Abstract
The dynamic nature of finding male sexual partners (sex-finding) among Chinese men who have sex with men (MSM) may play a substantial role in the HIV epidemic. We compared characteristics and behaviors of MSM who mostly sought sex via the Internet versus traditional venues in a cross-sectional survey among 3,588 Chinese MSM. We assessed the sociodemographic predictors and compared high-risk behaviors of using Internet vs. traditional venues for sex-finding. Compared to non-Internet MSM, Internet-user MSM were more likely to have been: younger, currently single, better educated, health-insured, with higher income, with Beijing residency (‘Hukou’), living longer in the city, HIV-positive, ever using drug and engaging in condomless receptive anal sex. Internet sex-finding users were less likely to be sexually active for longer duration, drink alcohol, drink alcohol before sex, or ever have sex with women. Knowledge of differential characteristics of various sex-finding MSM can help design targeted interventions.
Keywords: Men who have sex with men, China, sex-finding, Internet, HIV/AIDS
INTRODUCTION
Men who have sex with men (MSM) have become the most dynamic high-risk subgroup in China, driving the upward trend of HIV since 2006 [1]. By 2013, MSM accounted for 21.3% of all people living with HIV/AIDS (PLWHA) in China [2], and their HIV prevalence increased from 3.0% in 2006, to 7.6% in 2013 [2]. Although many HIV prevention intervention programs highlight Chinese MSM as a key population, MSM are documented to continue with a high prevalence of risky behaviors, such as condomless anal sex, substance abuse, multiple sexual partnership and lack of routine HIV testing [3–7]. Hence, continued HIV transmission occurs within and beyond this population through both homosexual and heterosexual contacts [8].
A diversity of channels are used among MSM to find sexual partners (sex-finding); this adds to the complexity of sexual networks and presents a huge challenge in coping with the ever-growing HIV epidemic among Chinese MSM [9–13]. Traditionally, sex-finding has been concentrated in public locations such as parks, public toilets, entertainment facilities (e.g., gay-friendly bars/pubs, bathhouses, and saunas) [14,15]. Such venues were fixed physical locations for MSM to identify partners and have sex anonymously and/or privately [16]. Risk reduction interventions were often venue-based to reach the largest number of vulnerable men [17]. The rapid development of greater economic purchasing power and affordable technologies have resulted in 45.8% of China’s 1.3 billion person population using the Internet in 2013, the highest absolute number of users of any nation in the world [18]. As the Internet has become widely available and can be used privately and anonymously, many Chinese MSM have embarked on online sex-finding platforms [19,20]. A 2013 study among 50,000 MSM from 61 cities in China showed that approximately 45% of the participants had ever used Internet to find sexual partners [21]. This proportion is likely higher in 2016.
In a variety of countries, MSM who were recruited via Internet were younger, better educated, had more sexual partners, and/or engaged in more condomless anal sex [22–24], while those recruited from traditional venues were less likely to use illicit drugs and were more likely to know the HIV status of their sexual partners [25]. However, findings vary by geographic location and source of sampling. In China, little is known about the characteristics among online versus offline sex-finding MSM. We sought to assess demographic factors associated with sex-finding using Internet versus traditional venues among Chinese MSM, comparing their HIV-related behaviors.
METHODS
Study design and participants
This study was part of an NIH-funded clinical trial ‘Multi-component HIV Intervention Package for Chinese MSM—Test, Link and Care’ (the China-MP3 Project), which was conducted in Beijing, China. The China-MP3 Project included two study phases: Phase I— expanded recruitment of MSM for study participation and HIV testing in MSM community; Phase II—a randomized clinical trial of linkage to HIV care intervention among HIV-positive MSM. A convenience sample of HIV-negative or status-unknown MSM who lived in Beijing were recruited by our collaborated local gay community-based organization (Chaoyang AIDS Volunteer Group, CAVG) via short message service; website advertisement, outreach to gay-frequented venues, peer referral, and self-participation when visiting the clinics. Participants who were 18 years or older, currently living in Beijing, self-reporting having sex with men (or transgender women) in the past 12 months prior to the survey, self-reporting being HIV-negative or status-unknown (the national HIV/AIDS database was used to validate these self-reported data), have not previously participated in the current study (names and cell phone numbers of potential participants were used to screen for potential duplicate participations in each study clinic), and willing to provide informed consent were considered eligible to participate in the study. Participants received both pre- and post-testing counseling, and were given 50 yuan (about US$8) to compensate their transportation costs. Each participant completed a questionnaire survey and gave a blood sample for HIV and syphilis testing. The study protocol was reviewed and approved by the institutional review boards of Vanderbilt University, and the National Center for AIDS/STD Control and Prevention (NCAIDS) of Chinese Center for Disease Control and Prevention.
Data collection and measurement
Eligible participants were invited to complete the interview and have a blood test for HIV in a private room at one of four specified clinics including Beijing Municipal Center for Disease Control and Prevention (CDC), Chaoyang District CDC, Xicheng District CDC, and Jingcheng Dermatology Hospital. A questionnaire was administered by trained interviewers to survey on the following information: (1) sociodemographic characteristics, including age, education, ethnicity, employment, current marital status, monthly income, years of living in Beijing, legal Beijing residency status (‘Hukou’), and insurance coverage; (2) behavioral factors, including lifetime male and female sexual partners, age of first sex, HIV risk perception, HIV testing history, channels of seeking male sexual partners (we defined Internet use as email communication, website browsing, using of computer-based chatting platforms [e.g. QQ, chat room, etc.] and social networking apps [e.g. WeChat, Weibo, etc.]), alcohol consumption in the past 3 months, drug use in the past 3 months, having sex with women in the past 3 months, and patterns of sexual behaviors (insertive/receptive anal sex, condomless anal sex, sex with HIV-positive men, oral sex and sex with male commercial sex worker) with men in the past 3 months; (3) HIV infection status and syphilis serology.
Laboratory testing
HIV rapid tests were performed using Alere Determine™ HIV1/2 (Colloidal Selenium Device; Alere Medical Co, Ltd., USA). HIV antibody was further screened using ELISA (HIV ELISA testing kit 1, Zhuhai Livzon Diagnostics Inc., China). If positive, the specimen was tested again using another ELISA kit (HIV ELISA testing kit 2, Beijing Wantai Biological Pharmacy Enterprise Co. Ltd., China). A specimen with a positive reaction in both or either ELISA tests was confirmed by Western blot test (HIV Blot 2.2 WB; MP Biomedicals Co, Ltd., China). One Step Anti-TP (Treponema pallidum/Syphilis) Test (Colloidal Gold Device, Standard Diagnostics, Inc., Korea) was used as a syphilis rapid tests. For rapid test positive persons, syphilis serology was determined through Syphilis Toluidine red unheated serum test (Beijing WANTAI Biological Pharmacy Enterprise Co. Ltd., China) and confirmed by the Treponema palladium particle assay (Fujirebio Inc., Tokyo, Japan).
Statistical analysis
Data analyses were conducted using Stata 12.0™ (StataCorp LP, College Station, Texas, USA). Frequency distribution with percentage and median with interquartile range (IQR) were used to characterize categorical and continuous variables, respectively. Pearson Chi square tests were used to compare categorical variables, while Wilcoxon rank-sum tests were used to compare continuous variables across channels of seeking male sexual partner (Internet vs. non-Internet). Statistical significance was consider at p < 0.05. Bivariate and multivariable logistic regression analyses were conducted to assess socio-demographic factors associated with using Internet for seeking male sexual partners. In building the multivariable model, we individually used direct acyclic graph (DAG) to identify a minimum sufficient set of confounders for the association between each sociodemographic predictor and channels of sex-finding (Internet vs. non-Internet) and different set of confounders were fitted into each multivariable model to yield adjusted odds ratios [26,27]. Collinearity was also assessed among covariates in the multivariable model.
RESULTS
Of 3,760 participants, 3,588 (95.4%) participants were included in the analysis; 6.6% participants were recruited via SMS; 6.8% web advertising, 2.0% outreach, 41.0% peer referral, and the remaining 43.6% participated in the study by themselves. A total of 172 men were excluded, including duplicate participation through multiple clinics(126), confirmed HIV-positive prior to the study after validating with national HIV/AIDS database (30), non-MSM or transgender women (5), no blood sample (5), invalid identification numbers (4), and lack of questionnaires (2).The median age was 28 years (IQR: 24–33). Most participants were single (85.0%), currently employed (82.5%), college educated (71.9%), without Beijing ‘Hukou’ (75.2%), and of the Han majority ethnic group (93.7%). Lab-confirmed HIV prevalence was 12.7% and syphilis prevalence was 7.5%.
Figure 1 shows the channels that study participants (n=3,588) used most frequently for seeking male sexual partners. The Internet was the most common channel (79.1%), while 21.9% used traditional public or gay-frequented venues. Among the non-Internet venues, the top three were public parks (6.7%), bar or dance club (4.0%), and public/male bathhouse (2.6%).
Figure 1.
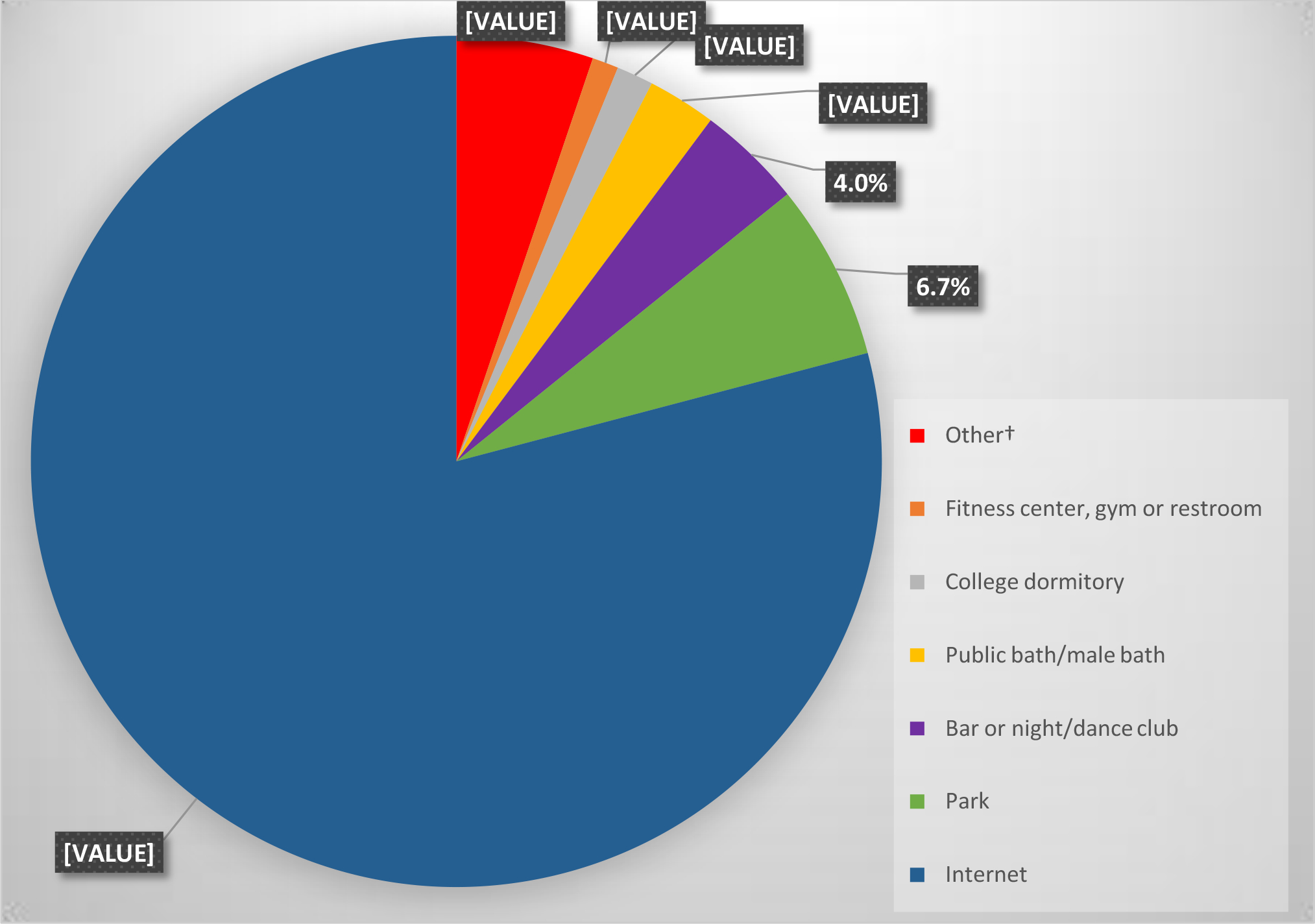
Most frequently used channels to find male sexual partners among Chinese men who have sex with men (N=3,588)
† Includes: beach, woods, street, theater, public transportation, hotel and private homes
Table 1 shows the bivariate and multivariable logistic regression analyses of the sociodemographic factors associated with venues of seeking male sexual partners. Being non-Han ethnicity (OR=1.60, 95% confidence interval [CI] 1.10–2.33; p=0.016), being currently single (adjusted odds ratio [AOR]=1.55, 95% CI 1.21–1.98; p<0.001), having higher education level (e.g., college and above vs junior school or less, AOR= 5.32, 95% CI 4.21–6.74; p<0.001), having higher monthly income (AOR= 1.41, 95% CI 1.15–1.74; p<0.001), living in Beijing for longer (AOR= 1.25, 95% CI 1.03–1.51; p=0.022), being health insured (aOR= 1.58, 95% CI 1.32–1.89; p<0.001) and being a Beijing registered resident (AOR= 1.39, 95% CI 1.12–1.73; p=0.003) were associated with a higher likelihood of using Internet to find male sexual partners. However, being older in age (OR= 0.93, 95% CI 0.92–0.94; p<0.001), being unemployed (AOR= 0.62, 95% CI 0.43–0.89; p=0.008) or a student (AOR= 0.64, 95% CI 0.47–0.90; p=0.009) were associated with a lower likelihood of using the Internet to find male sexual partners (more likely to find sex via public venues).
Table 1.
Predictors of using Internet versus non-Internet venues for finding male sexual partners among men who have sex with men in Beijing, China (N = 3588)
| Characteristics | Total N = 3588 n (%) | Partner-seeking route | OR (95 % CI) | p value | AOR (95 % CI) | p value | |
|---|---|---|---|---|---|---|---|
| Internet N = 2838 n (%) | Non-Internet N = 750 n (%) | ||||||
| Age (year) | |||||||
| Median, IQR | 28 (24–33) | 27 (24–32) | 31 (26–41) | 0.93 (0.92, 0.94) | <0.001 | NA | NA |
| Monthly income (Chinese yuan) | |||||||
| <5000 | 1698 (47.3) | 1230 (43.3) | 468 (62.4) | 1.00 | 1.00 | ||
| ≥5000 | 1890 (52.7) | 1608 (56.7) | 282 (37.6) | 2.17 (1.84, 2.56) | <0.001 | 1.41 (1.15, 1.74)a | 0.001 |
| Year of living in Beijing | |||||||
| <5 | 1533 (42.7) | 1229 (43.3) | 304 (40.5) | 1.00 | 1.00 | ||
| ≥5 | 2055 (57.3) | 1609 (56.7) | 446 (59.5) | 0.89 (0.76, 1.05) | 0.172 | 1.25 (1.03, 1.51)b | 0.022 |
| Ethnicity | |||||||
| Han | 3361 (93.7) | 2644 (93.2) | 717 (95.6) | 1.00 | |||
| Non-Han | 227 (6.3) | 194 (6.8) | 33 (4.4) | 1.60 (1.10, 2.33) | 0.016 | NA | NA |
| Current marital status | |||||||
| Currently married | 539 (15.0) | 308 (10.8) | 231 (30.8) | 1.00 | 1.00 | ||
| Currently single | 3049 (85.0) | 2530 (89.2) | 519 (69.2) | 3.65 (3.00, 4.44) | <0.001 | 1.55 (1.21, 1.98)c | 0.001 |
| Education (year of schooling) | |||||||
| Junior middle school (≤9) | 416 (11.6) | 191(6.7) | 225 (30.0) | 1.00 | 1.00 | ||
| Senior high (10–12) | 593 (16.5) | 422 (17.9) | 171 (22.8) | 2.55 (2.06, 3.14) | <0.001 | 2.18 (1.75, 2.71)d | <0.001 |
| College and above (>12) | 2579 (71.9) | 2225 (78.4) | 354 (47.2) | 7.40 (5.22, 9.25) | <0.001 | 5.32 (4.21, 6.74)d | <0.001 |
| Employment | |||||||
| Employed | 2960 (82.5) | 2351 (82.8) | 609 (81.2) | 1.00 | 1.00 | ||
| Unemployed/retired | 182 (5.1) | 109 (3.9) | 73 (9.7) | 0.39 (0.28, 0.53) | <0.001 | 0.62 (0.43, 0.89)c | 0.008 |
| Student | 388 (10.8) | 335 (11.8) | 53 (7.1) | 1.64 (1.20, 2.22) | 0.001 | 0.64 (0.47, 0.90)c | 0.009 |
| Other | 58 (1.6) | 43 (1.5) | 15 (2.0) | 0.74 (0.41, 1.35) | 0.326 | 1.11 (0.58, 2.14)c | 0.835 |
| Health insurance | |||||||
| No | 1395 (38.9) | 1008 (35.5) | 387 (51.6) | 1.00 | 1.00 | ||
| Yes | 2193 (61.1) | 1830 (64.5) | 363 (48.4) | 1.94 (1.65, 2.28) | <0.001 | 1.58 (1.32, 1.89)e | <0.001 |
| Beijing Hukou | |||||||
| No | 2699 (75.2) | 2113 (74.5) | 586 (78.1) | 1.00 | 1.00 | ||
| Yes | 889 (24.8) | 725 (25.5) | 164 (21.9) | 1.23 (1.01, 1.49) | 0.038 | 1.39 (1.12, 1.73)f | 0.003 |
Hukou household registration, IQR interquartile range, CI confidence interval, OR odds ratio, AOR adjusted odds ratio, NA denoting no confounders identified based on DAG and only crude odds ratio with corresponding p value was reported
Adjusted for age, education and employment
Adjusted for age and Beijing ‘Hukou’
Adjusted for age and education
Adjusted for age
Adjusted for age, income and employment
Adjusted for age and years of living in Beijing
Table 2 shows the comparison of the risk behaviors, risk perception and syphilis/HIV prevalence between participants who mostly sought sex via Internet versus non-Internet venues. Compared with MSM who mostly used non-Internet venues, those using Internet to find sex were more likely to use drugs in the past 3 months (30.0% vs. 18.3%, χ2=40.831, p<0.001), have receptive (53.6% vs. 47.2%, χ2=9.721, p=0.002) or condomless receptive anal sex (21.1% vs. 17.7%, χ2=4.239, p<0.039) with men in the past 3 months, have high/very high HIV risk perception (41.7% vs.37.2%, χ2=4.941, p=0.026) and be recently newly diagnosed as HIV-positive (13.4% vs.10.0%, χ2=6.156, p=0.013).Conversely, MSM who use non-Internet venues to find sex were more likely to have ≥ 1 lifetime female sexual partners (61.5% vs.33.8%, χ 2=190.534, p<0.001), frequently consume alcohol (33.2% vs. 23.1%, χ2=42.714, p<0.001), use alcohol before sex (≥ once per week:25.3% vs. 19.3%, χ2=13.176, p<0.001), have sex (20.0% vs.8.0%, χ2=90.868, p<0.001) or condomless vaginal sex (12.9% vs. 4.9%, χ2=61.548, p<0.001) with women in the past 3 months and being newly diagnosed as syphilis seropositive (9.6% vs. 6.9%, χ2=6.046, p=0.014).
Table 2.
Comparison of high-risk behaviors between Chinese men who have sex with men seeking male sexual partners via Internet and non-Internet venues (N=3,588)
| High-risk behaviors | Total N=3,588 n (%) | Partner-seeking route | χ2 or z-statistics† | p-value | |
|---|---|---|---|---|---|
| Internet N=2,838 n (%) | non-Internet N=750 n (%) | ||||
| Age of sex debut, year | −1.728 | 0.084 | |||
| Median, IQR | 20, (18–23) | 20, (18–23) | 20, (18–23) | ||
| Year of sexual activity | −11.342 | <0.001 | |||
| Median, IQR | 7, (4–12) | 7, (4–11) | 10, (5–19) | ||
| Lifetime number of male sexual partners | 0.212 | 0.645 | |||
| <10 | 1,815 (50.6) | 1,430 (50.4) | 385 (51.3) | ||
| ≥10 | 1,773 (49.4) | 1,408 (49.6) | 365 (48.7) | ||
| Lifetime number of female sexual partners | 190.534 | <0.001 | |||
| 0 | 2,169 (60.5) | 1,880 (66.2) | 289 (38.5) | ||
| ≥1 | 1,419 (39.5) | 958 (33.8) | 461 (61.5) | ||
| Alcohol consumption in the past 3 month | 42.714 | <0.001 | |||
| Never | 1,574 (43.9) | 1,259 (44.4) | 315 (42) | ||
| Once a month | 1,108 (30.9) | 922 (32.5) | 186 (24.8) | ||
| 2–4 times a month | 594 (16.5) | 446 (15.7) | 148 (19.7) | ||
| ≥ twice a week | 312 (8.7) | 211 (7.4) | 101 (13.5) | ||
| Alcohol use before sex in the past 3 month | 13.176 | <0.001 | |||
| No | 2,850 (79.4) | 2,290 (80.7) | 560 (74.7) | ||
| Yes | 738 (20.6) | 548 (19.3) | 190 (25.3) | ||
| Drug use in the past 3 month | 40.831 | <0.001 | |||
| No | 2,600 (72.5) | 1,987 (70.0) | 613 (81.7) | ||
| Yes | 988 (27.5) | 851 (30.0) | 137 (18.3) | ||
| Had insertive anal sex with men in the past 3 month | 0.139 | 0.710 | |||
| No | 1,414 (39.4) | 1,114 (39.3) | 300 (40.0) | ||
| Yes | 2,174 (60.6) | 1,724 (60.7) | 450 (60.0) | ||
| Had condomless insertive anal sex with men in the past 3 month | 1.301 | 0.254 | |||
| No | 2,801 (78.1) | 2,227 (78.5) | 574 (76.5) | ||
| Yes | 787 (21.9) | 611 (21.5) | 176 (23.5) | ||
| Had receptive anal sex with men in the past 3 month | 9.721 | 0.002 | |||
| No | 1,713 (47.7) | 1,317 (46.4) | 396 (52.8) | ||
| Yes | 1,875 (52.3) | 1,521 (53.6) | 354 (47.2) | ||
| Had condomless receptive anal sex with men in the past 3 month | 4.239 | 0.039 | |||
| No | 2,855 (79.6) | 2,238 (78.9) | 617 (82.3) | ||
| Yes | 733 (20.4) | 600 (21.1) | 133 (17.7) | ||
| Had sex with women in the past 3 month | 90.868 | <0.001 | |||
| No | 3,211 (89.5) | 2,611 (92.0) | 600 (80.0) | ||
| Yes | 377 (10.5) | 227 (8.0) | 150 (20.0) | ||
| Had condomless vaginal sex with women in the past 3 month | 61.548 | <0.001 | |||
| No | 3,351 (93.4) | 2,698 (95.1) | 653 (87.1) | ||
| Yes | 237 (6.6) | 140 (4.9) | 97 (12.9) | ||
| Had anal sex with HIV-positive men in the past 3 month | 0.004 | 0.952 | |||
| No | 3,946 (97.4) | 2,765 (97.4) | 731 (97.4) | ||
| Yes | 92 (2.6) | 73 (2.6) | 19 (2.5) | ||
| Had oral sex with HIV-positive men in the past 3 month | 0.812 | 0.368 | |||
| No | 3,500 (97.5) | 2,765 (97.4) | 735 (98.0) | ||
| Yes | 88 (2.5) | 73 (2.6) | 15 (2.9) | ||
| Had anal sex with male commercial sex worker in the past 3 month | 2.313 | 0.128 | |||
| No | 3,488 (97.2) | 2,765 (97.4) | 723 (96.4) | ||
| Yes | 100 (2.3) | 73 (2.6) | 27 (3.6) | ||
| Perception of HIV risk prior to HIV diagnosis | 4.941 | 0.026 | |||
| Low or very low | 2,126 (59.3) | 1,655 (58.3) | 471 (62.8) | ||
| High or very high | 1,462 (40.7) | 1,183 (41.7) | 279 (37.2) | ||
| Ever tested for HIV | 1.666 | 0.197 | |||
| No | 1,054 (29.4) | 848 (29.9) | 206 (27.5) | ||
| Yes | 2,534 (70.6) | 1,990 (70.1) | 544 (72.5) | ||
| Newly diagnosed as HIV-positive | 6.156 | 0.013 | |||
| No | 3,133 (87.3) | 2,458 (86.6) | 675 (90.0) | ||
| Yes | 455 (12.7) | 380 (13.4) | 75 (10.0) | ||
| Newly diagnosed as syphilis seropositive | 6.046 | 0.014 | |||
| No | 3,319 (92.5) | 2,641 (93.1) | 678 (90.4) | ||
| Yes | 269 (7.5) | 197 (6.9) | 72 (9.6) | ||
Note: IQR, interquartile range; Drug use, intake of any of these drugs: methamphetamine, MDMA, rush, magu, ketamine, cannabis/marijuana, cocaine, opium, heroin, morphine in past 3 months prior to the survey
χ2 statistics from Pearson Chi square test for categorical variables; z-statistics from Wilcoxon rank-sum tests for continuous variables
DISCUSSION
Our study showed that the Internet was the most common venue for Chinese MSM to seek male sexual partners, consistent with findings from previous studies that online sex-finding has become the predominant mode among MSM in China, as in other countries [15,16,28–30]. China has been experiencing vast economic and information technology developments in the past decades, allowing an unprecedented number of people to get access to Internet [28]. The Internet has been gaining tremendous popularity among Chinese MSM, as many gay-friendly online platforms for interaction have now been established (e.g., chat rooms, gay websites, web-based gay apps, instant messaging) which help them to expand their social networks and facilitate sexual hook-ups, saving travel time and cost and improving the likelihood of finding compatible sexual partners [28,31,32]. In contrast, traditional venue-based sex-seeking has disadvantages such as time and location constraints, concerns about privacy disclosure, encountering stigma, trouble with legal authorities, and fewer opportunities to find compatible partners [33]. Nonetheless, we have highlighted that certain subgroups of Chinese MSM still preferentially frequent these venues (e.g., park, bathhouse, pub/club), but our understanding of specific factors influencing sex-finding preferences remains limited by our convenience sampling strategy. We believe that improved knowledge of the correlates of online vs. offline sex-finding can help design targeted HIV risk reduction interventions for specific MSM subgroups.
Our results were in line with previous studies assessing samples recruited online or offline [15,16,20,28,34–40] that Chinese MSM mostly using Internet to find sex were more likely to be younger, currently single, have higher education, have higher monthly income, engage in condomless receptive anal sex, or have higher odds of being HIV-positive; while less likely to drink alcohol, use alcohol before sex, have sex with women. Our study also uniquely documented that online sex-finding MSM tended to live in the city for longer, being a registered local resident, have health insurance, ever use illicit drugs, or have fewer years in sexual activity.
Participants in our study reporting mostly using Internet to find sex represented a large sample of young (63.6% were younger than 30 years old) or well-educated (78.4% with college or above education) MSM. Of particular note, student MSM (age≤ 21), a growing population affected by HIV/AIDS [41], accounted for 12% of this convenience sample population. Externally, the superior accessibility and availability of the Internet in Beijing, a large metropolitan city with high Internet access, where our survey was conducted, is a contributing factor. Our younger, higher socioeconomic status, urban MSM [42,43] may be more computer literacy, adapt more quickly to the evolution of modern information technology, and/or be more financially able to purchase computers, notebooks, smart phones, and data plan for Internet use. In contrast, the MSM in our study living in Beijing for fewer years or without Beijing ‘Hukou’ were more likely to frequent non-Internet venues. This subgroup might include a majority of transient workers (migrants) from village/township/country level cities to large cities for better employment opportunities and living condition [44,45]. These marginal population might be less educated and faced financial constraints [44], both barriers to the conduct of online sex-finding. MSM who were unemployed or retired also tended to visit traditional venues to find sex. It was possible that these MSM had more time to spend at venues, and also that lower income impeded their routine Internet use.
The patterns of high risk behaviors also varied between Internet and non-Internet sex-finding MSM. Non-Internet MSM seemed to engage in more high risk behaviors than Internet using MSM, possibly related to their higher likelihood to perceive low or very low HIV risk and their lower education attainment. Alcohol consumption and alcohol use before sex were more common among non-Internet MSM. It is highly likely that frequenting bars/clubs would greatly increase the likelihood of alcohol drinking. In contrast, drug use was more prevalent among Internet-using MSM. We speculate, along with others, that the use of the Internet has shifted MSM from fixed (the established venues, such as entertainment or leisure provision facilities with stable geographic location, where men frequent for seeking male sexual partners, e.g., business-based sauna house and bar/pub) to mobile locations (places to meet-up with more flexibility upon personal arrangement and mutual agreement between two or more men, e.g., party, hotel, apartment) where drugs are more popular [37,46,47]. Having sex with women was more prevalent among non-Internet MSM. As indicated by our finding, this bisexual subgroup included a higher proportion of MSM married to women; we also suspect that these MSM may also search for venue-based female sex workers (FSW), given that many venues house both homosexual and heterosexual commercial sex. However, we did not probe this in detail.
Given our findings indicating that Chinese MSM seeking sex via the Internet were quite different from those frequenting non-Internet venues, we highlight the importance of surveying representative samples of MSM to minimize selection bias. Moreover, specific prevention intervention strategies should be designed to match preferred sex-finding patterns [24]. Since most Chinese MSM in our Beijing study conducted online sex-seeking, Internet and information technology-based platforms must be used for the dissemination of HIV knowledge, enhancing their testing services and subsequent linkage to HIV care. For example, these can be realized by targeting and collaborating with some most frequently visited gay websites for advertising the benefits of prevention intervention programs, and developing/tailoring some gay-friendly smartphone applications to expand targeted MSM populations [16]. In the meantime, venue-based prevention interventions in collaboration with community-based organizations (CBOs), such as onsite provision of volunteer testing and counseling, HIV prevention promotion and awareness/knowledge enhancement campaign, should also be emphasized, with the consideration of accommodating specific sex-finding patterns, cultural/psychological needs, and literacy level of many Chinese MSM.
There are limitations to our study. First, our questionnaire included culturally-sensitive and private questions regarding sexual practice. Even though we trained interviewers to conduct the interviews, and used identification numbers instead of participant names in questionnaires and blood specimens, recall bias and social desirability bias could not be excluded. Second, we did not further ascertain sub-categories of Internet-based sex-seeking channels (e.g., E-mail, forum, chat room, social networking platforms, smartphone-based apps, etc.), or survey frequency distribution of the ‘Other’ subgroup of the non-Internet venue, which limited our ability to examine a detailed spectrum of these channels and how they may vary in terms of their sexual risk. Third, only a convenience sample of MSM in Beijing were recruited without using a sophisticated sampling frame (e.g. Respondent driven sampling, RDS), which limits the generalizability of our findings. Despite these limitations, strengths of our study include that it is among just very few studies among Chinese MSM to reveal socio-demographic and behavioral distinction between online and offline sex-seeking MSM; it is also among the largest such studies. We believe that our findings provide valuable guidance for future interventions and investigations among MSM in large Chinese cities.
CONCLUSIONS
In conclusion, MSM who seek sex via the Internet and via specific venues both represent high HIV risk populations. The emergence of Internet-based sex-finding websites has become a major force for propelling HIV transmission among Chinese MSM. Innovated intervention implementation strategies are needed. Knowledge of the factors that correlate with Internet vs. venue-based sex-finding can help guide targeted intervention implementations in such high-risk populations.
ACKNOWLEDGEMENTS
This research was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Numbers R01AI094562 and R34AI091446. We thank volunteers from Chaoyang Chinese AIDS Volunteer Group, staff from Xicheng and Chaoyang District Center for Disease Control and Prevention, for their assistance in recruiting the participants, collecting data, and conducting focus group discussions.
Footnotes
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Conflict of interest: The authors declare that they have no conflict of interest
REFERENCES
- 1.Lou J, Blevins M, Ruan Y, et al. Modeling the impact on HIV incidence of combination prevention strategies among men who have sex with men in Beijing, China. PLoS One. 2014;9(3):e90985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.State Council AIDS Working Committee Office (SCAWCO):China. UNGASS Country Progress Report; Beijing: 2014. CMoHotPsRoC. [Google Scholar]
- 3.Zhong F, Liang B, Xu H, et al. Increasing HIV and Decreasing Syphilis Prevalence in a Context of Persistently High Unprotected Anal Intercourse, Six Consecutive Annual Surveys among Men Who Have Sex with Men in Guangzhou, China, 2008 to 2013. PLoS One. 2014;9(7):e103136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bai X, Luo S, Wang X, et al. [Change of risky sexual behaviors among men who have sex with men before and after recent identification of HIV diagnosis]. Zhonghua Liu Xing Bing Xue Za Zhi. May 2014;35(5):489–493. [PubMed] [Google Scholar]
- 5.Chang YH, Liu WC, Chang SY, et al. Associated factors with syphilis among human immunodeficiency virus-infected men who have sex with men in Taiwan in the era of combination antiretroviral therapy. J Microbiol Immunol Infect. December 31 2013. [DOI] [PubMed] [Google Scholar]
- 6.Wang QQ, Chen XS, Yin YP, et al. HIV prevalence, incidence and risk behaviours among men who have sex with men in Yangzhou and Guangzhou, China: a cohort study. J Int AIDS Soc. 2014;17(1):18849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu Y, Sun X, Qian HZ, et al. Qualitative Assessment of Barriers and Facilitators of Access to HIV Testing Among Men Who Have Sex with Men in China. AIDS Patient Care STDS. September 2015;29(9):481–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davis A, Best J, Wei C, et al. Intimate Partner Violence and Correlates With Risk Behaviors and HIV/STI Diagnoses Among Men Who Have Sex With Men and Men Who Have Sex With Men and Women in China: A Hidden Epidemic. Sex Transm Dis. July 2015;42(7):387–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tang W, Huan X, Mahapatra T, et al. Factors associated with unprotected anal intercourse among men who have sex with men: results from a respondent driven sampling survey in Nanjing, China, 2008. AIDS Behav. May 2013;17(4):1415–1422. [DOI] [PubMed] [Google Scholar]
- 10.Li Y, Xu J, Reilly KH, et al. Prevalence of HIV and Syphilis Infection among High School and College Student MSM in China: A Systematic Review and Meta-Analysis. PLoS One. 2013;8(7):e69137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu H, Han Y, He X, et al. Alcohol use and HIV risk taking among Chinese MSM in Beijing. Drug Alcohol Depend. July 19 2013. [DOI] [PubMed] [Google Scholar]
- 12.Liu J, Qu B, Ezeakile MC, Zhang Y, Liang S. Factors associated with HIV infection among men who have sex with men in Henan Province, China: a cross-sectional study. BMC Public Health. 2013;13:356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruan Y, Luo F, Jia Y, et al. Risk factors for syphilis and prevalence of HIV, hepatitis B and C among men who have sex with men in Beijing, China: implications for HIV prevention. AIDS Behav. August 2009;13(4):663–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Qi J, Zhang D, Fu X, et al. High Risks of HIV Transmission for Men Who Have Sex with Men - A Comparison of Risk Factors of HIV Infection among MSM Associated with Recruitment Channels in 15 Cities of China. PloS one. 2015;10(4):e0121267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lau JT, Zhao JK, Wu XB, Gu J, Hao C. Gay saunas and the risks of HIV and syphilis transmissions in China--results of a meta-analysis. J Sex Med. March 2013;10(3):642–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bien CH, Best JM, Muessig KE, Wei C, Han L, Tucker JD. Gay Apps for Seeking Sex Partners in China: Implications for MSM Sexual Health. AIDS Behav. June 2015;19(6):941–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bai X, Xu J, Yang J, et al. HIV prevalence and high-risk sexual behaviours among MSM repeat and first-time testers in China: implications for HIV prevention. J Int AIDS Soc. 2014;17:18848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The World Bank. Internet users as percentage of population. https://www.google.com/publicdata/explore?ds=d5bncppjof8f9_&met_y=it_net_user_p2&idim=country:CHN:IND:USA&hl=en&dl=en (Data updated July 27, 2015. Accessed October 15, 2015.).
- 19.Lau JT, Lau M, Cheung A, Tsui HY. A randomized controlled study to evaluate the efficacy of an Internet-based intervention in reducing HIV risk behaviors among men who have sex with men in Hong Kong. AIDS Care. August 2008;20(7):820–828. [DOI] [PubMed] [Google Scholar]
- 20.Tsui HY, Lau JT. Comparison of risk behaviors and socio-cultural profile of men who have sex with men survey respondents recruited via venues and the internet. BMC Public Health. 2010;10:232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu Z, Xu J, Liu E, et al. HIV and syphilis prevalence among men who have sex with men: a cross-sectional survey of 61 cities in China. Clin Infect Dis. July 2013;57(2):298–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kerr ZY, Pollack LM, Woods WJ, Blair J, Binson D. Use of multiple sex venues and prevalence of HIV risk behavior: identifying high-risk men who have sex with men. Arch Sex Behav. February 2015;44(2):443–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhao J, Chen L, Cai WD, et al. HIV infection and sexual behaviors among non-commercial men who have sex with men at different venues. Arch Sex Behav. May 2014;43(4):801–809. [DOI] [PubMed] [Google Scholar]
- 24.Hernandez-Romieu AC, Sullivan PS, Sanchez TH, et al. The comparability of men who have sex with men recruited from venue-time-space sampling and facebook: a cohort study. JMIR Res Protoc. 2014;3(3):e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sanchez T, Smith A, Denson D, Dinenno E, Lansky A. Internet-based methods may reach higher-risk men who have sex with men not reached through venue-based sampling. Open AIDS J. 2012;6:83–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hernan MA, Hernandez-Diaz S, Werler MM, Mitchell AA. Causal knowledge as a prerequisite for confounding evaluation: an application to birth defects epidemiology. Am J Epidemiol. January 15 2002;155(2):176–184. [DOI] [PubMed] [Google Scholar]
- 27.Kipp AM, Pungrassami P, Nilmanat K, et al. Socio-demographic and AIDS-related factors associated with tuberculosis stigma in southern Thailand: a quantitative, cross-sectional study of stigma among patients with TB and healthy community members. BMC Public Health. 2011;11:675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li Q, Liu Y, Zhou Z, et al. Online sex-seeking behaviors among men who have sex with men: implications for investigation and intervention. AIDS Behav. August 2012;16(6):1690–1698. [DOI] [PubMed] [Google Scholar]
- 29.Klein H HIV risk practices sought by men who have sex with other men, and who use internet websites to identify potential sexual partners. Sex Health. September 2008;5(3):243–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosser BR, Miner MH, Bockting WO, et al. HIV risk and the internet: results of the Men’s INTernet Sex (MINTS) Study. AIDS Behav. August 2009;13(4):746–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gravningen K, Aicken CR, Schirmer H, Mercer CH. Meeting sexual partners online: associated sexual behaviour and prevalent chlamydia infection among adolescents in Norway: a cross-sectional study. Sex Transm Infect. August 12 2015. [DOI] [PubMed] [Google Scholar]
- 32.Wall KM, Stephenson R, Sullivan PS. Frequency of sexual activity with most recent male partner among young, Internet-using men who have sex with men in the United States. J Homosex. 2013;60(10):1520–1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ross MW, Rosser BR, McCurdy S, Feldman J. The advantages and limitations of seeking sex online: a comparison of reasons given for online and offline sexual liaisons by men who have sex with men. J Sex Res. February 2007;44(1):59–71. [DOI] [PubMed] [Google Scholar]
- 34.Huang L, Nehl EJ, Lin L, et al. Sociodemographic and sexual behavior characteristics of an online MSM sample in Guangdong, China. AIDS Care. 2014;26(5):648–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang Z, Zhang S, Dong Z, Jin M, Han J. Prevalence of unprotected anal intercourse in men who have sex with men recruited online versus offline: a meta-analysis. BMC Public Health. 2014;14:508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang D, Bi P, Lv F, Tang H, Zhang J, Hiller JE. Internet use and risk behaviours: an online survey of visitors to three gay websites in China. Sex Transm Infect. December 2007;83(7):571–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee SS, Tam DK, Mak DW, Wong KH. Use of the Internet for sex partnership in men who have sex with men before HIV infection. Public Health. July 2011;125(7):433–435. [DOI] [PubMed] [Google Scholar]
- 38.Muessig KE, Bien CH, Wei C, et al. A mixed-methods study on the acceptability of using eHealth for HIV prevention and sexual health care among men who have sex with men in China. J Med Internet Res. 2015;17(4):e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jin M, Yang Z, Dong Z, Han J. Correlates of consistent condom use among men who have sex with men recruited through the Internet in Huzhou city: a cross-sectional survey. BMC Public Health. 2013;13:1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lau JT, Kim JH, Lau M, Tsui HY. Prevalence and risk behaviors of Chinese men who seek same-sex partners via the internet in Hong Kong. AIDS Educ Prev. December 2003;15(6):516–528. [DOI] [PubMed] [Google Scholar]
- 41.Guo J, Huang XJ, Wang XB, Weng HY, Guo W. [Estimation on the size of men who have sex with men among college students in Beijing through the Network Scale-Up Method (NSUM)]. Zhonghua Liu Xing Bing Xue Za Zhi. November 2013;34(11):1080–1082. [PubMed] [Google Scholar]
- 42.Qian HZ, Ruan Y, Liu Y, et al. Lower HIV risk among circumcised men who have sex with men in China: Interaction with anal sex role in a cross-sectional study. J Acquir Immune Defic Syndr. September 21 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu Y, Qian HZ, Ruan Y, et al. Alcohol use among Chinese men who have sex with men: an epidemiological survey and meta-analysis. Biomed Res Int. 2014;2014:414381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang B, Li X, Stanton B, Liu Y, Jiang S. Socio-demographic and behavioral correlates for HIV and syphilis infections among migrant men who have sex with men in Beijing, China. AIDS Care. 2013;25(2):249–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mao H, Ma W, Lu H, et al. High incidence of HIV and syphilis among migrant men who have sex with men in Beijing, China: a prospective cohort study. BMJ Open. 2014;4(9):e005351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Halkitis PN, Parsons JT, Wilton L. Barebacking among gay and bisexual men in New York City: explanations for the emergence of intentional unsafe behavior. Arch Sex Behav. August 2003;32(4):351–357. [DOI] [PubMed] [Google Scholar]
- 47.Boddiger D Metamphetamine use linked to rising HIV transmission. Lancet. April 2–8 2005;365(9466):1217–1218. [DOI] [PubMed] [Google Scholar]


