Anxiety and Depressive Scales- Total Anxiety Symptoms Subscale
Revised Child Anxiety and Depressive Scales- Depression Symptoms Subscale
Manipulation check of condition and treatment acceptability.
Preliminary analyses suggested youth in the ASAP-Y were more likely to report learning about AS [χ2 (1, n = 88) = 80.18, p < .001] and bodily sensations [χ2 (1, n = 88) = 59.40, p < .001] post-intervention compared to GHI youth, whereas GHI youth were more likely to report reviewing healthy food [χ2 (1, n = 88) = 72.88, p < .001] and sleep [χ2 (1, n = 88) = 70.04, p < .001]. The weekly ASAP-Y homework appeared to be manageable for families to complete, as suggested by the high ratings of the homework as reasonable or manageable reported by both the youth (M = 8.9; SD = 1.3) and parent (M = 8.9; SD = 1.3). The acceptability of the weekly ASAP-Y homework was also demonstrated by the high compliance rates for the weekly homework. Participants (including those participants who dropped out) reported completing 3.4 weeks (n = 44; SD = 1.1), on average, of the four weeks possible, and 3.7 weeks (n = 38; SD = 0.80) among the participants who completed the follow-up.
Primary Analyses
Anxiety sensitivity.
The unconditional latent difference score model for AS was first fit to the data. This model provided good fit to the data (Y-B χ = 2.19, df = 2, p = .33, CFI = 1.00, RMSEA = .03, 90% CI [.00, .22]). Although the RMSEA upper-bound CI exceeded .10, there is evidence that the RMSEA performs poorly in models with few degrees of freedom (e.g., Hu & Bentler, 1999). The conditional latent difference score model, including condition and grand mean-centered age predicting the intercept (mean centered at post-intervention), the difference score from baseline to post-intervention, the difference score from post-intervention to two-weeks, and the difference score from two-weeks to one-month provided good fit to the data (Y-B χ2 = 1.95, df= 2, p = .38, CFI = 1.00, RMSEA = .00, 90% CI [.00, .21]), though again the upper bound RMSEA CI contained .10. Model parameters are provided in Table 3 and estimated mean scores by condition are provided in Figure 2. There was a significant decrease in AS scores from baseline to post-intervention, which was not significantly influenced by condition. There were no significant changes in AS from post-intervention to two-weeks, which was also not influenced by condition. Finally, there was not a significant change in AS from two-weeks to one-month. However, change was related to condition, such that scores decreased 2.13 points more in the ASAP-Y condition compared to scores in the GHI condition. At one-month, a medium-to-large effect size was found favoring ASAP-Y (d = .75). A 22.8% reduction was found for the ASAP-Y condition whereas a 14.0% reduction was found for the GHI condition.
Table 3.
Model Parameters for the Latent Difference Score Model of Anxiety Sensitivity
| Parameters | Mean/B | SE | p |
|---|---|---|---|
| Intercept | 27.94 | .85 | < .001 |
| Condition | −.18 | 1.10 | .87 |
| Age | .18 | .41 | .67 |
| Change 1 | 4.58 | .60 | < .001 |
| Condition | .96 | 1.00 | .34 |
| Age | −.22 | .35 | .52 |
| Change 2 | −.32 | .63 | .60 |
| Condition | −.42 | .84 | .62 |
| Age | −.004 | .34 | .99 |
| Change 3 | .47 | .87 | .59 |
| Condition | −2.13 | 1.05 | .04 |
| Age | −.50 | .40 | .20 |
| Intercept (Centered one-month) | 28.41 | .94 | < .001 |
| Condition | −2.32 | 1.17 | .05 |
| Age | −.33 | .45 | .28 |
Note. The intercept was centered on the post-intervention score. Age was centered. Condition was coded such that 0 = GHI and 1 = ASAP-Y. Change 1 reflected changes from baseline to post-intervention, Change 2 reflected changes from post-intervention to two-week follow-up, and Change 3 reflected changes from two-week follow-up to one-month follow-up.
Figure 2.
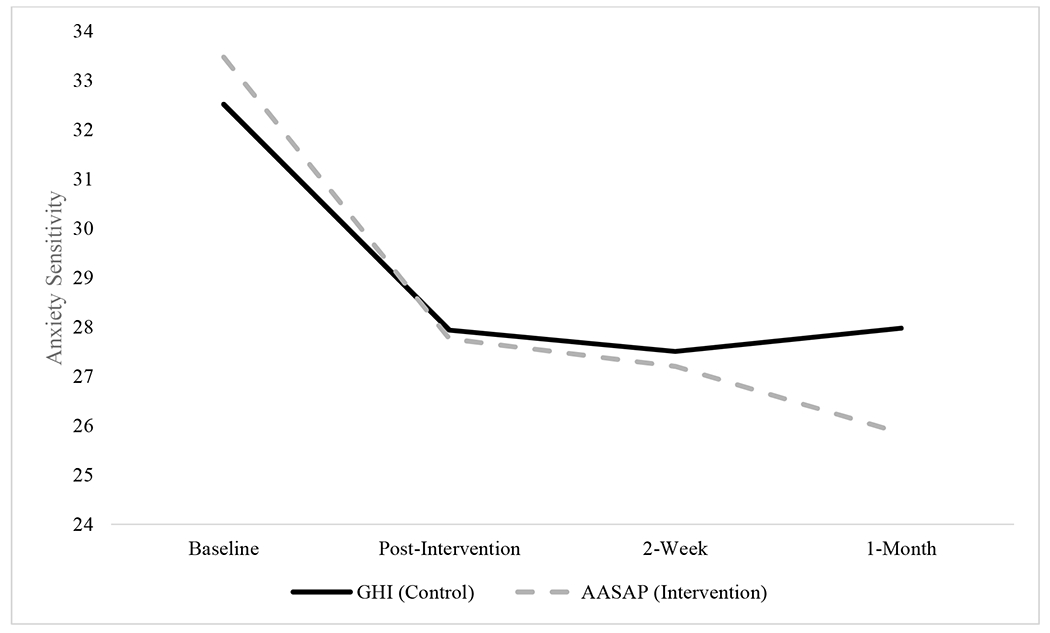
Trajectories of anxiety sensitivity across the intervention and follow-up period as a function of condition.
Direct effects on anxiety and depression symptoms.
The direct and indirect effects of condition on one-month RCADS total score, anxiety score, and depression score (controlling for age) are provided in Table 4. The model examining the direct effect of RCADS total score provided good fit to the data (χ2 = .28, df = 2, p = .87, CFI = 1.00, RMSEA = .11, 90% CI [.07, .14]). Examination of results indicated no direct effect of condition on one-month RCADS total scores (B = −4.15, p = .15). There was a 6.4% reduction in RCADS total scores in ASAP-Y and a 2.4% reduction in RCADS total scores in GHI. The differences were associated with a small effect size (d = .16; effect size estimates are based on raw data provided in Table 2). The direct effects model of condition on the anxiety and depression scores, controlling for age, provided excellent fit to the data (χ2 = 1.68, df= 3, p = .64, CFI = 1.00, RMSEA = .00, 90% CI [.00, .14]). Examination of results indicated no direct effects of condition on one-month anxiety scores (B = −3.94, p = .09) or on one-month depression scores (B = −.19, p = .81).
Table 4.
Direct and Indirect Effects of Intervention condition on One-Month RCADS Total Score, Anxiety Symptoms, and Depression Symptoms
| Direct Effects | Indirect Effects | |||||
|---|---|---|---|---|---|---|
| 1-Month RCADS Total | B | SE | p | B | SE (95% CI LL) | p (95% CI UL) |
| Baseline RCADS Total | .77 | .09 | < .001 | .57 | .09 | < .001 |
| Condition | −4.15 | 2.88 | .15 | −.16 | 2.28 | .94 |
| Age | −.40 | 1.04 | .70 | −.12 | 1.15 | .92 |
| 1-Month Anxiety Sensitivity | 1.58 | .28 | < .001 | |||
| Indirect | −4.50 | (−8.49) | (−.85) | |||
| 1-Month Anxiety Symptoms | B | SE | p | B | SE (95% CI LL) | p (95% CI UL) |
| Depression Symptoms | .17 | .39 | .66 | .46 | .29 | .12 |
| Anxiety Symptoms | .73 | .11 | < .001 | .43 | .09 | < .001 |
| Condition | −3.94 | 2.31 | .09 | −.09 | 1.69 | .96 |
| Age | −.88 | .96 | .36 | −.55 | .89 | .54 |
| 1-Month Anxiety Sensitivity | 1.38 | .20 | < .001 | |||
| Indirect | −4.20 | (−7.21) | (−1.17) | |||
| 1-Month Dep Symptoms | B | SE | p | B | SE (95% CI LL) | p (95% CI UL) |
| Depression Symptoms | .52 | .20 | .01 | .58 | .19 | .003 |
| Anxiety Symptoms | .05 | .06 | .34 | −.01 | .06 | .85 |
| Condition | −.19 | .86 | .83 | .65 | .84 | .44 |
| Age | .28 | .31 | .38 | .35 | .32 | .28 |
| 1-Month Anxiety Sensitivity | .30 | .09 | .001 | |||
| Indirect | −.92 | (−1.81) | (−.21) | |||
Note. RCADS = Revised Child Anxiety and Depressive Scales. For condition, 0 = GHI, 1 = ASAP-Y. SE = Standard error. 95% CI LL = 95% confidence interval lower limit. 95% CI UL = 95% confidence interval upper limit. CIs not containing 0 are significant.
Indirect effect models for anxiety and depression symptoms.
The model examining the indirect effects on RCADS total score provided adequate fit to the data (χ2 = 12.36, df = 6, p = .05, CFI = .94, RMSEA = .11 90% CI [.00, .20]; see Figure 3), although the RMSEA was again elevated. Examination of modification indices revealed no empirically supported modifications that could be made to improve model fit. A significant indirect effect was found from condition to one-month RCADS total score through one-month AS score (B = −4.50, 95% CI [−8.49, −.86]), revealing that RCADS total scores were reduced 4.5 points more in ASAP-Y compared to GHI, through AS reductions. The model examining the indirect effects on RCADS anxiety and depression scores provided excellent fit to the data (χ2 = 4.07, df = 6, p = .67, CFI = 1.00, RMSEA = .00, 90% CI [.00, .11]). Significant indirect effect was found from condition to one-month anxiety (B = −4.20, 95% CI [−7.21, −.117]) and one-month depression (B = −.92, 95% CI [−1.81, −.21]) through one-month AS scores.
Figure 3.
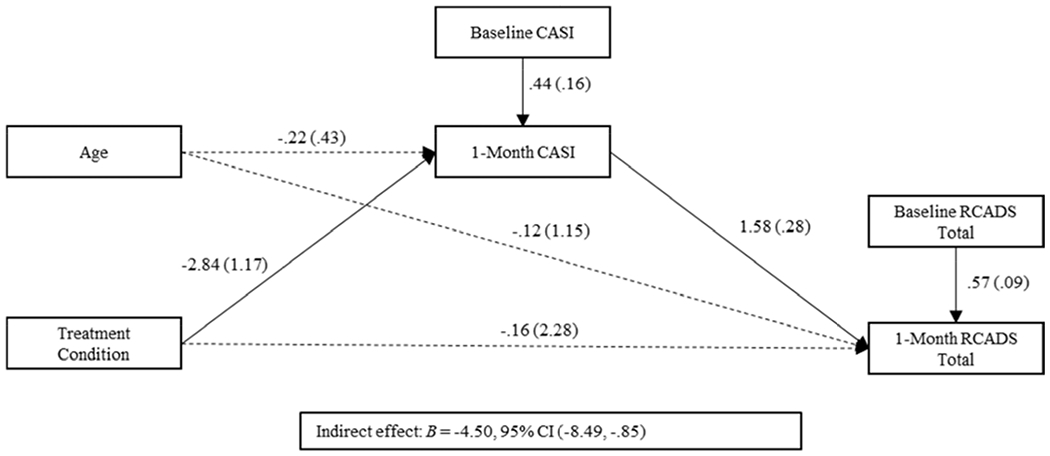
Indirect effects of intervention condition (0 = GHI, 1 = ASAP-Y) predicting 1-month RCADS total scores through 1-month CASI scores. Nonsignificant path estimates are represented by dashed lines.
Direct effects on laboratory-based outcomes.
In the WIP Δ SUDs model, scores in GHI (M = 35.45) were similar to scores in ASAP-Y (M = 40.16; p = .54). There was a significant effect of time (B = −12.89, p = .01), indicating that Δ SUDs scores were significantly lower from post-intervention to the one-month in GHI. In contrast, one-month scores in ASAP-Y (M = 40.66) were similar to post-intervention scores in ASAP-Y. In the VH Δ API model, scores in GHI (M = 5.53) were similar to scores in ASAP-Y (M = 8.93; p = .10). There was no effect of time (B = −1.65, p = .06), indicating that Δ API scores were similar across post-intervention and one-month in GHI. The condition by time interaction was nonsignificant (B = −.91, p = .53), indicating that Δ API scores were also similar across timepoints in ASAP-Y.
Discussion
The primary aim of the current investigation was to examine a selective preventive intervention that integrated psychoeducation and experimenter- and family-directed IE exercises with the aim of reducing AS and vulnerability for anxiety and depression psychopathology among at-risk youth. The high homework compliance rates and dyad ratings of homework manageability support the acceptability of the ASAP-Y. Youth in the intervention condition sustained low AS levels across the intervention period, and although both conditions decreased in AS levels across the intervention, youth in the intervention condition evidenced significantly lower AS levels at the one-month follow-up period compared to youth in the control condition. The trends in AS reductions between baseline and the one-month follow-up within both conditions (23% reduction in intervention condition, 14% in control condition at the one-month follow-up) are consistent with those observed in the youth and adult AS amelioration literatures. For example, Schmidt and colleagues (2007) detected a 30% reduction in the intervention condition and 17% reduction in control condition at the 1-year follow-up among adults, whereas Balle and Tortella-Feliu (2010) reported a 25% reduction in the intervention condition and 18% reduction in the control condition at the 6-month follow-up among youth. Our pattern of results could suggest that both conditions evidenced systematic decline due to repeated assessment, but the intervention condition evidenced further reductions in AS due to the intervention itself.
As hypothesized, the indirect effects of condition on anxiety and depression symptoms through one-month AS were significant. This suggests that psychoeducation and IE exercises yield specific anxiety- and depression-related benefits through the indirect effects of reduced AS. This finding is consistent with adult AS amelioration programs, in which the interventions evidenced beneficial effects on anxiety and mood symptoms through changes in AS (Schmidt, Norr, Allan, Raines, & Capron, 2017; Smits et al., 2008). This finding has exciting potential implications for anxiety and depression psychopathology prevention, in that a small dose may contribute to significant and long-term change. It will be critical to employ longer-term assessments to assess durable change and to examine if increasing dose or including more robust intervention components (e.g., cognitive-bias modification; Capron & Schmidt, 2016) yield greater effects.
In contrast to prediction, no differences in emotional reactivity elicited using experimental psychopathology methods were detected between conditions. While the effects of an AS amelioration program on reactivity to a worry induction have not yet been directly evaluated, our breathing exercise results are in contrast to past AS amelioration work among adults that have detected differences between conditions in reactivity to a biological challenge (Schmidt et al., 2007). These inconsistent findings underscore the early phases of development of this intervention and that refinement is needed to better engage youth AS to produce meaningful effects on the incidence of anxiety and related disorders.
Limitations of the current study merit mention. The current investigation primarily relied on youth self-report measures. A promising avenue for future work would be inclusion of additional assessment modalities from multiple informants to better inform the design and evaluation of the ASAP-Y intervention. Further, the PI who administered the programs was not blind to condition. Utilizing a technology-delivered intervention modality would enhance the internal validity of the observed findings (Schmidt, Capron, Raines, & Allan, 2014) . Lastly, extended post-intervention assessment intervals and inclusion of older youth are essential for determining the impact of the intervention on incidence of psychopathology across the course of adolescence.
Given the public health significance of decreasing risk for anxiety and depression psychopathology onset among youth, the goal of current study was to investigate the effects of a brief intervention on anxiety and depression outcomes for at-risk youth. Taken together, the current findings offer preliminary support for the ASAP-Y intervention as an acceptable, selective preventive intervention for at-risk youth, with specific short-term effects on AS and support for anxiety- and depression-related effects via reduced AS. The intervention implications of the current results are promising, in that a small dose may contribute to substantial and lasting change. Future work is now needed to refine ASAP-Y and prospectively evaluate the effects of the optimized intervention on the incidence of anxiety and depression psychopathology.
Highlights.
Intervention condition had greater decreases in anxiety sensitivity (AS) at 1-month
Indirect effects of condition on 1-month mood symptoms via AS were significant
Self-report and homework data supported the acceptability of the AS intervention
No differences between conditions were detected in challenge procedures outcomes
Acknowledgements
This work was supported by the National Institute of Mental Health [T32 MH115882, 1F31 MH102856-01A1].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ames ME, & Leadbeater BJ (2018). Depressive symptom trajectories and physical health: Persistence of problems from adolescence to young adulthood. J Affect Disord, 240, 121–129. [DOI] [PubMed] [Google Scholar]
- Balle M, & Tortella-Feliu M (2010). Efficacy of a brief school-based program for selective prevention of childhood anxiety. Anxiety Stress Coping, 23(1), 71–85. [DOI] [PubMed] [Google Scholar]
- Beardslee W, Chien P, & Bell C (2011). Prevention of mental disorders, substance abuse, and problem behaviors: a developmental perspective. Psychiatr Serv, 62(3), 247–254. [DOI] [PubMed] [Google Scholar]
- Browne MW, & Cudeck R (1993). Alternative ways of assessing model fit In Bollen KA & Long JS (Eds.), Testing structural equation models. Newbury Park, CA: Sage. [Google Scholar]
- Capron DW, & Schmidt NB (2016). Development and randomized trial evaluation of a novel computer-delivered anxiety sensitivity intervention. Behav Res Ther, 81, 47–55. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, & Francis SE (2000). Assessment of symptoms of DSM-IV anxiety and depression in children: a revised child anxiety and depression scale. Behav Res Ther, 38(8), 835–855. [DOI] [PubMed] [Google Scholar]
- Conrod PJ, Castellanos-Ryan N, & Strang J (2010). Brief, personality-targeted coping skills interventions and survival as a non-drug user over a 2-year period during adolescence. Arch Gen Psychiatry, 67(1), 85–93. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Angold A, Shanahan L, & Costello EJ (2014). Longitudinal patterns of anxiety from childhood to adulthood: the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry, 53(1), 21–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran PJ, West SG, & Finch JF (1996). The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological methods, 1(1), 16. [Google Scholar]
- Dahl RE (2004). Adolescent brain development: a period of vulnerabilities and opportunities. Keynote address. Ann N YAcad Sci, 1021, 1–22. [DOI] [PubMed] [Google Scholar]
- Dillon DJ, Gorman JM, Liebowitz MR, Fyer A, & Klein D (1987). Measurement of lactate-induced panic and anxiety. Psychiatry Research, 20, 97–105. [DOI] [PubMed] [Google Scholar]
- Feldner MT, Zvolensky M, & Schmidt NB (2004). Prevention of anxiety psychopathology: A critical review of the empirical literature. Clinical Psychology: Science and Practice, 11, 405–424. [Google Scholar]
- Frala J, Mischel E, Knapp AA, Autry K, & Leen-Feldner EW (2014). Adolescent worry induction: An experimental laboratory evaluation. Journal of Experimental Psychopathology(5), 52–71. [Google Scholar]
- Fried R, & Grimaldi J (1993). The psychology and physiology of breathing: In behavioral medicine, clinical psychology, and psychiatry. New York: Plenum Press. [Google Scholar]
- Hirshfeld-Becker D, & Biederman J (2002). Rationale and principles for early intervention with young children at risk for anxiety disorders. Clin Child Fam Psychol Rev, 5, 161–172. [DOI] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling, 6, 1–55. [Google Scholar]
- Joiner TE, Catanzaro SJ, & Laurent J (1996). Tripartite structure of positive and negative affect, depression, and anxiety in child and adolescent psychiatric inpatients. J Abnorm Psychol, 105(3), 401–409. [DOI] [PubMed] [Google Scholar]
- Keough ME, & Schmidt NB (2012). Refinement of a brief anxiety sensitivity reduction intervention. J Consult Clin Psychol, 80(5), 766–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, Gruber MJ, … Merikangas KR (2012). Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Arch Gen Psychiatry, 69(4), 372–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB (2011). Principles and practice of structure equation modeling (3rd ed.).New York, NY: The Guilford Press. [Google Scholar]
- Knapp AA, Blumenthal H, Mischel ER, Badour CL, & Leen-Feldner EW (2016). Anxiety sensitivity and its factors in relation to generalized anxiety disorder among adolescents. J Abnorm Child Psychol, 44(2), 233–244. [DOI] [PubMed] [Google Scholar]
- Mahabee-Gittens E, Xiao Y, Gordon J, & Khoury J (2013). The dynamic role of parental influences in preventing adolescent smoking initiation. AddictBehav, 38(4), 1905–1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mun EY, von Eye A, & White HR (2009). An SEM Approach for the Evaluation of Intervention Effects Using Pre-Post-Post Designs. Struct Equ Modeling, 16(2), 315–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naragon-Gainey K (2010). Meta-analysis of the relations of anxiety sensitivity to the depressive and anxiety disorders. Psychol Bull, 136(1), 128–150. [DOI] [PubMed] [Google Scholar]
- Noël VA, & Francis SE (2011). A meta-analytic review of the role of child anxiety sensitivity in child anxiety. J Abnorm Child Psychol, 39(5), 721–733. [DOI] [PubMed] [Google Scholar]
- Norton GR, Dorward J, & Cox BJ (1986). Factors associated with panic attacks in nonclinical subjects. Behavior Therapy, 17, 239–252. [Google Scholar]
- O’Connell M, Boat T, & Warner KE (2009). Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. Washington, DC US: National Academic Press. [PubMed] [Google Scholar]
- Olatunji BO, Leen-Feldner EW, Feldner MT, & Forsyth JP (2007). Handbook of Research Methods in Abnormal and Clinical Psychology. In (pp. 47–60). Thousands Oaks, CA: Sage Publications. [Google Scholar]
- Olatunji BO, & Wolitzky-Taylor KB (2009). Anxiety sensitivity and the anxiety disorders: a meta-analytic review and synthesis. Psychol Bull, 135(6), 974–999. [DOI] [PubMed] [Google Scholar]
- Otto MW, Eastman A, Lo S, Hearon BA, Bickel WK, Zvolensky M, … Doan SN (2016). Anxiety sensitivity and working memory capacity: Risk factors and targets for health behavior promotion. Clin Psychol Rev, 49, 67–78. doi: 10.1016/j.cpr.2016.07.003 [DOI] [PubMed] [Google Scholar]
- Pina AA, Zerr AA, Villalta IK, & Gonzales NA (2012). Indicated prevention and early intervention for childhood anxiety: a randomized trial with Caucasian and Hispanic/Latino youth. J Consult Clin Psychol, 80(5), 940–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher K, & Hayes A (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods, 40, 879–891. [DOI] [PubMed] [Google Scholar]
- Reiss S, & McNally RJ (1985). In Reiss S & Bootzin RR (Eds.), Theoretical Issues in Behavior Therapy. San Diego: Academic Press. [Google Scholar]
- Schmidt NB, Capron DW, Raines AM, & Allan NP (2014). Randomized clinical trial evaluating the efficacy of a brief intervention targeting anxiety sensitivity cognitive concerns. J Consult Clin Psychol, 82(6), 1023–1033. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Eggleston A, Woolaway-Bickel K, Fitzpatrick K, Vasey M, & Richey J (2007). Anxiety Sensitivity Amelioration Training (ASAT): a longitudinal primary prevention program targeting cognitive vulnerability. J Anxiety Disord, 21(3), 302–319. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Norr AM, Allan NP, Raines AM, & Capron DW (2017). A randomized clinical trial targeting anxiety sensitivity for patients with suicidal ideation. J Consult Clin Psychol, 55(6), 596–610. [DOI] [PubMed] [Google Scholar]
- Silverman WK, & Albano AM (1996). The Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. San Antonio, TX: Physiological Corporation. [Google Scholar]
- Silverman WK, Fleisig W, Rabian B, & Peterson RA (1991). Childhood Anxiety Sensitivity Index. Journal of Clinical Child Psychology, 20, 162–168. [DOI] [PubMed] [Google Scholar]
- Smits JA, Berry AC, Rosenfield D, Powers MB, Behar E, & Otto MW (2008). Reducing anxiety sensitivity with exercise. Depress Anxiety, 25(8), 689–699. [DOI] [PubMed] [Google Scholar]
- Susman EJ, & Rogol A (2004). In Lerner RM & Steinberg L (Eds.), Handbook of Adolescent Psychology (2nd ed., pp. 15–44). Hoboken, NJ: Wiley & Sons. [Google Scholar]
- Wolpe J (1958). Psychotherapy by reciprocal inhibition. Stanford, CA: Stanford University Press. [Google Scholar]


